Measuring Spirituality and Religiosity in Clinical Settings: A Scoping Review of Available Instruments
Abstract
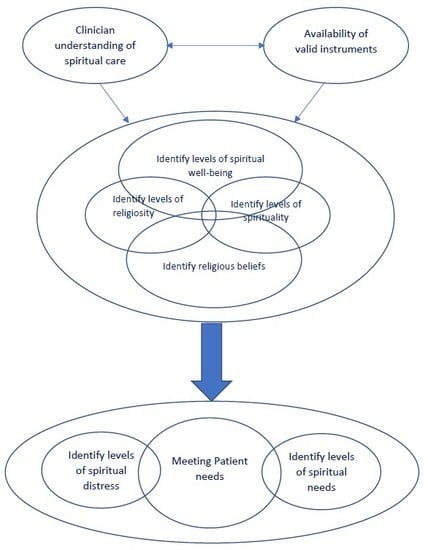
:1. Introduction
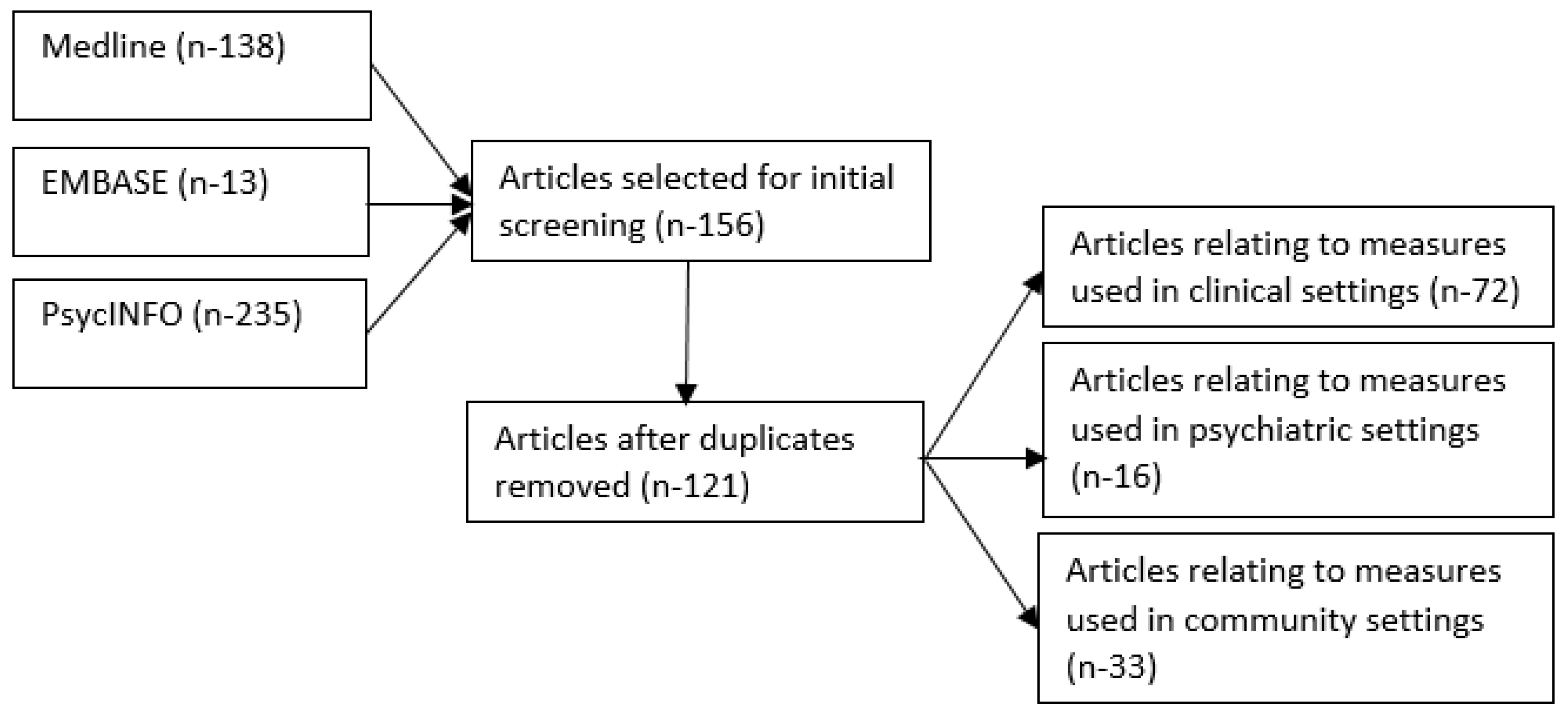
2. Methods
3. Results
4. Self-Reporting Measures (Spiritual and Religious Well-Being)
5. Self-Reporting Measures (Spiritual Needs and Distress)
- The BENEFIT Through spirituality/religiosity scale (chronic diseases and spinal cord injury) (Bussing and Koenig 2008; Xue et al. 2016),
- The Brief Pictorial Instrument for Assessing Spirituality (primary care patients) (McBride et al. 1998b),
- The Spirituality Scale (cardiovascular disease and chronic disease patients) (Delaney 2005; Delaney et al. 2011),
- The Index of Core Spiritual Experience (primary care and hospital outpatients) (McBride et al. 1998a; VandeCreek et al. 1995),
- The Ironson–Wood Spirituality/Religiosity Index (HIV and chronic heart failure patients) (Bekelman et al. 2010; Ironson et al. 2002; Mistretta et al. 2017)
- The Brief Multidimensional Measure of Religion and Spirituality (hospital inpatients) (Curcio et al. 2015; Johnstone et al. 2009)
- The Daily Spiritual Experience Scale (surgical, hospice care and HIV patients) (Kimura et al. 2012; Oji et al. 2017; Steinhauser et al. 2008)
- The Brief Serenity Scale (post-transplant patients (Kreitzer et al. 2009)
- The Spiritual Needs Inventory (Hermann 2006; Buck and McMillan 2012)
- The Spiritual Distress Assessment Tool (SDAT) (Monod et al. 2010, 2012a)
- The Advance Cancer Patients’ Distress Scale (Fischbeck et al. 2013)
- The Spiritual Care Competence Scale (Van Leeuwen et al. 2009)
6. Clinician-Administered Measures
7. Self-Reporting Tools Assessing Healthcare Staff Understanding of Spirituality and Spiritual Care
8. Discussion
9. Conclusions
Author Contributions
Conflicts of Interest
References
- Astrow, Alan B., Rashmi K. Sharma, Yiwu Huang, Yiquing Xu, and Daniel P. Sulmasy. 2012. A Chinese version of the Spiritual Needs Assessment for patients survey instrument. Journal of Palliative Medicine 15: 1297–315. [Google Scholar] [CrossRef] [PubMed]
- Astrow, Alan B., Gary Kwok, Rashmi K. Sharma, and Daniel Sulmasy. 2015. Spiritual needs and patient satisfaction in multi-cultural patient population. Journal of Clinical Oncology 33: e20589. [Google Scholar]
- Austin, Philip D., Roderick Macleod, Philip J. Siddall, Wilf McSherry, and Richard Egan. 2016. The Ability of Hospital Staff to Recognize and Meet Patients’ Spiritual Needs: A Pilot Study. Journal for the Study of Spirituality 6: 20–37. [Google Scholar] [CrossRef]
- Austin, Philip, Roderick Macleod, Philip Siddall, Wilf McSherry, and Richard Egan. 2017. Spiritual care training is needed for clinical and non-clinical staff to manage patients’ spiritual needs. Journal for the Study of Spirituality 7: 50–63. [Google Scholar] [CrossRef]
- Balboni, Michael J., Adam Sullivan, Adaugo Amobi, Andrea C. Phelps, Daniel P. Gorman, Angelika Zollfrank, John R. Peteet, Holly G. Prigerson, Tyler J. VanderWeele, and Tracy A. Balboni. 2013. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. Journal of Clinical Oncology 31: 461–67. [Google Scholar] [CrossRef]
- Baumsteiger, Rachel, and Tiffany Chenneville. 2015. Challenges to the Conceptualization and Measurement of Religiosity and Spirituality in Mental Health Research. Journal of Religion and Health 54: 2344–54. [Google Scholar] [CrossRef] [PubMed]
- Becker, Penny Edgell, and Pawan H. Dhingra. 2001. Religious involvement and volunteering: Implications for civil society. Sociology of Religion 62: 315–35. [Google Scholar] [CrossRef]
- Bekelman, David B., Carla Parry, Farr A. Curlin, Traci E. Yamashita, Diane L. Fairclough, and Frederick S. Wamboldt. 2010. A comparison of two spirituality instruments and their relationship with depression and quality of life in chronic heart failure. Journal of Pain and Symptom Management 39: 515–26. [Google Scholar] [CrossRef] [PubMed]
