Antioxidant and Anti-Hepatitis C Viral Activities of Commercial Milk Thistle Food Supplements
Abstract
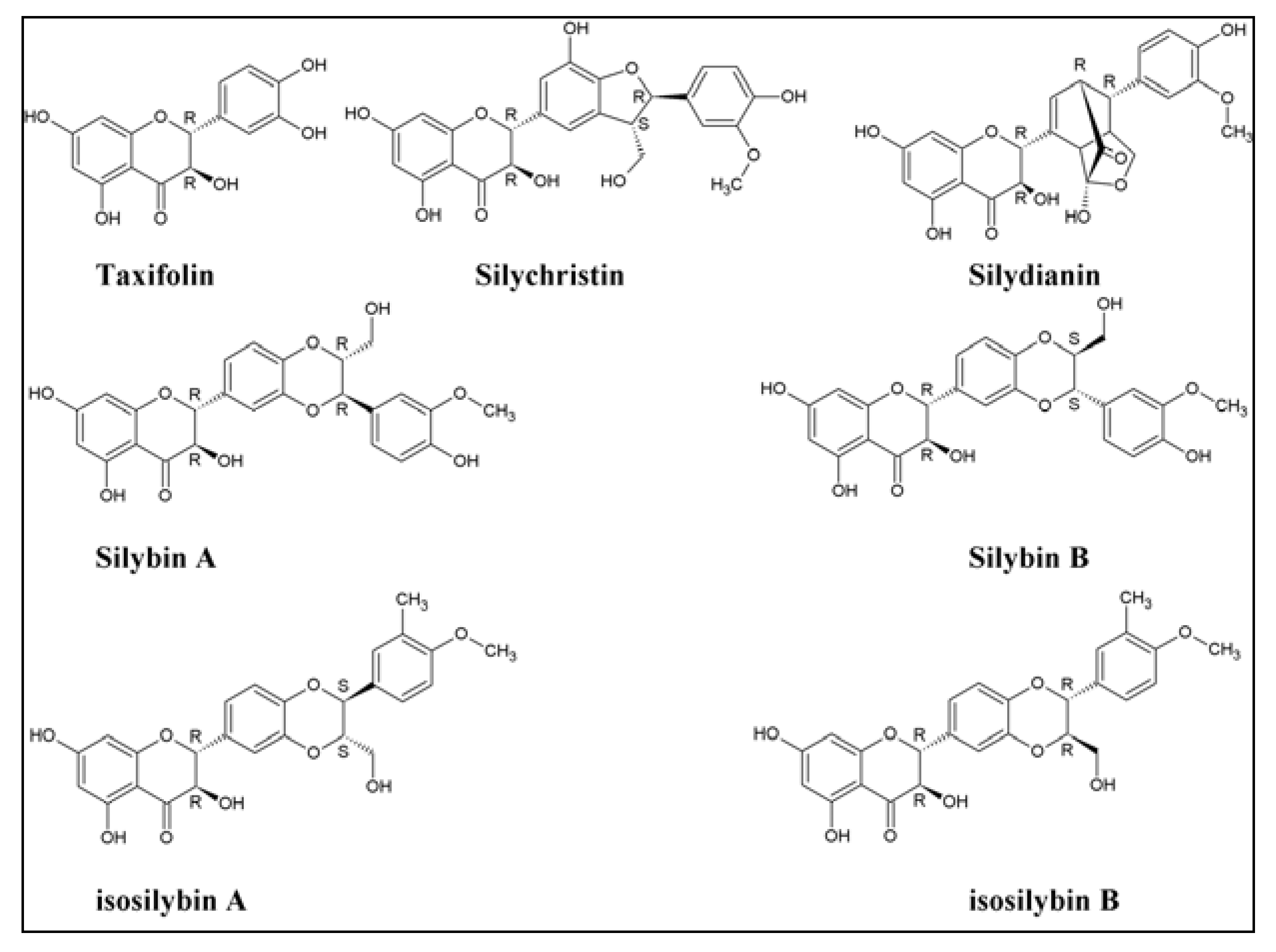
:1. Introduction
2. Experimental Section
2.1. Chemicals and Reagents
| Sample ID/Description/Sources & Average weight of each tablet | Sample ID/Description/Sources & Average weight of each tablet | ||
|---|---|---|---|
| 1 | Swanson Superior Herbs® | 24 | Nature’s Bounty®/Natural Whole Herbs |
| Milk Thistle 80% Silymarin/USA (0.5504 g/tablet) | Milk Thistle 1000 mg/USA (0.3939 g/tablet) | ||
| 2 | Ortho Molecular Products® | 25 | Legalon® 140 Silymarin Egypt/Germany (0.3939 g/tablet) |
| Silymarin Forte/USA (0.4502 g/tablet) | |||
| 3 | Metabolic Response Modifiers® | 26 | Hepatic Forte® |
| Silymarin with Bio Sorb/USA (0.4975 g/tablet) | Silymarin/Egypt (0.7944 g/tablet) | ||
| 4 | Advance Physician Formulas® (0.3319 g/tablet) | 27 | Levatech® |
| Milk Thistle (Standardize Silymarin 80%)/USA | Silymarin/Egypt (0.4569 g/tablet) | ||
| 5 | Pure Encapsulations® (0.2430 g/tablet) | 28 | Livit® (1.3158 g/tablet) |
| Silymarin Milk Thistle Extract/USA | Liver support, Soft gelatin capsules/Egypt | ||
| 6 | Thorne Research T.A.P.S® | 29 | Liverin® (0.6589 g/tablet) |
| Dietary Supplement/USA (0.6789 g/tablet) | Improvement of liver function/Egypt | ||
| 7 | Metagenics® | 30 | Levatone® |
| Silymarin 80/USA (0.2450 g/tablet) | Food Supplement/Egypt (1.2484 g/tablet) | ||
| 8 | Himalaya Liver Care® | 31 | Liver Albumin Plus® (0.9610 g/tablet) |
| Liv.52/USA (0.3768 g/tablet) | Dietary Supplement/Egypt | ||
| 9 | Jarrow Formulas®/USA (0.2786 g/tablet) | 32 | Hipamax Plus® (1.5340 g/tablet) |
| Milk Thistle (Standardize Silymarin Extract 30:1) | Dietary Supplement/Egypt | ||
| 10 | Metabolic Maintenance® | 33 | SEDICO® (13597 g/tablet) |
| Silymarin/USA (0.5696 g/tablet) | Silymarin Plus, Dietary Supplement/Egypt | ||
