Definition of Motion and Biophysical Indicators for Home-Based Rehabilitation through Serious Games
Abstract
:1. Introduction
2. Description of the System
2.1. Overall Architecture
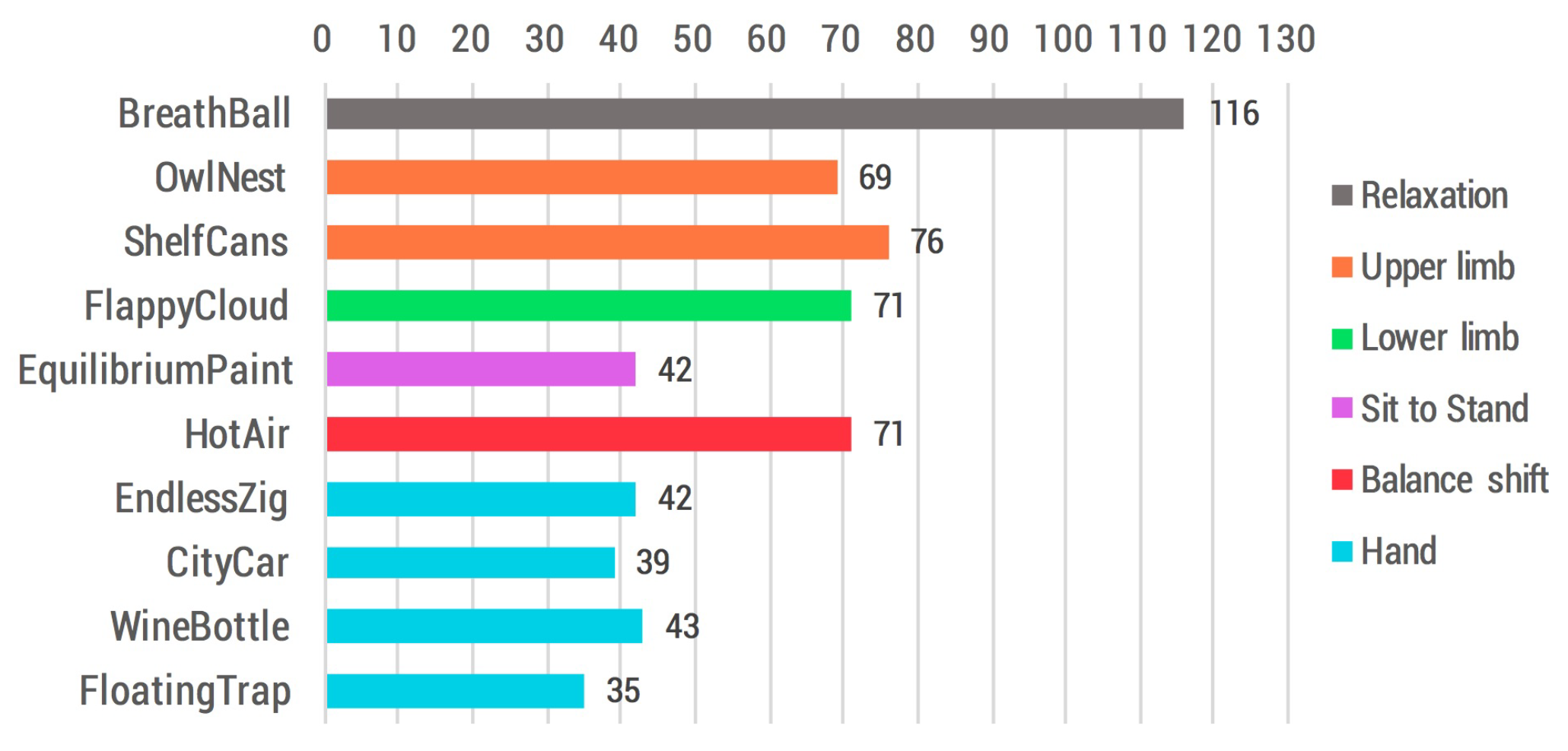
- Serious games are digital games that were completely developed in our labs exclusively for the ReMoVES platform. The system currently includes 10 main serious games and 60 variations: they encourage the patient to carry out functional exercises autonomously along with the traditional motion rehabilitation. A representative screenshot for each serious game is given in Figure 1 (from a to i) and in Figure 2. The creation of these activities involved different processes, technologies, and specialists. In the case of serious games, special attention must be paid to the specifications given by physiotherapists and physiatrists, who shared their expertise to define game parameters such as the level of difficulty. The interface was designed using the Unity3D platform, which is a popular engine often used for developing games and virtual reality applications. The games are scripted in C#. All art assets in both 2D and 3D formats were downloaded from different online sources under Creative Commons license [11]. The whole set of games shares a core library that were developed to allow easy and straightforward communication with the Application Programming Interfaces (APIs) exposed by the cloud back-end that will be presented later.