- Buck, Harleah G., and Susan C. McMillan. 2012. A psychometric analysis of the spiritual needs inventory in informal caregivers of patients with cancer in hospice home care. Oncology Nursing Forum 39: E332–9. [Google Scholar] [CrossRef] [PubMed]
- Bussing, Arndt, and Harold G. Koenig. 2008. The BENEFIT through spirituality/religiosity scale—A 6-item measure for use in health outcome studies. The International Journal of Psychiatry in Medicine 38: 493–506. [Google Scholar]
- Büssing, Arndt, and Harold G. Koenig. 2010. Spiritual Needs of Patients with Chronic Diseases. Religions 1: 18. [Google Scholar] [CrossRef]
- Büssing, Arndt, and Daniela Rodrigues Recchia. 2016. Spiritual and Non-spiritual Needs Among German Soldiers and Their Relation to Stress Perception, PTDS Symptoms, and Life Satisfaction: Results from a Structural Equation Modeling Approach. Journal of Religion and Health 55: 747–64. [Google Scholar] [CrossRef] [PubMed]
- Büssing, Arndt, Hans J. Balzat, and Peter Heusser. 2010. Spiritual needs of patients with chronic pain diseases and cancer—validation of the spiritual needs questionnaire. European Journal of Medical Research 15: 266–73. [Google Scholar] [CrossRef]
- Bussing, A., Xiao F. Zhai, Wen B. Peng, and Chang Q. Ling. 2013. Psychosocial and spiritual needs of patients with chronic diseases: Validation of the Chinese version of the Spiritual Needs Questionnaire. Journal of Integrative Medicine 11: 106–15. [Google Scholar] [CrossRef] [PubMed]
- Büssing, Arndt, Andreas Günther, Klaus Baumann, Eckhard Frick, and Christoph Jacobs. 2013. Spiritual Dryness as a Measure of a Specific Spiritual Crisis in Catholic Priests: Associations with Symptoms of Burnout and Distress. Evidence-Based Complementary and Alternative Medicine 2013: 10. [Google Scholar] [CrossRef] [PubMed]
- Büssing, Arndt, Annina Janko, Klaus Baumann, Niels Christian Hvidt, and Andreas Kopf. 2013. Spiritual Needs among Patients with Chronic Pain Diseases and Cancer Living in a Secular Society. Pain Medicine 14: 1362–73. [Google Scholar] [CrossRef] [PubMed]
- Büssing, Arndt, Undine Waßermann, Niels Christian Hvidt, Alfred Laengler, and Michael Thiel. 2017. Spiritual needs of mothers with sick new born or premature infants—A cross sectional survey among German mothers. Women and Birth: Journal of the Australian College of Midwives. [Google Scholar] [CrossRef]
- Büssing, Arndt, Daniela R. Recchia, Harold Koenig, Klaus Baumann, and Ecjhard Frick. 2018. Factor Structure of the Spiritual Needs Questionnaire (SpNQ) in Persons with Chronic Diseases, Elderly and Healthy Individuals. Religions 9: 13. [Google Scholar] [CrossRef]
- Cetinkaya, Bengü, Sebahat Dundar, and Arife Azak. 2013. Nurses’ perceptions of spirituality and spiritual care. Australian Journal of Advanced Nursing 31: 5–10. [Google Scholar]
- Chiang, Yi-chien, Hsiang-chun Lee, Tsung-lan Chu, Chin-yen Han, and Ya-chu Hsiao. 2017. Psychometric Testing of a Religious Belief Scale. The Journal of Nursing Research: JNR 25: 419–28. [Google Scholar] [CrossRef] [PubMed]
- Colquhoun, Heather L., Danielle Levac, Kelly K. O’Brien, Sharon Straus, Andrea C. Tricco, Laure Perrier, Monika Kastner, and David Moher. 2014. Scoping reviews: Time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology 67: 1291–94. [Google Scholar] [CrossRef] [PubMed]
- Cotton, Sian, Christina M. Puchalski, Susan N. Sherman, Joseph M. Mrus, Amy H. Peterman, Judith Feinberg, Kenneth I. Pargament, Amy C. Justice, Anthony C. Leonard, and Joel Tsevat. 2006. Spirituality and Religion in Patients with HIV/AIDS. Journal of General Internal Medicine 21: S5–S13. [Google Scholar] [CrossRef] [PubMed]
- Curcio, Cristiane S., Giancarlo Lucchetti, and Alexander Moreira-Almeida. 2015. Validation of the Portuguese version of the Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS-P) in clinical and non-clinical samples. Journal of Religion and Health 54: 435–48. [Google Scholar] [CrossRef]
