Religious Beliefs and Their Relevance for Treatment Adherence in Mental Illness: A Review
Abstract
:1. Introduction
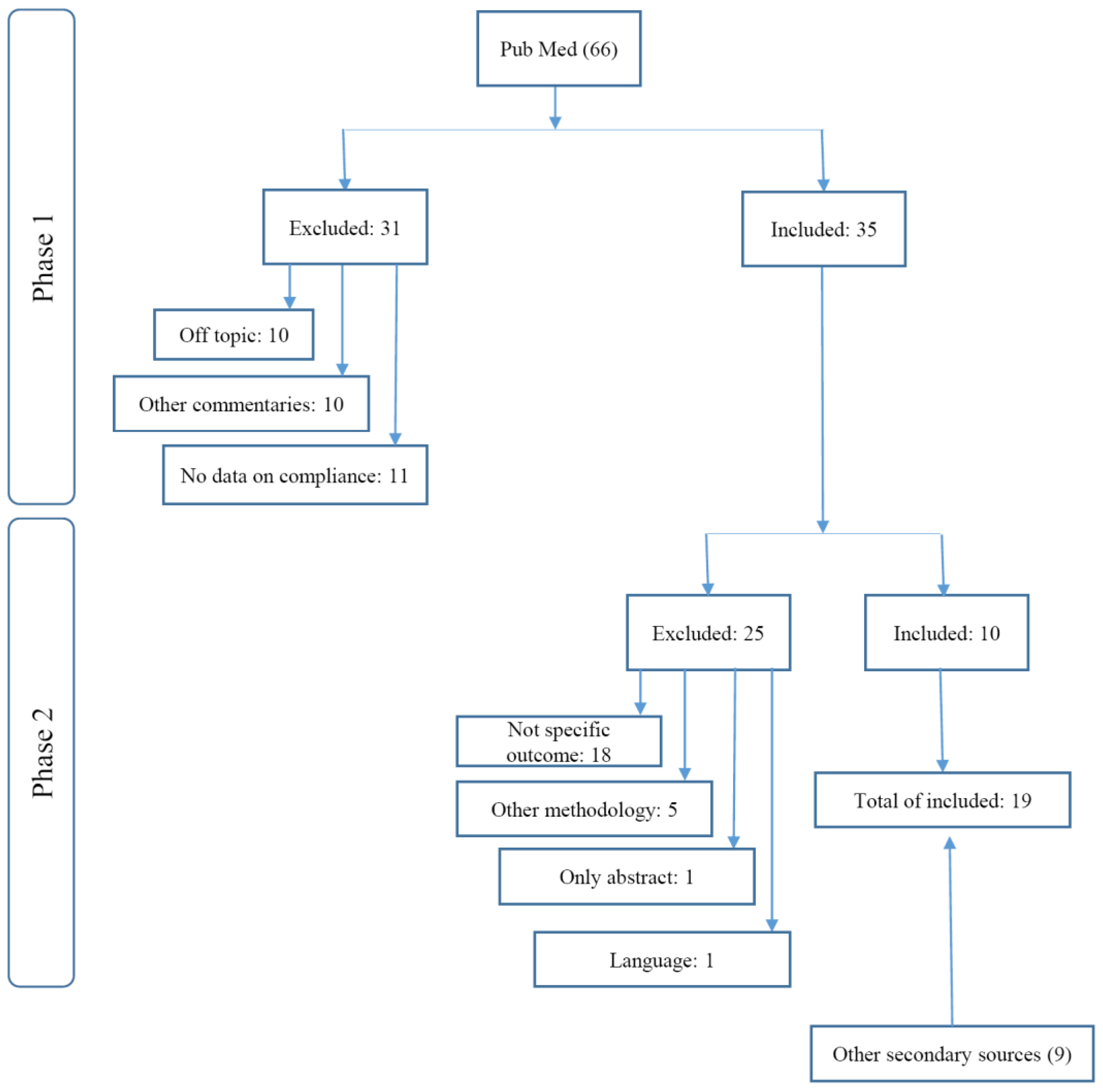
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategies
2.3. Data Items
2.4. Risk of Bias
3. Results
3.1. Characteristics of Studies
3.2. Interventions and/or Outcome Measures
3.3. Outcomes and Associations
4. Discussion
4.1. Treatment Adherence in Schizophrenia
4.2. Treatment Adherence in Addiction
4.3. Treatment Adherence in Depression and Anxiety
4.4. Quality of Evidence
4.5. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Arnold, Ruth M., S. Kelly Avants, Arthur Margolin, and David Marcotte. 2002. Patient Attitudes Concerning the Inclusion of Spirituality into Addiction Treatment. Journal of Substance Abuse Treatment 23: 319–26. [Google Scholar] [CrossRef]
- Borras, Laurence, S. Mohr, P.-Y. Brandt, C. Gilliéron, A. Eytan, and P. Huguelet. 2007. Religious Beliefs in Schizophrenia: Their Relevance for Adherence to Treatment. Schizophrenia Bulletin 33: 1238–46. [Google Scholar] [CrossRef] [PubMed]
- Brown, Barry S., Kevin E. O’Grady, Eugene V. Farrell, Ilene S. Flechner, and David N. Nurco. 2001. Factors Associated with Frequency of 12-Step Attendance by Drug Abuse Clients. The American Journal of Drug and Alcohol Abuse 27: 147–60. [Google Scholar] [CrossRef] [PubMed]
- Caqueo-Urízar, Alejandra, Laurent Boyer, Karine Baumstarck, and Stephen E. Gilman. 2015. The Relationships between Patients’ and Caregivers’ Beliefs about the Causes of Schizophrenia and Clinical Outcomes in Latin American Countries. Psychiatry Research 229: 440–46. [Google Scholar] [CrossRef] [PubMed]
- Chi, Felicia W., Lee A. Kaskutas, Stacy Sterling, Cynthia I. Campbell, and Constance Weisner. 2009. Twelve-Step Affiliation and 3-Year Substance Use Outcomes among Adolescents: Social Support and Religious Service Attendance as Potential Mediators. Addiction (Abingdon, England) 104: 927–39. [Google Scholar] [CrossRef] [PubMed]
- Christo, George, and Christine Franey. 1995. Drug Users’ Spiritual Beliefs, Locus of Control and the Disease Concept in Relation to Narcotics Anonymous Attendance and Six-Month Outcomes. Drug and Alcohol Dependence 38: 51–56. [Google Scholar] [CrossRef]
- Cramer, Joyce A., and Robert Rosenheck. 1998. Compliance with Medication Regimens for Mental and Physical Disorders. Psychiatric Services (Washington, D.C.) 49: 196–201. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, Russell F., and Angelo Rodrigo. 2004. Spiritually Augmented Cognitive Behavioural Therapy. Australasian Psychiatry: Bulletin of Royal Australian and New Zealand College of Psychiatrists 12: 148–52. [Google Scholar] [CrossRef] [PubMed]
