Performance of the Adult ADHD Self-Report Scale-v1.1 in Adults with Major Depressive Disorder
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Participants
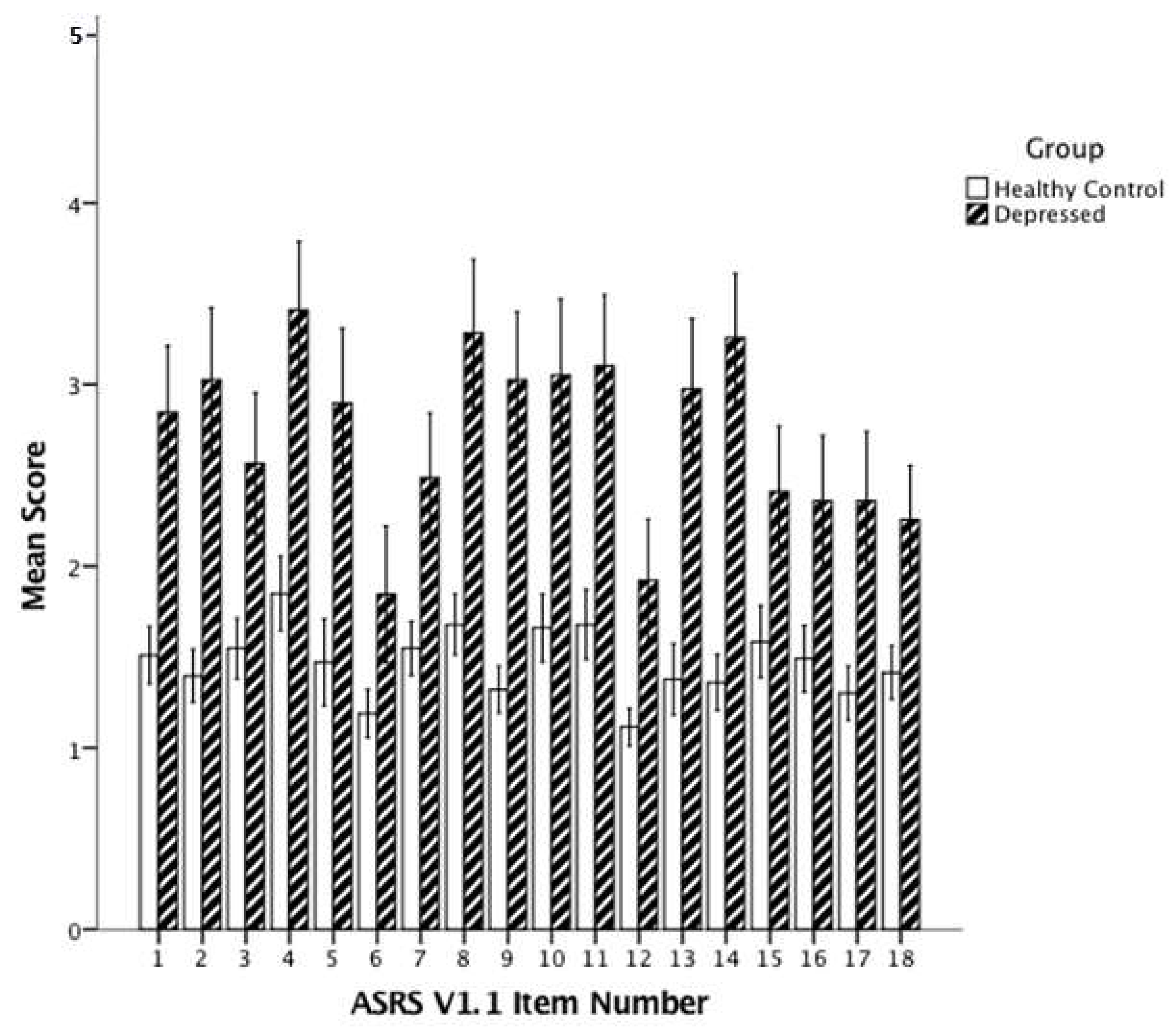
3.2. ASRS-v1.1 Descriptive Results
3.3. ADHD Symptoms and Diagnosis by MINI
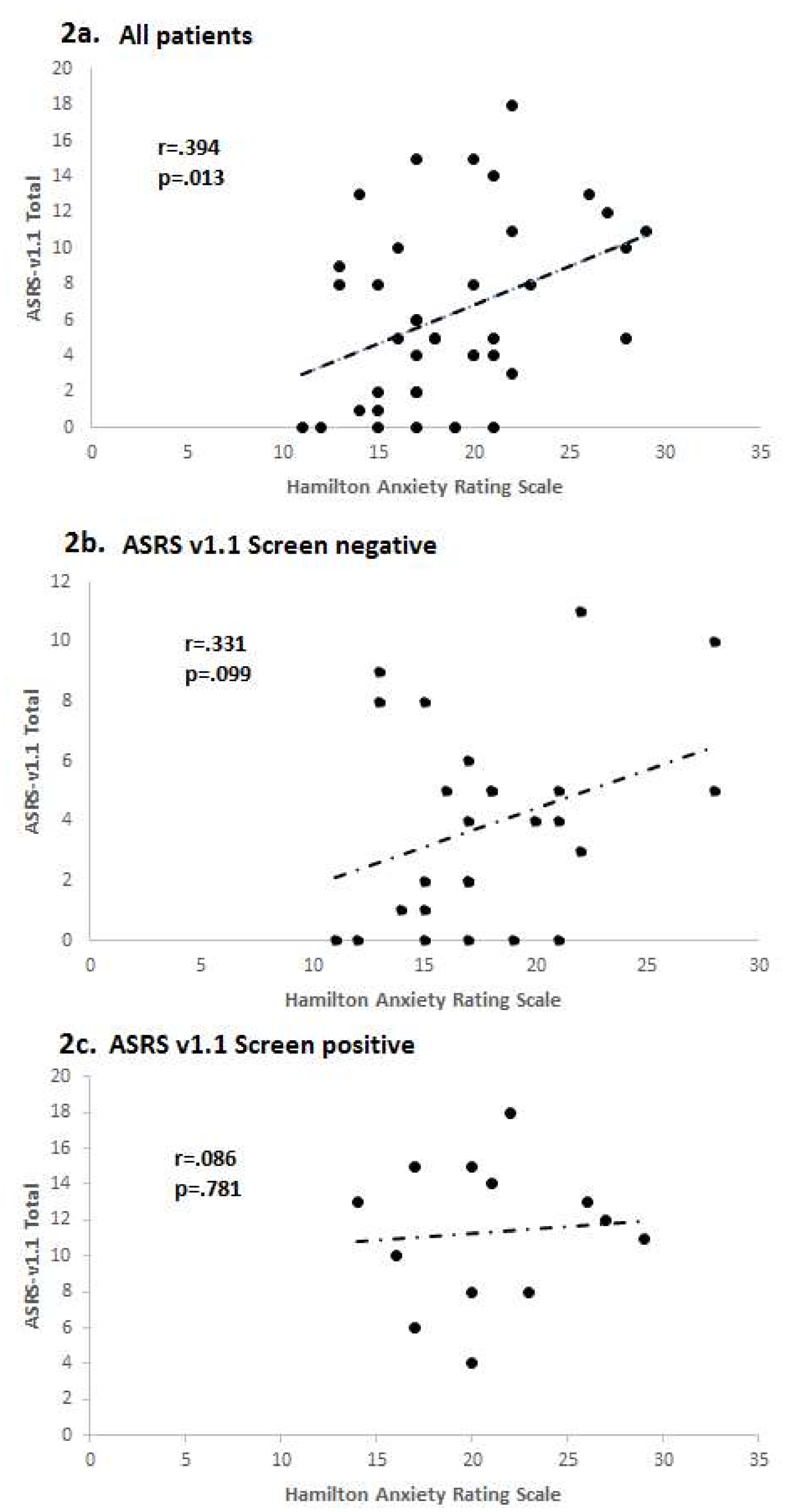
3.4. Utility of ASRS-v1.1 in Depressed Patients
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Hechtman, L.; Swanson, J.M.; Sibley, M.H.; Stehli, A.; Owens, E.B.; Mitchell, J.T.; Arnold, L.E.; Molina, B.S.; Hinshaw, S.P.; Jensen, P.S.; et al. MTA Cooperative Group. Functional adult outcomes 16 Years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. J. Am. Acad. Child. Adolesc. Psychiatry 2016, 55, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Fayyad, J.; De Graaf, R.; Kessler, R.; Alonso, J.; Angermeyer, M.; Demyttenaere, K.; De Girolamo, G.; Haro, J.M.; Karam, E.G.; Lara, C.; et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br. J. Psychiatry 2007, 190, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Adler, L.; Barkley, R.; Biederman, J.; Conners, C.K.; Demler, O.; Faraone, S.V.; Greenhill, L.L.; Howes, M.J.; Secnik, K.; et al. The prevalence and correlates of adult AHD in the United States: Results from the National Comorbidity Survey Replication. Am. J. Psychiatry 2006, 163, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Matza, L.S.; Paramore, C.; Prasad, M. A review of the economic burden of ADHD. Cost Eff. Resour. Alloc. 2005, 3, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fletcher, J.; Wolfe, B. Long-term consequences of childhood ADHD on criminal activities. J. Ment. Health Policy Econ. 2009, 12, 119–138. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, T.E.; Houts, R.; Asherson, P.; Belsky, D.W.; Corcoran, D.L.; Hammerle, M.; Harrington, H.; Hogan, S.; Meier, M.H.; Polanczyk, G.V.; et al. Is adult ADHD a childhood-onset neurodevelopmental disorder? evidence from a four-decade longitudinal cohort study. Am. J. Psychiatry 2015, 172, 967–977. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Gao, K.; Wang, Z.; Chen, J.; Kemp, D.E.; Chan, P.K.; Conroy, C.M.; Serrano, M.B.; Ganocy, S.J.; Calabrese, J.R. Should an assessment of Axis I comorbidity be included in the initial diagnostic assessment of mood disorders? Role of QIDS-16-SR total score in predicting number of Axis I comorbidity. J. Affect. Disord. 2013, 148, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J. Impact of comorbidity in adults with attention-deficit/hyperactivity disorder. J. Clin. Psychiatry 2004, 65 (Suppl. 3), 3–7. [Google Scholar] [PubMed]
