Facial Nerve Paralysis after Onyx Embolization of a Jugular Paraganglioma: A Case Report with a Long-Term Follow Up
Abstract
:1. Introduction
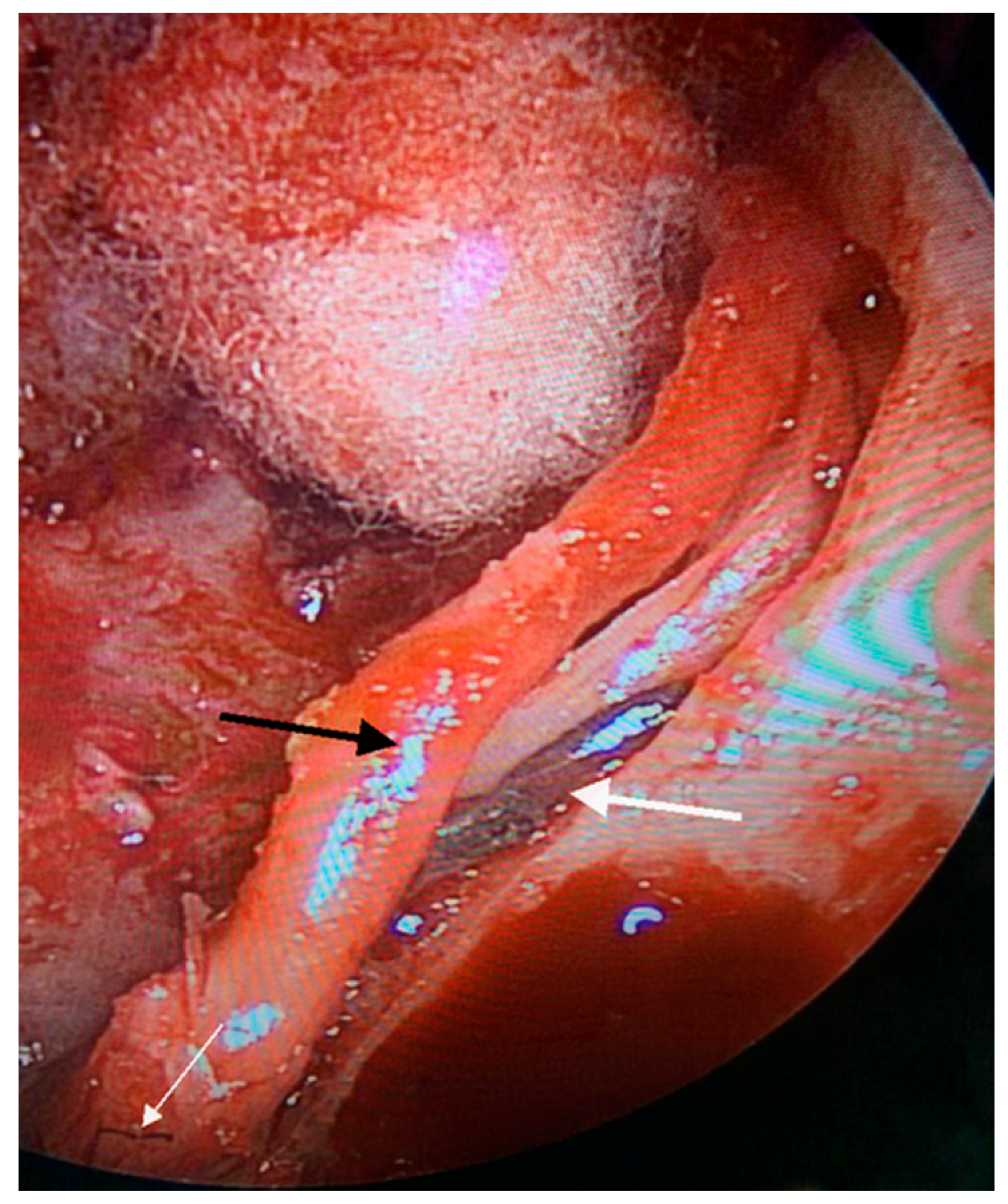
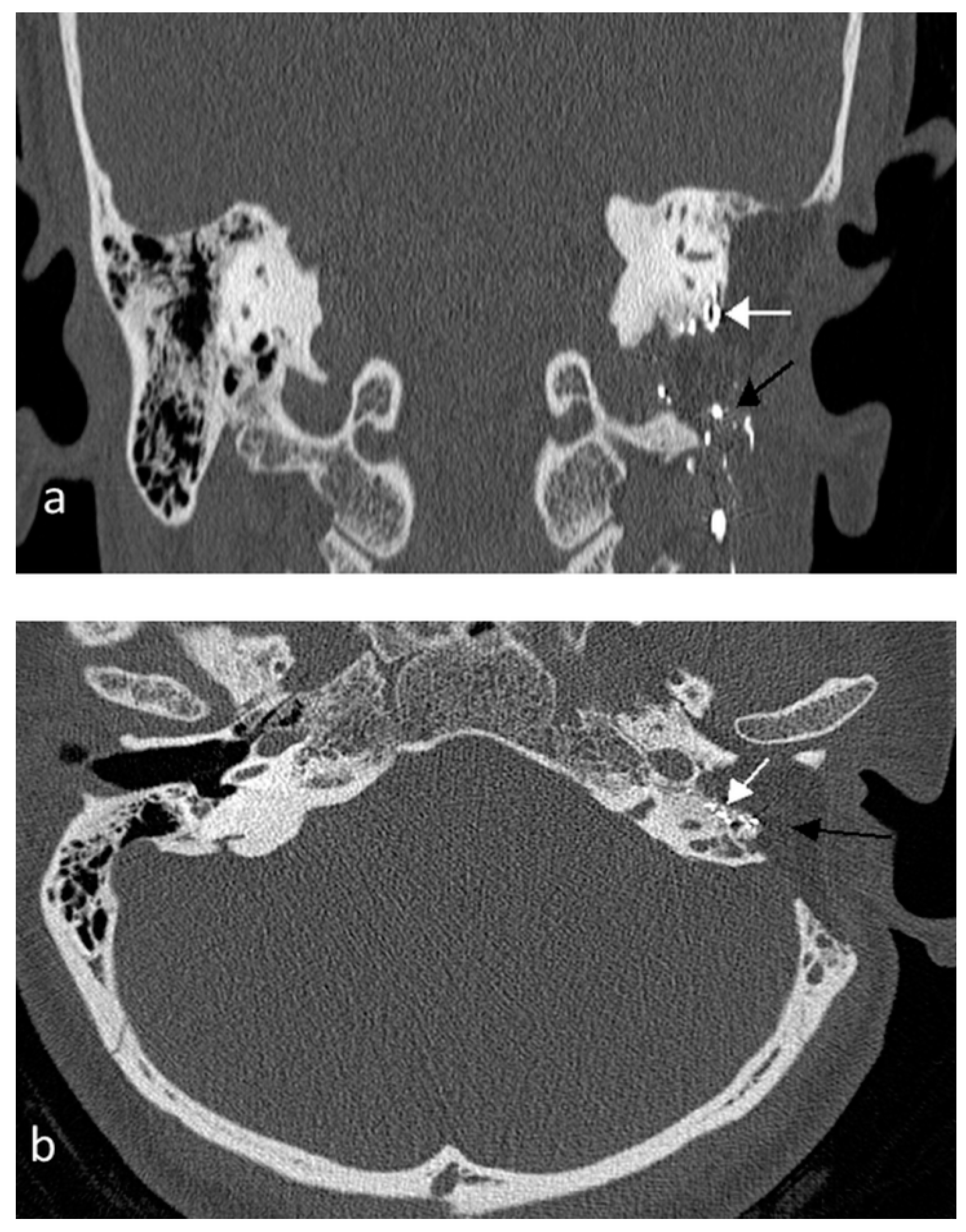
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Sanna, M.; Jain, Y.; De Donato, G.; Lauda, L.; Taibah, A. Management of jugular paragangliomas: The Gruppo Otologico experience. Otol. Neurotol. 2004, 25, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Odat, H.; Shin, S.H.; Odat, M.A.; Alzoubi, F. Facial nerve management in jugular paraganglioma surgery: A literature review. J. Laryngol. Otol. 2016, 130, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Gartrell, B.C.; Hansen, M.R.; Gantz, B.J.; Gluth, M.B.; Mowry, S.E.; Aagaard-Kienitz, B.L.; Baskaya, M.K.; Gubbels, S.P. Facial and lower cranial neuropathies after preoperative embolization of jugular foramen lesionswith ethylene vinyl alcohol. Otol. Neurotol. 2012, 33, 1270–1275. [Google Scholar] [CrossRef] [PubMed]
- Ayad, M. Onyx: A Unique Neuroembolic Agent. Expert Rev. Med. Devices 2006, 3, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Kadakia, S.; Koss, S.; Isseroff, T.F.; Holliday, R.A.; Kim, A.H. Facial nerve paralysis after pre-operative embolization of a paraganglioma. Am. J. Otolaryngol. 