Relationship between Self-Rated Health and Lifestyle and Food Habits in Japanese High School Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Data Collection
2.2. SRH Status
2.3. Statistical Analyses
2.4. Ethics Statement
3. Results
3.1. Sample Characteristics and Item-Specific Responses
3.2. Relationships between SRH and Student’s Food Habits/Attitude
3.3. Multiple Logistic Regression Analysis
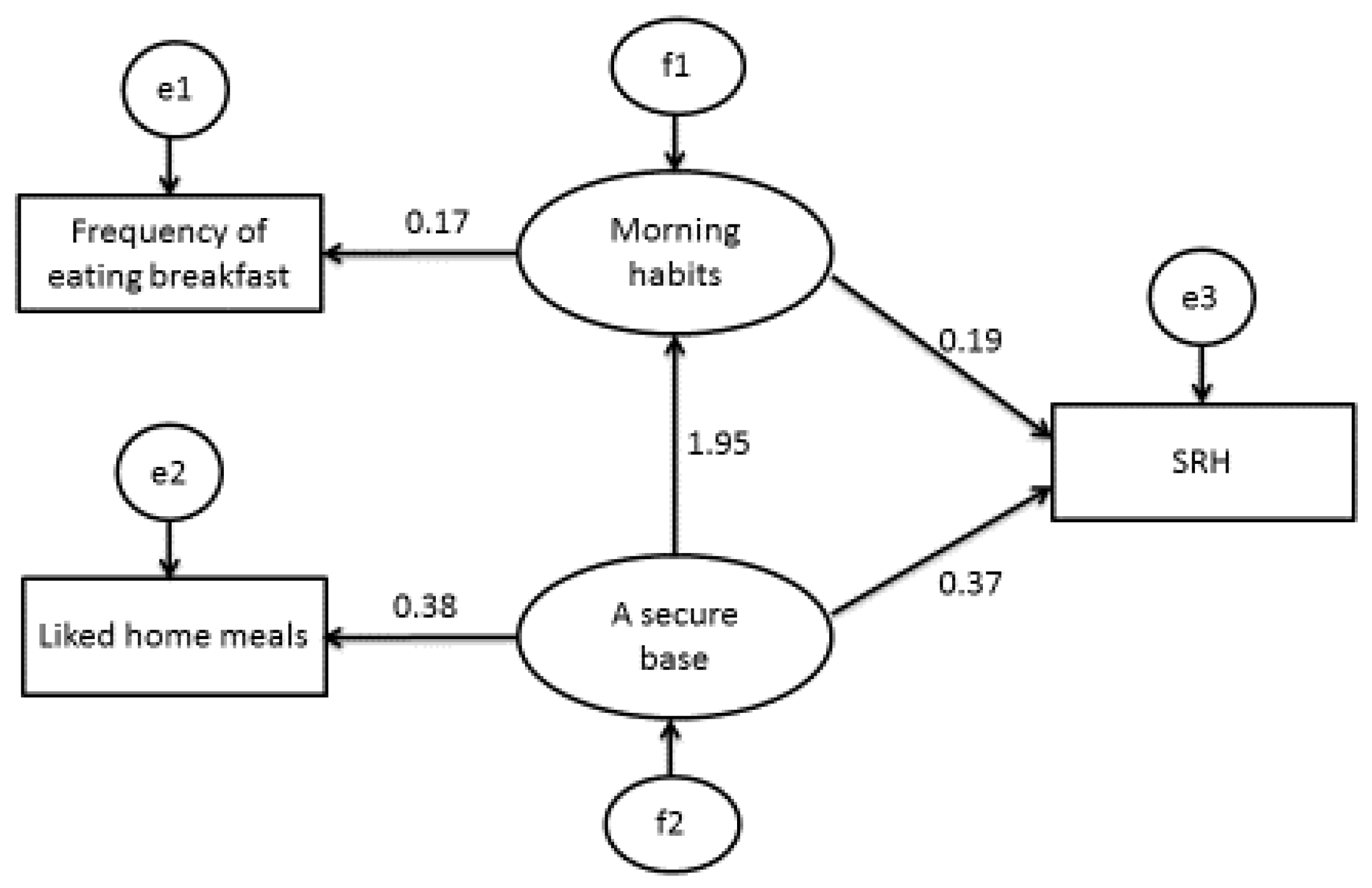
3.4. Structural Equation Modelling
4. Discussion
Study Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| SRH | Self-related health |
| CMIN | Column Minima |
| CMIN/DF | Column Minima Degrees of Freedom |
| GFI | Goodness of fit index |
| AGFI | Adjusted goodness of fit index |
| NFI Deltal | Normed Fit Index Deltal |
| CFI | Comparative fit index |
| RMSEA | Root-mean square error of approximation |
| AIC | Akaike’s Information Criterion |
| CAIC | Consistent Akaike’s Information Criterion |
| SD | Standard deviation |
| N.S. | Not significant |
References
- Finch, B.K.; Hummer, R.A.; Reindl, M.; Vega, W.A. Validity of self-rated health among latino(a)s. Am. J. Epidemiol. 2002, 155, 755–759. [Google Scholar] [CrossRef] [PubMed]
- Robinson-Cohen, C.; Hall, Y.N.; Katz, R.; Rivara, M.B.; Boer, I.H.; Kestenbaum, B.R.; Himmelfarb, J. Self-rated health and adverse events in CKD. Clin. J. Am. Soc. Nephrol. 2014, 9, 2044–2051. [Google Scholar] [CrossRef] [PubMed]
- McClave, A.K.; Dube, S.R.; Strine, T.W.; Mkdad, A.H. Associations between health-rated quality of life and smoking status among a large sample of U.S. adults. Prev. Med. 2009, 48, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Yamada, C.; Moriyama, K.; Takahashi, E. Self-rated health as a comprehensive indicator of lifestyle-related health status. Enviorn. Health Prev. Med. 2012, 17, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Zajacova, A.; Dowd, J.B. Reliability of Self-rated health in US Adults. Am. J. Epidemiol. 2011, 174, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Ethnic groups differ in how poor self-rated mental health reflects psychiatric disorders. J. Racial Ethn. Health Disparit. 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- Lankarani, M.M.; Assari, A. Demographic and socioeconomic determinants of physical and mental self-rated health across 10 ethnic groups in the United States. Int. J. Epidemiol. Res. 2017, 4, 185–193. [Google Scholar] [CrossRef]
