Social Factors Determine the Emergency Medical Admission Workload
Abstract
:1. Introduction
2. Experimental Section
2.1. Background
2.2. Data Collection
2.3. Deprivation Indices
2.4. Risk Predictors
2.5. Statistical Methods
3. Results
3.1. Patient Demographics
3.2. Emergency Medical Patient Admission Characteristics
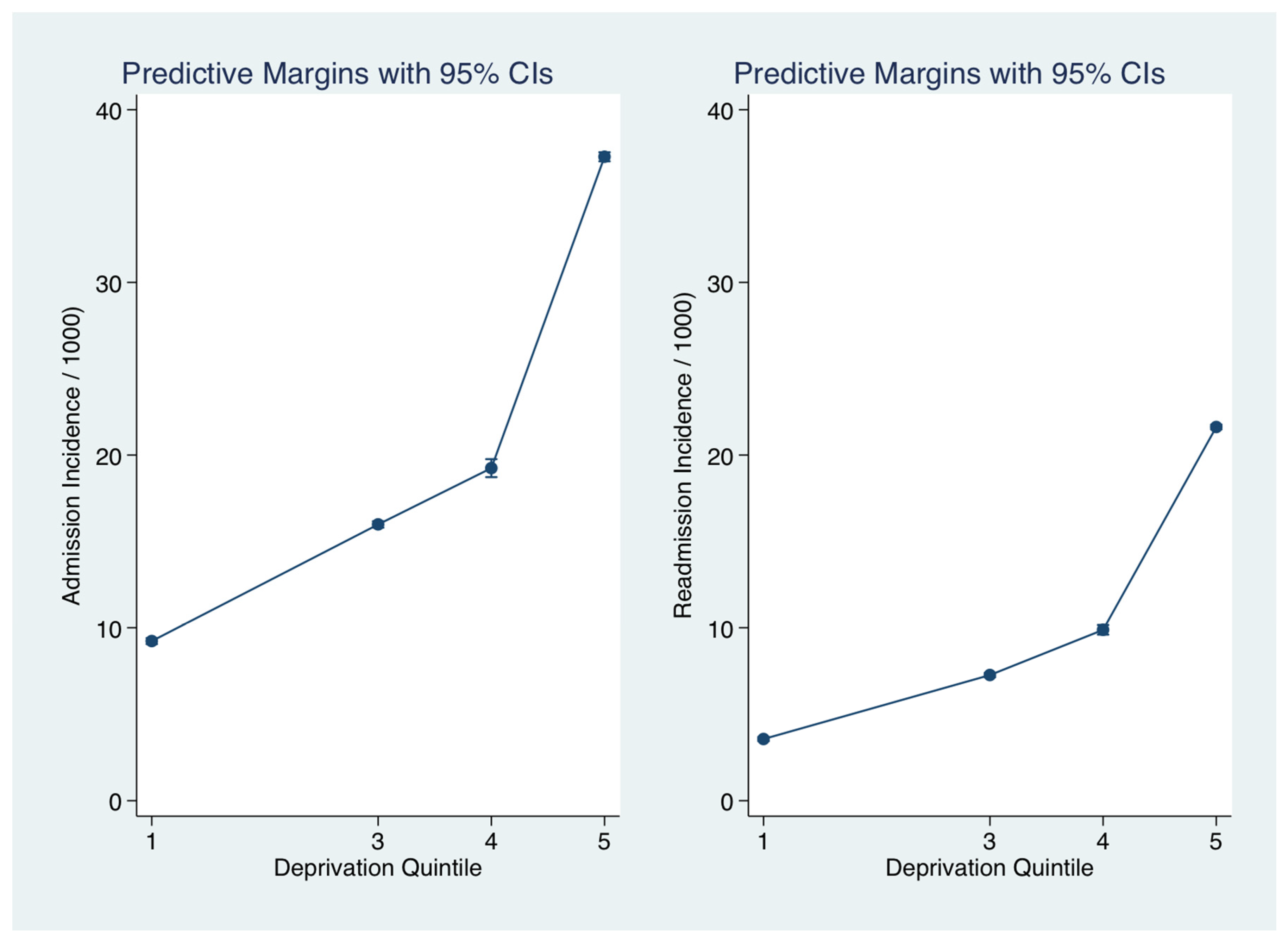
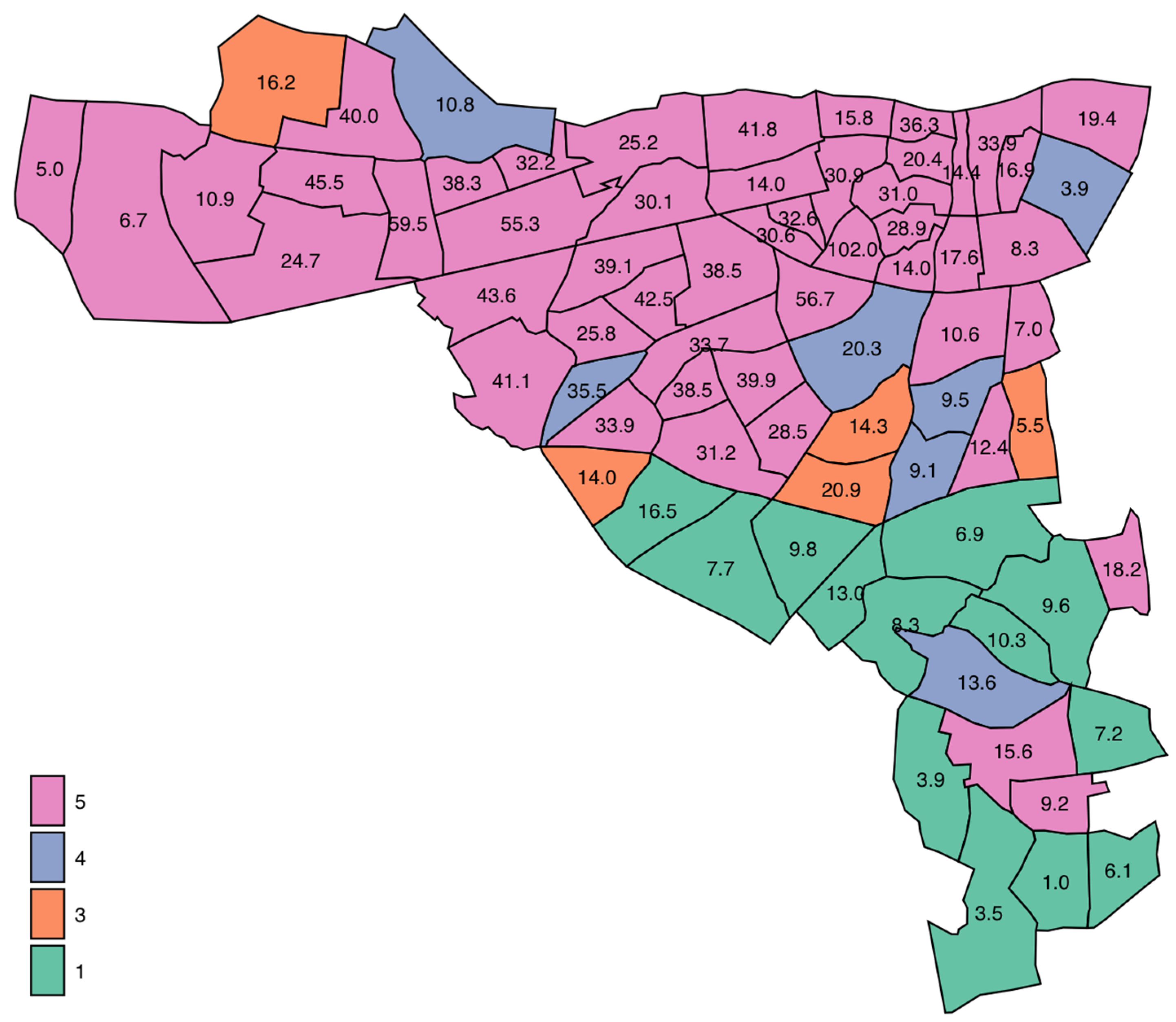
3.3. Deprivation Parameters and Admission Incidence Rates
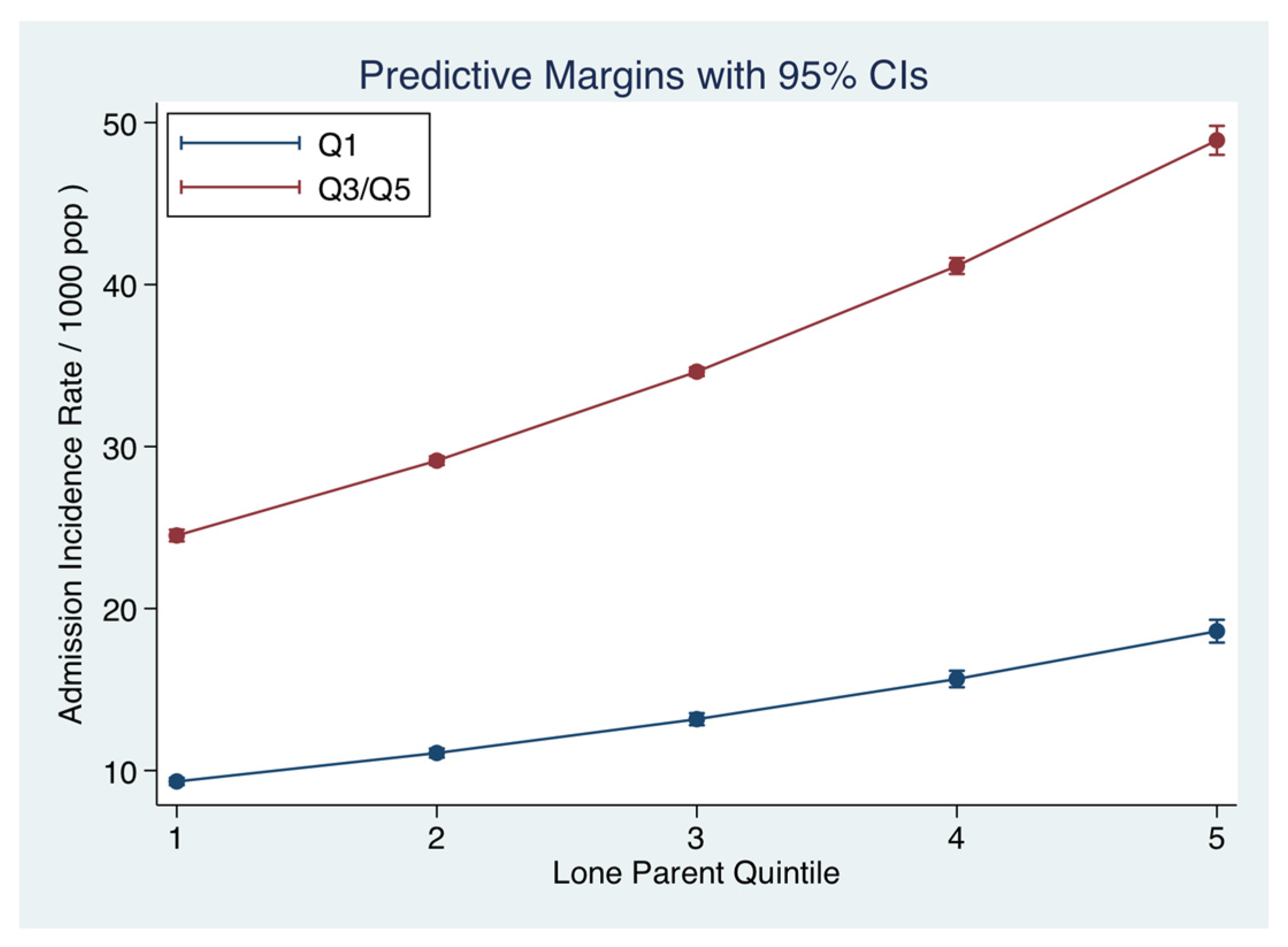
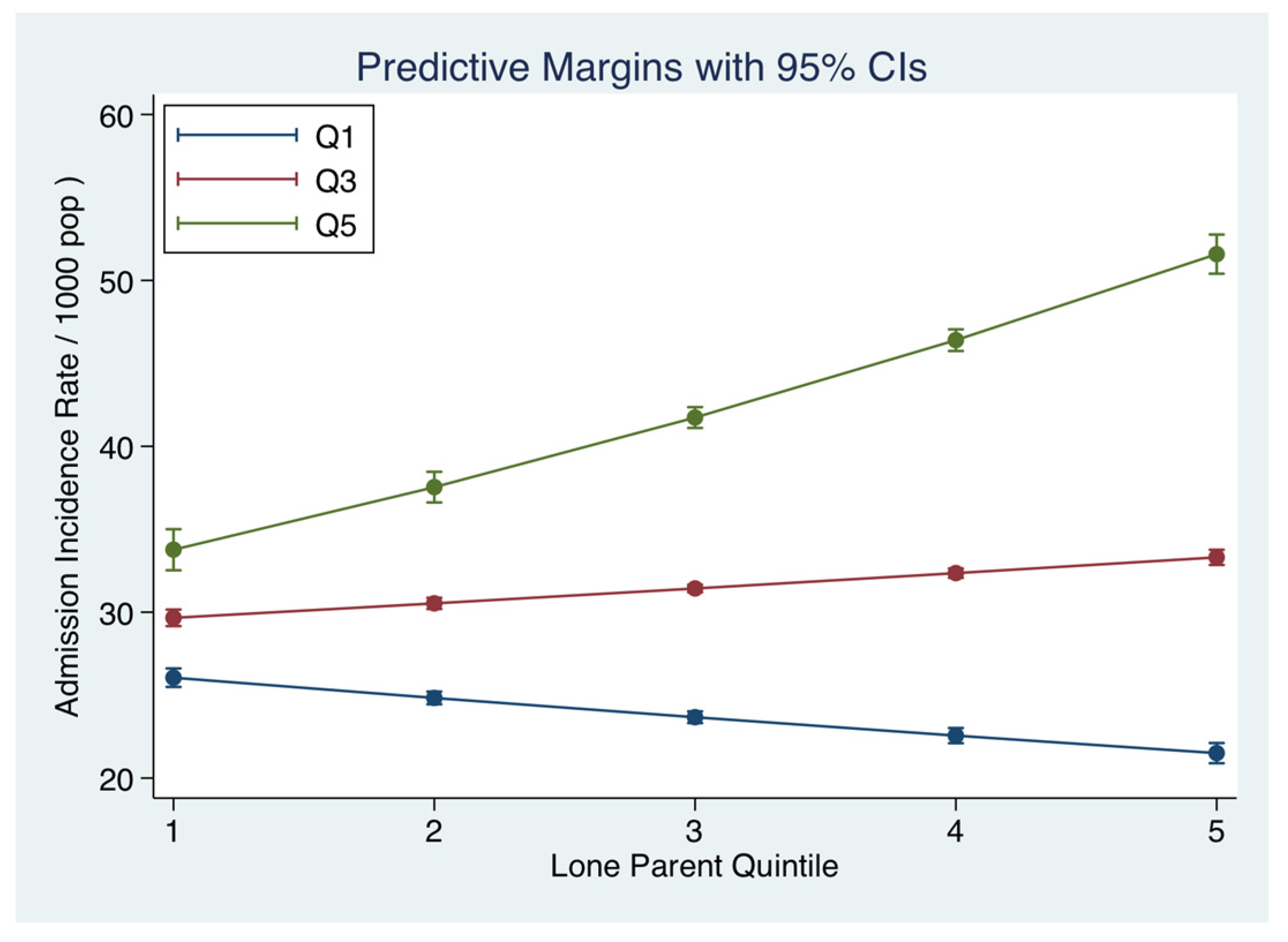
3.4. Other Small Area Descriptors and the Admission Incidence Rates
3.5. Multivariable Model with Adjustment for Deprivation Index
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Townsend, P. Deprivation. J. Soc. Policy 1987, 16, 25–46. [Google Scholar] [CrossRef]
