Efficacy of Web-Based Weight Loss Maintenance Programs: A Randomized Controlled Trial Comparing Standard Features Versus the Addition of Enhanced Personalized Feedback over 12 Months
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
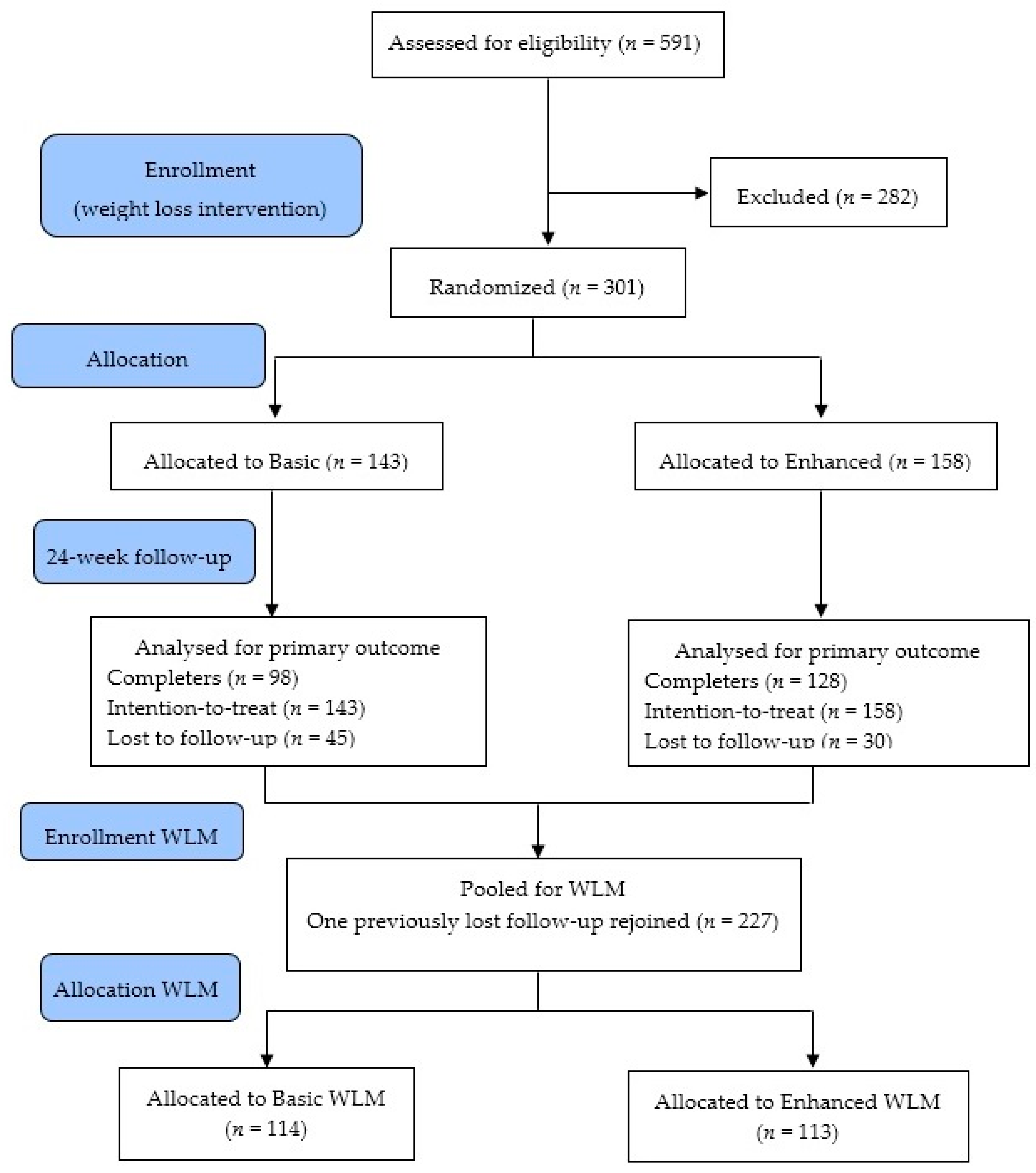
2.2. Study Design
2.3. Measures
2.4. Data Analysis
3. Results
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017. [Google Scholar] [CrossRef]
- Collins, C.E.; Neve, M.J.; Williams, R.; Young, M.; Morgan, P.J.; Fletcher, K.R.C. Effectiveness of interventions with a dietary component on weight loss maintenance: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2013, 11, 317–414. [Google Scholar] [CrossRef]
- Bond, D.S.; Phelan, S.; Leahey, T.M.; Hill, J.O.; Wing, R.R. Weight-loss maintenance in successful weight losers: Surgical vs non-surgical methods. Int. J. Obes. 2009, 33, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Steenkiste, A.; Music, E.; Styn, M.A. A descriptive study of past experiences with weight-loss treatment. J. Am. Diet. Assoc. 2008, 108, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Douketis, J.D.; Macie, C.; Thabane, L.; Williamson, D.F. Systematic review of long-term weight loss studies in obese adults: Clinical significance and applicability to clinical practice. Int. J. Obes. 2005, 29, 1153–1167. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Crerand, C.E.; Brock, J. Behavioral treatment of obesity. Psychiatr. Clin. N. Am. 2005, 28, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Dombrowski, S.; Knittle, K.; Avenell, A.; Araujo-Soares, V.; Sniehotta, F. Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ 2014, 348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Painter, S.L.; Ahmed, R.; Hill, J.O.; Kushner, R.F.; Lindquist, R.; Brunning, S.A.M. What matters in weight loss? An in-depth analysis of self-monitoring. J. Med. Internet Res. 2017, 19, e160. [Google Scholar] [CrossRef] [PubMed]
- Balk-Møller, N.C.; Poulsen, S.K.; Larsen, T.M. Effect of a nine-month web- and app-based workplace intervention to promote healthy lifestyle and weight loss for employees in the social welfare and health care sector: A randomized controlled trial. J. Med. Internet Res. 2017, 19, e108. [Google Scholar] [CrossRef] [PubMed]
- Watson, S.; Woodside, J.V.; Ware, L.J.; Hunter, S.J.; McGrath, A.; Cardwell, C.R.; Appleton, K.M.; Young, I.S.; Mckinlev, M.C. Effect of a web-based behavior change program on weight loss and cardiovascular risk factors in overweight and obese adults at high risk of developing cardiovascular disease: Randomized controlled trial. J. Med. Internet Res. 2015, 17, e177. [Google Scholar] [CrossRef] [PubMed]