- Foulks, Edward F., J. B. Persons, and R. L. Merkel. 1986. The Effect of Patients’ Beliefs about Their Illnesses on Compliance in Psychotherapy. The American Journal of Psychiatry 143: 340–44. [Google Scholar] [CrossRef] [PubMed]
- Galanter, Marc, Helen Dermatis, Gregory Bunt, Caroline Williams, Manuel Trujillo, and Paul Steinke. 2007. Assessment of Spirituality and Its Relevance to Addiction Treatment. Journal of Substance Abuse Treatment 33: 257–64. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, Juliane P. B., G. Lucchetti, P. R. Menezes, and H. Vallada. 2015. Religious and Spiritual Interventions in Mental Health Care: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Psychological Medicine 45: 2937–49. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R. Brian, David L. Sackett, D. Wayne Taylor, R. S. Roberts, and A. L. Johnson. 1977. Manipulation of the Therapeutic Regimen to Improve Compliance: Conceptions and Misconceptions. Clinical Pharmacology and Therapeutics 22: 125–30. [Google Scholar] [CrossRef] [PubMed]
- Holzinger, Anita, Watter Loffler, Peter Muller, Stefan Priebe, and Matthias C. Angermeyer. 2002. Subjective Illness Theory and Antipsychotic Medication Compliance by Patients with Schizophrenia. The Journal of Nervous and Mental Disease 190: 597–603. [Google Scholar] [CrossRef] [PubMed]
- Huguelet, Philippe, and Koenig Harold. 2009. Introduction: Key Concepts. In Religion and Spirituality in Psychiatry, 1st ed. Cambridge: Cambridge University Press, pp. 1–4. [Google Scholar]
- Huguelet, Philippe, Sylvia Mohr, Carine Betrisey, Laurence Borras, Christiane Gillieron, Adham Mancini Marie, Isabelle Rieben, Nader Perroud, and Pierre-Yves Brandt. 2011. A Randomized Trial of Spiritual Assessment of Outpatients with Schizophrenia: Patients’ and Clinicians’ Experience. Psychiatric Services (Washington, D.C.) 62: 79–86. [Google Scholar] [CrossRef] [PubMed]
- Huguelet, Philippe, Sylvia Mohr, Laurence Borras, Christiane Gillieron, and Pierre-Yves Brandt. 2006. Spirituality and Religious Practices among Outpatients with Schizophrenia and Their Clinicians. Psychiatric Services (Washington, D.C.) 57: 366–72. [Google Scholar] [CrossRef] [PubMed]
- Van Rensburg, ABR Janse, C. P. H. Myburgh, C. P. Szabo, and M. Poggenpoel. 2013. The Role of Spirituality in Specialist Psychiatry: A Review of the Medical Literature. African Journal of Psychiatry 16: 247–55. [Google Scholar] [CrossRef]
- Kelly, John F., Robert L. Stout, Molly Magill, J. Scott Tonigan, and Maria E. Pagano. 2011. Spirituality in Recovery: A Lagged Mediational Analysis of Alcoholics Anonymous’ Principal Theoretical Mechanism of Behavior Change. Alcoholism, Clinical and Experimental Research 35: 454–63. [Google Scholar] [CrossRef] [PubMed]