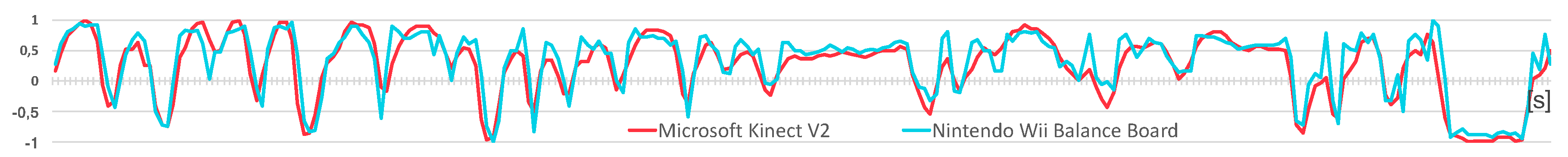
- Microsoft Kinect V2 is a motion sensing input device based on a high-resolution colour camera and an infrared emitter for depth analysis that can simultaneously 3D-track up to 25 fundamental joints of the framed human body. It offers a wide field of view (70 × 60 degrees) and recognition up to 4.5 m from the device [12]. Several studies have demonstrated that spatiotemporal parameters can be validly obtained by Microsoft Kinect V2 [13,14]. The set-up of the interface between the Microsoft Kinect V2 and the Unity3D engine is effortless because the manufacturer provides a Software Development Kit (SDK) and a Unity add-on, which gives developers access to body joint positions and orientations that can be used directly in rehabilitation game development.
- Leap Motion is explicitly targeted at hand gesture recognition and computes the position of the fingertips and the hand orientation. Its interaction zone is limited to a semi-sphere of radius 0.60 m around the device, with a theoretical accuracy of 0.01 mm according to the manufacturer (or 0.7 mm under real conditions as measured by [15]). Examples of clinical studies that have used the Leap Motion controller are [16,17]. The manufacturer provides a Unity Assets bundle to allow a straightforward interface with the development engine.
- Microsoft Band 2 is a physiological sensor used to collect the two signals chosen as a measure of involvement during the rehabilitation program: heart rate (HR) and electrodermal activity (EDA). It also includes a wide range of additional built-in sensors: accelerometer, gyroscope, barometer, GPS, skin temperature sensor, ambient light, and ultraviolet sensor. Microsoft Band 2 offers the opportunity to collect real-time data in a continuous manner for at least 4 h without recharging [18]. Our interface with Microsoft Band 2 is implemented using the Band SDK for the Universal Windows Platform in C#.
- Cloud back-end was developed using state-of-the-art techniques to provide scalable, secure, and efficient data processing and storage. In Figure 1 it is schematically represented as the Data Processing cloud. The architecture of this component is not the subject of this paper, but it plays a fundamental role since it exposes REpresentational State Transfer (REST) APIs for all-around management (authentication, initialization, data storage) of the activity sessions which can take place remotely and simultaneously in different locations (rehabilitation centres, hospitals, or patients’ homes). In detail, the ReMoVES cloud back-end was developed with PHP 5 and is hosted on an Apache/2.4.6 web server running CentOS 7. The JavaScript Object Notation (JSON) standard has been adopted for encrypted (over SSL) message communication between the cloud back-end and other components. Data is stored in a MySQL relational database running on the same machine: it is made up of tables for users management, rehabilitation sessions scheduling and game log storage. The motion and biophysical values originating from the serious games and the peripherals are stored in the database at 2 Hz in an integer or float numeric data type (four bytes, single-precision) along with a timestamp to identify when that event occurred (it is generated on the machine running the serious games, not on the cloud back-end since this would be affected by unpredictable delay). The raw measures from the sensors are provided with different data types and are stored without rounding as reported in Table 1.
2.2. Serious Games
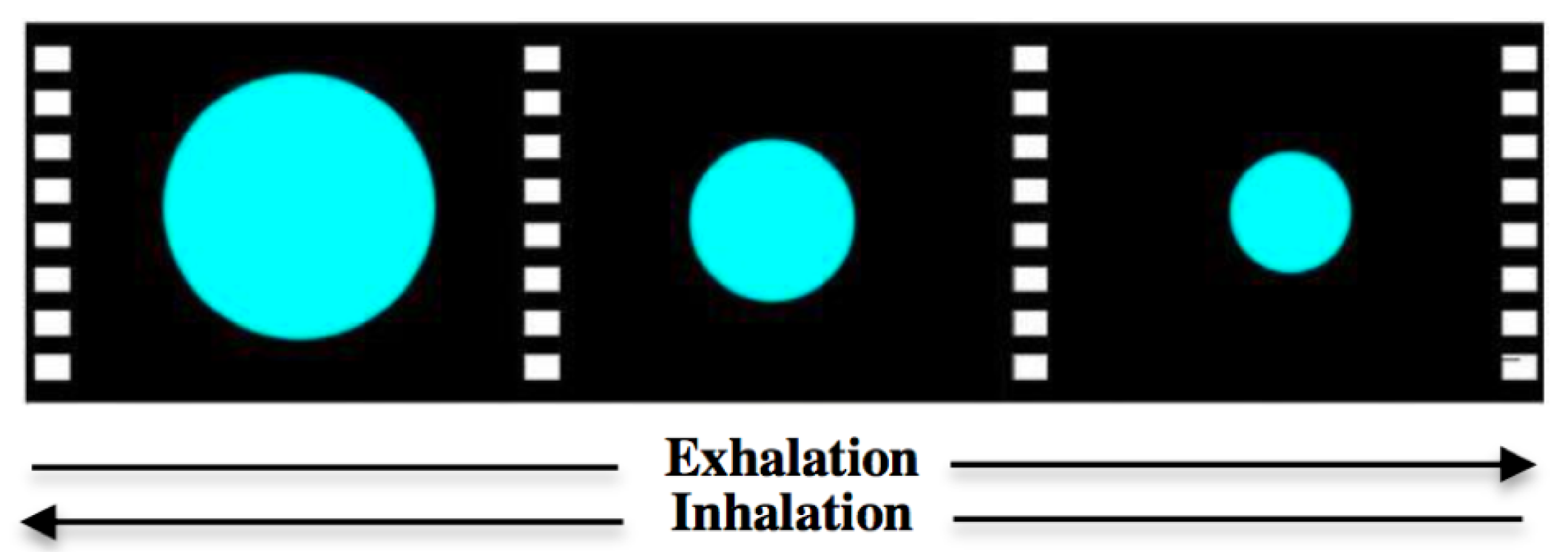
- BreathBall This activity (see Figure 2) helps the patient to relax and focus on their breathing. It is not an interactive game. The patient is led to breathe with a regular rhythm by following a “breath ball” displayed on the monitor. The BreathBall exercise makes the subject comfortable and brings back their heartbeat to a basal value before the actual rehabilitation session starts.
