Spasticity Management in Disorders of Consciousness
Abstract
:1. Introduction
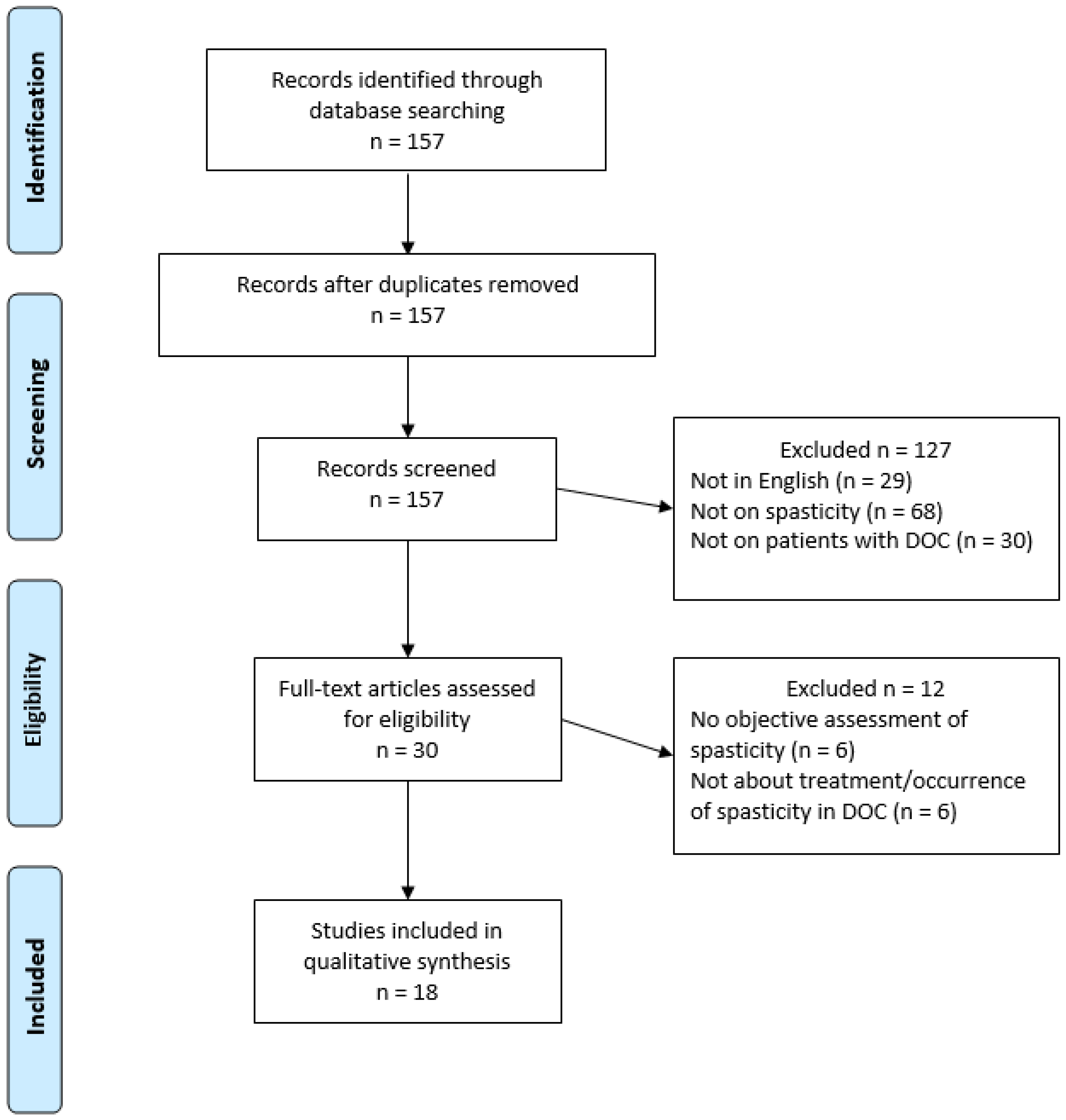
2. Materials and Methods
3. Results
3.1. Occurrence of Spasticity in DOC Patients
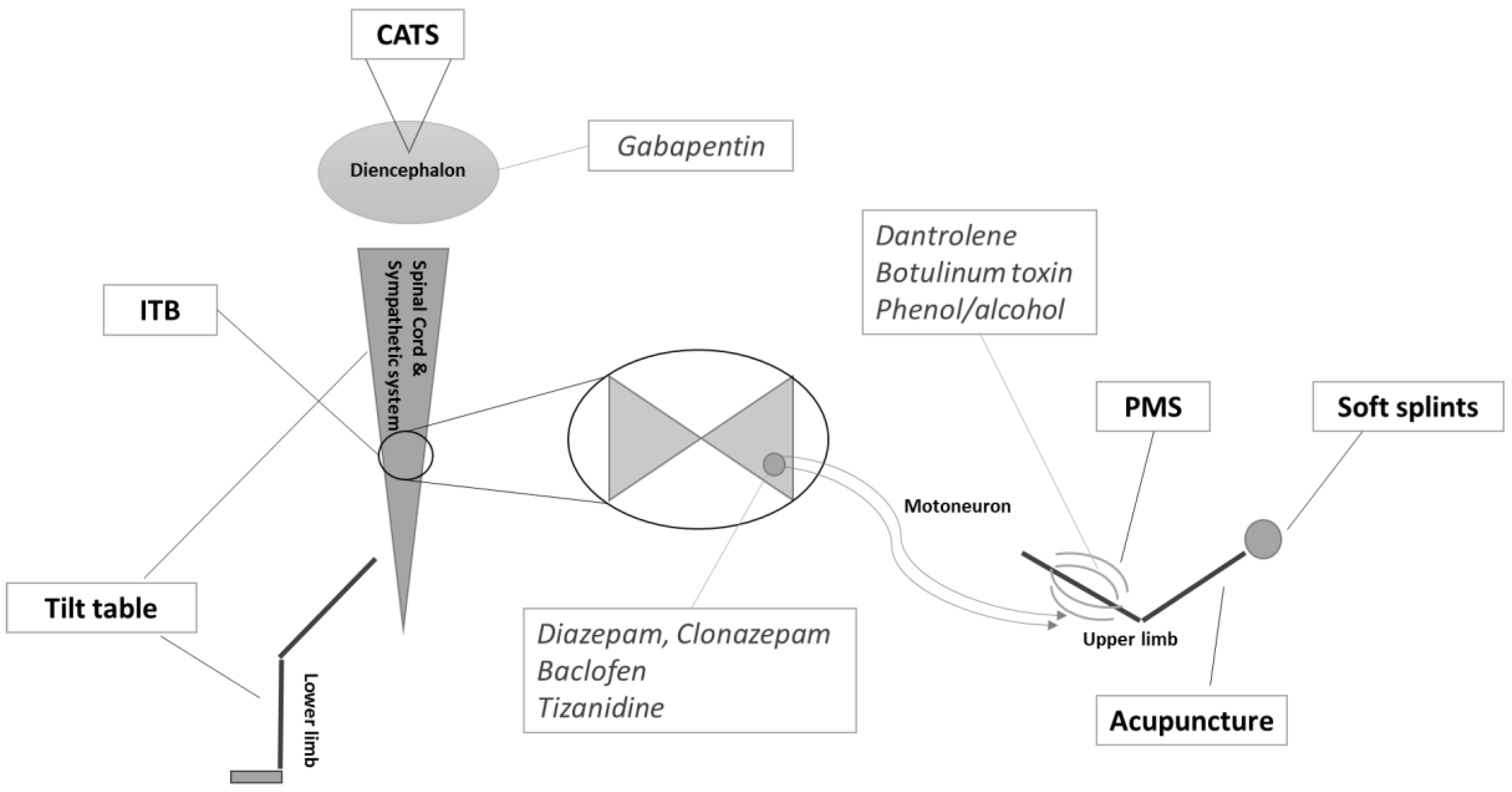
3.2. Treatments Targetting Spasticity in DOC Patients
3.3. Treatments with Spasticity as a Secondary Outcome in DOC Patients
4. Discussion
5. Conclusion
Acknowledgments
Conflicts of Interest
References
- Laureys, S.; Celesia, G.G.; Cohadon, F.; Lavrijsen, J.; Leon-Carrion, J.; Sannita, W.G.; Sazbon, L.; Schmutzhard, E.; von Wild, K.R.; Zeman, A.; et al. Unresponsive wakefulness syndrome: A new name for the vegetative state or apallic syndrome. BMC Med. 2010, 8, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giacino, J.T.; Ashwal, S.; Childs, N.; Cranford, R.; Jennett, B.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Whyte, J.; Zafonte, R.D.; et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 2002, 58, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Chatelle, C.; Wannez, S.; Deltombe, T.; Stender, J.; Schnakers, C.; Laureys, S.; Gosseries, O. Spasticity in disorders of consciousness: A behavioral study. Eur. J. Phys. Rehabil. Med. 2015, 51, 389–397. [Google Scholar] [PubMed]
- Lance, J.W. Spasticity: Disorders Motor Control. Symposium Synopsis; Feldman, R.G., Young, R.P., Koella, W.P., Eds.; Year Book Medical Publishers: Miami, FL, USA, 1980. [Google Scholar]
- Dietz, V.; Sinkjaer, T. Spastic movement disorder: Impaired reflex function and altered muscle mechanics. Lancet Neurol. 2007, 6, 725–733. [Google Scholar] [CrossRef]
- Burke, D.; Wissel, J.; Donnan, G.A. Pathophysiology of spasticity in stroke. Neurology 2013, 80 (Suppl. S2), S20–S26. [Google Scholar] [CrossRef] [PubMed]
- Gracies, J.M. Pathophysiology of spastic paresis. I: Paresis and soft tissue changes. Muscle Nerve 2005, 31, 535–551. [Google Scholar] [CrossRef] [PubMed]
- Wissel, J.; Schelosky, L.D.; Scott, J.; Christe, W.; Faiss, J.H.; Mueller, J. Early development of spasticity following stroke: A prospective, observational trial. J. Neurol. 2010, 257, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- McClelland, S.; Bethoux, F.A.; Boulis, N.M.; Sutliff, M.H.; Stough, D.K.; Schwetz, K.M.; Gogol, D.M.; Harrison, M.; Pioro, E.P. Intrathecal baclofen for spasticity-related pain in amyotrophic lateral sclerosis: Efficacy and factors associated with pain relief. Muscle Nerve 2008, 37, 396–398. [Google Scholar] [CrossRef] [PubMed]
