Virtual Reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and Binge Eating Disorder: A Systematic Review
Abstract
:1. Introduction
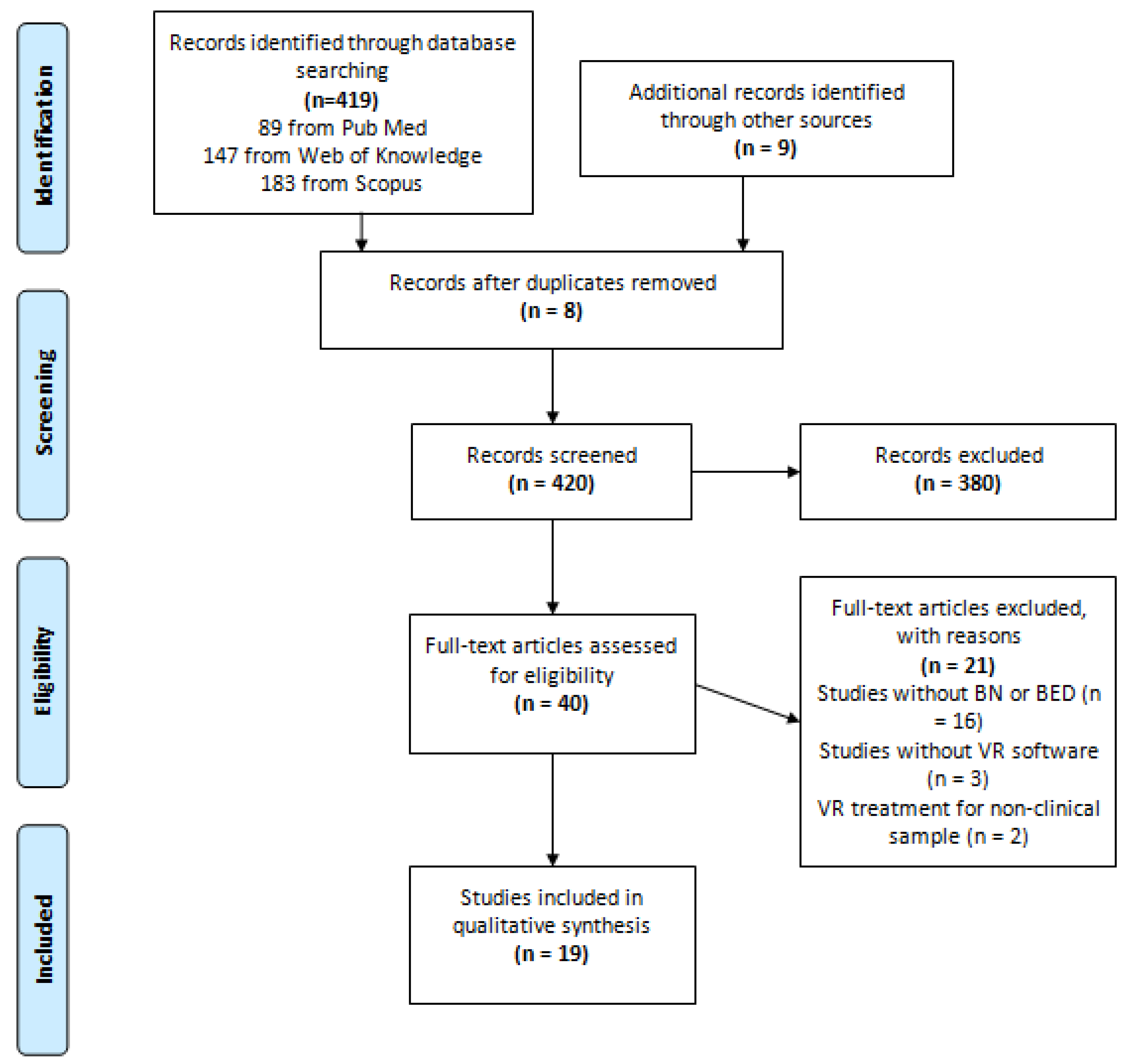
2. Methods
3. Results
3.1. VR in the Assessment of BN and BED
3.2. VR in the Treatment of BN and BED
3.2.1. Case Report
3.2.2. Non-Controlled Clinical Trials
3.2.3. Randomized Controlled Trials
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Whiteford, H.A.; Ferrari, A.J.; Degenhardt, L.; Feigin, V.; Vos, T. The Global Burden of Mental, Neurological and Substance Use Disorders: An Analysis from the Global Burden of Disease Study 2010. PLoS ONE 2015, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.; Degenhardt, L.; Rehm, J.; Baxter, A.; Ferrari, A.; Erskine, H.; Charlson, F.; Norman, R.; Flaxman, A.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Smink, F.; Hoeken, D.; Hoek, H. Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; (DSM-5); American Psychiatric Association Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Brooks, S.; Rask-Andersen, M.; Benedict, C.; Schiöth, H. A debate on current eating disorder diagnoses in light of neurobiological findings: Is it time for a spectrum model? BMC Psychiatry 2012, 12, 76. [Google Scholar] [CrossRef] [PubMed]
- Vervaet, M.; Van Heeringen, C.; Audenaert, K. Personality-Related Characteristics in Restricting Versus Binging and Purging Eating Disordered Patients. Compr. Psychiatry 2004, 45, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Pennesi, J.-L.; Wade, T.D. A systematic review of the existing models of disordered eating: Do they inform the development of effective interventions? Clin. Psychol. Rev. 2016, 43, 175–192. [Google Scholar] [CrossRef] [PubMed]
- Ahrberg, M.; Trojca, D.; Nasrawi, N.; Vocks, S. Body image disturbance in binge eating disorder: A review. Eur. Eat. Disord. Rev. 2011, 19, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.B.; Lewis, R.J. Assessing the roles of impulsivity, food-related cognitions, BMI, and demographics in the dual pathway model of binge eating among men and women. Eat. Behav. 2015, 18, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Stice, E. Interactive and Mediational Etiologic Models of Eating Disorder Onset: Evidence from Prospective Studies. Annu. Rev. Clin. Psychol. 2016, 12, 359–381. [Google Scholar] [CrossRef] [PubMed]
- Claes, L.; Robinson, M.D.; Muehlenkamp, J.J.; Vandereycken, W.; Bijttebier, P. Differentiating bingeing/purging and restrictive eating disorder subtypes: The roles of temperament, effortful control, and cognitive control. Pers. Individ. Dif. 2010, 48, 166–170. [Google Scholar] [CrossRef]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W.; Hannay, H.J.; Fischer, J.S. Neuropsychological Assessment, 4th ed.; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Wu, M.; Hartmann, M.; Skunde, M.; Herzog, W.; Friederich, H.C. Inhibitory control in bulimic-type eating disorders: A systematic review and meta-analysis. PLoS ONE 2013, 8, e83412. [Google Scholar] [CrossRef] [PubMed]
- Racine, S.E.; Culbert, K.M.; Larson, C.L.; Klump, K.L. The possible influence of impulsivity and dietary restraint on associations between serotonin genes and binge eating. J. Psychiatr. Res. 2009, 43, 1278–1286. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, U.; Campbell, I.C. Treatment of eating disorders can not remain “brainless”: The case for brain-directed treatments. Eur. Eat. Disord. Rev. 2013, 21, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Reeve, S.; Robinson, A.; Ehlers, A.; Clark, D.; Spanlang, B.; Slater, M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 2017, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Rizzo, A.A. The application of virtual reality technology in rehabilitation. Rehabil. Psychol. 2001, 46, 296–311. [Google Scholar] [CrossRef]