- ShelfCans This serious game (Figure 1a) introduces the patient to a virtual environment similar to a kitchen. With the arm movement, the patient grabs one of the colourful drink cans appearing in the middle of the screen and drags it to the corresponding shelf. This game is appealing because it requires the user to be attentive to drop off the drink can in the correct shelf according to its colour.
- OwlNest The patient is encouraged to reach an on-screen target (Figure 1b) with the arm motion (Reaching Task) in order to achieve a high in-game score. Many colourful owls appear randomly in any position of the screen for a given time-frame: the user should carry them in the nest before they disappear.
- FlappyCloud This is a functional exercise for the lower limb. The leg Abduction–Adduction movement reflects the position of a cloud object in the game screen: the patient should make it move forward without hitting some obstacles (Figure 1c).
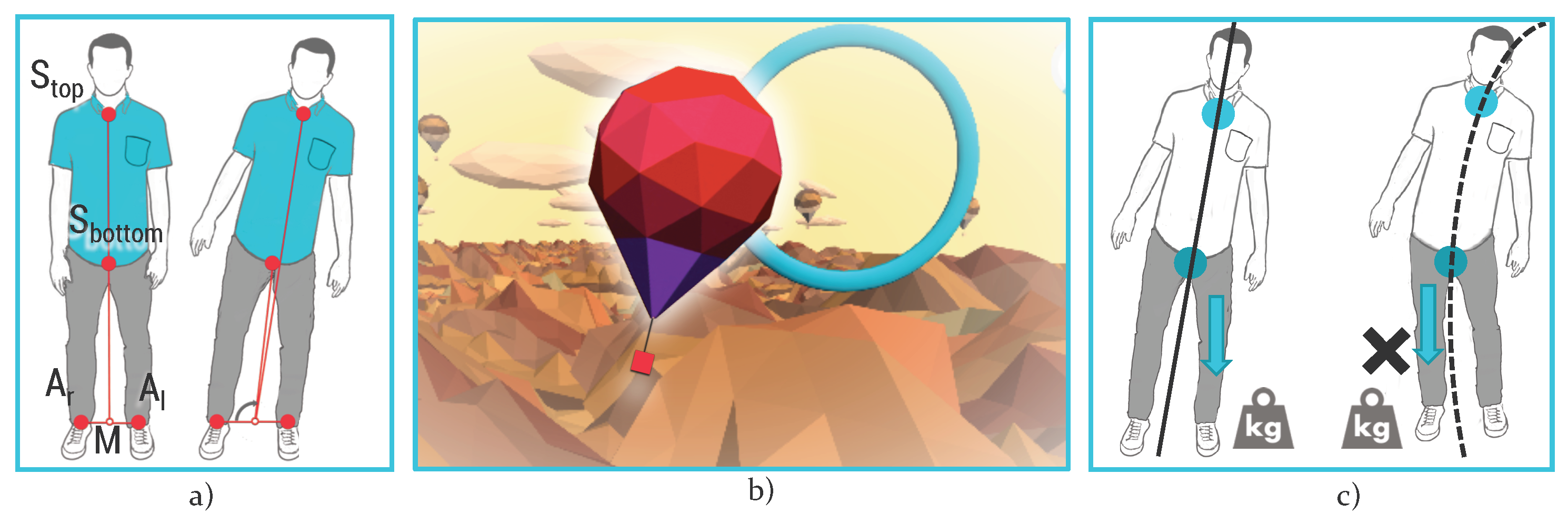
- HotAir This is an activity to improve control of the patient’s body balance. The user can control the direction of a hot-air balloon, floating in the sky with the balance shift: in-game scores are collected when it is led towards the bonus targets (Figure 1d).
- EquilibriumPaint This serious game is an interactive version of the Sit to Stand (STS) exercise, typically used in traditional rehabilitation to evaluate patient performance. The user should stand up and sit down repeatedly within a predefined amount of time (usually 30 or 60 s [19]); their trunk must remain erect: an erroneous lateral shift causes the fall of the cans of paint leaning on an unstable wooden beam (Figure 1e).
- WineBottle This exercise mimics a real-world scenario: pouring liquids from a bottle. With the Pronation–Supination movement of the hand, the patient should control the rotation of a bottle of wine appearing on the screen. They must fill a glass over and over again to collect as many points as possible (Figure 1f).
- EndlessZig In this activity, the patient drives a marble along a zigzag path appearing on the screen. Going out of the boundaries causes score loss; similarly, some bonus gems appear on the path. The patient controls the marble movement with Radial–Ulnar deviation (Figure 1g).