- Lyratzopoulos, G.; Havely, D.; Gemmell, I.; Cook, G.A. Factors influencing emergency medical readmission risk in a UK district general hospital: A prospective study. BMC Emerg. Med. 2005, 5, 1. [Google Scholar]
- Epstein, A.M.; Stern, R.S.; Weissman, J.S. Do the poor cost more? A multihospital study of patients’ socioeconomic status and use of hospital resources. N. Engl. J. Med. 1990, 322, 1122–1128. [Google Scholar] [CrossRef] [PubMed]
- Benach, J.; Yasui, Y. Geographical patterns of excess mortality in Spain explained by two indices of deprivation. J. Epidemiol. Community Health 1999, 53, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Carstairs, V.; Morris, R. Deprivation: Explaining differences in mortality between Scotland and England and Wales. BMJ 1989, 299, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Coary, R.; Byrne, D.; O’Riordan, D.; Conway, R.; Cournane, S.; Silke, B. Does admission via an Acute Medical Unit influence hospital mortality? 12 years’ experience in a large Dublin Hospital. Acute Med. 2014, 13, 152–158. [Google Scholar] [PubMed]
- Conway, R.; O’Riordan, D.; Silke, B. Long-term outcome of an AMAU—A decade’s experience. Q. J. Med. 2014, 107, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Holt, P.J.E.; Sinha, S.; Ozdemir, B.A.; Karthikesalingam, A.; Poloniecki, J.D.; Thompson, M.M. Variations and inter-relationship in outcome from emergency admissions in England: A retrospective analysis of Hospital Episode Statistics from 2005–2010. BMC Health Serv. Res. 2014, 14, 270. [Google Scholar] [CrossRef] [PubMed]
- Carstairs, V.; Morris, R. Deprivation and mortality: An alternative to social class? J. Public Health 1989, 11, 210–219. [Google Scholar] [CrossRef]
- Kelly, A.; Teljeur, C. SAHRU National Deprivation Index Trinity College, Dublin 2007. Available online: http://www.sahru.tcd.ie/services/deprivation/DeprivationFiles/WebReport07.pdf (accessed on 1 April 2017).
- Gordon, D.; Levitas, R.; Pantazis, C.; Patsios, D.; Payne, S.; Townsend, P. Poverty and social exclusion in Britain. Townsend Centre for International Poverty Research, University of Bristol Centre for Research in Social Policy, Loughborough University Social Policy Research Unit, University of York, 2000. Available online: http://www.poverty.ac.uk/system/files/JRF-Full-report-Poverty-social-exclusion_0.pdf (accessed on 1 April 2017).
- Spencer, N. Does material disadvantage explain the increased risk of adverse health, educational, and behavioural outcomes among children in lone parent households in Britain? A cross sectional study. J. Epidemiol. Community Health 2005, 59, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Mooney, A.; Oliver, C.; Smith, M. Impact of Family Breakdown on Children’s Well-Being. Evidence Review. University of London: Institute of Education, 2009. Available online: http://dera.ioe.ac.uk/11165/1/DCSF-RR113.pdf (accessed on 1 April 2017).