- Daaleman, Timothy P., and Bruce B. Frey. 2004. The Spirituality Index of Well-Being: A New Instrument for Health-Related Quality-of-Life Research. Annals of Family Medicine 2: 499–503. [Google Scholar] [CrossRef] [PubMed]
- Daaleman, Timothy P., Bruce B. Frey, Dennise Wallace, and Stephanie A. Studenski. 2002. Spirituality Index of Well-Being Scale: Development and testing of a new measure. The Journal of Family Practice 51: 952. [Google Scholar] [PubMed]
- De Araujo Toloi, Diego, Deise Uema, Felipe Matsushita, Paulo Antonio da Silva Andrade, Tiago Pugliese Branco, Fabiana Tomie Becker de Carvalho Chino, Raquel Bezerra Guerra, Túlio Eduardo Flesch Pfiffer, Toshio Chiba, Rodrigo Santa Cruz Guindalini, and et al. 2016. Validation of questionnaire on the Spiritual Needs Assessment for Patients (SNAP) questionnaire in Brazilian Portuguese. Ecancermedicalscience [Internet] 10: 1–694. [Google Scholar] [CrossRef] [PubMed]
- De Araujo Toloi, Diego, Deise Uema, Felipe Matsushita, Paulo Antonio da Silva Andrade, Tiago Pugliese Branco, Fabiana Tomie Becker de Carvalho Chino, Raquel Bezerra Guerra, Túlio Eduardo Flesch Pfiffer, Toshio Chiba, Rodrigo Santa Cruz Guindalini, and et al. 2016b. Validation of questionnaire on the Spiritual Needs Assessment for Patients (SNAP) questionnaire in Brazilian Portuguese. Ecancermedicalscience 10: 694. [Google Scholar] [CrossRef] [PubMed]
- Delaney, Colleen. 2005. The Spirituality Scale: Development and psychometric testing of a holistic instrument to assess the human spiritual dimension. Journal of Holistic Nursing 23: 145–67, discussion 68–71. [Google Scholar] [CrossRef]
- Delaney, Colleen, Cynthia Barrere, and Mary Helming. 2011. The influence of a spirituality-based intervention on quality of life, depression, and anxiety in community-dwelling adults with cardiovascular disease: A pilot study. Journal of Holistic Nursing: Official Journal of the American Holistic Nurses’ Association 29: 21–32. [Google Scholar] [CrossRef] [PubMed]
- Erichsen, Nora-Beata, and Arndt Büssing. 2013. Spiritual Needs of Elderly Living in Residential/Nursing Homes. Evidence-Based Complementary and Alternative Medicine 2013: 10. [Google Scholar] [CrossRef] [PubMed]
- Exline, Julie J., Kenneth I. Pargament, Joshua B. Grubbs, and Ann Marie Yali. 2014. The Religious and Spiritual Struggles Scale: Development and initial validation. Psychology of Religion and Spirituality 6: 208–22. [Google Scholar] [CrossRef]
- Fallahi Khoshknab, Masoud, Monir Mazaheri, Sadat S.B. Maddah, and Mehdi Rahgozar. 2010. Validation and reliability test of Persian version of The Spirituality and Spiritual Care Rating Scale (SSCRS). Journal of Clinical Nursing 19: 2939–41. [Google Scholar] [CrossRef] [PubMed]
- Fernander, Anita, John F. Wilson, Michele Staton, and Carl Leukefeld. 2004. An exploratory examination of the Spiritual Well-Being Scale among incarcerated black and white male drug users. International Journal of Offender Therapy and Comparative Criminology 48: 403–13. [Google Scholar] [CrossRef] [PubMed]
- Fischbeck, Sabine, Bernd O. Maier, Ulrike Reinholz, Cornelia Nehring, Rainer Schwab, and Manfred E. Beutel. 2013. Assessing somatic, psychosocial, and spiritual distress of patients with advanced cancer: Development of the Advanced Cancer Patients’ Distress Scale. The American Journal of Hospice & Palliative Care 30: 339–46. [Google Scholar]
- Genia, Vickly. 2001. Evaluation of the Spiritual Well-Being Scale in a Sample of College Students. The International Journal for the Psychology of Religion 11: 25–33. [Google Scholar]
- Gherghina, Viorel, I. Cindea, R. Popescu, and A. Balcan. 2014. Spiritual distress assessment tool a valid instrument for elderly patients in the perioperative period: 18AP3-7. European Journal of Anaesthesiology 31: 267. [Google Scholar] [CrossRef]
