Group vs. Individual Treatment for Acute Insomnia: A Pilot Study Evaluating a “One-Shot” Treatment Strategy
Abstract
:1. Introduction
2. Method
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Analytic Strategy
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
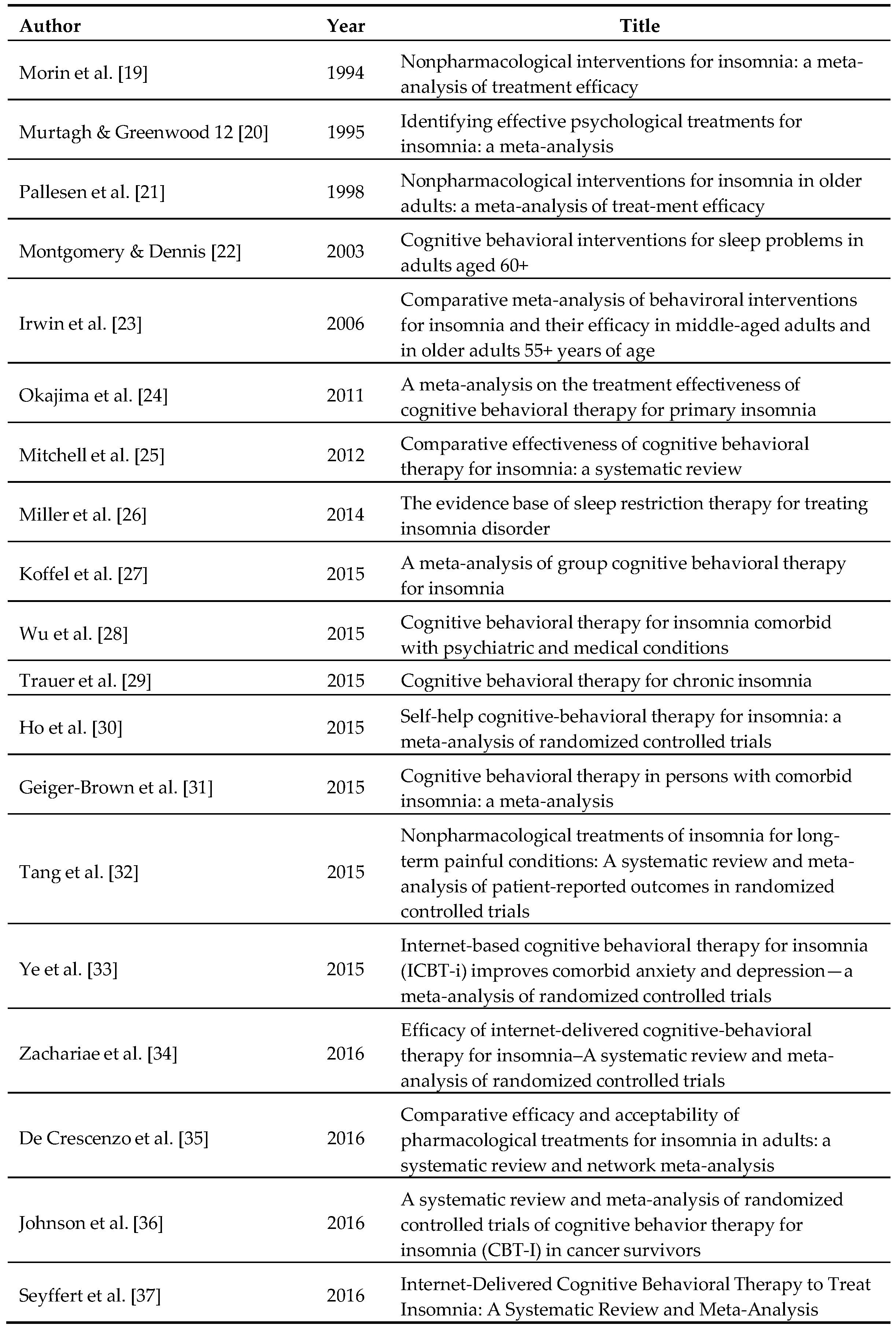
References
- Leblanc, M.; Mérette, C.; Savard, J.; Ivers, H.; Baillargeon, L.; Morin, C.M. Incidence and risk factors of insomnia in a population-based sample. Sleep 2009, 32, 1027–1037. [Google Scholar] [PubMed]
- Ellis, J.G.; Perlis, M.L.; Neale, L.F.; Espie, C.A.; Bastien, C.H. The natural history of insomnia: Focus on prevalence and incidence of acute insomnia. J. Psychiatr. Res. 2012, 46, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Léger, D.; Bayon, V. Societal costs of insomnia. Sleep Med. Rev. 2010, 14, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.K. Clinical and socioeconomic correlates of insomnia. J. Clin. Psychiatry 2004, 65, 13–19. [Google Scholar] [PubMed]
- Daley, M.; Morin, C.M.; LeBlanc, M.; Gregoire, J.P.; Savard, J. The economic burden of insomnia: Direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep 2009, 32, 55–64. [Google Scholar] [PubMed]
- Morin, C.M.; Bélanger, L.; LeBlanc, M.; Ivers, H.; Savard, J.; Espie, C.A.; Mérette, C.; Baillargeon, L.; Grégoire, J.P. The natural history of insomnia: A population-based 3-year longitudinal study. Arch. Intern. 2009, 169, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Angst, J.; Gamma, A.; Ajdacic, V.; Eich, D.; Rossler, W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 2008, 31, 473–480. [Google Scholar] [PubMed]
- Wilson, S.J.; Nutt, D.J.; Alford, C.; Argyropoulos, S.V.; Baldwin, D.S.; Bateson, A.N.; Britton, T.C.; Crowe, C.; Dijk, D.J.; Espie, C.A.; et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J. Psychopharmacol. 2010, 24, 1577–1601. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Kansagara, D.; Forciea, M.A.; Cooke, M.; Denberg, T.D. Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2016, 165, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.T.; Huang, M.I.; Manber, R. Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clin. Psychol. Rev. 2005, 25, 559–592. [Google Scholar] [CrossRef] [PubMed]
- Gotts, Z.; Deary, V.; Newton, J.L.; Ellis, J. Treatment of insomnia reduces fatigue in chronic fatigue syndrome in those able to comply with the intervention. Fatigue Biomed. Health Behav. 2016, 4, 208–216. [Google Scholar] [CrossRef]
- Lamberg, L. Despite effectiveness, behavioral therapy for chronic insomnia still underused. JAMA 2008, 300, 2474–2475. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.C.; Kuo, T.F.; Manber, R. Who is at risk for dropout from group cognitive-behavior therapy for insomnia? J. Psychosom. Res. 2008, 64, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Edinger, J.D.; Sampson, W.S. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep 2003, 26, 177–184. [Google Scholar] [PubMed]