- Baños, R.M.; Botella, C.; Guerrero, B.; Liaño, V.; Alcañiz, M.; Rey, B. The third pole of the sense of presence: Comparing virtual and imagery spaces. Psychnol. J. 2005, 3, 90–100. [Google Scholar]
- North, M.M.; North, S.M. Virtual Reality Therapy. In Computer-Assisted and Web-Based Innovations in Psychology, Special Education, and Health; Academic Press: London, UK, 2016; pp. 141–156. [Google Scholar]
- De Carvalho, M.R.; De Freire, R.C.; Nardi, A.E. Virtual reality as a mechanism for exposure therapy. World J. Biol. Psychiatry 2010, 11, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Valmaggia, L.R.; Latif, L.; Kempton, M.J.; Rus-Calafell, M. Virtual reality in the psychological treatment for mental health problems: A systematic review of recent evidence. Psychiatry Res. 2016, 236, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Gutierrez-Maldonado, J.; Riva, G. Virtual reality based treatments in eating disorders and obesity: A review. J. Contemp. Psychother. 2013, 43, 207–221. [Google Scholar] [CrossRef]
- Koskina, A.; Campbell, I.C.; Schmidt, U. Exposure therapy in eating disorders revisited. Neurosci. Biobehav. Rev. 2013, 37, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Maldonado, J.; Ferrer-García, M.; Caqueo-Urízar, A.; Letosa-Porta, A. Assessment of Emotional Reactivity Produced by Exposure to Virtual Environments in Patients with Eating Disorders. Cyberpsychol. Behav. 2006, 9, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Gutierrez-Maldonado, J.; Caqueo-Urizar, A.; Moreno, E. The Validity of Virtual Environments for Eliciting Emotional Responses in Patients with Eating Disorders and in Controls. Behav. Modif. 2009, 33, 830–854. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Maldonado, J.; Ferrer-García, M.; Caqueo-Urízar, A.; Moreno, E. Body Image in Eating Disorders: The Influence of Exposure to Virtual-Reality Environments. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Gorini, A.; Griez, E.; Petrova, A.; Riva, G.; Pull, C.; Gorini, A.; Riva, G.; Gregg, L.; Tarrier, N.; Barfield, W.; et al. Assessment of the emotional responses produced by exposure to real food, virtual food and photographs of food in patients affected by eating disorders. Ann. Gen. Psychiatry 2010, 9, 30. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Gutierrez-Maldonado, J. Virtual reality exposure in patients with eating disorders: influence of symptom severity and presence. Stud. Health Technol. Inform. 2011, 167, 80–85. [Google Scholar] [PubMed]
- Perpiñá, C.; Roncero, M.; Fernández-Aranda, F.; Jiménez-Murcia, S.; Forcano, L.; Sánchez, I. Clinical validation of a virtual environment for normalizing eating patterns in eating disorders. Compr. Psychiatry 2013, 54, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Gutiérrez-Maldonado, J.; Pla-Sanjuanelo, J.; Vilalta-Abella, F.; Andreu-Gracia, A.; Dakanalis, A.; Fernandez-Aranda, F.; Fuste-Escolano, A.; Ribas-Sabate, J.; Riva, G.; et al. ExternalEating as a PredictorofCue-reactivitytoFood-related Virtual Environments. Stud. Health Technol. Inform. 2015, 219, 117–122. [Google Scholar] [PubMed]
- Pla-Sanjuanelo, J.; Ferrer-Garcia, M.; Gutiérrez -Maldonado, J.; Vilalta-Abella, F.; Andreu-Gracia, A.; Dakanalis, A.; Fernandez-Aranda, F.; Fuste-Escolano, A.; Ribas-Sabate, J.; Riva, G.; et al. TraitandStateCraving as IndicatorsofValidityof VR-based Software for BingeEatingTreatment. Stud. Health Technol. Inform. 2015, 219, 141–146. [Google Scholar] [PubMed]
