3. Results
3.1. Phase 1—Chronic Disease Patients’ Characteristics
A sample of 200 patients having 293 chronic disease criteria was obtained. Accordingly, 135 patients had one single chronic disease criteria and 65 patients had two to four chronic disease criteria. Chronic diseases were classified as cardiovascular disease (n = 178), malignant disease (n = 46), pulmonary disease (n = 43), hepatic disease (n = 9), renal disease (n = 6), neurologic disease (n = 6), autoimmune disease (n = 4), and HIV/AIDS (n = 1).
Chronic disease patients had a median age of 69 years (interquartile range or IQR = 18), with their ages being between 28 and 97 years old. The male to female ratio was 1.22 and there were no statistically significant age differences between men and women.
3.2. Phase 2—Palliative Patient’s Characteristics
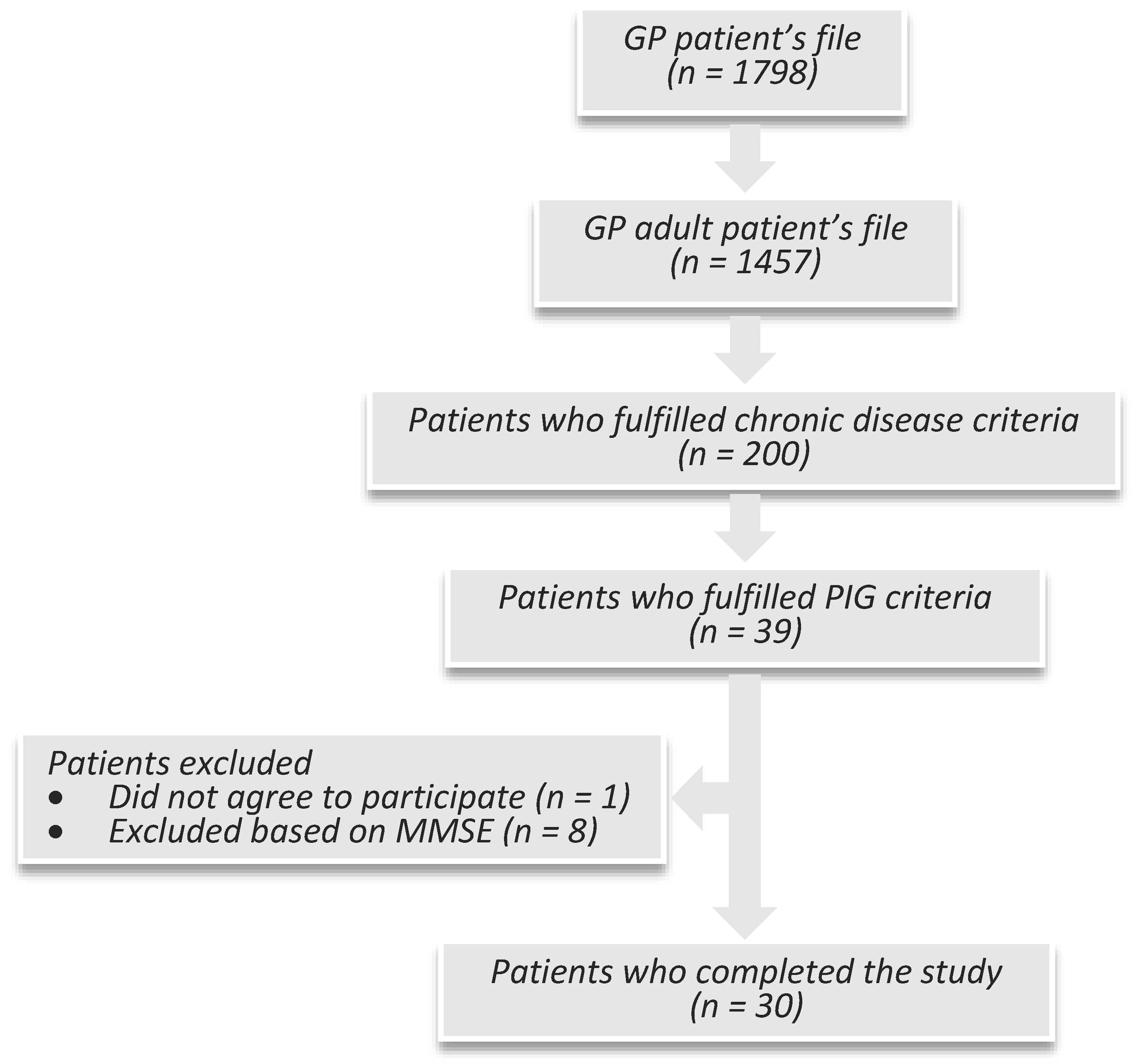
A sample of 39 patients, eligible from those with chronic disease, fulfilled the PIG criteria. One patient did not consent to participate, resulting in a response rate of 97%. Eight patients were excluded by MMSE. A total of 30 patients were enrolled in the study (
Figure 1).
