Abuse of Prescription Drugs in the Context of Novel Psychoactive Substances (NPS): A Systematic Review
Abstract
:1. Introduction
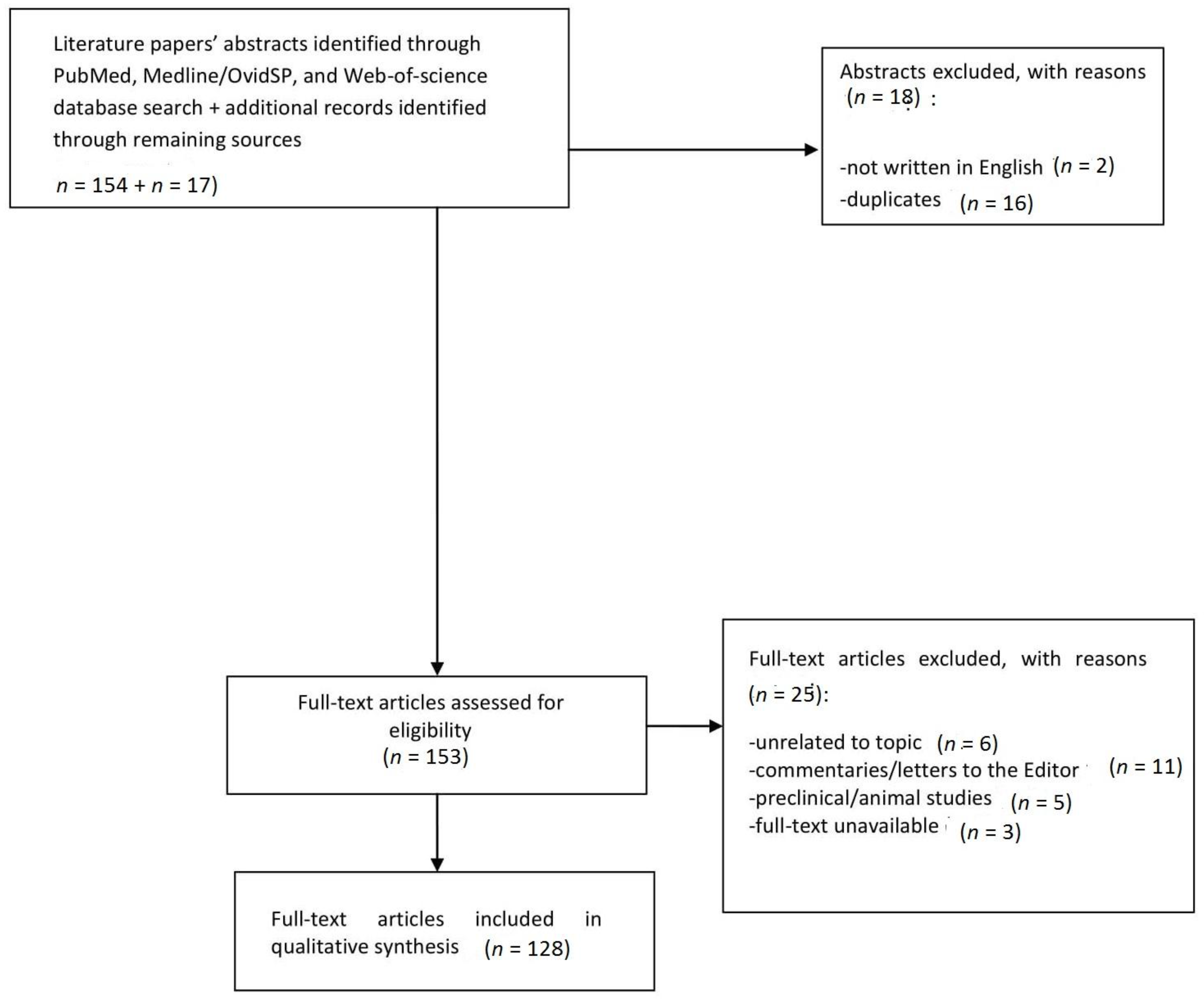
2. Materials and Methods
3. Results
3.1. Gabapentinoids
3.2. Antidepressants
3.3. Antipsychotics
3.4. Image-And Performance-Enhancing Drugs (IPEDs)
3.5. Over-The-Counter (OTC) Medicines—Loperamide
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Schifano, F.; Orsolini, L.; Papanti, D.; Corkery, J.M. Novel psychoactive substances of interest for psychiatry. World Psychiatry 2015, 14, 15–26. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office for Drugs and Crime (UNODC). Early Warning Advisory on New Psychoactive Substances. Available online: https://www.unodc.org/LSS/Page/NPS (accessed on 20 January 2018).
- European Monitoring Centre for Drugs and Drug Abuse (EMCDDA). European Drug Report. Trends and Developments; EMCDDA: Lisbon, Portugal, 2017. Available online: http://www.emcdda.europa.eu/system/files/publications/4541/TDAT17001ENN.pdf (accessed on 2 March 2018).
- Zawilska, J.B.; Andrzejczak, D. Next generation of novel psychoactive substances on the horizon—A complex problem to face. Drug Alcohol Depend. 2015, 157, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, M.C.; Hearne, E. New psychoactive substances (NPS) on crypto market fora: An exploratory study of characteristics of forum activity between NPS buyers and vendors. Int. J. Drug Policy 2017, 40, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Soussan, C.; Andersson, M.; Kjellgren, A. The diverse reasons for using Novel Psychoactive Substances—A qualitative study of the users’ own perspectives. Int. J. Drug Policy 2018, 52, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Chiappini, S.; Schifano, F. A decade of gabapentinoid misuse: An analysis of the European Medicines Agency’s ‘suspected adverse drug reactions’ database. Assessment of gabapentinoid misuse/dependence as reported to the EMA. CNS Drugs 2016, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Chiappini, S.; Schifano, F. Is there a potential of misuse for quetiapine? Literature review and analysis of the European Medicines Agency/EMA Adverse Drug Reactions’ database. J. Clin. Psychopharmacol. 2018, 38, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.F.; Sharma, M.S.; Brunoni, A.R.; Vieta, E.; Fava, G.A. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: A critical review of the literature. Psychother. Psychosom. 2016, 85, 270–288. [Google Scholar] [CrossRef] [PubMed]
- Milano, G.; Chiappini, S.; Mattioli, F.; Martelli, A.; Schifano, F. β-2 agonists as misusing Drugs? Assessment of both Clenbuterol- and Salbutamol-related European Medicines Agency (EMA) Pharmacovigilance Database Reports. Basic Clin. Pharmacol. Toxicol. 2018, 2. [Google Scholar] [CrossRef]
- Sheridan, D.C.; Hendrickson, R.G.; Beauchamp, G.; Laurie, A.; Fu, R.; Horowitz, B.Z. Adolescent Intentional Abuse Ingestions: Overall 10-Year Trends and Regional Variation. Pediatr. Emerg. Care 2016. [Google Scholar] [CrossRef] [PubMed]
- Lasoff, D.R.; Koh, C.H.; Corbett, B.; Minns, A.B.; Cantrell, F.L. Loperamide Trends in Abuse and Misuse Over 13 Years: 2002–2015. Pharmacotherapy 2017, 37, 249–253. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency (EMA). Pharmacovigilance. Available online: http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000258.jsp (accessed on 20 January 2017).