| 11 | Life Extension® (0.9040 g/tablet) | 34 | Hepaticum® (0.4228 g/tablet) |
| Mega Silymarin with isosilybin B/USA | Cyclodextrin enhanced formula/Egypt | ||
| 12 | Purintin’s Pride® | 35 | Silipex® (0.3351 g/tablet) |
| Silymarin Milk Thistle/USA (0.3466 g/tablet) | Dietary Supplement /Egypt | ||
| 13 | Natural Wellness®/USA (0.5063 g/tablet) Maximum Milk Thistle, Silybin Phytosome 240 mg | 36 | MEPACURE® (0.3907 g/tablet) |
| Liver support /Egypt | |||
| 14 | Enzymatic Therapy® | 37 | Hepanox® Cap. (1.3371 g/tablet) |
| Super Milk Thistle/USA (0.3262 g/tablet) | Napha food support/Egypt | ||
| 15 | Advanced Beta Glucon Therapy® (0.4867 g/tablet) | 38 | SELECTIVAL® (1.2695 g/tablet) |
| Bio-Silymarin, Aloha Medicinal Inc./USA | Dietary Supplement/Egypt | ||
| 16 | Futurebiotics® | 39 | Ursoplus® MINAPHARM |
| Silymarin Plus/USA (1.0514 g/tablet) | Silymarin 70%/Egypt (0.5625 g/tablet) | ||
| 17 | Planetary Herbals® (0.7060 g/tablet) | 40 | Leaglon® 70 Silymarin/Egypt/Germany (0.4259 g/tablet) |
| Full Spectrum Silymarin 80™/USA | |||
| 18 | Wonder Laboratories® Advanced B-12 Sublingual/USA (0.3443 g/tablet) | 41 | Hepamarin® 140mg |
| Hepatoprotective/Egypt (0.3124 g/tablet) | |||
| 19 | 21st Century® (0.4508 g/tablet) | 42 | Trade Mark® (0.0518 g/tablet) |
| 200 count Milk Thistle Extract/USA | Biphenyldicarboxylate/China/Egypt | ||
| 20 | Source Naturals® | 43 | MEPASIL® (0.5075 g/tablet) |
| Silymarin Plus/USA (0.9847 g/tablet) | Silymarin, Liver support/Egypt | ||
| 21 | Now® | 44 | MARIAGON® (0.4775 g/tablet) |
| Silymarin 100 V caps/USA (0.5090 g/tablet) | Hepatoprotective/Egypt | ||
| 22 | Good’N Natural® Milk Thistle Extract 250 mg/USA(0.6765 g/tablet) | 45 | Hepato-Forte® (1.2624 g/tablet) |
| Liver Supplement/Egypt | |||
| 23 | TwinLab® | ||
| Silymarin/USA (0.1610 g/tablet) | |||
2.2. Cells
2.3. Preparation of Samples