- CityCar In this game, the patient drives a car along a randomly-generated road. The user should steer in the presence of curves and crossroads with the movement of Flexion/Extension of the wrist. Penalties are introduced when the user goes off-track (Figure 1h).
- FloatingTrap In this serious game, the patient is led to open their hand and make a fist alternatively. This exercise requires a good level of concentration: in fact, the user moves a floating raft on the left or on right according to the finger Flexion/Extension in order to avoid some objects in the scene (Figure 1i).
3. Features Description
3.1. Relaxation
3.2. Upper Limb
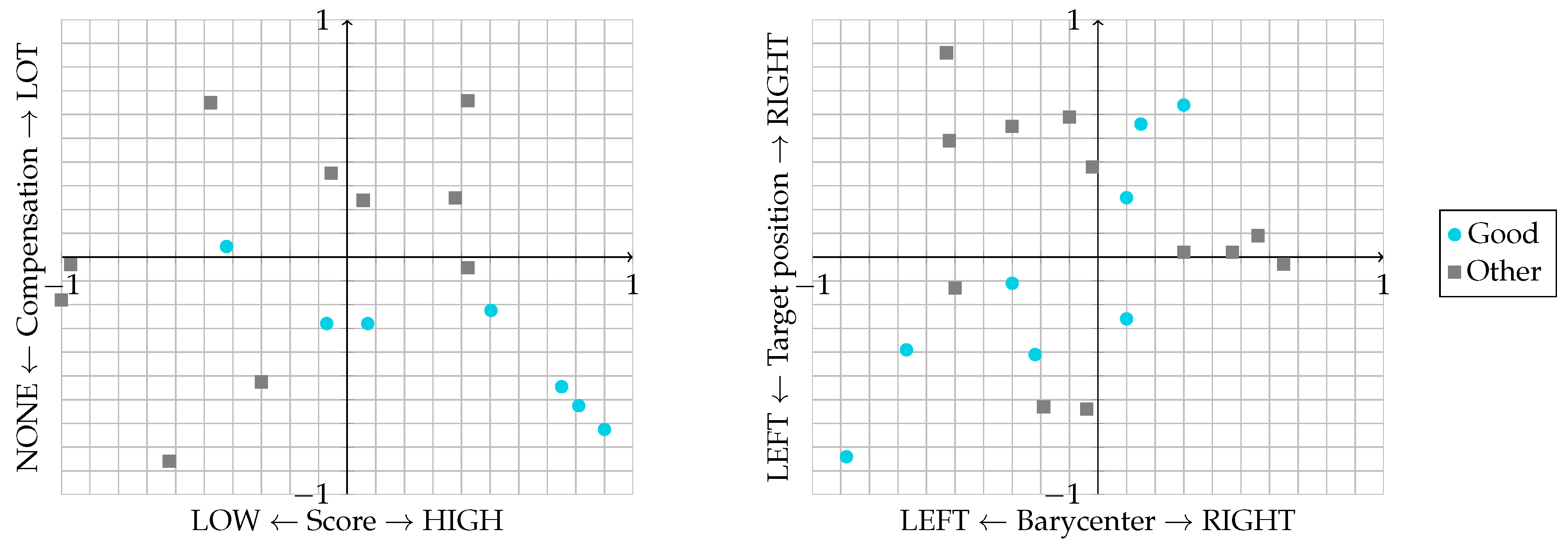
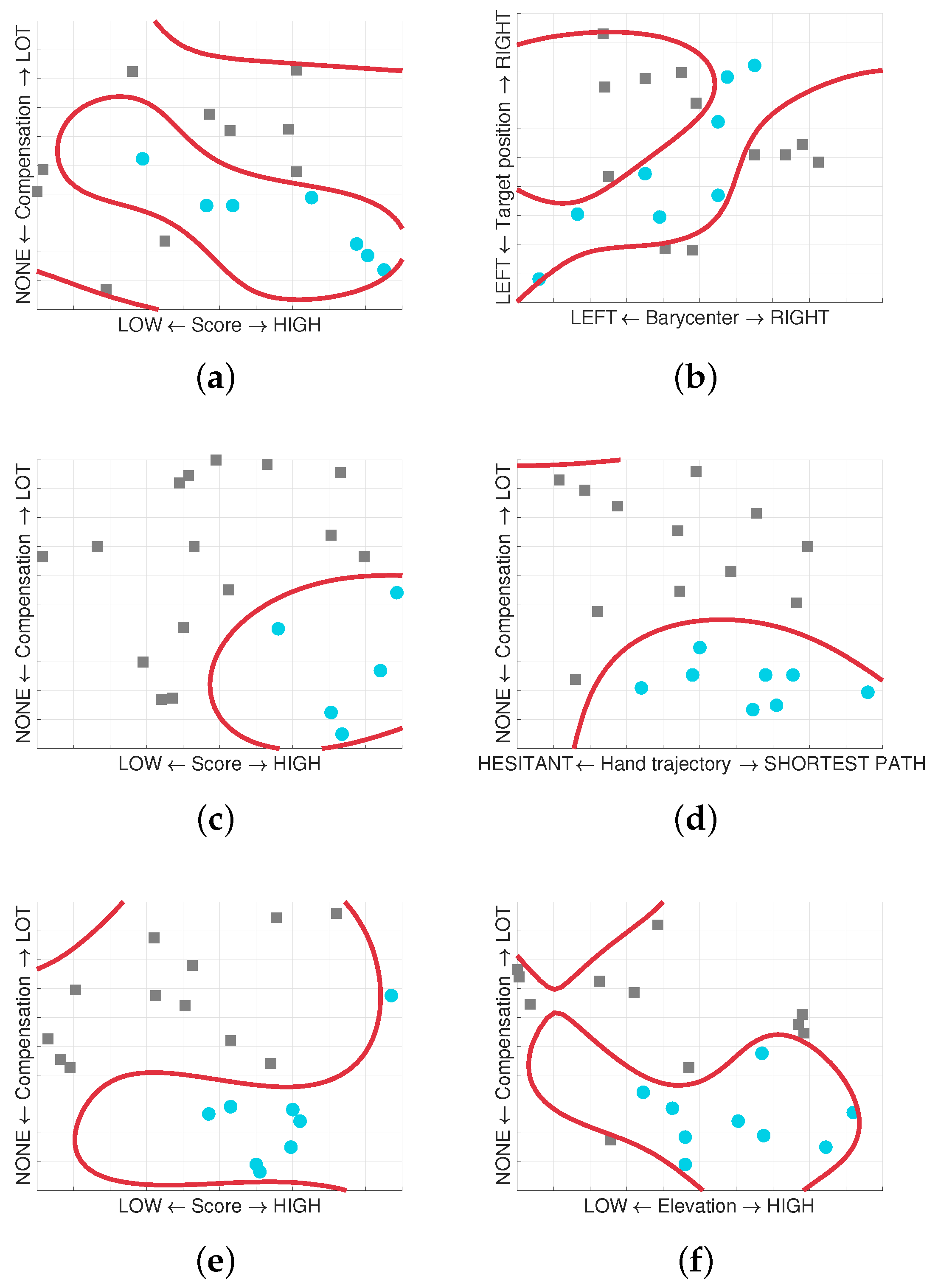
- Score: the score collected in-game is an abstract quantity associated to the player performance for their achievements. It acts as a quantitative indicator of success in the game introduced to motivate patients to attain a better score than their opponents/themselves.The Score feature is the ratio between the score collected by the user and the theoretical maximum achievable in the game:
- Hand trajectory: analysis of the hand trajectory is an indicator of the precision and the movement control level that the patient can keep during the activity. We calculate the distance between the trajectory (N samples over time , where x and y are the horizontal/vertical coordinates of the coronal plane) and the shortest line passing through the two points of (target spawn position) and (Figure 3b):