- Hageman, P.A.; Pullen, C.H.; Hertzog, M.; Pozehl, B.; Eisenhauer, C.; Boeckner, L.S. Web-based interventions alone or supplemented with peer-led support or professional email counseling for weight loss and weight maintenance in women from rural communities: Results of a clinical trial. J. Obes. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, M.S.; Daley, A.; Jolly, K. Evaluation of a text supported weight maintenance programme ‘lighten up plus’ following a weight reduction programme: Randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Re, F.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B.; et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: A systematic review of systematic reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef] [PubMed]
- Hutchesson, M.J.; Rollo, M.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.J.; Callister, R.; Plotnikoff, R.; Collins, C.E. Ehealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Morgan, P.J.; Neve, M.J.; Callister, R. Efficacy of standard versus enhanced features in a web-based commercial weight-loss program for obese adults, part 2: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e140. [Google Scholar] [CrossRef] [PubMed]
- Gold, B.; Burke, S.; Pintauro, S.; Buzzell, P.; Harvey-Berino, J. Weight loss on the web: A pilot study comparing a structured behavioral intervention to a commercial program. Obesity 2007, 15, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Morgan, P.J.; Jones, P.; Fletcher, K.; Martin, J.; Aguiar, E.J.; Lucas, A.; Neve, M.J.; Callister, R. A 12-week commercial web-based weight-loss program for overweight and obese adults: Randomized controlled trial comparing basic versus enhanced features. J. Med. Internet Res. 2012, 14, e57. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Morgan, P.J.; Jones, P.; Fletcher, K.; Martin, J.; Aguiar, E.J.; Lucas, A.; Neve, M.; McElduff, P.; Callister, R. Evaluation of a commercial web-based weight loss and weight loss maintenance program in overweight and obese adults: A randomised controlled trial. BMC Public Health 2010, 10, 669. [Google Scholar] [CrossRef] [PubMed]
- Bamia, C.; Orfanos, P.; Ferrari, P.; Overvad, K.; Hundborg, H.H.; Tjønneland, A.; Olsen, A.; Kesse, E.; Boutron-Ruault, M.; Clavel-Chapelon, F.; et al. Dietary patterns among older europeans: The epic-elderly study. Br. J. Nutr. 2005, 94, 100–113. [Google Scholar] [CrossRef] [PubMed]