- Kirov, George, R. Kemp, K. Kirov, and A. S. David. 1998. Religious Faith after Psychotic Illness. Psychopathology 31: 234–45. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G., Michelle J. Pearce, Bruce Nelson, Sally F. Shaw, Clive J. Robins, Noha S. Daher, Harvey Jay Cohen, L. S. Berk, D. L. Bellinger, K. I. Pargament, and et al. 2015. Religious vs. Conventional Cognitive Behavioral Therapy for Major Depression in Persons with Chronic Medical Illness: A Pilot Randomized Trial. The Journal of Nervous and Mental Disease 203: 243–51. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold, Dana King, and Verna B. Carson. 2012. Psychological, Social, and Behavioral Pathways. In Handbook of Religion and Health, 2nd ed. Oxford and New York: Oxford University Press, pp. 579–99. [Google Scholar]
- Krentzman, Amy R., James A. Cranford, and Elizabeth A. R. Robinson. 2013. Multiple Dimensions of Spirituality in Recovery: A Lagged Mediational Analysis of Alcoholics Anonymous’ Principal Theoretical Mechanism of Behavior Change. Substance Abuse 34: 20–32. [Google Scholar] [CrossRef] [PubMed]
- Lacro, Jonathan P., Laura B. Dunn, Christian R. Dolder, Susan G. Leckband, and Dilip V. Jeste. 2002. Prevalence of and Risk Factors for Medication Nonadherence in Patients with Schizophrenia: A Comprehensive Review of Recent Literature. The Journal of Clinical Psychiatry 63: 892–909. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, Jeffrey A., Brian Sheitman, Miranda Chakos, Delbert Robinson, Nina Schooler, and Sam Keith. 1998. The Development of Treatment Resistance in Patients with Schizophrenia: A Clinical and Pathophysiologic Perspective. Journal of Clinical Psychopharmacology 18: 20S–4S. [Google Scholar] [CrossRef]
- Lin, Shuai-Ting, Cheng-Chung Chen, Hin-Yeung Tsang, Chee-Siong Lee, Pinchen Yang, Kai-Da Cheng, Dian-Jeng Li, Chin-Jen Wang, Yung-Chi Hsieh, and Wei-Cheng Yang. 2014. Association between Antipsychotic Use and Risk of Acute Myocardial Infarction: A Nationwide Case-Crossover Study. Circulation 130: 235–43. [Google Scholar] [CrossRef] [PubMed]
- Margolin, Arthur, Mark Beitel, Zev Schuman-Olivier, and S. Kelly Avants. 2006. A Controlled Study of a Spirituality-Focused Intervention for Increasing Motivation for HIV Prevention among Drug Users. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education 18: 311–22. [Google Scholar] [CrossRef] [PubMed]
- Masand, Prakash S., Miquel Roca, Martin S. Turner, and John M. Kane. 2009. Partial Adherence to Antipsychotic Medication Impacts the Course of Illness in Patients with Schizophrenia: A Review. Primary Care Companion to the Journal of Clinical Psychiatry 11: 147–54. [Google Scholar] [CrossRef] [PubMed]
- McCann, Terence V., Cecil Deans, Eileen Clark, and Sai Lu. 2008. A Comparative Study of Antipsychotic Medication Taking in People with Schizophrenia. International Journal of Mental Health Nursing 17: 428–38. [Google Scholar] [CrossRef] [PubMed]