- Sauvola, A.; Makikyro, T.; Jokelainen, J.; Joukamaa, M.; Jarvelin, M.R.; Isohanni, M. Single-parent family background and physical illness in adulthood: A follow-up study of the Northern Finland 1966 birth cohort. Scand. J. Public Health 2000, 28, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; McCaffery, K. Health Literacy: A Brief Literature Review; NSW Clinical Excellence Commission: Sydney, Australia, 2010. [Google Scholar]
- Walsh, J.B.; Coakley, D.; Murphy, C.; Coakley, J.D.; Boyle, E.; Johnson, H. Demographic profile of the elderly population in Dublin accident and emergency hospital catchment areas. Ir. Med. J. 2004, 97, 84–86. [Google Scholar] [PubMed]
- Cournane, S.; Conway, R.; Byrne, D.; O’Riordan, D.; Coveney, S.; Silke, B. Social deprivation and the rate of emergency medical admission for older persons. QJM 2016, 109, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Rooney, T.; Moloney, E.D.; Bennett, K.; O’Riordan, D.; Silke, B. Impact of an acute medical admission unit on hospital mortality: A 5-year prospective study. QJM 2008, 101, 457–465. [Google Scholar] [CrossRef] [PubMed]
- O’Loughlin, R.; Allwright, S.; Barry, J.; Kelly, A.; Teljeur, C. Using HIPE data as a research and planning tool: Limitations and opportunities. Ir. J. Med. Sci. 2005, 174, 40–45. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, A.; Colgan, M.P.; McGuigan, C.; Smyth, F.; Haider, N.; O’Neill, S.; Madhavan, P. A critical evaluation of HIPE data. Ir. Med. J. 2012, 105, 21–23. [Google Scholar] [PubMed]
- Conway, R.; Galvin, S.; Coveney, S.; O’Riordan, D.; Silke, B. Deprivation as an outcome determinant in emergency medical admissions. QJM 2013, 106, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Shimrat, M. Algorithm 112: Position of point relative to polygon. Commun. ACM 1962, 5, 434. [Google Scholar] [CrossRef]
- Silke, B.; Kellett, J.; Rooney, T.; Bennett, K.; O’Riordan, D. An improved medical admissions risk system using multivariable fractional polynomial logistic regression modelling. Q. J. Med. 2010, 103, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Courtney, D.; Conway, R.; Kavanagh, J.; O’Riordan, D.; Silke, B. High-sensitivity troponin as an outcome predictor in acute medical admissions. Postgrad. Med. J. 2014. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Chotirmall, S.H.; Picardo, S.; Lyons, J.; D’Alton, M.; O’Riordan, D.; Silke, B. Disabling disease codes predict worse outcomes for acute medical admissions. Intern. Med. J. 2014, 44, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.; Trivedi, P. Microeconometrics Using Stata; Stata Press: College Station, TX, USA, 2009. [Google Scholar]
- O’Sullivan, E.; Callely, E.; O’Riordan, D.; Bennett, K.; Silke, B. Predicting outcomes in emergency medical admissions—Role of laboratory data and co-morbidity. Acute Med. 2012, 2, 59–65. [Google Scholar]
- Chotirmall, S.H.; Callaly, E.; Lyons, J.; O’Connell, B.; Kelleher, M.; Byrne, D.; Silke, B. Blood cultures in emergency medical admissions: A key patient cohort. Eur. J. Emerg. Med. 2016, 23, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Cournane, S.; Dalton, A.; Byrne, D.; Conway, R.; O’Riordan, D.; Coveney, S.; Silke, B. Social deprivation, population dependency ratio and an extended hospital episode—Insights from acute medicine. Eur. J. Intern. Med. 2015, 26, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Dixon, A.; Gao, H. Emergency Hospital Admissions for Ambulatory Care-Sensitive Conditions: Identifying the Potential for Reductions. 2012. (Updated 1–13 Februar 2016). Available online: http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/data-briefing-emergency-hospital-admissions-for-ambulatory-care-sensitive-conditions-apr-2012.pdf (accessed on 1 April 2017).