- Assari, S.; Lankarini, M.M.; Burgard, S. Black white difference in long term predictive power of self-rated health on all-cause mortality in United States. Ann. Epidemiol. 2017, 26, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Cross-country variation in additive effects of socio-economics, health behaviors, and comorbidities on subjective health of patients with diabetes. J. Diabetes Metab. Disord. 2014, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, D.; Hansell, S. Adolescent competence, psychological well-being, and self-assessed physical health. J. Health Soc. Behav. 1987, 28, 364–374. [Google Scholar] [CrossRef] [PubMed]
- Vingilis, E.; Waed, T.; Seeley, J. Predictors of adolescent self-rated health. Analysis of the National Population Health Survey. Can. J. Public Health 2002, 93, 193–197. [Google Scholar] [PubMed]
- Vingilis, E.; Wade, T.; Seeley, J. Predictors of adolescent health care utilization. J. Adolesc. 2007, 30, 773–800. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Nam, E.W.; Kim, D.; Yoon, Y.M.; Kim, Y.; Kim, H.Y. Role of gender, family, lifestyle and psychological factors in salf-rated health among urban adolescents in Peru: A school-based cross-sectional survey. BMJ Open 2016, e010149. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the social determinants of health. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Boardman, J.D. Self-rated health among US adolescents. J. Adolesc. Health 2006, 38, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Breidablik, H.J.; Meland, E.; Lydersen, S. Self-rated health in adolescence: A multifactorial composite. Scand. J. Public Health 2008, 36, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Piko, B.F. Self-perceived health among adolescents: The role of gender and psychosocial factors. Eur. J. Pediatr. 2007, 166, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Sharif, M.Z.; Rizzo, S.; Marino, E.; Belin, T.R.; Glik, D.C.; Kuo, A.A.; Ortega, A.N.; Prelip, M.L. The association between self-rated eating habits and dietary behaviour in two neighborhoods: Findings from Proyecto Mercado FRESCO. Prev. Med. Rep. 2016, 3, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Joffer, J.; Jerden, L.; Ohman, A.; Flacking, R. Exploring self-rated health among adolescents: A think-aloud study. BMC Public Health. 2016, 16, 156. [Google Scholar] [CrossRef] [PubMed]
- Warnoff, C.; Lekander, M.; Hemmingsson, T.; Sorjonen, K.; Melin, B.; Andreasson, A. Is poor self-rated health associated with low-grade inflammation in 43110 late adolescent men of the general population? A cross-sectional study. BMJ Open 2016, 6, e009440. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. BMC Public Health 2013, 13, 320. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.; Lindstrom, M.; Rosvall, M. Age at smoking initiation and self-rated health among second grade high school boys and girls in Scania, Sweden, a cross sectional study. BMC Public Health 2015, 15, 1143. [Google Scholar] [CrossRef] [PubMed]