- European Medicines Agency (EMA). EudraVigilance. Available online: http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000679.jsp (accessed on 3 March 2018).
- Prisma. Transparent Reporting of Systematic Reviews and Meta-Analyses. Available online: http://www.prisma-statement.org/ (accessed on 21 December 2017).
- Schifano, F. Misuse and Abuse of Pregabalin and Gabapentin: Cause for Concern? CNS Drugs 2014, 28, 491. [Google Scholar] [CrossRef] [PubMed]
- Evoy, K.E.; Morrison, M.D.; Saklad, S.R. Abuse and Misuse of Pregabalin and Gabapentin. Drugs 2017, 77, 403–426. [Google Scholar] [CrossRef] [PubMed]
- Schjerning, O.; Rosenzweig, M.; Pottegård, A.; Damkier, P.; Nielsen, J. Abuse Potential of Pregabalin: A Systematic Review. CNS Drugs 2016, 30, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Schjerning, O.; Pottegård, A.; Damkier, P.; Rosenzweig, M.; Nielsen, J. Use of Pregabalin—A Nationwide Pharmacoepidemiological Drug Utilization Study with Focus on Abuse Potential. Pharmacopsychiatry 2016, 49, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Erowid. Experiences. Available online: https://erowid.org/experiences/ (accessed on 16 January 2018).
- Drug Enforcement Administration. Schedules of Controlled Substances: Placement of Pregabalin into Schedule V. Available online: https://www.deadiversion.usdoj.gov/fed_regs/rules/2005/fr0728.htm (accessed on 16 January 2018).
- Bonnet, U.; Scherbaum, N. How addictive are gabapentin and pregabalin? A systematic review. Eur. Neuropsychopharmacol. 2017, 27, 1185–1215. [Google Scholar] [CrossRef] [PubMed]
- Daly, C.; Griffin, E.; Ashcroft, D.M.; Webb, R.T.; Perry, I.J.; Arensman, E. Intentional Drug Overdose Involving Pregabalin and Gabapentin: Findings from the National Self-Harm Registry Ireland, 2007–2015. Clin. Drug Investig. 2017, 20. [Google Scholar] [CrossRef] [PubMed]
- Reeves, R.R.; Ladner, M.E. Potentiation of the effect of buprenorphine/naloxone with gabapentin or quetiapine. Am. J. Psychiatry 2014, 171, 691. [Google Scholar] [CrossRef] [PubMed]
- Greater use of gabapentinoids in intentional drug overdose. Available online: https://doi.org/10.1007/s40278-018-40617-3 (accessed on 21 April 2018).
- OECD Indicators. Health at a Glance. 2015. Available online: http://www.keepeek.com/Digital-Asset-Management/oecd/social-issues-migration-health/health-at-a-glance-2015_health_glance-2015-en#page187 (accessed on 20 January 2018).
- Kantor, E.D.; Rehm, C.D.; Haas, J.S.; Chan, A.T.; Giovannucci, E.L. Trends in prescription drug use among adults in the US from 1999–2012. JAMA 2015, 314, 1818–1831. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.S.; Bell, H.G.; Gilbert, M.; Davidson, J.E.; Winter, C.; Barratt, M.J.; Win, B.; Painter, J.L.; Menone, C.; Sayegh, J.; et al. Using Social Listening Data to Monitor Misuse and Nonmedical Use of Bupropion: A Content Analysis. JMIR Public Health Surveill. 2017, 3, e6. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.A.; Sullivan, M.A. Abuse and misuse of antidepressants. Subst. Abuse Rehabil. 2014, 5, 107–120. [Google Scholar] [CrossRef] [PubMed]
- McCormick, J. Recreational bupropion abuse in a teenager. Br. J. Clin. Pharmacol. 2002, 53, 211–214. [Google Scholar] [CrossRef]
- Welsh, C.J.; Doyon, S. Seizure-induced by insufflation of bupropion. N. Engl. J. Med. 2002, 347, 951. [Google Scholar] [CrossRef] [PubMed]
- Glaxo Smith and Kline (GSK). 2012 35 Clinical Study Result Summary. PRJ2215: Assessment of Buproprion Misuse/Abuse 2004–2011; Updated August 2016. Available online: https://www.gsk-clinicalstudyregister.com/files2/201235-Clinical-Study-Result-Summary.pdf (accessed on 20 October 2017).
- Reeves, R.R.; Ladner, M.E. Additional evidence of the abuse potential of bupropion. J. Clin. Psychopharmacol. 2013, 33, 584–585. [Google Scholar] [CrossRef] [PubMed]
- Baribeau, D.; Araki, K.F. Intravenous bupropion: A previously undocumented method of abuse of a commonly prescribed antidepressant agent. J. Addict. Med. 2013, 7, 216–217. [Google Scholar] [CrossRef] [PubMed]
- Stahl, S.M.; Pradko, J.F.; Haight, B.R.; Modell, J.G.; Rockett, C.B.; Learned-Coughlin, S. A Review of the Neuropharmacology of Bupropion, a Dual Norepinephrine and DA Reuptake Inhibitor. J. Clin. Psychiatry 2004, 6, 159–166. [Google Scholar] [CrossRef]
- Guzman, F. The Psychopharmacology of Bupropion: An Illustrated Overview. Available online: http://psychopharmacologyinstitute.com/antidepressants/bupropion-psychopharmacology/ (accessed on 7 October 2017).