- Mohr, Sylvia, Laurence Borras, Jennifer Nolan, Christiane Gillieron, Pierre-Yves Brandt, Ariel Eytan, Claude Leclerc, Nader Perroud, Kathryn Whetten, and Carl Pieper. 2012. Spirituality and Religion in Outpatients with Schizophrenia: A Multi-Site Comparative Study of Switzerland, Canada, and the United States. International Journal of Psychiatry in Medicine 44: 29–52. [Google Scholar] [CrossRef] [PubMed]
- Mutsatsa, Stan H., E. M. Joyce, S. B. Hutton, E. Webb, H. Gibbins, S. Paul, and T. R. E. Barnes. 2003. Clinical Correlates of Early Medication Adherence: West London First Episode Schizophrenia Study. Acta Psychiatrica Scandinavica 108: 439–46. [Google Scholar] [CrossRef] [PubMed]
- Olfson, Mark, David Mechanic, Stephen Hansell, Carol A. Boyer, James Walkup, and Peter J. Weiden. 2000. Predicting Medication Noncompliance After Hospital Discharge Among Patients With Schizophrenia. Psychiatric Services 51: 216–22. [Google Scholar] [CrossRef] [PubMed]
- O Sarri, Katerina, Siobhan Higgins, and Anthony G. Kafatos. 2005. Are Religions “Healthy”? A Review on Religious Recommendations on Diet and Lifestyle. Human Ecology Special Issue 14: 7–20. [Google Scholar]
- Pargament, Kenneth I., and James W. Lomax. 2013. Understanding and Addressing Religion among People with Mental Illness. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 12: 26–32. [Google Scholar] [CrossRef] [PubMed]
- Perkins, D. O. 2002. Predictors of noncompliance in patients with schizophrenia. Journal of Clinical Psychiatry 63: 1121–28. [Google Scholar]
- Rosmarin, David H., Kenneth I. Pargament, Steven Pirutinsky, and Annette Mahoney. 2010. A Randomized Controlled Evaluation of a Spiritually Integrated Treatment for Subclinical Anxiety in the Jewish Community, Delivered via the Internet. Journal of Anxiety Disorders 24: 799–808. [Google Scholar] [CrossRef] [PubMed]
- Stahler, Gerald J., Kimberly C. Kirby, and MaryLouise E. Kerwin. 2007. A Faith-Based Intervention for Cocaine-Dependent Black Women. Journal of Psychoactive Drugs 39: 183–90. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, Richard Jed. 1991. Neuroleptics and the Natural Course of Schizophrenia. Schizophrenia Bulletin 17: 325–51. [Google Scholar] [CrossRef] [PubMed]
- Zivin, Kara, and Helen C. Kales. 2008. Adherence to Depression Treatment in Older Adults: A Narrative Review. Drugs & Aging 25: 559–71. [Google Scholar]
- Zolnierek, Kelly B. Haskard, and M. Robin Dimatteo. 2009. Physician Communication and Patient Adherence to Treatment: A Meta-Analysis. Medical Care 47: 826–34. [Google Scholar] [CrossRef] [PubMed]
| Mental Illness | Study | N of pts | Study Design | Tx / Exposure | Outcome | Effect |