The researcher had negative answers to the PIG surprise question “Would you be surprised if this patient were to die in the next few months, weeks, days?” in five patients, namely: a 34-year-old male with AIDS and plasmablastic non-Hodgkin lymphoma stage IIIB; a 43-year-old female with metastatic colon adenocarcinoma of Dukes C stage; a 77-year-old male with Parkinson’s disease, hyperthyroidism, congestive heart disease stage III NYHA, chronic kidney disease stage III and atrial fibrillation; a 91-year-old female with congestive heart disease stage IV NYHA, previous stroke and previous myocardial infarction; and a 92-year-old male with congestive heart disease stage III NYHA, COPD Gold III/stage C and peripheral artery disease.
The researcher identified PIG general indicators of decline in 25 patients, namely: significant co-morbidity (n = 21); advanced disease (n = 16); general physical decline (n = 8); repeated or unplanned crisis admissions (n = 4); decreasing reversibility or decreasing response to treatments (n = 3); decreasing activity (n = 3); increasing need for support (n = 2); and progressive weight loss above 10% (n = 2). Nineteen of these 25 patients (76%) had more than one general indicator of decline.
Palliative patients included in the study (n = 30) had a median age of 77 (IQR = 16), with their ages being between 34 and 91 years. The male to female ratio was 1.5 and there were no statistically significant age differences between men and women. Most palliative patients were married or living together (67%), while the remainder were widowed (23%) or single (10%). Most had a low–medium socioeconomic status (87%), a low educational level (94% had four or fewer years of education), and were retired (90%). These socioeconomic–educational results reflect an aged sample from a village in Portugal, as it was about half a century ago that people had no proper access to education.
3.3. Prevalence of Depression and Spiritual Distress
The prevalence of depression was 23% (n = 7) in this sample. The semi-structured clinical interview identified seven patients with depression. There were scores of ≥ 11 in the depression subscale in eight patients, meaning probable depression. One of these patients, a woman aged 91, had recently broken her left arm. In this case, the researcher and family physician who previously knew her clinically classified her sadness as an adjustment reaction instead of depression. The agreement between a diagnosis of clinical depression and results of the depression subscale was 87.5%. The prevalence of spiritual distress was 23% (n = 7) in this sample. Depression and spiritual distress criteria co-occurred in four patients (13%).
3.4. Spiritual Distress Palliative Patient's Defining Characteristics
In the present study, all palliative patients with spiritual distress diagnosis had more than one defining characteristic of spiritual distress (
Table 1).
Anger (towards God/divinity or in general), grief, and regret, as well as the need for forgiveness, were the most important defining characteristics in this sample. Additionally, the researcher observed major past traumatic life events in four patients (57%) with spiritual distress, such as a false allegation of paternity with major implications, a loss of a young spouse from gunfire homicide, a loss of a young husband, and the loss of a son from suicide. These patients were the 57-year-old male, 68-year-old male, 74-year-old female, and 75-year-old male. Patients with major past traumatic life events presented more defining characteristics of spiritual distress, particularly grief, and three of them (75%) had a diagnosis of alcoholic use disorder.