- Prosser, J.M.; Nelson, L.S. The toxicology of bath salts: A review of synthetic cathinones. J. Med. Toxicol. 2012, 8, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Vento, A.E.; Schifano, F.; Gentili, F.; Pompei, F.; Corkery, J.M.; Kotzalidis, G.D.; Girardi, P. Bupropion perceived as a stimulant by two patients with a previous history of cocaine misuse. Ann. Super Sanita 2013, 49, 402–405. [Google Scholar] [CrossRef]
- Rettew, D.C.; Hudziak, J.J. Bupropion. In Essentials of Clinical Psychopharmacology, 2nd ed.; Schatzberg, A.F., Nemeroff, C.B., Eds.; American Psychiatric Publishing Inc.: Arlington, VA, USA, 2001; ISBN 1585624195. [Google Scholar]
- Stall, N.; Godwin, J.; Juurlink, D. Bupropion abuse and overdose. CMAJ 2014, 186, 1015. [Google Scholar] [CrossRef] [PubMed]
- Stassinos, G.L.; Klein-Schwartz, W. Bupropion “Abuse” Reported to US Poison Centers. J. Addict. Med. 2016, 10, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Toxnet, Toxicology Data Network. Bupropion; National Library of Medicine HSDB Database. 2015. Available online: https://toxnet.nlm.nih.gov/cgi-bin/sis/search/a?dbs+hsdb:@term+@DOCNO+6988 (accessed on 19 October 2017).
- Hill, S.; Sikand, H.; Lee, J. Letter to the editor. A case report of seizure induced by bupropion nasal insufflation. J. Clin. Psychiatry 2007, 9, 67–69. [Google Scholar]
- Yoon, G.; Westermeyer, J. Intranasal bupropion abuse case report. Am. J. Addict. 2013, 22, 180. [Google Scholar] [CrossRef] [PubMed]
- Hilliard, W.T.; Barloon, L.; Farley, P.; Penn, J.V.; Koranek, A. Bupropion diversion and misuse in the correctional facility. J. Correct. Health Care 2013, 19, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D. Wellbutrin: Misuse and abuse by incarcerated individuals. J. Addict. Nurs. 2012, 23, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Laird, G.; Narayan, P. Formulary Controls: Abuse of Psychotropics, and Dispensary Costs in the Incarceration Environment. Available online: http://www.fmhac.net/Assets/Documents/2009/Presentations/Laird%20Formulary%20Controls.pdf (accessed on 6 October 2017).
- European Medicines Agency (EMA). Venlafaxine. 2007. Available online: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Efexor/human_referral_000020.jsp (accessed on 20 December 2017).
- Harvey, A.T.; Rudolph, R.L.; Preskorn, S.H. Evidence of the dual mechanisms of action of venlafaxine. Arch. Gen. Psychiatry 2000, 57, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Weikop, P.; Kehr, J.; Scheel-Krüger, J. The role of alpha1- and alpha2-adrenoreceptors on venlafaxine-induced elevation of extracellular serotonin, noradrenaline and DA levels in the rat prefrontal cortex and hippocampus. J. Psychopharmacol. 2004, 18, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Maj, J.; Rogoz, Z. Pharmacological effects of venlafaxine, a new antidepressant, given repeatedly, on the alpha 1-adrenergic, DA and serotonin systems. J. Neural Transm. 1999, 106, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Sabljić, V.; Ružić, K.; Rakun, R. Venlafaxine withdrawal syndrome. Psychiatr. Danub. 2011, 23, 117–119. [Google Scholar] [PubMed]
- Fava, M.; Mulroy, R.; Alpert, J.; Nierenberg, A.; Rosenbaum, J. Emergence of adverse events following discontinuation of treatment with extended-release venlafaxine. Am. J. Psychiatry 1997, 12, 1760–1762. [Google Scholar] [CrossRef] [PubMed]
- Stahl, S.M.; Grady, M.M.; Moret, C.; Briley, M. SNRIs: Their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. 2005, 10, 732–747. [Google Scholar] [CrossRef] [PubMed]
- Sir, A.; D’Souza, R.F.; Uguz, S.; George, T.; Vahip, S.; Hopwood, M.; Martin, A.J.; Lam, W.; Burt, T. Randomized Trial of Sertraline Versus Venlafaxine XR in Major Depression: Efficacy and Discontinuation Symptoms. J. Clin. Psychiatry 2005, 66, 1312–1320. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.; Stewart, S.; Connolly, A. Antidepressant withdrawal symptoms-telephone calls to a national medication helpline. J. Affect. Disord. 2006, 95, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Llorca, P.M.; Fernandez, J.L. Escitalopram in the treatment of major depressive disorder: Clinical efficacy, tolerability and cost-effectiveness vs. venlafaxine extended-release formulation. Int. J. Clin. Pract. 2007, 61, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Kotzalidis, G.D.; de Pisa, E.; Patrizi, B.; Savoja, V.; Ruberto, G.; Girardi, P. Similar discontinuation symptoms for withdrawal from medium-dose paroxetine and venlafaxine. J. Psychopharmacol. 2008, 22, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Koga, M.; Kodaka, F.; Miyata, H.; Nakayama, K. Symptoms of delusion: The effects of discontinuation of low-dose venlafaxine. Acta Psychiatr. Scand. 2008, 120, 329–331. [Google Scholar] [CrossRef] [PubMed]
- Holland, J.; Brown, R. Neonatal venlafaxine discontinuation syndrome: A mini-review. Eur. J. Paediatr. Neurol. 2017, 21, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Cutler, N. Severe Venlafaxine Withdrawal Successfully Treated With a Short Course of Duloxetine. Prim. Care Companion CNS Disord. 2017, 19. [Google Scholar] [CrossRef] [PubMed]
- Groot, P.C. Consensus group Tapering. [Tapering strips for paroxetine and venlafaxine]. Tijdschr. Psychiatr. 2013, 55, 789–794. [Google Scholar] [PubMed]
- Francesconi, G.; Orsolini, L.; Papanti, D.; Corkery, J.M.; Schifano, F. Venlafaxine as the ‘baby ecstasy’? Literature overview and analysis of web-based misusers’ experiences. Hum. Psychopharmacol. 2015, 30, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.P.; Grant, K.M.; Bhatia, S.C. A case of venlafaxine abuse. N. Engl. J. Med. 2003, 348, 764–765. [Google Scholar] [CrossRef] [PubMed]
- Venlafaxine overdose. Available online: https://doi.org/10.1007/s40278-018-40604-4 (accessed on 21 April 2018).