- Shiel, A.; Gelling, L.; Wilson, B.; Coleman, M.; Pickard, J. Difficulties in diagnosing the vegetative state. Br. J. Neurosurg. 2004, 18, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Whyte, J.; Bagiella, E.; Kalmar, K.; Childs, N.; Khademi, A.; Eifert, B.; Long, D.; Katz, D.I.; Cho, S.; et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N. Engl. J. Med. 2012, 366, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Bruno, M.-A.; Ledoux, D.; Demertzi, A.; Laureys, S. tDCS in patients with disorders of consciousness: Sham-controlled randomized double-blind study. Neurology 2014, 82, 1112–1128. [Google Scholar] [CrossRef] [PubMed]
- Monti, M.M.; Schnakers, C.; Korb, A.S.; Bystritsky, A.; Vespa, P.M. Non-Invasive Ultrasonic Thalamic Stimulation in Disorders of Consciousness after Severe Brain Injury: A First-in-Man Report. Brain Stimul. 2016, 9, 940–941. [Google Scholar] [CrossRef] [PubMed]
- Burchiel, K.J.; Hsu, F.P.K. Pain and Spasticity After Spinal Cord Injury Mechanisms and Treatment. Spine 2001, 26, 146–160. [Google Scholar] [CrossRef]
- Ward, A.B. A summary of spasticity management—A treatment algorithm. Eur. J. Neurol. 2002, 9, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Chatelle, C.; De Val, M.D.; Catano, A.; Chaskis, C.; Seeldrayers, P.; Laureys, S.; Biston, P.; Schnakers, C. Is the Nociception Coma Scale-Revised a Useful Clinical Tool for Managing Pain in Patients with Disorders of Consciousness? Clin. J. Pain. 2016, 32, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Nakase-Richardson, R.; McNamee, S.; Howe, L.L.; Massengale, J.; Peterson, M.; Barnett, S.D.; Harris, O.; McCarthy, M.; Tran, J.; Scott, S.; et al. Descriptive characteristics and rehabilitation outcomes in active duty military personnel and veterans with disorders of consciousness with combat- and noncombat-related brain injury. Arch. Phys. Med. Rehabil. 2013, 94, 1861–1869. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, S.; Guernon, A.; Chalcraft, L.; Harton, B.; Smith, B.; Louise-Bender Pape, T. Medical comorbidities in disorders of consciousness patients and their association with functional outcomes. Arch. Phys. Med. Rehabil. 2013, 94, 1899–1907. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Deltombe, T.; Wannez, S.; Gosseries, O.; Ziegler, E.; Dieni, C.; Deroy, M.; Laureys, S. Impact of soft splints on upper limb spasticity in chronic patients with disorders of consciousness: A randomized, single-blind, controlled trial. Brain Inj. 2015, 29, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto-Miyazaki, J.; Asano, Y.; Ikegame, Y.; Kawasaki, T.; Nomura, Y.; Shinoda, J. Acupuncture Reduces Excitability of Spinal Motor Neurons in Patients with Spastic Muscle Overactivity and Chronic Disorder of Consciousness Following Traumatic Brain Injury. J. Altern. Complement. Med. 2016, 22, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, P.; Malla, H.; Pant, B.; Taira, T. Intrathecal baclofen therapy in severe head injury, first time in Nepal, a technique suitable for underdeveloped countries. Asian J. Neurosurg. 2011, 6, 49–51. [Google Scholar] [PubMed]