- Ghodsbin, Fariba, Marzieh Safaei, Iahanbin Jahanbin, Mohammed A. Ostovan, and Sareh Keshvarzi. 2015. The effect of positive thinking training on the level of spiritual well-being among the patients with coronary artery diseases referred to Imam Reza specialty and subspecialty clinic in Shiraz, Iran: A randomized controlled clinical trial. ARYA Atherosclerosis 11: 341–48. [Google Scholar] [PubMed]
- Hatch, Robert L., Mary A. Burg, Debra S. Naberhaus, and Linda K. Hellmich. 1998. The Spiritual Involvement and Beliefs Scale. Development and testing of a new instrument. The Journal of Family Practice 46: 476–86. [Google Scholar] [PubMed]
- Hermann, Carla. 2006. Development and testing of the spiritual needs inventory for patients near the end of life. Oncology Nursing Forum 33: 737–44. [Google Scholar] [CrossRef] [PubMed]
- Hill, Peter C., and Kenneth I. Pargament. 2003. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. The American Psychologist 58: 64–74. [Google Scholar] [CrossRef] [PubMed]
- Hood, Ralph W., and Bernard Spilka. 2003. The Psychology of Religion: An Empirical Approach, 3rd ed. New York: Guilford Press. [Google Scholar]
- Hyman, Corine, and Paul J. Handal. 2006. Definitions and Evaluation of Religion and Spirituality Items by Religious Professionals: A Pilot Study. Journal of Religion and Health 45: 264–82. [Google Scholar] [CrossRef]
- Ironson, Gail, George F. Solomon, Elizabeth G. Balbin, Conall O’Cleirigh, Annie George, Mahendra Kumar, David Larson, and Teresa E. Woods. 2002. The Ironson-woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine 24: 34–48. [Google Scholar] [CrossRef]
- Johnstone, Brick, Dong P. Yoon, Kelly L. Franklin, Laura Schopp, and Joseph Hinkebein. 2009. Re-conceptualizing the factor structure of the brief multidimensional measure of religiousness/spirituality. Journal of Religion and Health 48: 146–63. [Google Scholar] [CrossRef]
- Kimura, Miako, Acacia L. de Oliveira, Lina S. Mishima, and Lynn G. Underwood. 2012. Cultural adaptation and validation of the Underwood’s Daily Spiritual Experience Scale—Brazilian version. Revista da Escola de Enfermagem da U S P 46: 99–106. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G. 2009. Research on religion, spirituality, and mental health: A review. Canadian Journal of Psychiatry Revue Canadienne de Psychiatrie 54: 283–91. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G. 2012. Religion, Spirituality, and Health: The Research and Clinical Implications. ISRN Psychiatry 2012: 33. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G., Nathan A. Boucher, and Michelle J. Pearce. 2017. Rationale for Spiritually Oriented Cognitive Processing Therapy for Moral Injury in Active Duty Military and Veterans with Posttraumatic Stress Disorder. The Journal of Nervous and Mental Disease 205: 147–53. [Google Scholar] [PubMed]
- Kouloulias, Vassilis, John Kokakis, Nikolaos Kelekis, and John Kouvaris. 2017. A New Questionnaire (QRFPC25) Regarding the Religiosity and Spirituality in People with Life-Threatening Disease: Reliability and Validity in a Population of Cancer Patients Undergoing Radiotherapy. Journal of Religion and Health 56: 1137–54. [Google Scholar] [CrossRef]
- Kreitzer, Mary J., Cynthia R. Gross, On A. Waleekhachonloet, Maryanne Reilly-Spong, and Marcia Byrd. 2009. The brief serenity scale: A psychometric analysis of a measure of spirituality and well-being. Journal of Holistic Nursing 27: 7–16. [Google Scholar] [CrossRef]
- Ku, Ya L., Shih M. Kuo, and Ching Y. Yao. 2010. Establishing the validity of a spiritual distress scale for cancer patients hospitalized in southern Taiwan. International Journal of Palliative Nursing 16: 134–38. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, Giancarlo, Alessandra Lamas Granero Lucchetti, and Homero Vallada. 2013. Measuring spirituality and religiosity in clinical research: A systematic review of instruments available in the Portuguese language. Sao Paulo Medical Journal = Revista paulista de medicina 131: 112–22. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, Rod, Donna M. Wilson, Jackie Crandall, and Phil Austin. 2017. Death Anxiety among New Zealanders: The Predictive Roles of Religion, Spirituality, and Family Connection. Omega. [Google Scholar] [CrossRef] [PubMed]