|---|---|---|---|---|---|---|
| Depression | Koenig 2015 | 132 | RCT* | religiously integrated cognitive behavioral therapy | adherence | no association |
| Anxiety | Rosmarin 2010 | 125 | randomized controlled evaluation | spiritually integrated treatment | perceptions of treatment, treatment completion | positive |
| Schizophrenia | Huguelet 2011 | 78 | RCT | traditional treatment and a religious and spiritual assessment | treatment compliance | no association, better attendance |
| Huguelet 2006 | 100 | survey | religious beliefs | Synergy with psychiatric care | no association | |
| Caqueo-Urízar A 2015 | 253 | survey | religious beliefs about causes of schizophrenia | medication attitudes | negative | |
| Mohr 2012 | 276 | survey | religious coping | compatibility with psychiatric treatment | positive | |
| McCann 2008 | 81 | survey | religious beliefs/activities | neuroleptic taking | no association | |
| Kirov 1998 | 52 | survey | religious faith after psychosis | compliance | positive | |
| Borras 2007 | 103 | survey | religious and spiritual activities | blood level of the drug | negative | |
| D’Souza 2004 | 2 | case series | SACBT (spirituality augmented) | treatment collaboration/relapse rate | positive | |
| Addiction | Krentzman 2013 | 364 | cohort | spirituality dimensions | AA participation | positive |
| Kelly 2011 | 1726 | cohort | spirituality religiousness | AA attendance | positive | |
| Arnold 2002 | 68 | survey | spirituality | expectations/perceptions | positive | |
| Brown 2001 | 71 | cohort | measures of religiosity | attendance | no association | |
| Stahler 2007 | 18 | RCT | Church communities | treatment retention | positive | |
| Chi 2009 | 357 | cohort | 12-step/religiosity co-variate | abstinence | positive | |
| Margolin 2006 | 72 | controlled study | 3-S (Spiritual Self Schema therapy) | motivation for HIV prevention | positive | |
| Christo 1995 | 101 | cohort | spiritual beliefs | NA (narcotics anonymous) attendance | no association | |
| Mental Illness | Foulks 1986 | 60 | cohort | patients' beliefs | compliance | no association |
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zagożdżon, P.; Wrotkowska, M. Religious Beliefs and Their Relevance for Treatment Adherence in Mental Illness: A Review. Religions 2017, 8, 150. https://doi.org/10.3390/rel8080150
Zagożdżon P, Wrotkowska M. Religious Beliefs and Their Relevance for Treatment Adherence in Mental Illness: A Review. Religions. 2017; 8(8):150. https://doi.org/10.3390/rel8080150
Chicago/Turabian StyleZagożdżon, Paweł, and Magdalena Wrotkowska. 2017. "Religious Beliefs and Their Relevance for Treatment Adherence in Mental Illness: A Review" Religions 8, no. 8: 150. https://doi.org/10.3390/rel8080150