- Siega-Riz, A.M.; Popkin, B.M.; Carson, T. Trends in breakfast consumption for children in the United States from 1965 to 1991. Am. J. Clin. Nutr. 1998, 67, 748S–756S. [Google Scholar] [PubMed]
- Sjoberg, A.; Hallberg, L.; Hoglund, D.; Hulthen, L. Meal paggern, food choice, nutrient intake and lifestyle factors in the Goteborg adolescence study. Eur. J. Clin. Nutr. 2003, 57, 1569–1578. [Google Scholar] [CrossRef] [PubMed]
- Ruxton, C.H.S.; Kirk, T.R. Breakfast: A review of associations with measures of dietary intake, physiology and biochemistry. Br. J. Nutr. 1997, 78, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Alexander, K.E.; Ventura, E.E.; Spruijt-Metz, D.; Weigensberg, M.J.; Goran, M.I.; Davis, J.N. Association of breakfast skipping with visceral fat and insulin indices in overweight Latino youth. Obesity 2009, 17, 1528–1533. [Google Scholar] [CrossRef] [PubMed]
- Boutelle, K.; Neumark-Sztainer, D.; Story, M. Weight control behaviors among obese, overweight, and nonoverweight adolescents. J. Pediatr. Psychol. 2002, 27, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Osera, T.; Tsutie, S.; Kobayashi, M.; Kurihara, N. Associations between children’s food preferences and food habits towards healthy eating in Japanese children. J. Child Adolesc. Behav. 2016, 4, 1000292. [Google Scholar] [CrossRef]
- Fayet-Moore, F.; Kim, J.; Sritharan, N.; Petocz, P. Impact of breakfast skipping and breakfast choice on the nutrient intake and body mass index of Australian children. Nutrients 2016, 8, 487. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.W.; Larson, N.I.; Nelson, M.C.; Story, M.; Neumark-Sztainer, D. Fast food intake among adolescents: secular and longitudinal trends from 1999 to 2004. Prev. Med. 2009, 3, 284–287. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.; Siega-Riz, A.; Popkin, B. Trends in energy intake in U.S. between 1977 and 1996: similar shifts seen across age groups. Obes. Res. 2002, 10, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.W.; Lovato, C.Y.; Barr, S.; Hanning, R.M.; Masse, L.C. Experiences of overweight/obese adolescents in navigating their home food environment. Public Health Nutr. 2015, 18, 3278–3286. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Song, W.O.; Cho, M.S. Dietary quality differs by consumption of meals prepared at home vs. outside in Korean adults. Nutr. Res. Pract. 2016, 10, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Roustit, C.; Campoy, E.; Renahy, E.; King, G.; Parizot, I.; Chauvin, P. Family social environment in childhood and self-rated health in young adulthood. BMC Public Health 2011, 11, 949. [Google Scholar] [CrossRef] [PubMed]