- Perpinã, C.; Roncero, M. Similarities and differences between eating disorders and obese patients in a virtual environment for normalizing eating patterns. Compr. Psychiatry 2016, 67, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Perpiñá, C.; Botella, C.; Baños, R.; Marco, H.; Alcañiz, M.; Quero, S. Body image and virtual reality in eating disorders: Is exposure to virtual reality more effective than the classical body image treatment? Cyberpsychol. Behav. 1999, 2, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Rinaldi, S.; Vincelli, F.; Molinari, E. Virtual reality-based experiential cognitive treatment of obesity and binge-eating disorders. Clin. Psychol. Psychother. 2000, 7, 209–219. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Cirillo, G.; Molinari, E. Virtual Reality Environment for Body Image Modification: A Multidimensional Therapy for the Treatment of Body Image in Obesity and Related Pathologies. Cyberpsychol. Behav. 2000, 3, 421–431. [Google Scholar] [CrossRef]
- Riva, G.; Bacchetta, M.; Baruffi, M.; Molinari, E. Virtual-reality-based multidimensional therapy for the treatment of body image disturbances in binge eating disorders: A preliminary controlled study. IEEE Trans. Inf. Technol. Biomed. 2002, 6, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bacchetta, M.; Cesa, G.; Conti, S.; Molinari, E. Six-Month Follow-Up of In-Patient Experiential Cognitive Therapy for Binge Eating Disorders. Cyberpsychol. Behav. 2003, 6, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bacchetta, M.; Cesa, G.; Conti, S.; Molinari, E. The use of VR in the treatment of eating disorders. Stud. Health Technol. Inform. 2004, 99, 121–163. [Google Scholar] [PubMed]
- Marco, J.H.; Perpiñá, C.; Botella, C. Effectiveness of cognitive behavioral therapy supported by virtual reality in the treatment of body image in eating disorders: One year follow-up. Psychiatry Res. 2013, 209, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Cesa, G.L.; Manzoni, G.M.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cardenas-López, G.; Riva, G. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: Randomized controlled study with one-year follow-up. J. Med. Internet Res. 2013, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Roncero, M.; Perpiñá, C. Normalizing the eating pattern with virtual reality for bulimia nervosa: A case report. Rev. Mex. Trastor. Aliment. 2015, 6, 152–159. [Google Scholar] [CrossRef]
- Perpiñá, C.; Marco, J.H.; Botella, C.; Baños, R. Tratamiento de laimagen corporal enlostrastornosalimentarios mediante tratamiento cognitivo-comportamental apoyadoconrealidad virtual: Resultados al año de seguimiento. Psicol. Conductual 2004, 12, 519–537. [Google Scholar]
- Riva, G.; Bolzoni, M.; Carella, F.; Galimberti, C.; Griffin, M.J.; Lewis, C.H.; Luongo, R.; Mardegan, P.; Melis, L.; Molinari-Tosatti, L.; et al. Virtual Reality Environments for Psycho-Neuro-Physiological Assessment and Rehabilitation. Stud. Health Technol. Inform. 1997, 39, 34–45. [Google Scholar] [PubMed]
- Fairburn, C.G.; Marcus, M.D.; Wilson, G.T. Cognitive-behavioral therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. In Binge Eating: Nature, Assessment, and Treatment; Weill Cornell Medical College: New York, NY, USA, 1993; pp. 361–404. [Google Scholar]
- Fairburn, C.; Garner, D.; Garnfinkel, P. Cognitive-Behavioral Treatment for Bulimia. In Handbook of Psychotherapy for Anorexia and Bulimia; Gamer, D.M., Garnfinkel, P.E., Eds.; Guilford Press: New York, NY, USA, 1985; pp. 160–192. [Google Scholar]
- Fairburn, C. Overcoming Binge Eating; Guilford Press: New York, NY, USA, 1995. [Google Scholar]
- Garner, D.; Vitousek, K.; Pike, K. Cognitive-Behavioral Therapy for AN. In Handbook of Treatment for Eating Disorders; Garner, D., Garfinkel, P., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 94–145. [Google Scholar]