- Biederman, J.; Petty, C.R.; Fried, R.; Kaiser, R.; Dolan, C.R.; Schoenfeld, S.; Doyle, A.E.; Seidman, L.J.; Faraone, S.V. Educational and occupational underattainment in adults with attention-deficit/hyperactivity disorder: A controlled study. J. Clin. Psychiatry 2008, 69, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- Ljung, T.; Chen, Q.; Lichtenstein, P.; Larsson, H. Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior: A population-based study in Sweden. JAMA Psychiatry 2014, 71, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Alpert, J.E.; Maddocks, A.; Nierenberg, A.A.; O’Sullivan, R.; Pava, J.A.; Worthington, J.J., III; Biederman, J.; Rosenbaum, J.F.; Fava, M. Attention deficit hyperactivity disorder in childhood among adults with major depression. Psychiatry Res. 1996, 62, 213–219. [Google Scholar] [CrossRef]
- Diler, R.S.; Daviss, W.B.; Lopez, A.; Axelson, D.; Iyengar, S.; Birmaher, B. Differentiating major depressive disorder in youths with attention deficit hyperactivity disorder. J. Affect. Disord. 2007, 102, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.R.; Adler, L.A. Assessing attention-deficit/hyperactivity disorder in adults: Focus on rating scales. J. Clin. Psychiatry 2004, 65 (Suppl. 3), 12–17. [Google Scholar] [PubMed]
- Surman, C.B.H. Clinical assessment of ADHD in adults. In ADHD in Adults: A Practical Guide to Evaluation and Management; Humana Press: New York, NY, USA, 2013. [Google Scholar]
- Kessler, R.C.; Adler, L.; Ames, M.; Demler, O.; Faraone, S.; Hiripi, E.; Howes, M.J.; Jin, R.; Secnik, K.; Spencer, T.; et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychol. Med. 2005, 35, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Reyes, M.M.; Schneekloth, T.D.; Hitschfeld, M.J.; Geske, J.R.; Atkinson, D.L.; Karpyak, V.M. The clinical utility of ASRS-v1.1 for identifying ADHD in alcoholics using PRISM as the reference standard. J. Atten. Disord. 2016. [Google Scholar] [CrossRef] [PubMed]