- Mateen, Farrah J., Jiwon Oh, Ana I. Tergas, Neil Bhayani, and Biren Bharat Kamdar. 2013. Titles versus titles and abstracts for initial screening of articles for systematic reviews. Clinical Epidemiology 5: 89–95. [Google Scholar] [CrossRef] [PubMed]
- McBride, J.L., G. Arthur, R. Brooks, and L. Pilkington. 1998a. The relationship between a patient’s spirituality and health experiences. Family Medicine 30: 122–6. [Google Scholar]
- McBride, J.L., L. Pilkington, and G. Arthur. 1998b. Development of brief pictorial instruments for assessing spirituality in primary care. The Journal of Ambulatory care Management 21: 53–61. [Google Scholar] [CrossRef]
- McSherry, Wilfred, Peter Draper, and Don Kendrick. 2002. The construct validity of a rating scale designed to assess spirituality and spiritual care. International Journal of Nursing Studies 39: 723–34. [Google Scholar] [CrossRef]
- Mistretta, Erin G., Danetta Sloan, Karlynn BrintzenhofeSzoc, Kathleen M. Weber, and Ann Berger. 2017. Testing domains of the healing experiences in all life stressors questionnaire in a cohort of HIV-infected and HIV-uninfected Chicago women. Psychology Research and Behavior Management 10: 201–8. [Google Scholar] [CrossRef] [PubMed]
- Moeini, Babak, Hadi Zamanian, Zahra Taheri-Kharameh, Tehereh Ramezani, Mohamadhasan Saati-Asr, Mohamadhasan Hajrahimian, and Mohammadali Amini-TehraniMscb. 2018. Translation and Psychometric Testing of the Persian Version of the Spiritual Needs Questionnaire Among Elders with Chronic Diseases. Journal of Pain and Symptom Management 55: 94–100. [Google Scholar] [CrossRef] [PubMed]
- Monod, Stefanie M., Etienne Rochat, Christophe J. Bula, Guy Jobin, Estelle Martin, and Brenda Spencer. 2010. The spiritual distress assessment tool: An instrument to assess spiritual distress in hospitalised elderly persons. BMC Geriatrics 10: 88. [Google Scholar] [CrossRef] [PubMed]
- Monod, Stefanie, Mark Brennan, Etienne Rochat, Estelle Martin, Stephane Rochat, and Chrisotphe J. Büla. 2011. Instruments Measuring Spirituality in Clinical Research: A Systematic Review. Journal of General Internal Medicine 26: 1345–57. [Google Scholar] [CrossRef] [PubMed]
- Monod, Stefanie, Estelle Martin, B. Spencer, Etienne Rochat, and Christophe Bula. 2012. Validation of the Spiritual Distress Assessment Tool in older hospitalized patients. BMC Geriatrics 12: 13. [Google Scholar] [CrossRef] [PubMed]
- Monod, Stepfanie, Estelle Martin, Brenda Spencer, Etienne Rochat, and Christophe Büla. 2012. Validation of the spiritual distress assessment tool in older hospitalized patients. BMC Geriatrics 12: 13. [Google Scholar] [CrossRef] [PubMed]
- Munoz, Alexis R., John M. Salsman, Kevin D. Stein, and David Cella. 2015. Reference Values of the Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being (FACIT-Sp-12): A Report from the American Cancer Society’s Studies of Cancer Survivors. Cancer 121: 1838–44. [Google Scholar] [CrossRef] [PubMed]
- Mystakidou, Kyriaki, Eleni Tsilika, Efi Parpa, M. Smyrnioti, and Lambros Vlahos. 2006. Assessing spirituality and religiousness in advanced cancer patients. The American Journal of Hospice & Palliative Care 23: 457–63. [Google Scholar]
- Mystakidou, Kyriaki, Eleni Tsilika, Efi Parpa, Maria Pathiaki, Elisabeth Patiraki, Antonis Galanos, and Lambros Vlahos. 2007. Exploring the relationships between depression, hopelessness, cognitive status, pain, and spirituality in patients with advanced cancer. Archives of Psychiatric Nursing 21: 150–61. [Google Scholar] [CrossRef] [PubMed]
- Mystakidou, Kyriaki, Eleni Tsilika, Efi Parpa, Ioanna Hatzipli, Marilena Smyrnioti, Antonis Galanos, and Lambros Vlahos. 2008. Demographic and clinical predictors of spirituality in advanced cancer patients: a randomized control study. Journal of Clinical Nursing 17: 1779–85. [Google Scholar] [CrossRef] [PubMed]