3.5. Depression Palliative Patient's Characteristics
There were seven palliative patients with a depressive disorder, namely: major depressive disorder (n = 2), depressive disorder secondary to Parkinson’s disease (n = 2), depressive disorder secondary to stroke (n = 1), persistent depressive disorder/dysthymia (n = 1), and adjustment disorder with depressed mood (n = 1). Alcoholism was observed in one palliative patient with a depressive disorder, who additionally had a comorbidity of spiritual distress.
3.6. Statistical Analysis
A significantly positive association between depression and a lack of meaning in life was found, although the association between depression and expression of suffering was not statistically significant (1A) (
Table 2).
Palliative patients with depression had significantly lower FACIT-Sp scores than those who did not have depression (2A) (
Table 3). However, the lowest FACIT-Sp scores were associated with the use of sedative or anxiolytic medication (4A), but not with the use of antidepressants (3A) (
Table 3).
Accordingly, a significant association between spiritual distress and the use of sedative or anxiolytic medication was found, although spiritual distress was not significantly correlated with the use of antidepressants (6A) (
Table 4).
A significantly negative correlation was found for FACIT-Sp scores with HADS-D and HADS-T scores, although this was not found for HADS-A scores (7A) (
Table 5).
Moreover, spiritual distress was found to not be associated with HADS scores (6B) (
Table 6).
A significant association was found between alcoholism and spiritual distress diagnosis (6C), although this association was not found with depression (5A) (
Table 7). Alcoholism had been codified by ICPC-2 with a code of “P15—Chronic alcohol abuse”. These were patients with alcoholic liver disease.
4. Discussion
This study focused on applying the diagnosis of spiritual distress and depression to the clinical setting, based on their definitions and using selected related scales. We hypothesized that there would be palliative patients with one clinical diagnosis or neither. Our main objective was to describe the clinical and statistical findings of palliative patients with depression and spiritual distress. Thus, we would identify criteria to make a differential diagnosis. Although the study showed promising results, it also has underlying obstacles and limitations that need to be addressed.
The prevalence of depression in the sample (23%) is similar to that described in previous research. A systematic review conducted in 2002 summarized the prevalence of depression in advanced diseases according to HADS definition (score on the depression subscale of > 10) as being 29% (IQR = 19.50–34.25%). In comparison, according to psychiatric interviews, values fluctuated between 5% and 26% (a median of 15%) (
Hotopf et al. 2002). A more recent meta-analysis, from 2011, found a prevalence of depression defined by the DSM or International Classification of Diseases (ICD) criteria of 16.5% (95% confidence interval of 13.1–20.3) in palliative care settings and of 16.3% (13.4–19.5%) in oncologic and hematologic settings (
Mitchell et al. 2011). Previous research describes a prevalence of spiritual distress varying between 28% and 44% in oncology and palliative patients (
Delgado-Guay et al. 2011;
Hui et al. 2011;
Blanchard et al. 2012). In this sample, the prevalence of spiritual distress was 23%. To our knowledge, this is the first study to describe the prevalence of spiritual distress in palliative patients in primary care.
A significant proportion of palliative patients in the sample had a mixed diagnosis of depression and spiritual distress (13%). Previous research showed that elderly patients admitted to geriatric rehabilitation with significant depressive symptoms might be especially vulnerable to concomitant spiritual distress. In that sample, the proportion of elderly patients with mixed depressive symptoms and spiritual distress was 15.1%, which is similar to our results (
Bornet et al. 2015).
Depression was also found to be positively and significantly related to a lack of meaning in life. Swinton states that “depression is a profound spiritual illness that digs into the heart of a person´s spirit and forces them to face experiences of meaninglessness and hopelessness” (
Swinton 2001, p. 167). It seems that previous qualitative and quantitative research suggests meaning in life is a core aspect of the human person (
Frankl 1992) and a lack of this dimension might be related to depression (
Swinton 2001;
Guerrero-Torrelles et al. 2017), addiction (
White et al. 2006;
Krentzman et al. 2015) and spiritual distress (
Caldeira et al. 2015;
Villagomeza 2005). However, the present study does not explain the nature and direction of the causal relationship between depression and a lack of meaning in life. A recent systematic review about meaning interventions among patients with advanced diseases states a core component of all the interventions was “the interpersonal encounter between patient and therapist, in which sources of meaning were explored and a sense of connectedness was re-established” (
Guerrero-Torrelles et al. 2017, p. 1). Logotherapeutic approaches led to the same results (
Robatmili et al. 2015). In European patients with advanced cancer, interpersonal relationships were reported as the area that provides more meaning in life to these patients (
Tomas-Sabado et al. 2015). Among patients with advanced diseases, having a sense of meaning in life is a buffer against depression and the wish to hasten death (
Guerrero-Torrelles et al. 2017). In the general population, interventions increasing gratitude and meaning in life facilitate the remission of depression (
Disabato et al. 2016).