- Neve, M.; Morgan, P.J.; Jones, P.R.; Collins, C.E. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: A systematic review with meta-analysis. Obes. Rev. 2010, 11, 306–321. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Subgroup or Mean (SD) | Treatment Group | p-Value | ||
|---|---|---|---|---|---|
| Basic WLM (n = 114) | Enhanced WLM (n = 113) | All (n = 227) | |||
| Sex | Men | 48 (42%) | 52 (46%) | 100 (44%) | 0.55 |
| Country of birth | Australia | 108 (95%) | 100 (88%) | 208 (92%) | 0.23 |
| Highest level of education | School | 37 (32%) | 28 (25%) | 65 (29%) | 0.49 |
| Trade/Diploma | 41 (36%) | 40 (35%) | 81 (35%) | ||
| University Degree | 24 (21%) | 28 (25%) | 52 (23%) | ||
| Higher University Degree | 12 (11%) | 17 (15%) | 29 (13%) | ||
| Weekly household income (AUS$) | <$700 | 12 (11%) | 7 (6.4%) | 19 (8.8%) | 0.60 |
| $700 to <$1000 | 6 (5.7%) | 5 (4.5%) | 11 (5.1%) | ||
| $1000 to <$1400 | 13 (12%) | 11 (10%) | 24 (11%) | ||
| $1500 or more | 71 (67%) | 84 (76%) | 155 (72%) | ||
| Age (years) | mean (SD) | 43.3 (9.7) | 41.3 (10.3) | 42.3 (10.1) | 0.14 |
| Height (m) | mean (SD) | 1.70 (0.09) | 1.72 (0.09) | 1.71 (0.09) | 0.17 |
| Weight (kg) | mean (SD) | 88.5 (14.5) | 89.3 (15.6) | 88.9 (15.1) | 0.70 |
| Body mass index (kg/m2) | mean (SD) | 30.6 (4.1) | 30.1 (4.1) | 30.4 (4.1) | 0.45 |
| Waist circumference at umbilicus (cm) | mean (SD) | 100.6 (11.1) | 98.5 (11.7) | 99.6 (11.4) | 0.18 |
| Waist circumference at narrowest point (cm) | mean (SD) | 93.2 (11.5) | 92.2 (11.9) | 92.7 (11.7) | 0.52 |
| Waist to height ratio at umbilicus | mean (SD) | 0.59 (0.07) | 0.57 (0.07) | 0.58 (0.07) | 0.04 |
| Waist to height ratio at narrowest point | mean (SD) | 0.55 (0.07) | 0.54 (0.06) | 0.54 (0.06) | 0.15 |
| Weight loss at baseline entry to study (24 weeks) | mean (SD) | −4.38 (5.30) | −4.47 (6.37) | −4.42 (5.84) | 0.91 |
| Systolic blood pressure (mmHg) | mean (SD) | 117.5 (13) | 117.7 (12) | 117.6 (12.5) | 0.92 |
| Diastolic blood pressure (mmHg) | mean (SD) | 77.6 (10.6) | 77.2 (9.2) | 77.4 (9) | 0.76 |
| Resting heart rate (bpm) | mean (SD) | 64.6 (9.5) | 64.7 (10.2) | 64.6 (9.8) | 0.94 |
| Total serum cholesterol (mmol/L) | mean (SD) | 5.2 (1.1) | 4.8(1.0) | 5.0 (1.1) | 0.03 |
| LDL cholesterol (mmol/L) | mean (SD) | 3.1 (1.0) | 2.9 (0.8) | 3.0 (0.9) | 0.08 |
| HDL cholesterol (mmol/L) | mean (SD) | 1.3 (0.3) | 1.3 (0.3) | 1.3 (0.3) | 0.41 |
| Triglycerides (mmol/L) | mean (SD) | 1.5 (1.0) | 1.3 (0.7) | 1.4 (0.9) | 0.16 |
| Glucose (mmol/L) | mean (SD) | 4.6 (0.6) | 4.5 (0.7) | 4.6 (0.7) | 0.08 |
| Insulin (mIU/L) | mean (SD) | 6.6 (5.5) | 6.9 (6.2) | 6.7 (5.9) | 0.73 |