- Wilson, T.; Fairburn, C.; Agras, W. Cognitive-Behavioral Therapy for Bulimia Nervosa. In Handbook of Treatment for Eating Disorders; Garner, D., Garfinkel, P., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 67–93. [Google Scholar]
- Butters, J.; Cash, T. Cognitive-behavioral treatment of women’s body-image dissatisfaction. J. Consult. Clin. Psychol. 1987, 55, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Perpiñá, C.; Botella, C.; Baños, R. Imagen Corporal em Los Trastornos Alimentarios. In Evaluación y Tratamiento por Medio de Realidad Virtual; Promolibro: Valencia, Spain, 2000. [Google Scholar]
- Ricca, V.; Mannucci, E.; Zucchi, T.; Rotella, C.M.; Faravelli, C. Cognitive-behavioural therapy for bulimia nervosa and binge eating disorder. A review. Psychother. Psychosom. 2000, 69, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K.; Riva, G.; Gutiérrez-Maldonado, J. Virtual Reality in the Assessment and Treatment of Weight-Related Disorders. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.; Villa, H.; Garcia-Palacios, A.; Baños, R.; Perpiñá, C.; Alcañiz, M. Clinically significant virtual environments for the treatment of panic disorder and agoraphobia. Cyberpsychol. Behav. 2004, 7, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Baños, R.; Botella, C.; Mantovani, F.; Gaggioli, A. Transforming Experience: The Potential of Augmented Reality and Virtual Reality for Enhancing Personal and Clinical Change. Front. Psychiatry 2016, 7, 164. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.; Emmelkamp, P. Virtual reality exposure therapy for anxiety disorders: A meta-analysis. J. Anxiety Disord. 2008, 22, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Gaudio, S.; Dakanalis, A. The Neuropsychology of Self Objectification. Eur. Psychol. 2015, 20, 34–43. [Google Scholar] [CrossRef]
- Riva, G. Out of my real body: Cognitive neuroscience meets eating disorders. Front. Hum. Neurosci. 2014, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.; Cesa, G.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Riva, G. Virtual Reality-Enhanced Cognitive-Behavioral Therapy for Morbid Obesity: A Randomized Controlled Study with 1 Year Follow-Up. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-garcía, M.; Gutiérrez-maldonado, J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples : A review of the literature. Body Image 2012, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bohon, C.; Stice, E. Negative affect and neural response to palatable food intake in bulimia nervosa. Appetite 2012, 58, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Jones, A.; Lepage, L.; CONSORT Group. Use of the CONSORT Statement and Quality of Reports of Randomized Trials. JAMA 2001, 285, 1992–1995. [Google Scholar] [CrossRef] [PubMed]
| Study | Sample Size (M/F) | Diagnostic | Study Design | Intervention | Software Characteristics | Sessions | Follow-up | Instruments | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Gutiérrez-Maldonado et al. (2006) [24] | 30 (0/30) AN: 17 (0/17) BN:11 (0/11) EDNOS: 2 (0/2) | AN BN EDNOS | NCAS | Exposure to food and people. | 6 VR environments: living-room, kitchen with high calorie food, a kitchen with low-calorie food, a restaurant with high-calorie food, a restaurant with low-calorie food, swimming-pool. | 1 | - | STAI, CDB, EDI-2, PQ. | Higher state anxiety in the high-calorie food situations and the swimming-pool than in the neutral environment. Higher depressed mood in the high-calorie food situations. Significant differences on the level of state anxiety and depression mood comparing low-calorie and high-calorie food environments; no differences were found between environments with people and those without. AN and BN patients responded with similar levels of emotional intensity to the different situations. VR was useful for eliciting emotional reactions |