- Perroud, N.; Cordera, P.; Zimmermann, J.; Michalopoulos, G.; Bancila, V.; Prada, P.; Dayer, A.; Aubry, J.M. Comorbidity between attention deficit hyperactivity disorder (ADHD) and bipolar disorder in a specialized mood disorders outpatient clinic. J. Affect. Disord. 2014, 168, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Dalsgaard, S.; Kvist, A.P.; Leckman, J.F.; Nielsen, H.S.; Simonsen, M. Cardiovascular safety of stimulants in children with attention-deficit/hyperactivity disorder: A nationwide prospective cohort study. J. Child Adolesc. Psychopharmacol. 2014, 24, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Alexander, L.; Oliver, A.; Burdine, L.K.; Tang, Y.; Dunlop, B.W. Reported maladaptive decision-making styles in unipolar and bipolar depression and their change with treatment. Psychiatry Res. 2017, 257, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0); Biometrics Research Department, New York State Psychiatric Institute: New York, NY, USA, 1995. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33. [Google Scholar] [PubMed]
- Guy, W. Clinical Global Impressions. Publication ADM 76-338. ECDEU Assessment Manual for Psychopharmacology; US Department of Health, Education, and Welfare: Rockville, MD, USA, 1976; pp. 217–222.
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Treynor, W.; Gonzalez, R.; Nolen-Hoeksema, S. Rumination reconsidered: A psychometric analysis. Cog. Ther. Res. 2003, 27, 247–259. [Google Scholar] [CrossRef]
- Bernstein, D.P.; Fink, L. Childhood Trauma Questionnaire Manual; Psychological Corporation: San Antonio, TX, USA, 1998. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Kessler, R.C.; Adler, L.; Gruber, M.J.; Sarawate, C.A.; Spencer, T.; Van Brunt, D.L. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int. J. Met. Psychiatr. Res. 2007, 16, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Hines, J.L.; King, T.S.; Curry, W.J. The adult ADHD self-report scale for screening for adult attention deficit-hyperactivity disorder (ADHD). J. Am. Board Fam. Med. 2012, 25, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Sibley, M.H.; Rohde, L.A.; Swanson, J.M.; Hechtman, L.T.; Molina, B.S.G.; Mitchell, J.T.; Arnold, L.E.; Caye, A.; Kennedy, T.M.; Roy, A.; et al. Late-Onset ADHD reconsidered with comprehensive repeated assessments between ages 10 and 25. Am. J. Psychiatry 2018, 175, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Quinn, C.R.; Harris, A.; Felmingham, K.; Boyce, P.; Kemp, A. The impact of depression heterogeneity on cognitive control in major depressive disorder. Aust. N. Z. J. Psychiatry 2012, 46, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Christoff, K.; Irving, Z.C.; Fox, K.C.; Spreng, R.N.; Andrews-Hanna, J.R. Mind-wandering as spontaneous thought: A dynamic framework. Nat. Rev. Neurosci. 2016, 17, 718–731. [Google Scholar] [CrossRef] [PubMed]
- Joormann, J.; Gotlib, I.H. Emotion regulation in depression: Relation to cognitive inhibition. Cogn. Emot. 2010, 24, 281–298. [Google Scholar] [CrossRef] [PubMed]
- Whitmer, A.J.; Gotlib, I.H. An attentional scope model of rumination. Psychol. Bull. 2013, 139, 1036–1061. [Google Scholar] [CrossRef] [PubMed]
- Watkins, E.; Brown, R.G. Rumination and executive function in depression: An experimental study. J. Neurol. Neurosurg. Psychiatry 2002, 72, 400–402. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.P.; Siegle, G.J.; Muelly, E.R.; Haggerty, A.; Ghinassi, F. Poor performance on cognitive tasks in depression: Doing too much or not enough? Cogn. Affect. Behav. Neurosci. 2010, 10, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Agnew-Blais, J.C.; Polanczyk, G.V.; Danese, A.; Wertz, J.; Moffitt, T.E.; Arseneault, L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry 2016, 73, 713–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caye, A.; Rocha, T.B.-M.; Anselmi, L.; Murray, J.; Menezes, A.M.; Barros, F.C.; Gonçalves, H.; Wehrmeister, F.; Jensen, C.M.; Steinhausen, H.C.; et al. Attention-deficit/hyperactivity disorder trajectories from childhood to young adulthood: Evidence from a birth cohort supporting a late-onset syndrome. JAMA Psychiatry 2016, 73, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Biederman, J. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry 2016, 73, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Lecendreux, M.; Konofal, E.; Cortese, S.; Faraone, S.V. A 4-year follow-up of attention-deficit/hyperactivity disorder in a population sample. J. Clin. Psychiatry 2015, 76, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.; Micoulaud-Franchi, J.A.; Galera, C.; Dauvilliers, Y. Is adult-onset attention deficit/hyperactivity disorder frequent in clinical practice? Psychiatry Res. 2017, 257, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Sibley, M.H.; Mitchell, J.T.; Becker, S.P. Method of adult diagnosis influences estimated persistence of childhood ADHD: A systematic review of longitudinal studies. Lancet Psychiatry 2016, 3, 1157–1165. [Google Scholar] [CrossRef]