2.4. Determination of Total Silymarin
2.5. Free Radical-Scavenging Activity: DPPH Test
2.6. Trolox-Equivalent Antioxidant Capacity Assay
2.7. Anti HCV Bioassay
2.8. Cytotoxicity Assay
2.9. RNA Isolation and RTqPCR Analysis
2.10. Statistical Analysis
3. Results and Discussion
3.1. Determination of Total Silymarin

| ID | Total Silymarin mg/gram tablet | Antioxidant Activity | Anti-HCV activity | |
|---|---|---|---|---|
| DPPH | Trolox Equivalent mmol/g | % inhibition | ||
| EC50μg/mL | (100 μg of tablet/mL) | |||
| 1 | 366.7 ± 0.8 | 1.08 ± 0.02 | 9.0 ± 0.1 | 84 ± 8 |
| 2 | 478.5 ± 1.1 | 0.98 ± 0.02 | 9.3 ± 0.3 | 50 ± 4 |
| 3 | 107.0 ± 0.5 | 2.97 ± 0.02 | 5.3 ± 0.2 | 45 ± 21 |
| 4 | 467.4 ± 1.1 | 1.00 ± 0.00 | 8.9 ± 0.5 | 60 ± 20 |
| 5 | 849.9 ± 0.8 | 0.45 ± 0.00 | 9.0 ± 0.7 | 85 ± 5 |
| 6 | 57.8 ± 0.9 | 0.98 ± 0.13 | 4.1 ± 2.2 | 16 ± 16 |
| 7 | 326.0 ± 1.0 | 2.00 ± 0.00 | 7.7 ± 0.8 | 62 ± 14 |
| 8 | Not detected | 0.20 ± 0.00 | 9.5 ± 0.5 | 24 ± 23 |
| 9 | 467.8 ± 1.9 | 1.03 ± 0.02 | 8.7 ± 0.4 | 39 ± 7 |
| 10 | 568.3 ± 1.7 | 0.92 ± 0.02 | 9.2 ± 0.4 | 70 ± 8 |
| 11 | 848.7 ± 1.1 | 0.25 ± 0.01 | 9.1 ± 0.5 | 76 ± 11 |
| 12 | 67.7 ± 0.4 | 4.40 ± 0.00 | 3.4 ± 0.5 | 30 ± 5 |
| 13 | 162.4 ± 0.5 | 6.13 ± 0.09 | 4.8 ± 0.7 | 38 ± 22 |
| 14 | 75.0 ± 0.2 | 1.20 ± 0.00 | 5.8 ± 0.9 | 18 ± 2 |
| 15 | 685.1 ± 3.3 | 0.30 ± 0.00 | 9.4 ± 0.4 | 72 ± 2 |
| 16 | 81.2 ± 0.3 | 2.37 ± 0.12 | 4.0 ± 0.3 | 39 ± 25 |
| 17 | 314.9 ± 0.5 | 1.08 ± 0.02 | 8.3 ± 0.5 | 72 ± 1 |
| 18 | 82.4 ± 0.3 | 3.03 ± 0.05 | 6.6 ± 1.4 | 20 ± 17 |
| 19 | 109.5 ± 0.9 | 2.17 ± 0.05 | 7.6 ± 1.5 | 81 ± 4 |
| 20 | 248.5 ± 0.1 | 1.00 ± 0.00 | 7.5 ± 0.6 | 88 ± 8 |
| 21 | 341.9 ± 0.5 | 0.90 ± 0.00 | 8.9 ± 0.5 | 81 ± 4 |
| 22 | 276.8 ± 1.1 | 1.20 ± 0.00 | 7.7 ± 0.1 | 80 ± 12 |
| 23 | 408.4 ± 0.4 | 1.10 ± 0.00 | 9.2 ± 0.1 | 81 ± 20 |
| 24 | 72.6 ± 0.4 | 4.23 ± 0.12 | 4.0 ± 0.8 | Not tested |
| 25 | 522.8 ± 0.9 | 0.95 ± 0.04 | 9.0 ± 0.2 | 62 ± 2 |