- Germain, A.; Moul, D.E.; Franzen, P.L.; Miewald, J.M.; Reynolds, C.F.; Monk, T.H.; Buysse, D.J. Effects of a brief behavioral treatment for late-life insomnia: Preliminary findings. J. Clin. Sleep Med. 2006, 2, 403–406. [Google Scholar] [PubMed]
- Lovato, N.; Lack, L.; Wright, H.; Kennaway, D.J. Evaluation of a brief treatment program of cognitive behavior therapy for insomnia in older adults. Sleep 2014, 37, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Troxel, W.M.; Conrad, T.S.; Germain, A.; Buysse, D.J. Predictors of treatment response to brief behavioral treatment of insomnia (BBTI) in older adults. J. Clin. Sleep Med. 2013, 9, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- Perlis, M.L.; Smith, M.T. How can we make CBT-I and other BSM services widely available. J. Clin. Sleep Med. 2008, 4, 11–13. [Google Scholar]
- Morin, C.M.; Culbert, J.P.; Schwartz, S.M. Nonpharmacological interventions for insomnia. Am. J. Psychiatry 1994, 151, 1172–1180. [Google Scholar] [PubMed]
- Murtagh, D.R.; Greenwood, K.M. Identifying effective psychological treatments for insomnia: A meta-analysis. J. Consult. Clin. Psychol. 1995, 63, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, S.; Nordhus, I.H.; Kvale, G. Nonpharmacological interventions for insomnia in older adults: A meta-analysis of treatment efficacy. Psychotherapy 1998, 35, 472–482. [Google Scholar] [CrossRef]
- Montgomery, P.; Dennis, J.A. Cognitive behavioural interventions for sleep problems in adults aged 60+. Cochrane Database Syst. Rev. 2002, 2, CD003161. [Google Scholar]
- Irwin, M.R.; Cole, J.C.; Nicassio, P.M. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychol. 2006, 25, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Okajima, I.; Komada, Y.; Inoue, Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep Biol. Rhythms. 2011, 9, 24–34. [Google Scholar] [CrossRef]
- Mitchell, M.D.; Gehrman, P.; Perlis, M.; Umscheid, C.A. Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review. BMC Fam. Pract. 2012, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.B.; Espie, C.A.; Epstein, D.R.; Friedman, L.; Morin, C.M.; Pigeon, W.R.; Spielman, A.J.; Kyle, S.D. The evidence base of sleep restriction therapy for treating insomnia disorder. Sleep Med. Rev. 2014, 18, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Koffel, E.A.; Koffel, J.B.; Gehrman, P.R. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med. Rev. 2015, 19, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Q.; Appleman, E.R.; Salazar, R.D.; Ong, J.C. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: A meta-analysis. JAMA 2015, 175, 1461–1472. [Google Scholar] [CrossRef] [PubMed]