- Compensation: compensation is an undesired movement strategy adopted by the patient during the execution of the exercise. In detail, the distance d between the hand and the shoulder (Figure 3a) while performing the movement is evaluated in order to assess whether the patient reaches the targets by performing a correct Flexion–Extension or Abduction–Adduction movement or moves the whole body instead, implying that the hand-shoulder distance remains constant.Let us define the average of distances with respect to the N observations during a single session; the Compensation parameter, index of the wrong movement, is then extracted as follows:
- Barycenter: this indicator deals with the detection and measurement of a spatial negligence in hemiparetic patients who ignore the targets that are offered to their attention in a certain part of the in-game space. Spatial negligence affects approximately 30–40% of patients with acute stroke and consists of ignoring part of the space as a result of brain damage. The hand coordinates on the coronal plane, acquired over time, are used to populate a visual heatmap from which the therapist can evaluate the neglected areas; the spatial map is presented with a colour scale ranging from dark blue, where no movements were performed, to red, where there was the greatest occurrence (Figure 3c). This indicator is provided by the horizontal offset of the barycenter of the hand position observations over the session duration. In the evaluation of this indicator, it is also important to consider that in some variations of the OwlNest the targets are not equally distributed on both sides (e.g., to force a patient affected by left hemiparesis to focus his attention on the left side of the screen only).
3.3. Lower Limb
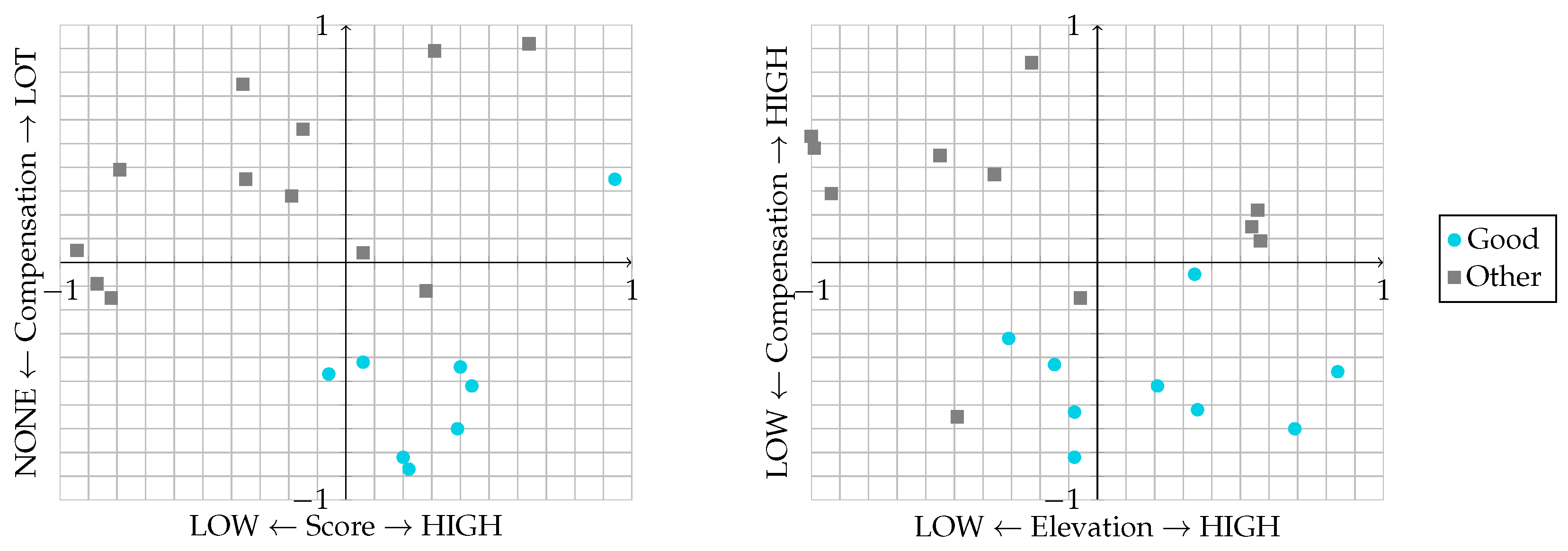
- Score: same as previous activities.