- Tian, Y.; Dixon, A.; Gao, H. Emergency Hospital Admissions for Ambulatory Care-Sensitive Conditions: Identifying the Potential for Reductions. Data briefing London 2012. Available online: www.kingsfund.org.uk/publications/data_briefing.html (accessed on 1 April 2017).
- Kellett, J.; Rasool, S.; McLoughlin, B. Prediction of mortality 1 year after hospital admission. QJM 2012, 105, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Inequality in Healthy Life Expectancy at Birth by National Deciles of Area Deprivation: England, 2011 to 2013. 2015. Available online: http://webarchive.nationalarchives.gov.uk/20160105160709/http://www.ons.gov.uk/ons/rel/disability-and-health-measurement/inequality-in-healthy-life-expectancy-at-birth-by-national-deciles-of-area-deprivation--england/2011-13/index.html (accessed on 1 April 2017).
- Downey, D. The school performance of children from single-mother and single-father families: Economic or interpersonal deprivation? J. Fam. Issues 1994, 1, 129–147. [Google Scholar] [CrossRef]
- Blakely, T.; Atkinson, J.; Kiro, C.; Blaiklock, A.; D’Souza, A. Child mortality, socioeconomic position, and one-parent families: Independent associations and variation by age and cause of death. Int. J. Epidemiol. 2003, 32, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.D.; Arozullah, A.M.; Cho, Y.I. Health literacy, social support, and health: A research agenda. Soc. Sci. Med. 2004, 58, 1309–1321. [Google Scholar] [CrossRef]
- Office, C.S. Life Expectancy: Period Life Expectancy at Various Ages (Years) by Sex, Year and Age Dublin: Central Statistics Office, Ireland. 2010. Available online: http://www.cso.ie/Quicktables/GetQuickTables.aspx?FileName=VSA30.asp&TableName=Life+Expectancy&StatisticalProduct=DB_VS (accessed on 1 April 2017).
- Wolff, J.; Edward Lamb, E.; Zur-Szpiro, E. A philosophical review of poverty. 2015. Available online: https://www.jrf.org.uk/report/philosophical-review-poverty (accessed on 1 April 2017).
| Factor | Level | Quintiles I/III | Quintiles IV/V | p-Value |
|---|---|---|---|---|
| N | 6150 | 56,219 | ||
| Gender | Male | 2791 (45.4%) | 27,654 (49.2%) | <0.001 |
| Female | 3359 (54.6%) | 28,565 (50.8%) | ||
| Outcome | Alive | 5750 (93.5%) | 53,479 (95.1%) | <0.001 |
| Died | 400 (6.5%) | 2740 (4.9%) | ||
| Age, median (IQR) | 74.9 (58.3, 83.2) | 64.3 (45.1, 77.9) | <0.001 | |
| Length of Stay (days) | 5.5 (2.4, 10.8) | 5.3 (2.3, 10.0) | <0.001 | |
| Admission Rate * | 14.0 (7.7, 16.2) | 33.9 (25.8, 41.8) | <0.001 | |
| Readmissions | 1.0 (0.0, 2.0) | 2.0 (0.0, 4.0) | <0.001 | |
| Acute Illness Severity | 1 | 117 (2.1%) | 1373 (2.7%) | <0.001 |
| 2 | 261 (4.7%) | 3305 (6.4%) | ||