- Baker, D.R.; Barron, L.; Kasprzyk-Hordern, B. Illicit and pharmaceutical drug consumption estimated via wastewater analysis. Part A: Chemical analysis and drug use estimates. Sci. Total Environ. 2014, 487, 629–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fountain, J.S.; Slaughter, R.J. TOXINZ, the New Zealand Internet poisons information database: The first decade. Emerg. Med. Australas. 2016, 28, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Schifano, F.; Chiappini, S. Is there a potential of misuse for venlafaxine and bupropion? Front. Neuropharmacol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Health and Social Care Information Centre (HSCIC). Prescriptions Dispensed in the Community. England 2004–2014. Available online: http://content.digital.nhs.uk/catalogue/PUB17644/pres-disp-com-eng-2004-14-rep.pdf (accessed on 20 February 2017).
- Bogart, G.T.; Ott, C.A. Abuse of second-generation antipsychotics: What prescribers need to know. Curr. Psychiatry 2011, 10, 77–79. [Google Scholar] [CrossRef]
- Sarker, A.; O’Connor, K.; Ginn, R.; Scotch, M.; Smith, K.; Malone, D.; Gonzalez, G. Social Media Mining for Toxicovigilance: Automatic Monitoring of Prescription Medication Abuse from Twitter. Drug Saf. 2016, 39, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Advisory Council on the Misuse Drugs (ACMD). ACMD Report on Diversion and Illicit Supply of Medicines. 2016. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/580296/Meds_report-_final_report_15_December_LU__2_.pdf (accessed on 26 February 2018).
- Food and Drug Administration (FDA). Seroquel Prescribing Information. 2010. Available online: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020639s049s054lbl.pdf (accessed on 20 February 2017).
- Terán, A.; Majadas, S.; Galan, J. Quetiapine in the treatment of sleep disturbances associated with addictive conditions: A retrospective study. Subst. Use Misuse 2008, 43, 2169–2171. [Google Scholar] [CrossRef]
- Srivastava, A.; Patil, V.; Da Silva Pereira, Y. A Case Series of Quetiapine Addiction/Dependence. Ger. J. Psychiatr. 2013, 16, 152–155. [Google Scholar]
- Kim, S.; Lee, G.; Kim, E.; Jung, H.; Chang, J. Quetiapine Misuse and Abuse: Is it an Atypical Paradigm of Drug-Seeking Behavior? J. Res. Pharm. Pract. 2017, 6, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Di Chiara, G.; Imperato, A. Drugs abused by humans preferentially increase synaptic DA concentrations in the mesolimbic system of freely moving rats. Proc. Natl. Acad. Sci. USA 1988, 85, 5274–5278. [Google Scholar] [CrossRef] [PubMed]
- Waters, B.M.; Joshi, K.G. Intravenous Quetiapine-Cocaine Use (“Q-Ball”). Am. J. Psychiatry 2007, 164, 173–174. [Google Scholar] [CrossRef] [PubMed]
- Pierre, J.M.; Shnayder, I.; Wirshing, D.A.; Wirshing, W.C. Intranasal quetiapine abuse. Am. J. Psychiatry 2004, 61, 1718. [Google Scholar] [CrossRef] [PubMed]
- George, M.; Haasz, M.; Coronado, A.; Salhanick, S.; Korbel, L.; Kitzmiller, J.P. Acute dyskinesia, myoclonus, and akathisia in an adolescent male abusing quetiapine via nasal insufflation: A case study. BMC Pediatr. 2013, 13, 187. [Google Scholar] [CrossRef] [PubMed]
- Morin, A.K. Possible intranasal quetiapine misuse. Am. J. Health Syst. Pharm. 2007, 64, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Fischer, B.A.; Boggs, D.L. The role of antihistaminic effects in the misuse of quetiapine: A case report and review of the literature. Neurosci. Biobehav. Rev. 2010, 34, 555–558. [Google Scholar] [CrossRef] [PubMed]
- Reeves, R.R.; Brister, J.C. Additional evidence of the abuse potential of quetiapine. South. Med. J. 2007, 100, 834–836. [Google Scholar] [CrossRef] [PubMed]
- Paparrigopoulos, T.; Karaiskos, D.; Liappas, J. Quetiapine: Another drug with potential for misuse? A case report. J. Clin. Psychiatry 2008, 69, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Shiah, I.S.; Lee, W.K.; Kuo, S.C.; Huang, C.C.; Wang, T.Y. Dependence on quetiapine in combination with zolpidem and clonazepam in bipolar depression. Psychiatry Clin. Neurosci. 2009, 63, 427–428. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.Z.; Waheed, W.; Hussain, S. Intravenous quetiapine abuse. Am. J. Psychiatry 2005, 162, 1755–1756. [Google Scholar] [CrossRef] [PubMed]
- Sansone, R.A.; Sansone, L.A. Is Seroquel developing an illicit reputation for misuse/abuse? Psychiatry 2010, 7, 13–16. [Google Scholar]
- Murphy, D.; Bailey, K.; Stone, M.; Wirshing, W.C. Addictive potential of quetiapine. Am. J. Psychiatry 2008, 165, 167. [Google Scholar] [CrossRef] [PubMed]
- Peyrière, H.; Diot, C.; Eiden, C.; Petit, P. Réseau de centres de d’Addictovigilance. Abuse Liability of Quetiapine (Xeroquel®): Analysis of the literature. Fundam. Clin. Pharmacol. 2015, 29, 27–28. [Google Scholar] [CrossRef]
- Pilgrim, J.L.; Drummer, O.H. The toxicology and comorbidities of fatal cases involving quetiapine. Forensic Sci. Med. Pathol. 2013, 9, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Haller, E.; Bogunovic, O.; Miller, M. Atypical antipsychotics new drugs of abuse. In Proceedings of the American Academy of Addiction Psychiatry (AAAP) 24th Annual Meeting & Symposium, Scottsdale, AZ, USA, 7 December 2013. Abstract 16. [Google Scholar]