- Ustun, B.; Adler, L.A.; Rudin, C.; Faraone, S.V.; Spencer, T.J.; Berglund, P.; Gruber, M.J.; Kessler, R.C. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry 2017, 74, 520–526. [Google Scholar] [CrossRef] [PubMed]
| Item No. | Item Description | Number Endorsing | % |
|---|---|---|---|
| 1 | Trouble wrapping up final details of a project | 25 | 62.5 |
| 9 | Difficulty concentrating on what people say to you, even when speaking to you directly. | 25 | 62.5 |
| 2 | Difficulty getting things in order for a task requiring organization | 24 | 60.0 |
| 4 | Avoiding getting started on a task requiring a lot of thought | 19 | 47.5 |
| 3 | Problems remembering appointments or obligations | 18 | 45.0 |
| 8 | Difficulty keeping your attention when doing boring or repetitive work | 17 | 42.5 |
| 16 | Finishing sentences of people you are talking to before they can finish them themselves | 17 | 42.5 |
| 10 | Misplacing or having difficulty finding things at home or work | 15 | 37.5 |
| 14 | Difficulty unwinding and relaxing when you have time to yourself | 15 | 37.5 |
| 5 | Fidget or squirm with your hands or feet when you have to sit down for a long time | 13 | 32.5 |
| 18 | Interrupting others when they are busy | 13 | 32.5 |
| 11 | Distracted by activity or noise around you | 12 | 30.0 |
| 13 | Feel restless or fidgety | 12 | 30.0 |
| 12 | Leave your seat in meetings or situations in which you are expected to remain still | 8 | 20.0 |
| 7 | Make careless mistakes when you have to work on a boring or difficulty project | 7 | 17.5 |
| 15 | Find yourself talking too much when you are in social situations | 7 | 17.5 |
| 17 | Difficulty waiting your turn in situations when turn taking is required | 6 | 15.0 |
| 6 | Feel overly active and compelled to do things, like you were driven by a motor | 4 | 10.0 |
| MINI ADHD Inattentive Symptom Count Criterion Negative (n = 20) | MINI ADHD Inattentive Symptom Count Criterion Positive (n = 20) | |||||
|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | t | p |