| 3 | 459 (8.2%) | 5973 (11.6%) | ||
| 4 | 726 (13.0%) | 8637 (16.8%) | ||
| 5 | 1156 (20.7%) | 10,454 (20.3%) | ||
| 6 | 2863 (51.3%) | 21,748 (42.2%) | ||
| Charlson Index | 0 | 2788 (45.4%) | 23,704 (42.3%) | <0.001 |
| 1 | 1658 (27.0%) | 16,666 (29.7%) | ||
| 2 | 1693 (27.6%) | 15,730 (28.0%) | ||
| Disabling Disease | 0 | 578 (9.4%) | 5696 (10.1%) | 0.014 |
| 1 | 1432 (23.3%) | 13,666 (24.3%) | ||
| 2 | 1771 (28.8%) | 16,269 (28.9%) | ||
| 3 | 1390 (22.6%) | 12,359 (22.0%) | ||
| 4 | 979 (15.9%) | 8229 (14.6%) | ||
| Sepsis Group | 1 | 4757 (77.3%) | 42,985 (76.5%) | 0.073 |
| 2 | 1171 (19.0%) | 11,347 (20.2%) | ||
| 3 | 222 (3.6%) | 1887 (3.4%) | ||
| MDC Respiratory | 4796 (78.0%) | 40,554 (72.1%) | <0.001 | |
| 1354 (22.0%) | 15,665 (27.9%) | |||
| MDC Cardiovascular | 0 | 4906 (79.8%) | 46,879 (83.4%) | <0.001 |
| 1 | 1244 (20.2%) | 9340 (16.6%) | ||
| MDC Neurology | 0 | 5015 (81.5%) | 47,296 (84.1%) | <0.001 |
| 1 | 1135 (18.5%) | 8923 (15.9%) |
| Predictor | IRR | SE | z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Single Parent | ||||||
| Q2 | 1.18 | 0.02 | 10.4 | 0.000 | 1.14 | 1.21 |
| Q3 | 1.45 | 0.02 | 25.6 | 0.000 | 1.41 | 1.49 |
| Q4 | 1.33 | 0.02 | 21.0 | 0.000 | 1.30 | 1.37 |
| Q5 | 1.69 | 0.02 | 30.5 | 0.000 | 1.63 | 1.75 |
| Education <15 years | ||||||
| Q2 | 1.46 | 0.03 | 16.9 | 0.000 | 1.40 | 1.53 |
| Q3 | 1.22 | 0.03 | 9.1 | 0.000 | 1.17 | 1.27 |
| Q4 | 1.07 | 0.02 | 3.3 | 0.001 | 1.03 | 1.12 |
| Q5 | 1.19 | 0.02 | 8.8 | 0.000 | 1.15 | 1.24 |
| Dependency Ratio | ||||||
| Q2 | 1.11 | 0.02 | 6.5 | 0.000 | 1.07 | 1.14 |
| Q3 | 1.97 | 0.03 | 44.4 | 0.000 | 1.91 | 2.03 |
| Q4 | 1.56 | 0.02 | 30.6 | 0.000 | 1.51 | 1.60 |
| Q5 | 1.82 | 0.02 | 36.8 | 0.000 | 1.76 | 1.88 |
| Deprivation Index | ||||||
| Q3 | 1.54 | 0.04 | 17.8 | 0.000 | 1.47 | 1.62 |
| Q4 | 2.13 | 0.05 | 33.0 | 0.000 | 2.04 | 2.23 |
| Q5 | 2.94 | 0.05 | 62.2 | 0.000 | 2.84 | 3.04 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cournane, S.; Conway, R.; Byrne, D.; O’Riordan, D.; Coveney, S.; Silke, B. Social Factors Determine the Emergency Medical Admission Workload. J. Clin. Med. 2017, 6, 59. https://doi.org/10.3390/jcm6060059
Cournane S, Conway R, Byrne D, O’Riordan D, Coveney S, Silke B. Social Factors Determine the Emergency Medical Admission Workload. Journal of Clinical Medicine. 2017; 6(6):59. https://doi.org/10.3390/jcm6060059
Chicago/Turabian StyleCournane, Seán, Richard Conway, Declan Byrne, Deirdre O’Riordan, Seamus Coveney, and Bernard Silke. 2017. "Social Factors Determine the Emergency Medical Admission Workload" Journal of Clinical Medicine 6, no. 6: 59. https://doi.org/10.3390/jcm6060059