- Trauer, J.M.; Qian, M.Y.; Doyle, J.S.; Rajaratnam, S.M.; Cunnington, D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 163, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Ho, F.Y.; Chung, K.F.; Yeung, W.F.; Ng, T.H.; Kwan, K.S.; Yung, K.P.; Cheng, S.K. Self-help cognitive-behavioral therapy for insomnia: A meta-analysis of randomized controlled trials. Sleep Med. Rev. 2015, 19, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Geiger-Brown, J.M.; Rogers, V.E.; Liu, W.; Ludeman, E.M.; Downton, K.D.; Diaz-Abad, M. Cognitive behavioral therapy in persons with comorbid insomnia: A meta-analysis. Sleep Med. Rev. 2015, 23, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.K.; Lereya, S.T.; Boulton, H.; Miller, M.A.; Wolke, D.; Cappuccio, F.P. Nonpharmacological treatments of insomnia for long-term painful conditions: A systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep 2015, 38, 1751–1764. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.Y.; Zhang, Y.F.; Chen, J.; Liu, J.; Li, X.J.; Liu, Y.Z.; Lang, Y.; Lin, L.; Yang, X.J.; Jiang, X.J. Internet-based cognitive behavioral therapy for insomnia (ICBT-i) improves comorbid anxiety and depression—A meta-analysis of randomized controlled trials. PLoS ONE 2015, 10, e0142258. [Google Scholar] [CrossRef] [PubMed]
- Zachariae, R.; Lyby, M.S.; Ritterband, L.M.; O’Toole, M.S. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–A systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2016, 30, 1–10. [Google Scholar] [CrossRef] [PubMed]
- De Crescenzo, F.; Foti, F.; Ciabattini, M.; Del Giovane, C.; Watanabe, N.; Sañé Schepisi, M.; Quested, D.J.; Cipriani, A.; Barbui, C.; Amato, L. Comparative efficacy and acceptability of pharmacological treatments for insomnia in adults: A systematic review and network meta-analysis. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Johnson, J.A.; Rash, J.A.; Campbell, T.S.; Savard, J.; Gehrman, P.R.; Perlis, M.; Carlson, L.E.; Garland, S.N. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med. Rev. 2016, 30, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Seyffert, M.; Lagisetty, P.; Landgraf, J.; Chopra, V.; Pfeiffer, P.N.; Conte, M.L.; Rogers, M.A. Internet-Delivered Cognitive Behavioral Therapy to Treat Insomnia: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0149139. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.G.; Gehrman, P.; Espie, C.A.; Riemann, D.; Perlis, M.L. Acute insomnia: Current conceptualizations and future directions. Sleep Med. Rev. 2012, 16, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.G.; Perlis, M.L.; Gardani, M.; Bastien, C.H.; Espie, C.A. The Natural History of Insomnia: Acute insomnia and first onset depression. Sleep 2014, 37, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.G.; Cushing, T.; Germain, A. Treating Acute Insomnia: A Randomized