In accordance with previous literature, the present study found depression to be related to a lack of spiritual well-being. On the whole, depression is related to a lack of spiritual well-being as it relates to a lack of meaning in life, which is a spiritual dimension of the human being (
Swinton 2001).
Conversely, in the present study, a lack of spiritual well-being was associated with the use of sedative or anxiolytic medication but not with the use of antidepressants. Although both depression and spiritual distress are associated with lower scores in the FACIT-Sp scale, the FACIT-Sp is a more accurate scale to measure the spiritual dimension compared with the emotional dimension of the human being (
Peterman et al. 2002). Therefore, this finding is probably a result of the observed association between spiritual distress and the use of sedative or anxiolytic medication.
A diagnosis of spiritual distress was obtained through three component criteria, which included the patient and the researcher report in addition to a FACIT-Sp score below 36. Recent research considered that the patient’s self-report of having spiritual distress and a lower result in a spiritual well-being scale, namely the Spiritual Well-Being Questionnaire, is an accurate resource for measuring spiritual distress (
Caldeira et al. 2017). Therefore, depression and spiritual distress correspond to distinct dimensions despite being related and might require different therapeutic interventions (
Bornet et al. 2015).
Other than a lack of meaning in life and expression of suffering, the most frequent defining characteristics for spiritual distress observed in the present sample were anger (towards God/divinity or in general), grief, and regret, as well as the need for forgiveness. Sedative or anxiolytic medication might be a means of muting the patient’s spiritual suffering. “A man’s concern, even his despair, over the worthwhileness of life is a spiritual distress but by no means a mental disease. It may well be that interpreting the first in terms of the latter motivates a doctor to bury his patient’s existential despair under a heap of tranquilizing drugs. It is his task, rather, to pilot the patient through his existential crises of growth and development” (
Frankl 1985, p. 125). However, the use of anxiolytic/sedative medication can also be a supportive and therapeutic measure until the patient overcomes his spiritual suffering.
The researcher observed the occurrence of major past traumatic life events in four patients (57%) with spiritual distress, who presented more defining characteristics of spiritual distress compared with the other patients with spiritual distress. Other defining characteristics of spiritual distress observed in this subset group of patients were grief, anger (towards God/divinity or in general), need for forgiveness and alienation. Additional studies on the subject might aid in the acknowledgement of spiritual distress.
As previously discussed, through the application of FACIT-Sp scale and DSM-5 criteria, we found a lack of spiritual well-being to be related to depression. Consequently, FACIT-Sp was found to be negatively related to HADS-D and HADS-T. The interesting finding was the lack of association between FACIT-Sp scores and HADS-A. Although depression and anxiety commonly co-occur, share several physical (e.g., insomnia, weight loss) and emotional features (e.g., stress and unrest) as well as having common underlying physiologic processes (
Kreitler et al. 2017), they are distinct pathologies exhaustively described in the DSM-5 classification. A recent study aimed at contributing to the clarification of the distinctiveness of anxiety and depression in terms of their cognitive characteristics, as reflected in their tendencies to assign meaning, concluded that anxiety and depression were different constructs, as the “anxiety profile indicated more focusing on one’s internal world whereas the depression profile indicated focusing both on the personal and the interpersonally-shared reality” (
Kreitler et al. 2017, p. 1).
In the present study, HADS was not significantly associated with a diagnosis of spiritual distress. Apart from the similarities between depression and spiritual distress, they seem to represent distinct dimensions, as highlighted by Frankl and Bornet (
Frankl 1985;
Bornet et al. 2015).