- McCurdy, K.; Kisler, T.; Gorman, K.S.; Metallinos-Katsaras, E. Food and health-related correlates of self-reported body mass index among low-income mothers of young children. J. Nutr. Educ. Behav. 2015, 47, 225–233. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, A.; Crawford, D.; Worsley, A. Associations between parental concern for adolescent weight and the home food environment and dietary intake. J. Nutr. Educ. Behav. 2010, 42, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Osera, T.; Tsutie, S.; Kobayashi, M.; Kurihara, N. Relationship of mothers’ food preferences and attitudes with children’s preferences. Food Nutr. Sci. 2012, 3, 1461–1466. [Google Scholar] [CrossRef]
- Osera, T.; Tsutie, S.; Kobayashi, M.; Kurihara, N. A retrospective study on the relationship of changes in likes/dislikes with food habits in 4- and 6-year-old children. Eur. J. Nutr. Food Saf. 2014, 4, 604–613. [Google Scholar] [CrossRef]
- Osera, T.; Tsutie, S.; Kobayashi, M.; Segawa, Y.; Kajiwara, C.; Hashimoto, H.; Kurihara, N. The effect of mothers’ and fathers’ food preferences on children’s preferences with their attitude. Eur. J. Nutr. Food Saf. 2016, 6, 93–100. [Google Scholar] [CrossRef]
- Bowlby, J. A Secure Base: Parent-Child Attachment and Healthy Human Development; Basic Books: New York, NY, USA, 2008. [Google Scholar]
- Bretherton, I. The origins of attachment theory: John Bowlby and Mary Ainsworth. Dev. Psychol. 1992, 28, 759–775. [Google Scholar] [CrossRef]
| Variable | Self-Rated Health | |||||
|---|---|---|---|---|---|---|
| Very Good to Excellent | Good to Poor | p Value | ||||
| All | 1079 | 83.3% | 217 | 16.7% | ||
| Gender | Male | 446 | 81.4% | 102 | 18.6% | N.S * |
| Female | 633 | 84.6% | 115 | 15.4% | N.S * | |
| Grade | Grade 2 | 449 | 41.6% | 97 | 44.7% | N.S * |
| Grade 3 | 630 | 58.4% | 120 | 55.3% | N.S * | |
| Height (m) | 1043 | 162.5 ± 8.5 | 203 | 163.5 ± 8.1 | N.S + | |
| All | Weight (kg) | 971 | 54.8 ± 9.7 | 190 | 55.4 ± 10.6 | N.S + |
| BMI (mg/kg2) | 971 | 20.6 ± 2.8 | 190 | 20.6 ± 3.1 | N.S + | |
| Height (m) | 441 | 169.8 ± 6.2 | 98 | 169.7 ± 5.7 | N.S + | |
| Male | Weight (kg) | 441 | 60.6 ± 9.7 | 96 | 60.6 ± 11.3 | N.S + |
| BMI (mg/kg2) | 439 | 21.0 ± 2.9 | 96 | 21.0 ± 3.5 | N.S + | |
| Height (m) | 602 | 157.0 ± 5.3 | 105 | 157.7 ± 5.3 | N.S + | |
| Female | Weight (kg) | 530 | 50.1 ± 6.7 | 94 | 50.1 ± 6.5 | N.S + |
| BMI (mg/kg2) | 530 | 20.2 ± 2.7 | 94 | 20.1 ± 2.5 | N.S + | |
| Bring Lunch Box | ||||||
| None | 25 | 2.4% | 6 | 2.9% | ||
| 4 times per week or less | 109 | 10.5% | 32 | 15.4% | N.S * | |
| More than 5 times per week | 908 | 87.1% | 169 | 81.6% | ||
| Self-Rated Health | ||||||
|---|---|---|---|---|---|---|
| Very Good to Excellent | Good to Poor | p Value * | ||||
| Sleeping habits | N | % | N | % | ||
| Less 4 h | 22 | 2.0% | 13 | 6% | ||