| 26 | 88.6 ± 0.3 | 3.13 ± 0.19 | 1.9 ± 1.2 | 35 ± 12 |
| 27 | 260.8 ± 0.4 | 1.20 ± 0.08 | 7.4 ± 0.3 | 51 ± 14 |
| 28 | 145.1 ± 0.1 | 2.80 ± 0.49 | 3.8 ± 1.0 | 17 ± 11 |
| 29 | Not detected | >10.00 | 0.0 | 42 ± 10 |
| 30 | 111.9 ± 0.1 | 2.27 ± 0.25 | 3.9 ± 1.4 | 10 ± 14 |
| 31 | 132.8 ± 0.1 | 4.08 ± 0.23 | 2.6 ± 1.1 | 14 ± 9 |
| 32 | 113.2 ± 0.3 | 3.87 ± 0.57 | 1.7 ± 0.9 | 47 ± 36 |
| 33 | 177.1 ± 0.1 | 0.31 ± 0.00 | 4.2 ± 0.7 | 24 ± 7 |
| 34 | 450.2 ± 0.6 | 1.10 ± 0.07 | 8.0 ± 1.1 | 35 ± 23 |
| 35 | 339.5 ± 0.2 | 0.95 ± 0.04 | 7.5 ± 1.0 | 48 ± 16 |
| 36 | 83.6 ± 0.5 | 2.17 ± 0.05 | 5.3 ± 0.8 | 26 ± 6 |
| 37 | 113.2 ± 0.1 | 1.18 ± 0.44 | 2.8 ± 0.9 | 33 ± 10 |
| 38 | 227.6 ± 0.1 | 2.07 ± 0.09 | 5.4 ± 0.7 | 37 ± 10 |
| 39 | 226.3 ± 0.3 | 1.67 ± 0.26 | 5.8 ± 0.8 | 46 ± 20 |
| 40 | 274.3 ± 0.5 | 2.13 ± 0.05 | 7.4 ± 0.5 | 46 ± 19 |
| 41 | 383.8 ± 0.3 | 1.03 ± 0.05 | 8.2 ± 0.8 | 42 ± 9 |
| 42 | Not detected | >10.00 | 0.0 | 15 ± 21 |
| 43 | 346.9 ± 0.9 | 1.13 ± 0.09 | 7.6 ± 1.3 | 45 ± 9 |
| 44 | 303.8 ± 0.6 | 1.15 ± 0.04 | 7.4 ± 0.9 | 21 ± 3 |
| 45 | Not detected | >10.00 | 0.0 | 28 ± 2 |
3.2. Free Radicals Scavenging Activity
3.3. Total Antioxidant Capacity as Trolox Equivalent (TEAC)
3.4. Anti HCV Activity

4. Conclusions
Acknowledgments
References
- Radimer, K.; Bindewald, B.; Hughes, J.; Ervin, B.; Swanson, C.; Picciano, M.F. Dietary supplement use by US adults: Data from the National Health and Nutrition Examination Survey, 1999–2000. Am. J. Epidemiol. 2004, 160, 339–349. [Google Scholar] [CrossRef]
- Qato, D.; Alexander, C.; Conti, R.; Johnson, M.; Schumm, P.; Lindau, S. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA 2008, 300, 2867–2878. [Google Scholar] [CrossRef]
- World Health Organization, The World Medicines Situation 2011—Traditional Medicines: Global Situation, Issues and Challenges; World Health Organization, 2011.