- Elevation: it is the maximum elevation of the impaired leg calculated as the angle between legs during the Abduction–Adduction movement. The Elevation feature is the ratio between the maximum angle reached by the user and the maximum reached on average by healthy subjects:
- Compensation: to accomplish the exercise correctly, the patient must keep the trunk erected and straight. In this case, the angle between the patient’s trunk and the ideal vertical attitude is considered.
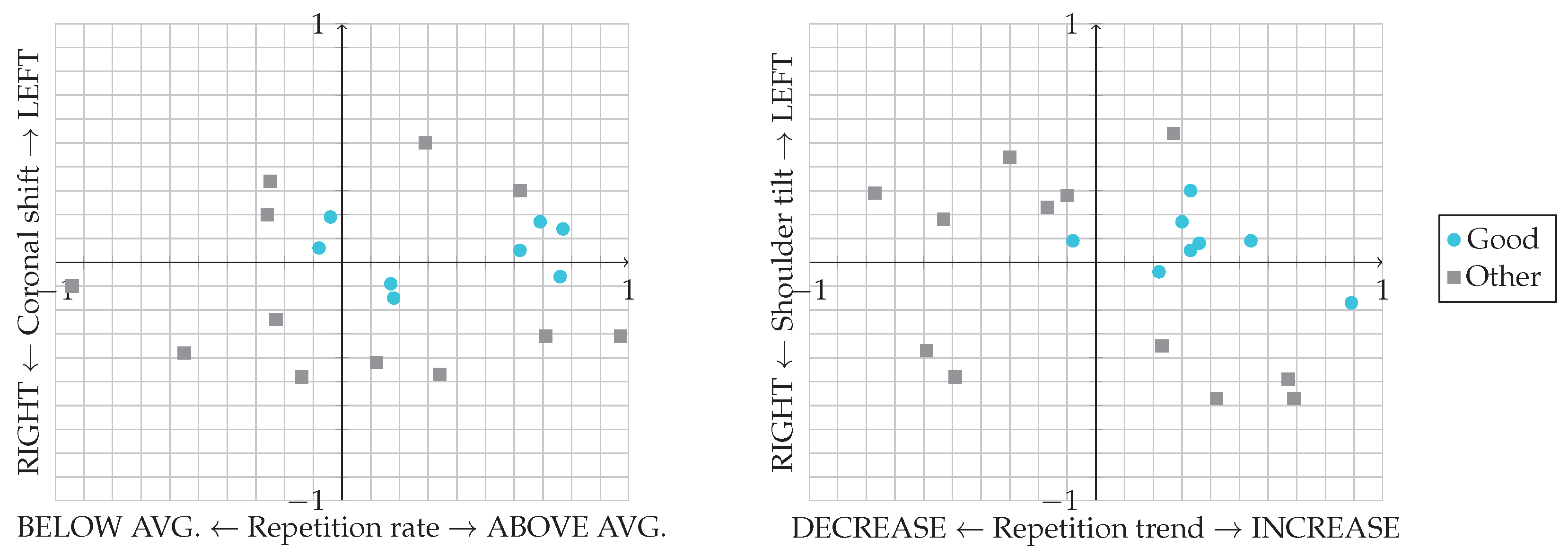
3.4. Sit to Stand
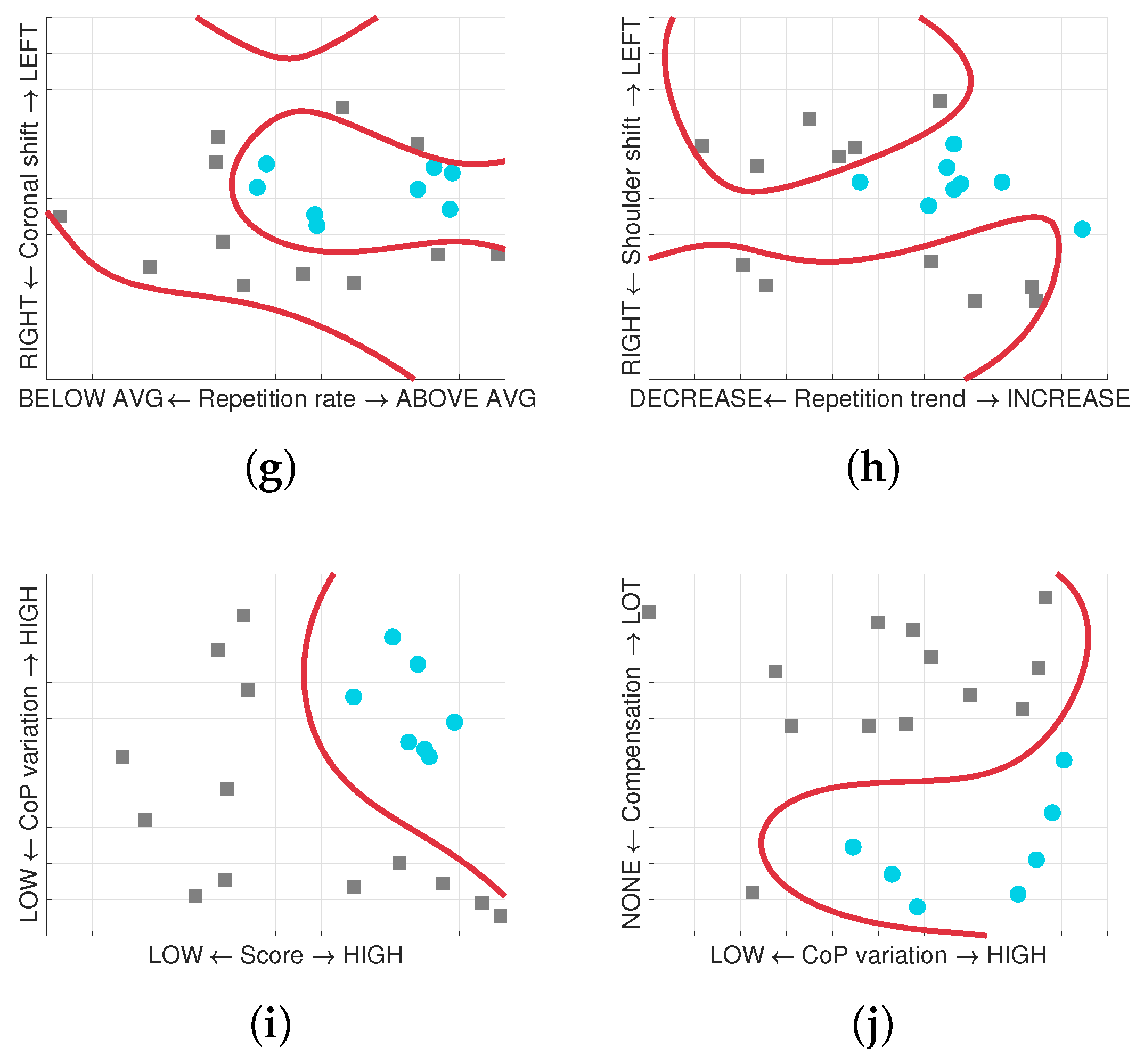
- Repetition rate: number of repetitions in a given time; it is proportional to the in-game score. The Repetition rate is the ratio between the rate maintained by the user and the average kept by healthy subjects:
- Repetition trend: the trend of the time required by the user to accomplish a single STS cycle. The analysis of the variability during a single session is, for example, important to detect the fatigue level of the patient. Given i the repetition number and the cycle duration, the Repetition trend is the slope (m) of the linear regression of with respect to i:
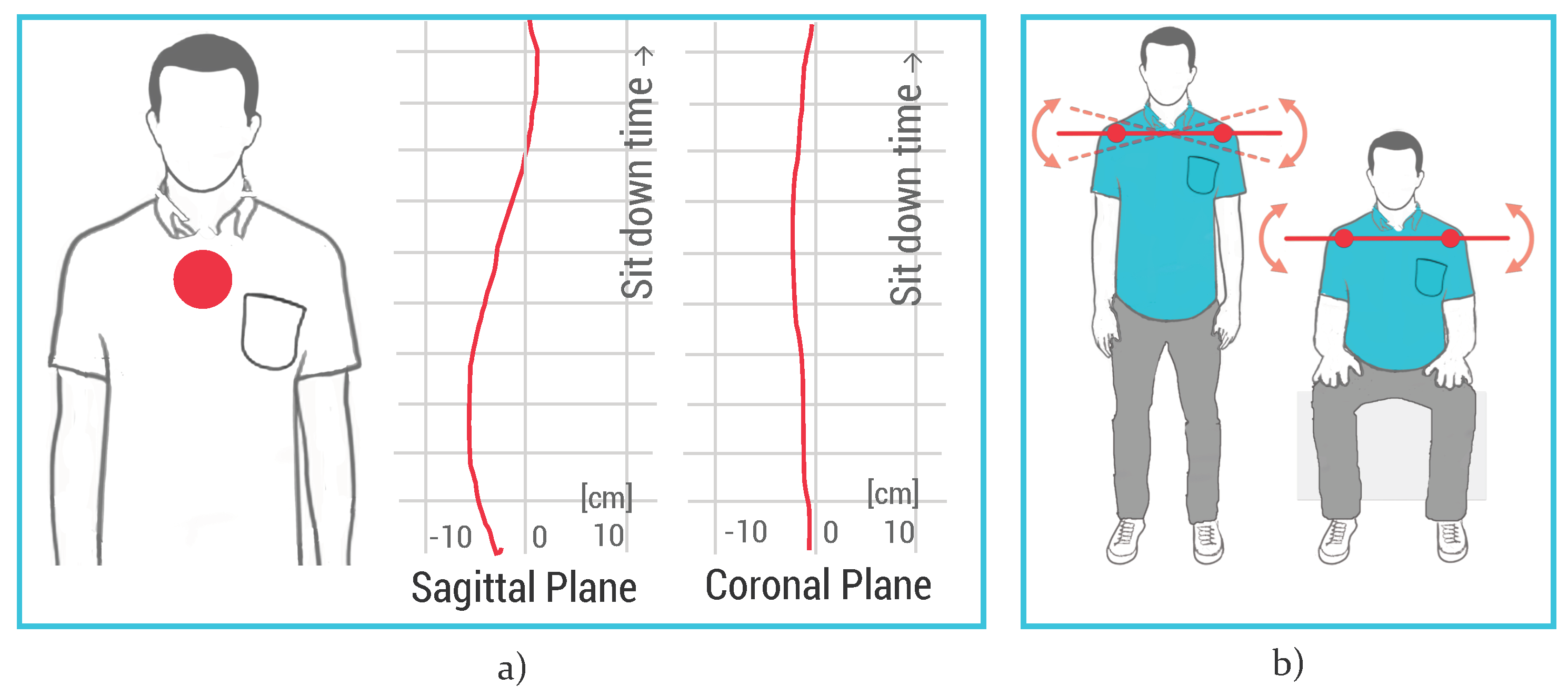
- Coronal shift: verification of the correct strategy used by the patient to stand up, considering the trunk tilt on coronal plane (Figure 7a). Even though the movement trajectory projected in the sagittal plane must show some forward/backward displacement, the correct coronal trajectory must be linear and constant around the zero value.
- Shoulder tilt: to accomplish the exercise correctly, the patient must stand up and sit down without twisting or tilting the shoulders. A correct movement provides very small angles of inclination with a tolerance of about 10 degrees, and therefore the average value must be around 0 degrees (Figure 7b).