| Ferrer-García et al. (2009) [25] | 193 (0/193) ClG: 85 (0/85) (AN: 49, BN:22, EDNOS:14) CG: 108 (0/108) | AN BN EDNOS | CAS | Exposure to food and people. | 6 VR environments: neutral, kitchen with high calorie food, a kitchen with low-calorie food, a restaurant with high-calorie food, a restaurant with low-calorie food, swimming-pool. | 1 | - | EAT, STAI, CDB. | ED patients showed significantly higher levels of anxiety and depressed mood in the high-calorie food environments and the swimming pool than in the neutral room. ED patients’ anxiety increased when other people were present, but in high-calorie environments, their anxiety increased when they were alone. ED patients showed a more depressed mood after eating low-calorie food when other people were present. After eating high-calorie food, they felt more depressed when they were alone. VR was useful for eliciting emotional reactions. |
| Gutiérrez-Maldonado et al. (2010) [26] | 193 (0/193) ClG: 85 (0/85) (AN: 49, BN:22, EDNOS:14) CG: 108 (0/108) | AN BN EDNOS | CAS | Exposure to food and people. | 4 VR environments: kitchen with high calorie food, a kitchen with low-calorie food, a restaurant with high-calorie food, a restaurant with low-calorie food. | 1 | - | EAT, BIAS. | ED patients showed more BI distortion and body dissatisfaction in the high-calorie food environments than in the low calorie food environments. People variable was not significant. BN patients showed greater BI distortion when were alone after eating high-calorie food than after eating low-calorie food. Where the patient was accompanied, BI distortion levels were similar, regardless of the kind of food. AN and EDNOS patients presented higher levels of body distortion after eating high-calorie food than after eating low-calorie food, independently of the presence or absence of people. BI distortion and BI dissatisfaction can be influenced by VR situational factors. |
| Gorini et al. (2010) [27] | ClG:20 (0/20) (AN:10, BN:10) CG:10 (0/10) | AN, BN (DSM-IV) | CAS | RF PH VR | Small restaurant with a buffet table, 6 foods. | 1 | - | EDI-2, STAI-S, VAS-A, ITC-SOPI. | Higher level of anxiety for patients compared to control. Patients felt more anxious when exposed to real and virtual food than to the pictures of food. Patients showed higher heart rate and skin conductance compared to control group. Their level of physiological anxiety was higher in the RF and VR condition, than in the PH condition. Higher sense of presence was associated with higher levels of anxiety. Virtual food was as effective as real food, and more effective than photographs, in producing psychological and physiological responses in ED patients. |
| Ferrer-García and Gutiérrez-Maldonado (2011) [28] | 71 (0/71) (AN:49, BN:22) | AN, BN | NCAS | Exposure to food and people. | 5 VR environments: neutral room, kitchen with high calorie food, a kitchen with low-calorie food, a restaurant with high-calorie food, a restaurant with low-calorie food. | 1 | - | EAT-26, PQ. | High-calorie environments and social situations produced the highest levels of subjective discomfort. Patients with severe symptomatology showed a higher subjective discomfort in all environments than with moderate symptoms. Reported sense of presence was low. Patients with high sense of presence showed the highest levels of subjective discomfort in all food situations. |