- Francois, B.; Vacher, P.; Roustan, J.; Salle, J.Y.; Vidal, J.; Moreau, J.J.; Vignon, P. Intrathecal baclofen after traumatic brain injury: Early treatment using a new technique to prevent spasticity. J. Trauma—Inj. Infect. Crit. Care 2001, 50, 158–161. [Google Scholar] [CrossRef]
- Leong, B. The vegetative and minimally conscious states in children: Spasticity, muscle contracture and issues for physiotherapy treatment. Brain Inj. 2002, 16, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Leong, B. Critical review of passive muscle stretch: Implications for the treatment of children in vegetative and minimally conscious states. Brain Inj. 2002, 16, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.; Alberti, O.; Bauer, B.L. Continuous intrathecal baclofen infusion in severe spasticity after traumatic or hypoxic brain injury. J. Neurol. 1997, 244, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Lehmkuhl, L.D.; Thoi, L.L.; Baize, C.; Kelley, C.J.; Krawczyk, L.; Bontke, C.F. Multimodality treatment of joint contractures in patients with severe brain injury: Cost, effectiveness, and integration of therapies in the application of serial/inhibitive casts. J. Head Trauma Rehabil. 1990, 5, 23–42. [Google Scholar] [CrossRef]
- Magrassi, L.; Maggioni, G.; Pistarini, C.; Di Perri, C.; Bastianello, S.; Zippo, A.G.; Iotti, G.A.; Biella, G.E.; Imberti, R. Results of a prospective study (CATS) on the effects of thalamic stimulation in minimally conscious and vegetative state patients. J. Neurosurg. Am. Assoc. Neurol. Surg. 2016, 125, 972–981. [Google Scholar] [CrossRef] [PubMed]
- Krewer, C.; Luther, M.; Koenig, E.; Müller, F. Tilt Table Therapies for Patients with Severe Disorders of Consciousness: A Randomized, Controlled Trial. PLoS ONE 2015, 10, e0143180. [Google Scholar] [CrossRef] [PubMed]
- Margetis, K.; Korfias, S.I.; Gatzonis, S.; Boutos, N.; Stranjalis, G.; Boviatsis, E.; Sakas, D.E. Intrathecal baclofen associated with improvement of consciousness disorders in spasticity patients. Neuromodulation 2014, 17, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Al-Khodairy, A.T.; Wicky, G.; Nicolo, D.; Vuadens, P. Influence of intrathecal baclofen on the level of consciousness and mental functions after extremely severe traumatic brain injury: Brief report. Brain Inj. 2015, 29, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Oyama, H.; Kito, A.; Maki, H.; Hattori, K.; Tanahashi, K. Consciousness Recovery Induced by Intrathecal Baclofen Administration After Subarachnoid Hemorrhage. Neurol. Med. Chir. 2010, 50, 386–390. [Google Scholar] [CrossRef]