- Mystakidou, Kyriaki, Eleni Tsilika, Efi Prapa, Marilena Smyrnioti, Anna Pagoropoulou, and Lambros Vlahos. 2008. Predictors of spirituality at the end of life. Canadian Family Physician Medecin de Famille Canadien 54: 1720–21.e5. [Google Scholar] [PubMed]
- Oji, V.U., L.C. Hung, R. Abbasgholizadeh, Hamilton F. Terrell, E.J. Essien, and E. Nwulia. 2017. Spiritual care may impact mental health and medication adherence in HIV+ populations. HIV/AIDS (Auckland, NZ) 9: 101–109. [Google Scholar] [CrossRef] [PubMed]
- Peterman, Amy H., George Fitchett, Marianne J. Brady, Lesbia Hernandez, and David Cella. 2002. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual well-being scale (FACIT-Sp). Annals of Behavioral Medicine 24: 49–58. [Google Scholar] [CrossRef] [PubMed]
- Puchalski, Christina M. 2001. The role of spirituality in health care. Proceedings (Baylor University Medical Center) 14: 352–57. [Google Scholar] [CrossRef]
- Puchalski, Christina, Betty Ferrell, Rose Virani, Shirley Otis-Green, Pamela Baird, Janet Bull, Harvey Chochinov, George Handzo, Holly Nelson-Becker, Maryjo Prince-Paul, and et al. 2009. Improving the Quality of Spiritual Care as a Dimension of Palliative Care: The Report of the Consensus Conference. Journal of Palliative Medicine 12: 885–904. [Google Scholar] [CrossRef] [PubMed]
- Rasinski, Kenneth A., Y.G. Kalad, J.D. Yoon, and F.A. Curlin. 2011. An assessment of US physicians’ training in religion, spirituality, and medicine. Medical Teacher 33: 944–45. [Google Scholar] [CrossRef] [PubMed]
- Rusa, Suzana Gabriela Rusa, Gabriele Ibanhes Peripato, Sofia Cristina Iost Pavarini, Keika Inouye, Marisa Silvana Zazzetta, and Fabiana de Souza Orlandi. 2014. Quality of life/spirituality, religion and personal beliefs of adult and elderly chronic kidney patients under hemodialysis. Revista Latino-Americana de Enfermagem 22: 911–17. [Google Scholar] [CrossRef] [PubMed]
- Sharma, Rashmi K., Alan B. Astrow, Kenneth Texeira, and Daniel P. Sulmasy. 2012. The Spiritual Needs Assessment for Patients (SNAP): development and validation of a comprehensive instrument to assess unmet spiritual needs. Journal of Pain and Symptom Management 44: 44–51. [Google Scholar] [CrossRef] [PubMed]
- Simao, Talita P., Erika de Cássia Lopes Chaves, Emília Campos de Carvalho, Denismar Alves Nogueira, Camila Csizmar Carvalho, Ya-Li Ku, and Denise Hollanda Iunes. 2016. Cultural adaptation and analysis of the psychometric properties of the Brazilian version of the Spiritual Distress Scale. Journal of Clinical Nursing 25: 231–39. [Google Scholar] [CrossRef] [PubMed]
- Steinhauser, Karen E., Stewart C. Alexander, Ira R. Byock, Linda K. George, Maren K. Olsen, and James A. Tulsky. 2008. Do preparation and life completion discussions improve functioning and quality of life in seriously ill patients? Pilot randomized control trial. Journal of Palliative Medicine 11: 1234–40. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, Rene, Lucas J. Tiesinga, Berrie Middel, Doeke Post, and Henk Jochemsen. 2009. The validity and reliability of an instrument to assess nursing competencies in spiritual care. Journal of Clinical Nursing 18: 2857–69. [Google Scholar] [CrossRef] [PubMed]
- VandeCreek, Larry, Susan Ayres, and Meredith Bassham. 1995. Using INSPIRIT to conduct spiritual assessments. Journal of Pastoral Care 49: 83–89. [Google Scholar] [CrossRef] [PubMed]
- Vivat, Bella, Teresa E. Young, J. Winstanley, J.I. Arraras, K. Black, F. Boyle, A. Bredart, A. Costantini, J. Guo, M.E. Irarrazaval, and et al. 2017. The international phase 4 validation study of the EORTC QLQ-SWB32: A stand-alone measure of spiritual well-being for people receiving palliative care for cancer. European Journal of Cancer Care (England) 26. [Google Scholar] [CrossRef] [PubMed]