- Flora, K.; Hahn, M.; Rosen, H.; Benner, K. Milk thistle (Silybum marianum) for the therapy of liver disease. Am. J. Gastroenterol. 1998, 93, 139–143. [Google Scholar] [CrossRef]
- Mayer, K.; Myers, P.; Lee, S. Silymarin treatment of viral hepatitis: A systematic review. J. Viral Hepat. 2005, 12, 559–567. [Google Scholar] [CrossRef]
- Wellington, K.; Jarvis, B. Silymarin: A review of its clinical properties in the management of hepatic disorders. BioDrugs 2001, 15, 465–489. [Google Scholar] [CrossRef]
- Saller, R.; Meier, R.; Brignoli, R. The use of silymarin in the treatment of liver diseases. Drugs 2001, 61, 2035–2063. [Google Scholar] [CrossRef]
- Roy, S.; Gagan, G.; Agarwal, R. Silibinin prevents ultraviolet B radiation-induced epidermal damages in JB6 cells and mouse skin in a p53-GADD45α-dependent manner. Carcinogenesis 2012, 33, 629–636. [Google Scholar] [CrossRef]
- Chilampalli, S.; Zhang, X.; Fahmy, H.; Kaushik, R.; Zeman, D.; Hildreth, M.; Dwivedi, C. Chemopreventive effects of honokiol on UVB-induced skin. Anticancer Res. 2010, 30, 777–783. [Google Scholar] [PubMed]
- Bárcena, R.; Moreno, A.; Rodríguez-Gandía, M.; Albillos, A.; Arocena, C.; Blesa, C.; García-Hoz, F.; Graus, J.; Nuño, J.; López-Hervás, P.; et al. Safety and anti-HCV effect of prolonged intravenous silibinin in HCV-genotype 1 subjects in the immediate liver transplant period. J. Hepatol. 2012, in press. [Google Scholar]
- Mariño, Z.; Crespo, G.; D’Amato, M.; Brambilla, N.; Giacovelli, G.; Rovati, L.; Costa, J.; Navasa, M.; Forns, X. Intravenous silibinin monotherapy shows significant antiviral activity in HCV-infected patients in the peri-transplantation period. J. Hepatol. 2012, in press.. [Google Scholar]
- Biermer, M.; Schlosser, B.; Fülöp, B.; van Bömmel, F.; Brodzinski, A.; Heyne, R.; Keller, K.; Sarrazin, C.; Berg, T. High-dose silibinin rescue treatment for HCV-infected patients showing suboptimal virologic response to standard combination therapy. J. Viral Hepat. 2012, 19, 547–553. [Google Scholar] [CrossRef]
- Rutter, K.; Scherzer, T.; Beinhardt, S.; Kerschner, H.; Stättermayer, A.; Hofer, H.; Popow-Kraupp, T.; Steindl-Munda, P.; Ferenci, P. Intravenous silibinin as “rescue treatment” for on-treatment non-responders to pegylated interferon/ribavirin combination therapy. Antivir. Ther. 2011, 16, 1327–1333. [Google Scholar] [CrossRef]
- Payer, B.; Reiberger, T.; Rutter, K.; Beinhardt, S.; Staettermayer, A.; Peck-Radosavljevic, M.; Ferenci, P. Successful HCV eradication and inhibition of HIV replication by intravenous silibinin in an HIV-HCV coinfected patient. J. Clin. Virol. 2010, 49, 131–133. [Google Scholar] [CrossRef]
- Neumann, U.; Biermer, M.; Eurich, D.; Neuhaus, P.; Berg, T. Successful prevention of hepatitis C virus (HCV) liver graft reinfection by silibinin mono-therapy. J. Hepatol. 2010, 52, 951–952. [Google Scholar] [CrossRef]
- Ferenci, P.; Scherzer, T.; Kerschner, H.; Rutter, K.; Beinhardt, S.; Hofer, H.; Schöniger-Hekele, M.; Holzmann, H.; Steindl-Munda, P. Silibinin is a potent antiviral agent in patients with chronic hepatitis C not responding to pegylated interferon/ribavirin therapy. Gastroenterology 2008, 135, 1561–1567. [Google Scholar] [CrossRef]
- Wagoner, J.; Negash, A.; Kane, O.; Martinez, L.; Nahmias, Y.; Bourne, N.; Owen, D.; Grove, J.; Brimacombe, C.; McKeating, J.; et al. Multiple effects of silymarin on the hepatitis C virus lifecycle. Hepatology 2010, 51, 1912–1921. [Google Scholar] [CrossRef]