- Taira, T. Intrathecal administration of GABA agonists in the vegetative state. Prog. Brain Res. 2009, 177, 317–328. [Google Scholar] [PubMed]
- Sara, M.; Pistoia, F.; Mura, E.; Onorati, P.; Govoni, S. Intrathecal baclofen in patients with persistent vegetative state: 2 hypotheses. Arch. Phys. Med. Rehabil. 2009, 90, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Mazaux, J.M.; De Sèze, M.; Joseph, P.A.; Barat, M. Early rehabilitation after severe brain injury: A French perspective. J. Rehabil. Med. 2001, 33, 99–109. [Google Scholar] [PubMed]
- Bobath, B. The very early treatment of cerebral palsy. Dev. Med. Child Neurol. 1967, 9, 373–390. [Google Scholar] [CrossRef] [PubMed]
- Pistoia, F.; Sacco, S.; Sarà, M.; Franceschini, M.; Carolei, A. Intrathecal Baclofen: Effects on Spasticity, Pain, and Consciousness in Disorders of Consciousness and Locked-in Syndrome. Curr. Pain Headache Rep. 2015, 19, 466. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Chatelle, C.; Ziegler, E.; Bruno, M.-A.; Laureys, S.; Gosseries, O. Spasticity after stroke: Physiology, assessment and treatment. Brain Inj. 2013, 27, 1093–1105. [Google Scholar] [CrossRef] [PubMed]
| Authors | Study Type | n | Intervention | Results |
|---|---|---|---|---|
| Occurrence of Spasticity in DOC Patients | ||||
| Thibaut et al., 2014 [3] | Prospective | 65 | / | 89% showed spasticity (MAS ≥ 1) |
| Nakase-Richardson, 2013 [17] | Prospective | 122 | / | 70% showed spasticity (requiring oral medications, injections or surgical procedure) |
| Ganesh et al., 2013 [18] | Prospective | 68 | / | 57% showed spasticity |
| Treatments targeting spasticity in DOC patients | ||||
| Thibaut et al., 2015 [19] | Randomized controlled trial | 17 | Soft splints applied to the hand for 30 min | Significant decrease (p = 0.014) in the MAS scores (3.5 to 2.5) of the finger flexor muscles |
| Mastumoto-Miyazaki et al., 2016 [20] | Randomized controlled trial | 11 | Japanese style acupuncture on 6 points for 10 min | Significant decrease in F/M ratio (p < 0.001) of the abductor pollicis brevis |
| Shrestha et al., 2011 [21] | Case report | 1 | ITB injections of 50 µg daily for 2 weeks then 100 µg daily for 3 weeks through epidural catheter | Significant decrease of spasticity (subjective report). Patients discharged 2.5 months later, could walk with support |