- Heilbronn, C.; Lloyd, B.; McElwee, P.; Eade, A.; Lubman, D.E. Trends in quetiapine use and non-fatal quetiapine-related ambulance attendances. Drug Alcohol Rev. 2013, 32, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.E.; Albright, V.; Yoon, J.; Council, C.L. Emergency Department Visits Involving Misuse and Abuse of the Antipsychotic Quetiapine: Results from the Drug Abuse Warning Network (DAWN). Subst. Abuse 2015, 9, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Klein, L.; Bang, S.; Cole, J.B. Intentional Recreational Abuse of Quetiapine Compared to Other Second-generation Antipsychotics. West. J. Emerg. Med. 2017, 18, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Pinta, E.R.; Taylor, R.E. Letter to the editor. Quetiapine Addiction? Am. J. Psychiatry 2007, 164, 1. [Google Scholar] [CrossRef] [PubMed]
- McLarnon, M.E.; Fulton, H.G.; MacIsaac, C.; Barrett, S.P. Characteristics of quetiapine misuse among clients of a community-based methadone maintenance program. J. Clin. Psychopharmacol. 2012, 32, 721–723. [Google Scholar] [CrossRef] [PubMed]
- Malekshahi, T.; Tioleco, N.; Ahmed, N.; Campbell, A.N.; Haller, D. Misuse of atypical antipsychotics in conjunction with alcohol and other drugs of abuse. J. Subst. Abuse Treat. 2015, 48, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Cha, H.J.; Lee, H.A.; Ahn, J.I.; Jeon, S.H.; Kim, E.J.; Jeong, H.S. Dependence potential of quetiapine: Behavioral pharmacology in rodents. Biomol. Ther. 2013, 21, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Tanda, G.; Valentini, V.; De Luca, M.A.; Perra, V.; Serra, G.P.; Di Chiara, G. A systematic microdialysis study of DA transmission in the accumbens shell/core and prefrontal cortex after acute antipsychotics. Psychopharmacology 2015, 232, 1427–1440. [Google Scholar] [CrossRef]
- Brutcher, R.E.; Nader, S.H.; Nader, M.A. Evaluation of the reinforcing effect of Quetiapine, alone and in combination with cocaine, in Rhesus monkeys. J. Pharmacol. Exp. Ther. 2016, 356, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S.; Seeman, P. Antipsychotic agents differ in how fast they come off the DA D2 receptors. Implications for atypical antipsychotic action. J. Psychiatry Neurosci. 2000, 25, 161–166. [Google Scholar] [PubMed]
- Tauscher, J.; Hussain, T.; Agid, O.; Verhoeff, N.P.; Wilson, A.A.; Houle, S.; Remington, G.; Zipursky, L.P.; Kapur, S. Equivalent occupancy of DA D1 and D2 receptors with clozapine: Differentiation from other atypical antipsychotics. Am. J. Psychiatry 2004, 161, 1620–1625. [Google Scholar] [CrossRef] [PubMed]
- Kuroki, T.; Nagao, N.; Nakahara, T. Neuropharmacology of second-generation antipsychotic drugs: A validity of the serotonin-DA hypothesis. Prog. Brain Res. 2008, 172, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S.; Remington, G. Atypical antipsychotics: New directions and new challenges in the treatment of schizophrenia. Ann. Rev. Med. 2001, 52, 503–517. [Google Scholar] [CrossRef] [PubMed]
- Montebello, M.E.; Brett, J. Misuse and Associated Harms of Quetiapine and Other Atypical Antipsychotics. Curr. Top. Behav. Neurosci. 2017, 34, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Navailles, S.; De Deurwaerdère, P. Presynaptic control of serotonin on striatal DA function. Psychopharmacology 2011, 213, 213–242. [Google Scholar] [CrossRef] [PubMed]
- Kotagale, N.R.; Mendhi, S.M.; Aglawe, M.M.; Umekar, M.J.; Taksande, B.G. Evidences for the involvement of sigma receptors in antidepressant-like effect of quetiapine in mice. Eur. J. Pharmacol. 2013, 702, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Yasui, Y.; Su, T.P. Potential Molecular Mechanisms on the Role of the Sigma-1 Receptor in the Action of Cocaine and Methamphetamine. J. Drug Alcohol Res. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, K. Quetiapine abuse and dependence: Is pharmacokinetics important? Acta Clin. Belg. 2017, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Dahr, R.; Sidana, A.; Singh, T. Olanzapine Dependence. Ger. J. Psychiatry 2010, 13, 51–53. [Google Scholar]
- Valeriani, G.; Corazza, O.; Bersani, F.S.; Melcore, C.; Metastasio, A.; Bersani, G.; Schifano, F. Olanzapine as the ideal “trip terminator”? Analysis of online reports relating to antipsychotics’ use and misuse following occurrence of novel psychoactive substance-related psychotic symptoms. Hum. Psychopharmacol. 2015, 30, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Reeves, R.R. Abuse of olanzapine by substance abusers. J. Psychoact. Drugs 2007, 39, 297–299. [Google Scholar] [CrossRef] [PubMed]
- Kumsar, N.A.; Erol, A. Olanzapine abuse. Subst. Abuse 2013, 34, 73–74. [Google Scholar] [CrossRef] [PubMed]
- James, P.D.; Fida, A.S.; Konovalov, P.; Smyth, B.P. Non-medical use of olanzapine by people on methadone treatment. BJPsych Bull. 2016, 40, 314–317. [Google Scholar] [CrossRef] [PubMed]
- Skilbeck, K.J.; O’Reilly, J.N.; Johnston, G.A.; Hinton, T. The effects of antipsychotic drugs on GABAA receptor binding depend on period of drug treatment and binding site examined. Schizophr. Res. 2007, 90, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Egerton, A.; Ahmad, R.; Hirani, E.; Grasby, P.M. Modulation of striatal DA release by 5-HT2A and 5-HT2C receptor antagonists: [11C]raclopride PET studies in the rat. Psychopharmacology 2008, 200, 487–496. [Google Scholar] [CrossRef] [PubMed]
- National Health Service (NHS) Prescription Cost Analysis (PCA) Data. 2016. Available online: http://www.nhsbsa.nhs.uk/PrescriptionServices/3494.aspx (accessed on 11 July 2017).
- Medicines and Health Regulatory Agency (MHRA). Drug Analysis Profiles. The Yellow Card Scheme. 2016. Available online: Https://yellowcard.mhra.gov.uk/the-yellow-card-scheme/ (accessed on 11 July 2017).