| Age (years) | 49.4 | 8.4 | 49.7 | 7.9 | 0.14 | 0.89 |
| Age at first episode (years) | 27.1 | 15.5 | 33.3 | 16.0 | 1.19 | 0.24 |
| Number of episodes | 2.3 | 1.2 | 2.3 | 1.3 | 0.13 | 0.90 |
| HDRS | 20.1 | 3.2 | 21.3 | 3.9 | 1.03 | 0.31 |
| CGI-S | 4.2 | 0.6 | 4.3 | 0.6 | 0.53 | 0.60 |
| HAMA | 18.1 | 4.2 | 19.6 | 4.9 | 1.02 | 0.32 |
| HAMA Item 5 (Concentration) | 1.9 | 0.8 | 2.5 | 0.5 | 3.03 | 0.004 |
| CTQ Total | 66.9 | 17.7 | 67.2 | 12.2 | 0.05 | 0.96 |
| RRS | 56.0 | 10.0 | 60.1 | 10.3 | 1.13 | 0.227 |
| ASRS-v1.1 Part A | 1.9 | 1.5 | 3.3 | 1.8 | 2.79 | 0.008 |
| ASRS-v1.1 Part B | 2.2 | 2.2 | 5.6 | 3.7 | 3.54 | 0.001 |
| ASRS-v1.1 Total | 4.0 | 3.2 | 8.9 | 5.3 | 3.50 | 0.001 |
| N | % | N | % | χ2 | p | |
| Sex | 0.13 | 0.72 | ||||
| Male | 6 | 30 | 5 | 25 | ||
| Female | 14 | 70 | 15 | 75 | ||
| Race * | 4.58 | 0.10 | ||||
| White | 12 | 67 | 7 | 35 | ||
| Black | 5 | 28 | 8 | 40 | ||
| Other/Multiple | 1 | 6 | 5 | 25 | ||
| Marital Status * | 0.21 | 0.65 | ||||
| Married/Partnered | 7 | 35 | 8 | 42 | ||
| Single | 13 | 65 | 11 | 58 | ||
| Currently Employed | 0.44 | 0.51 | ||||
| Yes | 12 | 60 | 14 | 70 | ||
| No | 8 | 40 | 6 | 30 | ||
| Lifetime Anxiety Disorder | 0.40 | 0.53 | ||||
| Yes | 10 | 50 | 8 | 42 | ||
| No | 10 | 50 | 12 | 58 | ||
| Lifetime Tobacco Use | 1.0 | 1.0 | ||||
| Yes | 10 | 50 | 10 | 50 | ||
| No | 10 | 50 | 10 | 50 | ||
| Lifetime Substance Abuse | 1.76 | 0.19 | ||||
| Yes | 5 | 25 | 9 | 45 | ||
| No | 15 | 75 | 11 | 55 | ||
| History of Stimulant Rx | 0.23 | 0.63 | ||||
| Yes | 3 | 15 | 2 | 10 | ||
| No | 17 | 85 | 2 | 90 | ||
| ASRS-v1.1 Part A Screen Negative (n = 26) | ASRS-v1.1 Part A Screen Positive (n = 14) | |||||
|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | t | p |
| Age (years) | 48.2 | 8.2 | 52.1 | 7.6 | 1.49 | 0.15 |
| Age at first episode (years) | 30.1 | 14.7 | 30.2 | 18.3 | 0.02 | 0.99 |
| Number of episodes | 2.3 | 1.2 | 2.4 | 1.4 | 0.26 | 0.80 |
| HDRS | 20.1 | 3.1 | 21.8 | 4.1 | 1.48 | 0.15 |
| CGI-S | 4.2 | 0.6 | 4.4 | 0.5 | 1.43 | 0.16 |
| HAMA | 17.8 | 4.3 | 20.9 | 4.5 | 2.14 | 0.039 |
| HAMA Item 5 (Concentration) | 2.0 | 0.7 | 2.5 | 0.5 | 2.57 | 0.014 |
| CTQ Total | 64.5 | 12.6 | 71.8 | 18.0 | 1.43 | 0.16 |
| RRS | 55.6 | 9.4 | 62.8 | 10.6 | 2.10 | 0.042 |
| No. MINI Inattention items | 4.1 | 2.3 | 6.8 | 2.5 | 3.42 | 0.002 |