- Sy-Cordero, A.; Graf, T.; Nakanishi, Y.; Wani, M.; Agarwal, R.; Kroll, D.; Oberlies, N. Large scale isolation of flavonolignans from Silybum marianum (milk thistle) extract affords new minor constituents and preliminary structure-activity relationships. Planta Med. 2010, 76, 644–647. [Google Scholar] [CrossRef]
- Daniela, D.; Gažák, R.; Marhol, P.; Biedermann, D.; Purchartová, K.; Fedrigo, M.; Riva, S.; Křen, V. Enzymatic kinetic resolution of silybin diastereoisomers. J. Nat. Prod. 2010, 73, 613–619. [Google Scholar] [CrossRef]
- Křen, V.; Kubisch, J.; Sedmera, P.; Halada, P.; Přikrylová, V.; Jegorov, A.; Cvak, L.; Gebhardt, R.; Ulrichová, J.; Šimánek, V. Glycosylation of silybin. J. Chem. Soc. 1997, 2467–2474. [Google Scholar] [CrossRef]
- Liu, J.; Manheimer, E.; Tsutani, K.; Gluud, C. Medicinal herbs for hepatitis C virus infection: A Cochrane hepato-biliary systematic review of randomized trials. Am. J. Gastroenterol. 2003, 98, 538–544. [Google Scholar] [CrossRef]
- Hammouda, F.; Ismail, S.; Hassan, N.; Zaki, A.; Kamel, A.; Rimpler, H. Evaluation of the silymarin content in Silybum marianum (L.) Gaertn. Cultivated under different agricultural conditions. Phytother. Res. 1993, 7, 90–91. [Google Scholar] [CrossRef]
- Simanek, V.; Kren, V.; Ulrichova, J.; Vicar, J.; Cvak, L. Silymarin: What is in the name...? An appeal for a change of editorial policy. Hepatology 2000, 32, 442–444. [Google Scholar] [CrossRef]
- Farghaly, T.; Abdel Hafez, N.; Ragab, E.; Awad, H.; Abdalla, M. Synthesis, anti-HCV, antioxidant and peroxynitrite inhibitory activity of fused benzosuberone derivatives. Eur. J. Med. Chem. 2010, 45, 492–500. [Google Scholar] [CrossRef]
- Blight, K.; Kolykhalov, A.; Rice, C. Efficient initiation of HCV RNA replication in cell culture. Science 2000, 290, 1972–1974. [Google Scholar] [CrossRef]
- Zhong, J.; Gastaminza, P.; Cheng, G.; Kapadia, S.; Kato, T.; Burton, D.R.; Wieland, S.; Uprichard, S.; Wakita, T.; Chisari, F. Robust hepatitis C virus infection in vitro. Proc. Natl. Acad. Sci. USA 2005, 102, 9294–9299. [Google Scholar] [CrossRef] [PubMed]
- Anthony, K.; Saleh, M. Chemical profiling and antioxidant activity of commercial milk thistle food supplements. J. Chem. Pharm. Res. 2012, 4, 4440–4450. [Google Scholar]
- Brand-Williams, W.; Cuvelier, M.; Berset, C. Use of free radical method to evaluate antioxidant activity. Lebensm. Wiss. Technol. 1995, 28, 25–30. [Google Scholar] [CrossRef]
- Choi, S.; Sainz, J.; Corcoran, P.; Uprichard, S.; Jeong, H. Characterization of increased drug metabolism activity in dimethyl sulfoxide (DMSO)-treated Huh7 hepatoma cells. Xenobiotica 2009, 39, 205–217. [Google Scholar] [CrossRef]
- Yu, X.; Sainz, B.; Uprichard, S. Development of a cell-based hepatitis C virus infection fluorescent resonance energy transfer assay for high-throughput antiviral compound screening. Antimicrob. Agents Chemother. 2009, 53, 4311–4319. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Uprichard, S. Cell-based hepatitis C virus infection fluorescence resonance energy transfer (FRET) assay for antiviral compound screening. Curr. Protoc. Microbiol. 2010, 17, 17–25. [Google Scholar]
- Statistics SPSS Software, version 20, IBM Corporation: New York, NY, USA, 2011.