| Francois et al., 2001 [22] | Case report | 4 | ITB injections of 25 µg/mL continuously through intrathecal catheter and then pump | Decrease in MAS score (4.5 to 3.5 for upper limbs and 4.5 to 2 for lower limbs, on average). |
| Leong, 2002 [23] | Review | / | / | / |
| Leong, 2002 [24] | Systematic review | 17 studies | Passive muscle stretch | Limited evidence |
| Treatments with spasticity as secondary outcome | ||||
| Magrassi et al., 2016 [27] | Clinical trial | 3 | Implantation of bilateral thalamic electrodes | Decrease in spasticity and myoclonus (Unified Myoclonus Rating Scale Section 2 and Section 3: decrease of >25 points) |
| Krewer et al., 2015 [28] | Randomized controlled trial | 50 | Tilt table therapy (with our without integrated stepping device) 10 × 1 h | No significant differences (8.5% of all MAS values showed improvement, 19.7% showed worsening and 71.8% showed no difference) |
| Margetis et al., 2014 [29] | Open-label | 8 | ITB pump | Decrease in MAS scores from 3.4 to 1, on average |
| Al-Khodairy et al., 2015 [30] | Case report | 2 | ITB pump | Decrease in MAS scores (minimum 2 points) |
| Oyama et al., 2010 [31] | Case report | 2 | ITB pump (50 µg/day) | Decrease in MAS scores (minimum 1 point) |
| Taira, 2009 [21] | Case report | 2 | ITB through lumbar puncture | Effective control of the spasticity |
| Sara et al., 2009 [36] | Case report | 5 | ITB pump (100 µg/day) | Decrease in MAS scores (1 point, on average) |
| Mazaux et al., 2001 [34] | Review | / | / | Good agreement exists among clinicians about prevention of orthopedic complications and treatment for spasticity. However, little consensus exists concerning treatment of non-pyramidal hypertonia and spasms. |
| Pistoia et al., 2015 [36] | Review | / | / | Although the current indication of ITB is the management of severe spasticity, its potential use in speeding the recovery of consciousness merits further investigation. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martens, G.; Laureys, S.; Thibaut, A. Spasticity Management in Disorders of Consciousness. Brain Sci. 2017, 7, 162. https://doi.org/10.3390/brainsci7120162
Martens G, Laureys S, Thibaut A. Spasticity Management in Disorders of Consciousness. Brain Sciences. 2017; 7(12):162. https://doi.org/10.3390/brainsci7120162
Chicago/Turabian StyleMartens, Géraldine, Steven Laureys, and Aurore Thibaut. 2017. "Spasticity Management in Disorders of Consciousness" Brain Sciences 7, no. 12: 162. https://doi.org/10.3390/brainsci7120162