- WHOQOL SRPB Group. 2006. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Social Science & Medicine 62: 1486–97. [Google Scholar]
- Wu, Li-Fen, and Lih-Ying Lin. 2011. Exploration of clinical nurses’ perceptions of spirituality and spiritual care. The Journal of Nursing Research: JNR 19: 250–6. [Google Scholar] [CrossRef] [PubMed]
- Wu, Li-Fen, Shu-Hui Yang, and Malcolm Koo. 2017. Psychometric properties of the Chinese version of Spiritual Index of Well-Being in elderly Taiwanese. BMC Geriatrics 17: 3. [Google Scholar] [CrossRef] [PubMed]
- Xue, S., S. Arya, A. Embuldeniya, H. Narammalage, Tricia da Silva, Shehan Williams, and A. Ravindran. 2016. Perceived functional impairment and spirituality/religiosity as predictors of depression in a Sri Lankan spinal cord injury patient population. Spinal Cord 54: 1158–63. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, Zachary, Carol Jagger, Chi-Tsun Chiu, Mary Beth Ofstedal, Florencia Rojo, and Yasuhiko Saito. 2016. Spirituality, religiosity, aging and health in global perspective: A review. SSM—Population Health 2: 373–81. [Google Scholar] [CrossRef] [PubMed]
| PubMed | EMBASE | PsycINFO |
|---|---|---|
Keywords limits
| Keywords limits
| Keyword limits
|
| AND | ||
| Keywords Spirituality Spiritual well-being Spiritual distress Spiritual needs Religiosity Religious beliefs | Keywords Scale Measure Instrument Index Inventory Questionnaire | |
| Authors | Instrument Name | Sample Size | Type of Study | Findings |
|---|---|---|---|---|
| Daaleman et al. 2004 | The Spirituality Index of Well-Being (SIWB) | 523 outpatients from family practice | Factor analysis/test–retest reliability | Correlations with quality of life, health status and depression |
| Kaczorowski 1989 | The Spiritual Well-Being Scale | 114 cancer patients | Cross-sectional | Inverse correlations between low levels of spiritual well-being and high levels of anxiety |
| Peterman et al. 2014 | The Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being (FACIT-Sp) | 2923 cancer and HIV patients | Factor analysis and Observational | Strong internal consistency and moderate to strong correlations between FACIT-Sp and quality of life, especially meaning and peace |
| De Camargos et al. 2015 | WHOQOL-SRPB | 525 oncology patients / 525 health professionals | Cross-sectional | Daily use of spiritual and religious resources positively effects patient perceptions of QOL |
| Bussing, Koenig 2008 | BENEFIT Scale | 229 chronic pain patients | Reliability and validation | The BENEFIT scale correlates uniquely with spiritual and religious attitudes in clinical studies |
| Vivat et al. 2017 | EORTIC QLC-SWB32 | 451 palliative care patients from 14 countries | Validation | The EORTIC QLC-SWB32 measures distinct aspects of QOL |
| Bussing et al. 2016 | SpREUK | 275 cancer patients | Factor analysis and reliability | A valid measure of important aspects of spirituality and religious attitudes |
| Kreitzer et al. 2009 | Brief Serenity Scale | 87 post solid organ transplant patients | Factor analysis and reliability | The Brief Serenity Scale captures dimensions of spirituality, a state of acceptance, inner haven and trust that is distinct from other spirituality instruments |
| Delaney 2005 | The Spirituality Scale | 226 patients with chronic illness | Reliability and validation | The Spirituality Scale provides a 3-factor framework (self-discovery, relationships and eco-awareness) that help with nursing care |
| Ironson et al. 2002 | The Ironson–Woods Spirituality/Religiosity Index | 279 HIV positive patients and long-term AIDS survivors | Reliability and validation | Long-term survival related to frequency of positive prayer and non-judgmental attitudes |
| Johnstone et al. 2016 | The Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS) | 109 traumatic brain injury patients | Factor analysis | The BMMRS is a valid measure of emotional connectedness with higher power and social support among different spiritual and religious variables |