| Over 4–5 h | 152 | 14.1% | 42 | 19.4% | ||
| Over 5–6 h | 403 | 37.4% | 72 | 33.2% | <0.001 *** | |
| Over 6–7 h | 361 | 33.5% | 70 | 32.3% | ||
| Over 7–8 h | 135 | 12.5% | 14 | 6.5% | ||
| Over 9 h | 5 | 0.5% | 6 | 2.8% | ||
| Frequency of eating breakfast | ||||||
| None | 80 | 7.4% | 40 | 18.4% | ||
| 1–2 times per week | 50 | 4.6% | 10 | 4.6% | <0.001 *** | |
| 3–4 times per week | 60 | 5.6% | 17 | 7.8% | ||
| Over 5 times per week | 886 | 82.3% | 150 | 69.1% | ||
| Frequency of eating breakfast with their family | ||||||
| None | 428 | 40.2% | 117 | 53.9% | ||
| 1–2 times per week | 118 | 11.1% | 15 | 6.9% | <0.01 ** | |
| 3–4 times per week | 94 | 8.8% | 11 | 5.1% | ||
| Over 5 times per week | 426 | 40.0% | 74 | 34.1% | ||
| Frequency of using convenience store | ||||||
| Every day | 43 | 4.0% | 15 | 6.9% | ||
| 3–4 times per week | 87 | 8.1% | 30 | 13.8% | <0.01 ** | |
| 1–2 times per week | 408 | 37.8% | 84 | 38.7% | ||
| None | 540 | 50.1% | 88 | 40.6% | ||
| Respect for food | ||||||
| None | 2 | 0.2% | 1 | 0.5% | ||
| Low respect | 12 | 1.1% | 7 | 3.3% | ||
| Medium respect | 101 | 9.4% | 34 | 15.8% | <0.000 *** | |
| High respect | 357 | 33.2% | 81 | 37.7% | ||
| Higher respect | 602 | 56.1% | 92 | 42.8% | ||
| Concern about food | ||||||
| None | 17 | 1.6% | 6 | 2.8% | ||
| Low Concern | 69 | 6.5% | 28 | 13.2% | ||
| Medium Concern | 204 | 19.1% | 44 | 20.8% | <0.01 ** | |
| High Concern | 364 | 34.1% | 73 | 34.4% | ||
| Higher Concern | 414 | 38.8% | 61 | 28.8% | ||
| Liked home meal | ||||||
| Disliked | 13 | 1.2% | 5 | 2.3% | ||
| Low liking | 55 | 5.1% | 22 | 10.3% | ||
| Medium liking | 193 | 18.0% | 54 | 25.4% | <0.000 *** | |
| Liked a lot | 318 | 29.7% | 62 | 29.1% | ||
| Liked very much | 491 | 45.9% | 70 | 32.9% | ||
| OR | (95% CI) | p Value | |
|---|---|---|---|
| Frequency of eating breakfast | 2.13 | (1.07, 4.24) | 0.031 |
| Liked home meals | 3.12 | (1.27, 7.65) | 0.013 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osera, T.; Awai, M.; Kobayashi, M.; Tsutie, S.; Kurihara, N. Relationship between Self-Rated Health and Lifestyle and Food Habits in Japanese High School Students. Behav. Sci. 2017, 7, 71. https://doi.org/10.3390/bs7040071
Osera T, Awai M, Kobayashi M, Tsutie S, Kurihara N. Relationship between Self-Rated Health and Lifestyle and Food Habits in Japanese High School Students. Behavioral Sciences. 2017; 7(4):71. https://doi.org/10.3390/bs7040071
Chicago/Turabian StyleOsera, Tomoko, Mitsuyo Awai, Misako Kobayashi, Setsuko Tsutie, and Nobutaka Kurihara. 2017. "Relationship between Self-Rated Health and Lifestyle and Food Habits in Japanese High School Students" Behavioral Sciences 7, no. 4: 71. https://doi.org/10.3390/bs7040071