- Frauger, E.; Pochard, L.; Boucherie, Q.; Chevallier, C.; Daveluy, A.; Gibaja, V.; Caous, A.S.; Eiden, C.; Authier, N.; Le Boisselier, R.; et al. Le Réseau français d’addictovigilance. Surveillance system on drug abuse: Interest of the French national OPPIDUM program of French addictovigilance network. Therapie 2017. [Google Scholar] [CrossRef] [PubMed]
- Cerovecki, A.; Musil, R.; Klimke, A.; Seemüller, F.; Haen, E.; Schennach, R.; Kühn, K.U.; Volz, H.P.; Riedel, M. Withdrawal symptoms and rebound syndromes associated with switching and discontinuing atypical antipsychotics: Theoretical background and practical recommendations. CNS Drugs 2013, 27, 545–572. [Google Scholar] [CrossRef] [PubMed]
- Parker, D.R.; McIntyre, I.M. Case studies of postmortem quetiapine: Therapeutic or toxic concentrations? J. Anal. Toxicol. 2005, 29, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Skov, L.; Johansen, S.S.; Linnet, K. Postmortem Quetiapine Reference Concentrations in Brain and Blood. J. Anal. Toxicol. 2015, 39, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Vance, C.; McIntyre, I.M. Postmortem Tissue Concentrations of Olanzapine. J. Anal. Toxicol. 2009, 33, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Aspirin/paracetamol/quetiapine overdose. Available online: https://doi.org/10.1007/s40278-018-40658-z (accessed on 21 April 2018).
- Quetiapine/trazodone overdose. Available online: https://doi.org/10.1007/s40278-018-40528-4 (accessed on 21 April 2018).
- McVeigh, J.; Evans-Brown, M.; Bellis, M.A. Human enhancement drugs and the pursuit of perfection. Adicciones 2012, 24, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Corazza, O.; Bersani, F.S.; Brunoro, R.; Valeriani, G.; Martinotti, G.; Schifano, F. The diffusion of Performance and Image-Enhancing Drugs (IPEDs) on the Internet: The Abuse of the Cognitive Enhancer Piracetam. Subst. Use Misuse 2014, 49, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Sagoe, D.; McVeigh, J.; Bjørnebekk, A.; Essilfie, M.; Schou Andreassen, C.; Pallesen, S. Polypharmacy among anabolic-androgenic steroid users: A descriptive metasynthesis. Subst. Abuse Treat. Prev. Policy 2015, 10, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennan, R.; Wells, J.S.G.; Van Hout, M.C. The injecting use of image and performance-enhancing drugs (IPED) in the general population: A systematic review. Health Soc. Care Community 2017, 25, 1459–1531. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, M.C.; Kean, J. An exploratory study of image and performance enhancement drug use in a male British South Asian community. Int. J. Drug Policy 2015, 26, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Rowe, R.; Berger, I.; Yaseen, B.; Copeland, J. Risk and blood-borne virus testing among men who inject image and performance enhancing drugs, Sydney, Australia. Drug Alcohol Rev. 2017, 36, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Van de Ven, K.; Koenraadt, R. Exploring the relationship between online buyers and sellers of image and performance enhancing drugs (IPEDs): Quality issues, trust and self-regulation. Int. J. Drug Policy 2017, 50, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Albertson, T.E.; Chenoweth, J.A.; Colby, D.K.; Sutter, M.E. The Changing Drug Culture: Use and Misuse of Appearance- and Performance-Enhancing Drugs. FP Essent. 2016, 441, 30–43. [Google Scholar] [PubMed]
- Cassidy, E.M.; O’Halloran, D.J.; Barry, S. Insulin as a substance of misuse in a patient with insulin dependent diabetes mellitus. BMJ 1999, 319, 1417–1418. [Google Scholar] [CrossRef] [PubMed]
- World Anti-Doping Agency (WADA). The Prohibited List 2017. Available online: https://www.wada-ama.org/sites/default/files/resources/files/2016-09-29_-_wada_prohibited_list_2017_eng_final.pdf (accessed on 24 January 2018).
- Grimmer, N.M.; Gimbar, R.P.; Bursua, A.; Patel, M. Rhabdomyolysis Secondary to Clenbuterol Use and Exercise. J. Emerg. Med. 2016, 50, e71–e74. [Google Scholar] [CrossRef] [PubMed]
- Mottram, D.R.; Chester, N. Drugs in Sports, 6th ed.; Routledge: Abington-on-Thames, UK, 2014; ISBN 9780415715287. [Google Scholar]
- Quinley, K.E.; Chen, H.Y.; Yang, H.S.; Lynch, K.L.; Olson, K.R. Clenbuterol causing non-ST-segment elevation myocardial infarction in a teenage female desiring to lose weight: Case and brief literature review. Am. J. Emerg. Med. 2016, 34, 1739. [Google Scholar] [CrossRef] [PubMed]
- Al-Majed, A.A.; Khalil, N.Y.; Khbrani, I.; Abdel-Aziz, H.A. Clenbuterol Hydrochloride. Profiles Drug Subst. Excip. Relat. Methodol. 2017, 42, 91–123. [Google Scholar] [CrossRef] [PubMed]
- Spiller, H.A.; James, K.J.; Scholzen, S.; Borys, D.J. A descriptive study of adverse events from clenbuterol misuse and abuse for weight loss and bodybuilding. Subst. Abuse 2013, 34, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Howard, R. The Size Zero Pill. Available online: http://www.dailymail.co.uk/femail/article-409347/The-size-zero-pill.html (accessed on 13 November 2017).
- Steroidal.com. Clenbuterol Dosage. Available online: Https://www.steroidal.com/fat-loss-agents/clenbuterol/clenbuterol-dosage/ (accessed on 2 November 2017).