| Hatch et al. 1998 | The Spiritual Involvement and Beliefs Scale | 50 primary care patients and 23 family practice educators | Factor analysis | The SIBS shows that included terms avoid cultural and religious bias in both beliefs and actions |
| McBride et al. 1998b | The Brief Pictorial Instrument for Assessing Spirituality | 442 family practice patients | Reliability and validation | The pictorial instrument provides a quick assessment of intrinsic spirituality correlating with other spirituality measures |
| VandeCreek et al. 1995 | The Index of Core Spiritual Experience (INSPIRIT) | 371 medical and surgical outpatients | Reliability and validation | INSPIRIT assessment reflects intrinsic religiosity and spirituality |
| Kimura et al. 2012 | The Daily Spiritual Experience Scale DSES) | 179 surgical patients | Cultural adaptation and validation | The DSES shows evidence of reliability and validity in assessing spiritual experiences among hospitalized patients |
| Gherghina et al. 2014 | The Spiritual Distress Assessment Tool (SDAT) | 72 elderly erioperative patients | Validation | The SDAT appears to be a reliable and valid instrument to assess spiritual distress in elderly hospitalized patients |
| Chiang et al. 2017 | The Religious Belief Scale | 619 clinical nurses | Factor analysis | A reliable and valid scale for measuring religious beliefs of nurses |
| McSherry et al. 2002 | The Spirituality and Spiritual Care Rating Scale | 549 ward-based nurses | Factor analysis | Factors identified: spirituality, spiritual care, religiosity and personal care |
| Kouloulias et al. 2017 | The QRFPC-25 | 156 cancer patients undergoing radiotherapy | Reliability and validation | A reliable and valid gauge for assessment of religiosity in cancer patients |
| Bussing et al. 2018 | Spiritual Needs Questionnaire | 627 chronic disease patients 940 elderly ill patients 1468 healthy adults | Factor analysis and reliability | This large study provides evidence for a cultural and religious sensitive measure that evaluates peoples spiritual needs |
| Ku et al. 2010 | The Spiritual Distress Scale (SDS) | 85 cancer patients | Factor analysis | The SDS is both reliable and valid in assessing patients in oncological settings and aids nurses in the assessment of spiritual distress |
| Bennet Astrow et al. 2015 | The Spiritual Needs Assessment for Patients (SNAP) | 727 haematology and cancer patients | Observational and validation | SNAP is reliable and valid in measuring spiritual needs in patients from different cultural and religious backgrounds |
| Buck et al. 2012 | The Spiritual Needs Inventory (SNI) | 410 cancer patient caregivers | Reliability and Validity | Use of the SNI in hospice caregivers can aid nurses in the identification of patients’ spiritual needs |
| Monod et al. 2010 | The Spiritual Needs Assessment Tool (SDAT) | 203 Geriatric rehabilitation patients | Reliability and Validity | The SDAT shows adequate reliability and validity in assessing levels of spiritual distress |
| Fischbeck et al. 2013 | The Advanced Cancer Patients’ Distress Scale | 168 advanced cancer patients | Factor analysis | Initially shown to be reliable in identifying patients spiritual needs |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Austin, P.; Macdonald, J.; MacLeod, R. Measuring Spirituality and Religiosity in Clinical Settings: A Scoping Review of Available Instruments. Religions 2018, 9, 70. https://doi.org/10.3390/rel9030070
Austin P, Macdonald J, MacLeod R. Measuring Spirituality and Religiosity in Clinical Settings: A Scoping Review of Available Instruments. Religions. 2018; 9(3):70. https://doi.org/10.3390/rel9030070
Chicago/Turabian StyleAustin, Philip, Jessica Macdonald, and Roderick MacLeod. 2018. "Measuring Spirituality and Religiosity in Clinical Settings: A Scoping Review of Available Instruments" Religions 9, no. 3: 70. https://doi.org/10.3390/rel9030070