| No. MINI Hyperactivity items | 1.9 | 1.7 | 3.7 | 2.3 | 2.86 | 0.007 |
| N | % | N | % | χ2 | p | |
| Sex | 0.40 | 0.52 | ||||
| Male | 8 | 31 | 3 | 21 | ||
| Female | 18 | 69 | 11 | 79 | ||
| Race * | 0.13 | 0.94 | ||||
| White | 12 | 46 | 7 | 50 | ||
| Black | 9 | 35 | 4 | 29 | ||
| Other/Multiple | 4 | 15 | 2 | 14 | ||
| Marital Status * | 0.05 | 0.49 | ||||
| Married/Partnered | 9 | 35 | 6 | 46 | ||
| Single/Widowed/Divorced | 17 | 65 | 7 | 54 | ||
| Currently Employed | 0.39 | 0.53 | ||||
| Yes | 16 | 62 | 10 | 71 | ||
| No | 10 | 38 | 4 | 29 | ||
| Lifetime Anxiety Disorder | 0.04 | 0.84 | ||||
| Yes | 12 | 46 | 6 | 43 | ||
| No | 14 | 54 | 8 | 57 | ||
| Lifetime Tobacco Use | 0.44 | 0.51 | ||||
| Yes | 12 | 46 | 8 | 57 | ||
| No | 14 | 54 | 6 | 43 | ||
| Lifetime Substance Abuse | 0.58 | 0.45 | ||||
| Yes | 8 | 31 | 6 | 43 | ||
| No | 18 | 69 | 8 | 57 | ||
| History of Stimulant Rx | 5.09 | 0.043 | ||||
| Yes | 1 | 4 | 4 | 29 | ||
| No | 25 | 96 | 10 | 71 | ||
| Item No. | Item Description | False Positive ASRS-v1.1 Part A (n = 11) | Full Syndrome ADHD (n = 5) |
|---|---|---|---|
| 1 | Trouble wrapping up final details of a project | 100% | 100% |
| 2 | Difficulty getting things in order for a task requiring organization | 100% | 80% |
| 3 | Problems remembering appointments or obligations | 91% | 60% |
| 4 | Avoiding getting started on a task requiring a lot of thought | 100% | 80% |
| 5 | Fidget or squirm with your hands or feet when you have to sit down for a long time | 27% | 60% |
| 6 | Feel overly active and compelled to do things, like you were driven by a motor | 18% | 40% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dunlop, B.W.; Wu, R.; Helms, K. Performance of the Adult ADHD Self-Report Scale-v1.1 in Adults with Major Depressive Disorder. Behav. Sci. 2018, 8, 37. https://doi.org/10.3390/bs8040037
Dunlop BW, Wu R, Helms K. Performance of the Adult ADHD Self-Report Scale-v1.1 in Adults with Major Depressive Disorder. Behavioral Sciences. 2018; 8(4):37. https://doi.org/10.3390/bs8040037
Chicago/Turabian StyleDunlop, Boadie W., Ruizhe Wu, and Kathleen Helms. 2018. "Performance of the Adult ADHD Self-Report Scale-v1.1 in Adults with Major Depressive Disorder" Behavioral Sciences 8, no. 4: 37. https://doi.org/10.3390/bs8040037