2015, 36, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Gore, P.; Theodore, N.; Brasiliense, L.; Kim, L.J.; Garrett, M.; Nakaji, P.; Gonzalez, L.F.; McDougall, C.G.; Albuquerque, F.C. The utility of Onyx for preoperative embolization of cranial and spinal tumors. Neurosurgery 2008, 62, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Thiex, R.; Wu, I.; Mulliken, J.B.; Greene, A.K.; Rahbar, R.; Orbach, D.B. Safety and clinical efficacy of Onyx for embolization of extracranial head and neck vascular anomalies. AJNR Am. J. Neuroradiol. 2011, 32, 1082–1086. [Google Scholar] [CrossRef] [PubMed]
- Gaynor, B.G.; Elhammady, M.S.; Jethanamest, D.; Angeli, S.I.; Aziz-Sultan, M.A. Incidence of cranial nerve palsy after preoperative embolization of glomus jugulare tumors using Onyx. J. Neurosurg. 2014, 120, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Michelozzi, C.; Januel, A.C.; Cuvinciuc, V.; Tall, P.; Bonneville, F.; Fraysse, B.; Deguine, O.; Serrano, E.; Cognard, C. Arterial embolization with Onyx of head and neck paragangliomas. J. Neurointerv. Surg. 2016, 8, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Ladner, T.R.; He, L.; Davis, B.J.; Yang, G.L.; Wanna, G.B.; Mocco, J. Initial experience with dual-lumen balloon catheter injection for preoperative Onyx embolization of skull base paragangliomas. J. Neurosurg. 2016, 124, 1813–1819. [Google Scholar] [CrossRef] [PubMed]

| Author, Year | FN H-B Grade Post-Emb. | FN H-B Grade Final | Follow-Up (Months) | Management | LCN Paralysis |