- Brett, J.; Dawson, A.H.; Brown, J.A. Clenbuterol toxicity: A NSW poisons information centre experience. Med. J. Aust. 2014, 200, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Van der Bijl, P.; Tutelyan, V.A. Dietary supplements containing prohibited substances. Vopr. Pitan 2013, 82, 6–13. [Google Scholar] [PubMed]
- Solimini, R.; Rotolo, M.C.; Pellegrini, M.; Minutillo, A.; Pacifici, R.; Busardò, F.P.; Zaami, S. Adulteration Practices of Psychoactive Illicit Drugs: An Updated Review. Curr. Pharm. Biotechnol. 2017, 18, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Barry, A.R.; Graham, M.M. Case report and review of clenbuterol cardiac toxicity. J. Cardiol. Cases 2013, 8, 131–133. [Google Scholar] [CrossRef]
- Huckins, D.S.; Lemons, M.F. Myocardial ischemia associated with clenbuterol abuse: Report of two cases. J. Emerg. Med. 2013, 44, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Daubert, G.P.; Mabasa, V.H.; Leung, V.W.; Aaron, C. Acute clenbuterol overdose resulting in supraventricular tachycardia and atrial fibrillation. J. Med. Toxicol. 2007, 3, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Ferrua, S.; Varbella, F.; Conte, M.R. Acute myocardial infarction due to coronary vasospasm and salbutamol abuse. Heart 2009, 95, 673. [Google Scholar] [CrossRef] [PubMed]
- Patanè, S.; Marte, F.; La Rosa, F.C.; La Rocca, R. Atrial fibrillation associated with chocolate intake abuse and chronic salbutamol inhalation abuse. Int. J. Cardiol. 2010, 145, e74–e76. [Google Scholar] [CrossRef] [PubMed]
- Boucher, A.; Payen, C.; Garayt, C.; Ibanez, H.; Dieny, A.; Doche, C.; Chuniaud, C.; Descotes, J. Salbutamol misuse or abuse with fatal outcome: A case report. Hum. Exp. Toxicol. 2011, 30, 1869–1871. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, J.M. Effects of clenbuterol and prenalterol on performance during differential reinforcement of low response rate in the rat. J. Pharmacol. Exp. Ther. 1987, 241, 68–75. [Google Scholar] [PubMed]
- Edwards, J.G.; Holgate, S.T. Dependency upon salbutamol inhalers. Br. J. Psychiatry 1979, 134, 624–626. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.J.; Paull, J.D.; Richmond, B.H.; Wilson-Evered, E.; Ziccone, S.P. Pharmacokinetics of intravenous and oral salbutamol and its sulphate conjugate. Br. J. Clin. Pharmacol. 1986, 22, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Pope, H.G.; Wood, R.I.; Rogol, A.; Nyberg, F.; Bowers, L.; Bhasin, S. Adverse health consequences of performance-enhancing drugs: An Endocrine Society scientific statement. Endocr. Rev. 2013, 35, 341–375. [Google Scholar] [CrossRef] [PubMed]
- Lewis, L.D.; Essex, E.; Volans, G.N.; Cochrane, G.M. A study of self- poisoning with oral salbutamol-laboratory and clinical features. Hum. Exp. Toxicol. 1993, 12, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Nicoli, R.; Petrou, M.; Badoud, F.; Dvorak, J.; Saugy, M.; Baume, N. Quantification of clenbuterol at trace level in human urine by ultra-high pressure liquid chromatography-tandem mass spectrometry. J. Chromatogr. A 2013, 1292, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Vaso, M.; Weber, A.; Tscholl, P.M.; Junge, A.; Dvorak, J. Use and abuse of medication during 2014 FIFA World Cup Brazil: A retrospective survey. BMJ Open 2015, 5, E007608. [Google Scholar] [CrossRef] [PubMed]
- EMA. Buying Medicine Online. Available online: http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000630.jsp&mid=WC0b01ac05808fd210 (accessed on 11 November 2017).
- Miller, H.; Panahi, L.; Tapia, D.; Tran, A.; Bowman, J.D. Loperamide misuse and abuse. J. Am. Pharm. Assoc. 2017, 57, S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Daniulaityte, R.; Carlson, R.; Falck, R.; Cameron, D.; Perera, S.; Chen, L.; Sheth, A. “I just wanted to tell you that loperamide WILL WORK”: A web-based study of the extra-medical use of loperamide. Drug Alcohol Depend. 2013, 130, 241–244. [Google Scholar] [CrossRef] [PubMed]
- Grey Pages: The Merits of High Dose Loperamide for Opiate Withdrawal. Available online: http://derekwmeyer.blogspot.com/2012/03/merits-of-high-dose-loperamide-for.html (accessed on 30 November 2017).
- Finch, M. How to Use Loperamide for Opiate Withdrawal. 2015. Available online: http://opiateaddictionsupport.com/how-to-use-loperamidefor-opiate-withdrawal/ (accessed on 30 November 2017).
- Levine, D.A. “Pharming”: The abuse of prescription and over-the-counter drugs in teens. Curr. Opin. Pediatr. 2007, 19, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.J. Over the counter medicine abuse—A review of the literature. J. Subst. Use 2013, 18, 82–107. [Google Scholar] [CrossRef] [PubMed]
- Fox, N.; Ward, K.; O’Rourke, A. The birth of the e-clinic. Continuity or transformation in the UK governance of pharmaceutical consumption? Soc. Sci. Med. 2005, 61, 1474–1484. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L. Prescription drug abuse: What is being done to address this new drug epidemic? Testimony before the Subcommittee on Criminal Justice, Drug Policy and Human Resources. Pain Physician 2006, 9, 287–321. [Google Scholar] [PubMed]
- National Association of Board of Pharmacy (NABP). Buying Medicine Online. Available online: https://nabp.pharmacy/initiatives/dot-pharmacy/buying-medicine-online/ (accessed on 11 November 2017).
- Food and Drug Administration (FDA) Imodium Label. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/017690s005lbl.pdf (accessed on 28 January 2018).
- Baker, D.E. Loperamide: A pharmacological review. Rev. Gastroenterol. Disord. 2007, 7 (Suppl. 3), S11-8. [Google Scholar] [PubMed]
- Jaffe, J.H.; Kanzler, M.; Green, J. Abuse potential of loperamide. Clin. Pharmacol. Ther. 1980, 28, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Wightman, R.S.; Hoffman, R.S.; Howland, M.A.; Rice, B.; Binary, R.; Lugassy, D. Not your regular high: Cardiac dysrhythmias caused by loperamide. Clin. Toxicol. 2016, 54, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Borron, S.W.; Watts, S.H.; Tull, J.; Baeza, S.; Diebold, S.; Barrow, A. Misuse and Abuse of Loperamide: A New Look at a Drug with “Low Abuse Potential”. J. Emerg. Med. 2017, 53, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Marraffa, J.M.; Holland, M.G.; Sullivan, R.W.; Morgan, B.W.; Oakes, J.A.; Wiegand, T.J.; Hodgman, M.J. Cardiac conduction disturbance after loperamide abuse. Clin. Toxicol. 2014, 52, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration (FDA) Drug Safety Communications. FDA Warns about Serious Heart Problems with High Doses of the Anti-Diarrheal Medicine Loperamide (Imodium), Including from Abuse and Misuse. Safety Announcement. 6 July 2016. Available online: https://www.fda.gov/Drugs/DrugSafety/ucm504617.htm (accessed on 22 November 2017).
- New York Times. Addicts Who Can’t Find Painkillers Turn to Anti-Diarrhea Drugs. 10 May 2016. Available online: https://www.nytimes.com/2016/05/11/health/imodium-opioid-addiction.html?_r=0. (accessed on 24 November 2017).