In the present study, a significantly positive association was found between spiritual distress and alcoholism, which implicitly involved an expression of suffering and a lack of meaning in life. As emphasized by Gerwood, clients with addiction try to fill their existential vacuum with alcohol and other drugs (
Gerwood 1998;
Kleftaras and Katsogianni 2012), which makes them excellent candidates for understanding the concept of the existential vacuum as described by Frankl (a dimension of the meaning of life construct that encapsulates the failure of a person to experience meaning in life) (
Frankl 1968). Alcoholics have a lower sense of meaning in life than non-alcoholics, with their sense of life purpose increasing during treatment programs for alcohol addiction (
White et al. 2006;
Kleftaras and Katsogianni 2012). Patients with alcoholism find meaning in survival, self-reclamation, service to others, and connections to the community (
White et al. 2006).
It seems that qualitative and quantitative research suggests a meaning in life is a core aspect of the human person and a lack of this dimension might be related to depression, addiction, and spiritual distress. Conversely, depression has been associated with alcohol use disorder, especially in older people (
Conner et al. 2009). Furthermore, previous research suggests that elderly patients with significant depressive symptoms might be more vulnerable to spiritual distress (
Bornet et al. 2015). A recent study of alcoholics showed higher levels of feelings of emptiness in those with higher levels of depressive symptomatology (
Kleftaras and Katsogianni 2012). Although depression and spiritual distress can co-occur, there is a gap in the research about the prevalence of spiritual distress in alcoholic use disorder.
The present study was designed toward differentiating depression from spiritual distress, which might have made possible the observed relation between alcoholism and spiritual distress but not with depression. Considering the theoretical and practical relations between spiritual distress and a lack of meaning in life (
Caldeira et al. 2015;
Villagomeza 2005) as well as between lack of meaning in life and alcoholism (
White et al. 2006;
Krentzman et al. 2015), the findings of the present study have a theoretical background. The observed relationship between spiritual distress and alcoholism might create an opportunity for practical research in the field.
This study underlines the importance of assessing spiritual distress in palliative patients, particularly in primary care. Primary health care professionals are at a privileged position in the delivery of care. Proximity to the patients and their family in addition to continuity of care are common issues in palliative and primary care. Recognizing spiritual distress as well as introducing guided mental and holistic care and referrals to the proper spiritual, social, or other health care facilities, including palliative care, can promote better quality of life for palliative patients at an earlier phase.
5. Conclusions
This study aimed to identify the prevalence in addition to the clinical indicators of depression and spiritual distress in palliative patients in primary care. Depression and spiritual distress seem to both be linked to the spiritual dimension of the human being, but seem to differ in the dimensions of suffering and the pharmacological treatment.
This study has three important findings: (1) apart from being associated with a lack of spiritual well-being, depression seems to be related to a lack of meaning in life, which is a core aspect of spiritual distress. Therefore, if this is true, depression is also a spiritual experience as having a meaning in life is a transcendent, personal, and unique experience; (2) depression seems to differ from spiritual distress, at least in two clinical indicators: there seems to be an association between relevant traumatic life events and spiritual distress. Furthermore, spiritual distress seems to be associated with alcoholism, although this was not seen for depression; (3) medical treatment for spiritual distress seems more prone to the use of anxiolytic medication instead of antidepressants.
The study is limited by its cross-sectional design and the small sample size will greatly reduce the validity and generalizability of the study findings and is a significant weakness of this investigation. The participants’ educational background might have yielded some bias during filling in the questionnaires, although some assistance in readings had been provided by personal assistants. Conclusions should be understood in this sample and context.
The authors believe the paper suggests two possible clinical markers of spiritual distress: alcoholism and past traumatic life events. The association between the use of anxiolytic medication and spiritual distress in primary care palliative patients will need to be further studied and, if so confirmed, there needs to be an examination of the proper class or drug that works best for this clinical entity. Palliative patients’ depression and spiritual distress need to be precisely identified for correct decision-making in addition to pinpointing the most effective treatment and holistic care. Further research, including broader samples and different cultural backgrounds, is needed.