| Perpiñá et al. (2013) [29] | ClG:22 (0/22) (AN:11, BN:4, EDNOS:7) CG:37 (0/37) | AN, BN, EDNOS (DSM-IV-TR) | CAS | Exposure to food. | Kitchen with 2 areas: prep area and area with a table and a chair. | 1 | - | BDI-II, BAI, RS, RJPQ, ITC-SOPI. | Before eating patients showed moderate–high scores on control urge to eat, fear, avoidance; and low desire to eat. After eating, they reported feelings of putting on weight, urge to continue eating, of being upset etc.; and reported wanted actions: to do exercise to “compensate”, to continue eating, to continue with their daily routine, to purge. Patients showed a high reality judgment and sense of presence and scored higher on emotional involvement, attention and negative effects. VR software was clinically meaningful to patients. |
| Ferrer-García et al. (2015) [30] | ClG: 40 (10/30) (BN:23, BED:17) CG: 78 (9/69) | BN, BED (DSM-5) | CAS | Exposure to food. | 4 VR scenarios (kitchen, dining room, bedroom, and bakery/café) + 10 foods (of 30 available foods that elicit craving). | 1 | - | DEBQ. | BN and BED patients showed higher levels of emotional, external and restrictive eating and food craving than controls. External eating was associated with food craving both in patients and controls. VR was useful for inducing food craving in BN and BED patients. |
| Pla-Sanjuanelo et al. (2015) [31] | 118 (19/99) ClG: 40 (10/30) (BED: 17 BN:23) CG: 78 (9/69) | BED (DSM-5) BN (SCID-I) | CAS | Exposure to Food. | 4 VR scenarios + 10 foods (of 30 available foods that elicit craving). | 1 | - | FCQ-T, FCQ-S. | Participants with higher levels of trait and state-craving showed a greater desire to eat during exposure to virtual foods. State-craving was associated with perceived craving experience in both groups during VR exposure. VR-CET model may be helpful in improving the treatment of BE and BN patients. |
| Perpiñá and Roncero (2016) [32] | 62 (0/62) ED: 20 (0/20) (AN:10, BN:4, EDNOS:6) Obese: 19 (0/19) CG:23 (0/23) | AN, BN, EDNOS (DSM-IV-TR) Obesity | CAS | Exposure to food. | Kitchen with 2 areas: prep area and area with a table and a chair. | 1 (30 min.) | - | RJPQ, ITC-SOPI. | ED group had the highest scores on emotional involvement, attention, reality judgment and presence, negative effects. Obese group had the lowest scores on reality judgment and presence, satisfaction, sense of physical space in VE experience. Attribution of reality to the virtual eating was predicted by engagement and belonging to the ED group. The palatability of a virtual food was predicted by attention capturing and belonging to the obese group. The level of emotional reactivity to VR proportionally increased the sense of presence. VR was useful for assessing and measuring ED patients’ responses in a naturalistic setting. |
| Study | Sample Size (M/F) | Diagnostic | Study Design | Intervention | Software Characteristics | Sessions | Follow-Up | Instruments | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Treatment | |||||||||
| Perpiñá et al. (1999) [33] | 13 (0/13) AN: 7 (0/7) BN: 6 (0/6) | AN, BN (DSM-IV) | RCCT | SBIT+VR SBIT + Relaxation | 6 situations: Accommodation zone, food area with a virtual balance, room with posters, room with mirrors, a doorframe with strips and a zone to contrast body areas. | SBIT: 8 (3 h, weekly, group) Relaxation: 6 (1 h, weekly) VR: 6 (1 h, weekly). | - | BDI, PANAS, EAT, RS, BITE, EDI-2, BSQ, BIAQ, BAT, BES, BIATQ, ASI, SIBID, BASS. | VR condition participants showed a greater improvement in specific BI variables, depression and anxiety when compared to non-VR group. VR was a helpful tool for confronting the patients with BI distortions. |
| Riva et al. (2000) [34] | 43 (0/43) Obese: 18 (0/18) BED: 25 (0/25) | Obesity (BMI>35) BED (DSM-IV) | NCCT | VEBIM 2 (ECT) | VEBIM 2 Different zones (Sitting-room, dining-room, kitchen, bedroom, working environments etc.). | 5 (biweekly). | - | MMPI-2, EDI-2, BSS, BIAQ, FRS, CDRS. | In both groups, results showed a reduced level of body dissatisfaction, an improvement on social activities and a reduced use of disguising clothes. Obtained data were promising, but controlled and follow-up studies are needed to test this VR approach. |