- Stanciu, C.N.; Gnanasegaram, S.A. Loperamide, the “Poor Man’s Methadone”: Brief Review. J. Psychoact. Drugs 2017, 49, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Eggleston, W.; Marraffa, J.M.; Stork, C.M.; Mercurio-Zappala, M.; Su, M.K.; Wightman, R.S.; Cummings, K.R.; Schier, J.G. Notes from the Field: Cardiac Dysrhythmias after Loperamide Abuse—New York, 2008–2016. MMWR Morb. Mortal Wkly. Rep. 2016, 65, 1276–1277. [Google Scholar] [CrossRef] [PubMed]
- Eggleston, W.; Clark, K.H.; Marraffa, J.M. Loperamide Abuse Associated With Cardiac Dysrhythmia and Death. Ann. Emerg. Med. 2017, 69, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Bhatti, Z.; Norsworthy, J.; Szombathy, T. Loperamide metabolite-induced cardiomyopathy and QTc prolongation. Clin. Toxicol. 2017, 55, 659–661. [Google Scholar] [CrossRef] [PubMed]
- Kozak, P.M.; Harris, A.E.; McPherson, J.A.; Roden, D.M. Torsades de pointes with high-dose loperamide. J. Electrocardiol. 2017, 50, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.E.; Juurlink, D.N. Clinical Review: Loperamide Toxicity. Ann. Emerg. Med. 2017, 70, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Bishop-Freeman, S.C.; Feaster, M.S.; Beal, J.; Miller, A.; Hargrove, R.L.; Brower, J.O.; Winecker, R.E. Loperamide-Related Deaths in North Carolina. J. Anal. Toxicol. 2016, 40, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Swank, K.A.; Wu, E.; Kortepeter, C.; McAninch, J.; Levin, R.L. Adverse event detection using the FDA post-marketing drug safety surveillance system: Cardiotoxicity associated with loperamide abuse and misuse. J. Am. Pharm. Assoc. 2017, 57, S63–S67. [Google Scholar] [CrossRef] [PubMed]
- Church, J.; Fletcher, E.J.; Abdel-Hamid, K.; MacDonald, J. Loperamide blocks high-voltage-activated calcium channels and N-methyl-D-aspartate-evoked responses in rat and mouse cultured hippocampal pyramidal neurons. Mol. Pharmacol. 1994, 45, 747–757. [Google Scholar] [PubMed]
- Nozaki-Taguchi, N.; Yaksh, T.L. Characterization of the antihyperalgesic action of a novel peripheral mu-opioid receptor agonist- loperamide. Anesthesiology 1999, 90, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Compton, D.R.; Vaz, R.J.; Rampe, D. Proarrhythmic mechanisms of the common anti-diarrheal medication loperamide: Revelations from the opioid abuse epidemic. Naunyn Schmiedebergs Arch. Pharmacol. 2016, 389, 1133–1137. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Lim, L.Y.; Chowbay, B. Herbal modulation of P-glycoprotein. Drug Metab. Rev. 2004, 36, 57–104. [Google Scholar] [CrossRef] [PubMed]
- Loperamide + Black Pepper Exctract = Feeling Really Nice. Available online: www.erowid.com (accessed on 3 January 2018).
- Corazza, O.; Assi, S.; Simonato, P.; Corkery, J.M.; Bersani, F.S.; Demetrovics, Z.; Stair, J.; Fergus, S.; Pezzolesi, C.; Pasinetti, M.; et al. Promoting innovation and excellence to face the rapid diffusion of novel psychoactive substances in the EU: The outcomes of the ReDNet project. Hum. Psychopharmacol. 2013, 28, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Larsen, T.R.; McMunn, J.; Ahmad, H.; AlMahameed, S.T. Ventricular Tachycardia Triggered by Loperamide and Famotidine Abuse. Drug Saf. Case Rep. 2018, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Sehring, M.; Chambers, J. Letter to the editor. Loperamide abuse and cardiotoxicity. J. Community Hosp. Intern. Med. Perspect. 2017, 7, 275. [Google Scholar] [CrossRef]
- Orsolini, L.; Papanti, G.D.; Francesconi, G.; Schifano, F. Mind navigators of chemicals’ experimenters? A web-based description of e-psychonauts. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Johanson, C.E.; Balster, R.L.; Henningfield, J.E.; Schuster, C.R.; Anthony, J.C.; Barthwell, A.G.; Coleman, J.J.; Dart, R.C.; Gorodetzky, C.W.; O’Keeffe, C.; et al. Risk management post-marketing surveillance for the abuse of medications acting on the central nervous system: Expert panel report. Drug Alcohol Depend. 2009, 105 (Suppl. 1), S65–S71. [Google Scholar] [CrossRef] [PubMed]
- Mackey, T.K.; Nayyar, G. Digital danger: A review of the global public health, patient safety and cybersecurity threats posed by illicit online pharmacies. Br. Med. Bull. 2016, 118, 110–126. [Google Scholar] [CrossRef] [PubMed]
- McColl, S.; Sellers, E.M. Research design strategies to evaluate the impact of formulations on abuse liability. Drug Alcohol Depend. 2006, 83 (Suppl. 1), S52–S62. [Google Scholar] [CrossRef] [PubMed]
- FDA’s Role in Preventing Prescription Drug Abuse. Statement of Robert J. Meyer, M.D. before the House Committee on Government Reform, September 13, 2005. Available online: http://www.fda.gov/NewsEvents/Testimony/ucm112718.htm (accessed on 30 November 2017).
- Schifano, F.; Papanti, G.D.; Orsolini, L.; Corkery, J.M. The consequences of drug misuse on post-marketing surveillance. Exp. Rev. Clin. Pharmacol. 2016, 9, 867–871. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schifano, F.; Chiappini, S.; Corkery, J.M.; Guirguis, A. Abuse of Prescription Drugs in the Context of Novel Psychoactive Substances (NPS): A Systematic Review. Brain Sci. 2018, 8, 73. https://doi.org/10.3390/brainsci8040073
Schifano F, Chiappini S, Corkery JM, Guirguis A. Abuse of Prescription Drugs in the Context of Novel Psychoactive Substances (NPS): A Systematic Review. Brain Sciences. 2018; 8(4):73. https://doi.org/10.3390/brainsci8040073
Chicago/Turabian StyleSchifano, Fabrizio, Stefania Chiappini, John M. Corkery, and Amira Guirguis. 2018. "Abuse of Prescription Drugs in the Context of Novel Psychoactive Substances (NPS): A Systematic Review" Brain Sciences 8, no. 4: 73. https://doi.org/10.3390/brainsci8040073