Controlled Trial of a “Single-Shot” of Cognitive Behavioral Therapy for Insomnia. Sleep 2015, 38, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Bower, P.; Gilbody, S. Stepped care in psychological therapies: Access, effectiveness and efficiency. Br. J. Psychiatry 2005, 186, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Morin, C.M.; Schaefer, K.; Wallenstein, G.V. Interpreting score differences in the Insomnia Severity Index: Using health-related outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2009, 25, 2487–2494. [Google Scholar] [CrossRef] [PubMed]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Morin, C.M.; Ouellet, M.C.; Blais, F.C.; Bouchard, S. Cognitive-behavioral therapy for insomnia: Comparison of individual therapy, group therapy, and telephone consultations. J. Consult. Clin. Psychol. 2004, 72, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Manber, R.; Bernert, R.A.; Suh, S.; Nowakowski, S.; Siebern, A.T.; Ong, J.C. CBT for insomnia in patients with high and low depressive symptom severity: Adherence and clinical outcomes. J. Clin. Sleep Med. 2011, 7, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Manber, R.; Edinger, J.D.; Gress, J.L.; San Pedro-Salcedo, M.G.; Kuo, T.F.; Kalista, T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep 2008, 31, 489–495. [Google Scholar] [PubMed]
| Variables | Baseline | Follow-Up | Change Scores | ||
|---|---|---|---|---|---|
| Group (n = 13) | Individual (n = 12) | Group (n = 13) | Individual (n = 12) | ||
| PHQ-9 | 7.39 (5.46) | 6.92 (2.68) | 2.15 (2.58) | 3.5 (1.68) | −4.36 (3.92) |
| GAD-7 | 7.08 (5.14) | 8.00 (3.44) | 2.54 (2.6) | 3.75 (1.91) | −4.4 (4.26) |
| ISI | 15.92 (6.14) | 14.5 (3.8) | 5.15 (3.69) | 6.08 (2.61) | −9.64 (5.01) |
| SL | 27.95 (25.58) | 28.53 (17.81) | 10.8 (6.93) | 12.24 (7.57) | −16.73 (19.81) |
| WASO | 54.33 (35.63) | 28.65 (26.98) | 17.1 (13.92) | 14.62 (14.89) | −26.11 (33.58) |
| SE | 74.75 (13.54) | 78.83 (9.81) | 89.19 (4.83) | 87.46 (7.58) | 11.65 (13.21) |
| TST | 397.55 (76.9) | 425 (35.71) | 407.47 (53.68) | 433.45 (41.91) | 9.21 (52.01) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boullin, P.; Ellwood, C.; Ellis, J.G. Group vs. Individual Treatment for Acute Insomnia: A Pilot Study Evaluating a “One-Shot” Treatment Strategy. Brain Sci. 2017, 7, 1. https://doi.org/10.3390/brainsci7010001
Boullin P, Ellwood C, Ellis JG. Group vs. Individual Treatment for Acute Insomnia: A Pilot Study Evaluating a “One-Shot” Treatment Strategy. Brain Sciences. 2017; 7(1):1. https://doi.org/10.3390/brainsci7010001
Chicago/Turabian StyleBoullin, Pam, Christina Ellwood, and Jason G. Ellis. 2017. "Group vs. Individual Treatment for Acute Insomnia: A Pilot Study Evaluating a “One-Shot” Treatment Strategy" Brain Sciences 7, no. 1: 1. https://doi.org/10.3390/brainsci7010001