| Riva et al. (2000) [35] | 57 (0/57) Obese: 18 (0/18) BED: 25 (0/25) EDNOS: 14 (0/14) | Obesity (BMI>35) BED, EDNOS (DSM-IV) | NCCT | VEBIM 2 | VEBIM 2 Different zones (Sitting-room, dining-room, kitchen, bedroom, working environments etc.). | 5 (biweekly). | - | BSS, BIAQ, FRS, CDRS. | All groups showed a reduced level of body dissatisfaction, an improvement on social activities and a reduced use of disguising clothes. In the EDNOS group the reduction in body dissatisfaction was slighter than in other samples. VR-based treatment could be useful to BI modification in obesity, BED and EDNOS; but more studies are needed. |
| Riva et al. (2002) [36] | 20 (0/20) | BED (DSM-IV) | RCCT | VR (+LCD+PT) PN (+LCD +PT) | VREDIM Different zones (Room with balance, drawing room, kitchen, dining room, bathroom, office, beach, supermarket etc.). | VR: 7 (50 min.) LCD: daily PT: NR (at least 30 min. walk/twice a week) PN: NR (3 times a week). | - | DIET, STAI, AI, WELSQ, URICA, BSS, BIAQ, FRS, CDRS. | VR treatment showed reduced level of body dissatisfaction and anxiety, increased self-efficacy and motivation for change, reduced concern about social judgment and reduced overeating. PN group presented anxiety reduction on the AI, but it was not confirmed by the STAI score. VR was more effective than PN on body satisfaction improvement, overeating and anxiety level reduction. VR-based therapy improved BI treatment. |
| Riva et al. (2003) [37] | 36 (0/36) | BED (DSM-IV) | RCCT | ECT (+NG+PT) CBT (+NG +PT) NG (+PT) WL | VREDIM Different zones (Room with balance, drawing room, kitchen, dining room, bathroom, office, beach, supermarket etc.). | ECT: 15 (over 6 weeks) 10 VR sessions CBT: 15 (over 6 weeks) NG: 5 (weekly). | 6 months | DIET, STAI, BDI II, RAS, RSEQ, WELSQ, URICA, BSS, BIAQ, CDRS. | ECT decreased anxiety and depression and improved assertive behavior. CBT decreased depression. NG decreased anxiety. All interventions groups improved patients’ self-esteem, eating control, eating self-efficacy, weight loss. They also reduced binge episodes. ECT was more effective than CBT on improving overall psychological state, body image, body satisfaction and resistance to social pressure. At follow-up, ECT improved body satisfaction and self-esteem and reduced the frequency of binge episodes when compared to CBT and NG. VR-based therapy improved BED patients’ treatment. |
| Riva et al. (2004) [38] | 120 (0/120) Obese: 68 (0/68) BED: 36 (0/36) BN: 12 (0/12) EDNOS: 3 (0/3) | Obesity, BED, BN, EDNOS | RCCT | ECT (+NG+PT) CBT (+NG+PT) NG (+PT+PI) WL | VREDIM Different zones (Room with balance, drawing room, kitchen, dining room, bathroom, office, beach, supermarket etc.). | ECT: 15 (10 VR sessions of 15 min.) CBT: 15 NG: 4–6 PI: NR. | - | STAI, BDI, RSEQ, RAS, DIET, WELSQ, URICA, BSS, BIAQ, CDRS. | ED: ECT was the best intervention for eating control improvement. ECT and CBT were better on improving body satisfaction and body perception. ECT was better than CBT on BI and self-efficacy improvement. Obesity: All intervention groups helped on improving body satisfaction and body perception. ECT was the best intervention for eating control improvement. ECT and CBT were better to improve motivation to change. ECT was better than CBT on BI improvement. ECT was more effective than the others approaches. |