- Gutteridge, J. Free radicals in disease processes: A compilation of cause and consequence. Free Radic. Res. Commun. 1993, 19, 141–158. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Estilla, A.; Marrugo, O.; Trujillo-Murillo, K.; Pérez-Ibave, D.; Charles-Niño, C.; Pedroza-Roldan, C.; Ríos-Ibarra, C.; Ramírez-Valles, E.; Ortiz-López, R.; Islas-Carbajal, M.; et al. Cu/Zn superoxide dismutase (sod 1) induction is implicated in the antioxidative and antiviral activity of acetylsalicylic acid in HCV-expressing cells. Am. J. Physiol. Gastrointest. 2012, 22. in press.. [Google Scholar]
- Farawela, H.; Khorshied, M.; Shaheen, I.; Gouda, H.; Nasef, A.; Abulata, N.; Mahmoud, H.; Zawam, H.; Mousa, S. The association between hepatitis C virus infection, genetic polymorphisms of oxidative stress genes and B-cell non-Hodgkin’s lymphoma risk in Egypt infection. Infect. Genetics Evol. 2012, 12, 1189–1194. [Google Scholar] [CrossRef]
- Agrawal, L.; Louboutina, J.; Reyes, B.; Bockstaele, E.; Strayer, D. HIV-1 Tat neurotoxicity: A model of acute and chronic exposure, and neuroprotection by gene delivery of antioxidant enzymes. Neurobiol. Dis. 2012, 45, 657–670. [Google Scholar] [CrossRef]
- Dworkin, B.; Wormser, G.; Axelrod, F.; Pierre, N.; Schwarz, E.; Seaton, T. Dietary intake in patients with acquired immunodeficiency syndrome (AIDS), patients with AIDS-related complex, and serologically positive human immunodeficiency virus patients: Correlations with nutritional status. J. Parenter. Enter. Nutr. 1990, 14, 605–609. [Google Scholar] [CrossRef]
- Abrams, B.; Duncan, D.; Hertz-Picciotto, I. A prospective study of dietary intake and acquired immune deficiency syndrome in HIV-seropositive homosexual men. J. Acquir. Immune Defic. Syndr. 1993, 6, 949–958. [Google Scholar] [PubMed]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Anthony, K.; Subramanya, G.; Uprichard, S.; Hammouda, F.; Saleh, M. Antioxidant and Anti-Hepatitis C Viral Activities of Commercial Milk Thistle Food Supplements. Antioxidants 2013, 2, 23-36. https://doi.org/10.3390/antiox2010023
Anthony K, Subramanya G, Uprichard S, Hammouda F, Saleh M. Antioxidant and Anti-Hepatitis C Viral Activities of Commercial Milk Thistle Food Supplements. Antioxidants. 2013; 2(1):23-36. https://doi.org/10.3390/antiox2010023
Chicago/Turabian StyleAnthony, Kevin, Gitanjali Subramanya, Susan Uprichard, Faiza Hammouda, and Mahmoud Saleh. 2013. "Antioxidant and Anti-Hepatitis C Viral Activities of Commercial Milk Thistle Food Supplements" Antioxidants 2, no. 1: 23-36. https://doi.org/10.3390/antiox2010023