| Characteristic | Treatment Group Mean Change (SD) | Absolute Difference between Groups LSM (95% CI) | p Values for Group Effect | |
|---|---|---|---|---|
| Basic | Enhanced | Enhanced vs. Basic | Difference at Specified Time | |
| Weight (kg) | 1.3 (5.1) | 1.5 (4.4) | 0.15 (−1.09, 1.39) | 0.81 |
| Systolic blood pressure (mmHg) | 1.1 (12.1) | 1.1 (10.2) | 0.24 (−2.59, 3.08) | 0.87 |
| Diastolic blood pressure (mmHg) | −1.5 (8.1) | −0.1 (6.5) | 1.15 (−0.76, 3.06) | 0.24 |
| Body mass index (kg/m2) | 0.5 (1.9) | 0.5 (1.6) | 0.02 (−0.46, 0.50) | 0.93 |
| Pulse rate (bpm) | −0.3 (6.7) | 0.5 (5.8) | 0.74 (−0.88, 2.35) | 0.37 |
| Waist circumference at umbilicus (cm) | 3.8 (5.4) | 3.3 (4.9) | 0.76 (−0.63, 2.16) | 0.28 |
| Waist circumference at narrowest point (cm) | 2.6 (4.6) | 2.6 (4.6) | 0.11 (−1.12, 1.35) | 0.86 |
| Waist to height ratio at umbilicus | 0.0 (0.0) | 0.0 (0.0) | 0.01 (−0.00, 0.01) | 0.21 |
| Waist to height ratio at narrowest point | 0.0 (0.0) | 0.0 (0.0) | 0.00 (−0.01, 0.01) | 0.80 |
| Total serum cholesterol (mmol/L) | 0.1 (0.8) | 0.2 (0.7) | 0.07 (−0.12, 0.26) | 0.50 |
| LDL cholesterol (mmol/L) | 0.0 (0.6) | 0.1 (0.5) | 0.01 (−0.15, 0.16) | 0.94 |
| HDL cholesterol (mmol/L) | 0.0 (0.2) | 0.0 (0.2) | 0.00 (−0.06, 0.06) | 0.88 |
| Triglycerides (mmol/L) | 0.0 (0.5) | 0.2 (0.5) | 0.13 (−0.02, 0.27) | 0.10 |
| Glucose (mmol/L) | 0.1 (0.5) | 0.2 (0.5) | 0.08 (−0.05, 0.22) | 0.20 |
| Insulin (mIU/L) | 1.6 (4.2) | 0.89 (6.5) | 0.61 (−0.719, 2.01) | 0.39 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collins, C.E.; Morgan, P.J.; Hutchesson, M.J.; Oldmeadow, C.; Barker, D.; Callister, R. Efficacy of Web-Based Weight Loss Maintenance Programs: A Randomized Controlled Trial Comparing Standard Features Versus the Addition of Enhanced Personalized Feedback over 12 Months. Behav. Sci. 2017, 7, 76. https://doi.org/10.3390/bs7040076
Collins CE, Morgan PJ, Hutchesson MJ, Oldmeadow C, Barker D, Callister R. Efficacy of Web-Based Weight Loss Maintenance Programs: A Randomized Controlled Trial Comparing Standard Features Versus the Addition of Enhanced Personalized Feedback over 12 Months. Behavioral Sciences. 2017; 7(4):76. https://doi.org/10.3390/bs7040076
Chicago/Turabian StyleCollins, Clare E., Philip J. Morgan, Melinda J. Hutchesson, Christopher Oldmeadow, Daniel Barker, and Robin Callister. 2017. "Efficacy of Web-Based Weight Loss Maintenance Programs: A Randomized Controlled Trial Comparing Standard Features Versus the Addition of Enhanced Personalized Feedback over 12 Months" Behavioral Sciences 7, no. 4: 76. https://doi.org/10.3390/bs7040076