| Perpiñá et al. (2004) [42] | 12 (0/12) AN: 7 (0/7) BN: 5 (0/5) | AN, BN (DSM-IV) | RCCT | SBIT+VR SBIT + Relaxation + VR | 6 situations: Accommodation zone, food area with a virtual balance, room with posters, room with mirrors, a doorframe with strips and a zone to contrast body areas. | SBIT: 8 (3 h, weekly, group) Relaxation: 6 (1 h, weekly) VR: 6 (1 h, weekly). | 6 months, 1 year | BIATQ, SIBID, ASI, BAT, EDI-2, EAT, BSI. | Improvement in all measures. Post-treatment results were maintained at follow-up, and for some measures like appearance-related schemas and ED related components the improvement continued along the follow-up period. General psychopathology improved from pre-treatment to one-year follow-up, and BSI score was always below the pre-treatment level, but it rose between 6 and 12 months. VR was useful in the treatment of BI and capable of enhancing the efficacy of the standard CBT. |
| Marco et al. (2013) [39] | 18 (0/18) | BN, AN, EDNOS (DSM-IV-TR) | RCCT | CBT CBT (BI)+VR | 5 situations: Virtual scale and kitchen, room with posters, room with mirrors, a doorframe with strips and a zone to contrast body areas. | CBT for BN:19 (Group, 2 h, weekly) CBTC for AN:23 (individual) CBT: 15 (group) + VR: 8 (1 h, weekly). | 1 year | BAT, BIATQ, BASS, SIBID, BITE, EAT. | CBT+VR showed more BI improvement than CBT; CBT+VR showed more body attitudes and frequency of negative automatic thoughts on BI improvement at post-treatment and this continued to rise at follow-up; more body satisfaction, discomfort caused by body-related situations and BN symptoms (BITE) improvement at post-treatment and follow-up; greater improvement in the behavior clinical measures. All participants improved in the ED measures and it was maintained at follow-up. CBT+VR post-treatment and follow-up showed clinically significant improvement and all BI and ED scores were similar to healthy population. CBT+VR also showed EAT better scores than healthy population. BITE normalization was achieved at follow-up. CBT focused on BI plus VR improved CBT standard treatment for ED. |
| Cesa et al. (2013) [40] | 66 (0/66) | Obesity + BED (DSM-IV-TR) | RCCT | ECT (+IP) CBT (+IP) IP | Neuro-VR 14 environments (Home, Supermarket, Pub, Restaurant, Swimming Pool, Beach, Gymnasium, BI comparison areas). | ECT: 15 (5 weeks, 10 biweekly VR sessions) CBT:15 (5 weeks) IP (6 weeks). | 1 year | EDI-Symptom Checklist, BSS, BIAQ, CDRS. | Weight decreased, number of binge eating episodes decreased to zero, body satisfaction improved in all groups. BI concerns improved only in ECT. ECT and CBT were more effective than IP alone in preventing weight regain at follow-up. Only ECT was effective in further weight loss. Binge eating episodes were reported at follow-up, ECT and CBT were successful in maintaining them at a low rate. |
| Roncero and Perpiñá (2015) [41] | 1 (0/1) | BN (DSM-IV-TR) | CR | CBT+VR | Kitchen with two areas that included elements to cook, drink and eat. | CBT:7 VR:7 (60 min/weekly or biweekly). | - | EDI-2, BITE, ACTA, BDI-2, BAI. | Reduction in binges, purges and food avoidance; development of the ability to make decisions over impulses. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Carvalho, M.R.; Dias, T.R.d.S.; Duchesne, M.; Nardi, A.E.; Appolinario, J.C. Virtual Reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and Binge Eating Disorder: A Systematic Review. Behav. Sci. 2017, 7, 43. https://doi.org/10.3390/bs7030043
De Carvalho MR, Dias TRdS, Duchesne M, Nardi AE, Appolinario JC. Virtual Reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and Binge Eating Disorder: A Systematic Review. Behavioral Sciences. 2017; 7(3):43. https://doi.org/10.3390/bs7030043
Chicago/Turabian StyleDe Carvalho, Marcele Regine, Thiago Rodrigues de Santana Dias, Monica Duchesne, Antonio Egidio Nardi, and Jose Carlos Appolinario. 2017. "Virtual Reality as a Promising Strategy in the Assessment and Treatment of Bulimia Nervosa and Binge Eating Disorder: A Systematic Review" Behavioral Sciences 7, no. 3: 43. https://doi.org/10.3390/bs7030043