|---|---|---|---|---|---|
| Gartrell et al., 2012 [3] * | 2 cases | 2 cases | |||
| 1. VI | 1. VI | 3 | Surgery | 1. X, XII | |
| 2. V | 2. II | 19 | Surgery | 2. X, XI | |
| Gaynor et al., 2014 [8] | VI | VI | 6 | Surgery | X paralysis |
| Ladner et al., 2014 [10] | V | I | 6 | Surgery | None |
| Kadakia et al., 2015 [5] | VI | No follow-up | Observation | None | |
| Michelozzi et al., 2016 [9] ** | 4 cases | 4 cases | |||
| 1. III | 1. I | 12 | Observation | 3 cases X | |
| 2. V | 2. II | 10 | |||
| 3. II | 3. I | 15 | 1 case X, XII | ||
| 4. IV | 4. II | 12 | |||
| Our case | V | II | 30 | Surgery | None |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Odat, H.; Alawneh, K.; Al-Qudah, M. Facial Nerve Paralysis after Onyx Embolization of a Jugular Paraganglioma: A Case Report with a Long-Term Follow Up. J. Clin. Med. 2018, 7, 48. https://doi.org/10.3390/jcm7030048
Odat H, Alawneh K, Al-Qudah M. Facial Nerve Paralysis after Onyx Embolization of a Jugular Paraganglioma: A Case Report with a Long-Term Follow Up. Journal of Clinical Medicine. 2018; 7(3):48. https://doi.org/10.3390/jcm7030048
Chicago/Turabian StyleOdat, Haitham, Khaled Alawneh, and Mohannad Al-Qudah. 2018. "Facial Nerve Paralysis after Onyx Embolization of a Jugular Paraganglioma: A Case Report with a Long-Term Follow Up" Journal of Clinical Medicine 7, no. 3: 48. https://doi.org/10.3390/jcm7030048