3.5. Balance Shift
- Track the position in space of these fundamental body joints provided by Kinect SDK: right ankle (), left ankle (), the base of the spine (), and the spine at the shoulder height () (Figure 9a).
- Compute the position in space of the middle point (M) between the right ankle and the left ankle.
- Compute the difference between the angles related to the shift of lower and higher sections of the trunk:
- Calculate the average between the and to get the estimated CoP:
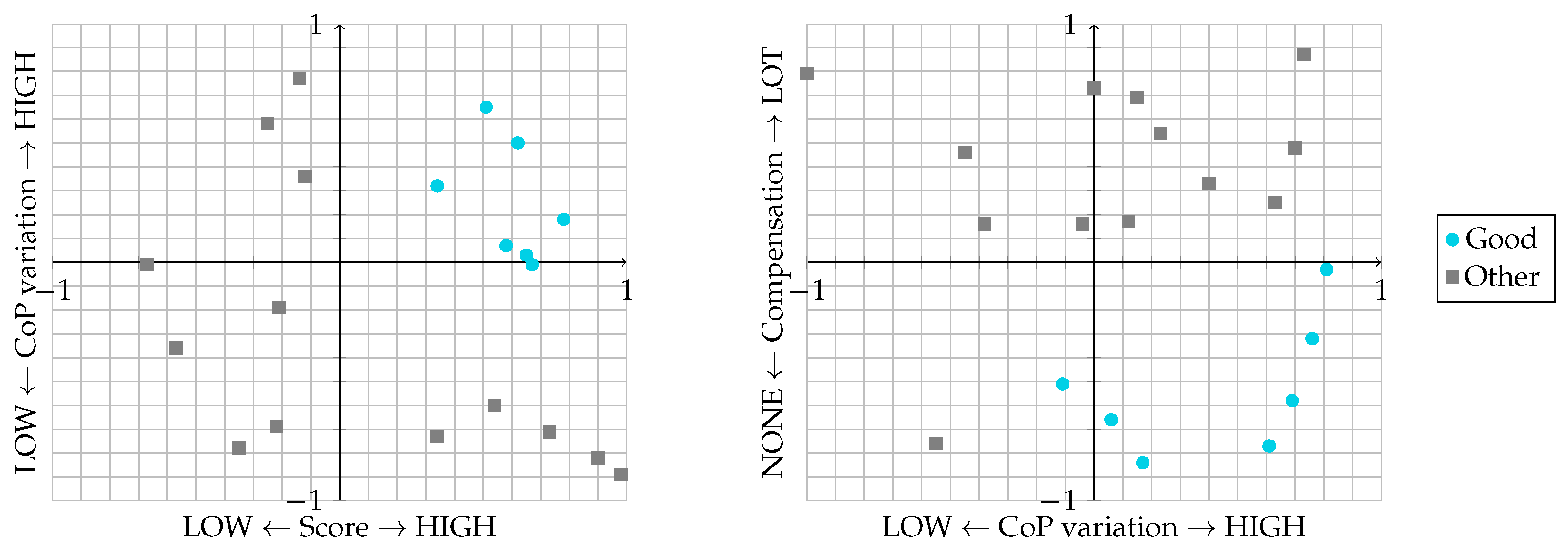
- Score: same as for upper limb games.
- Centre of pressure variation: during the Balance shift functional exercise, the patient must load weight on the two legs alternately, and thus the variation of CoP on the mediolateral axis is calculated.
- Compensation: to accomplish the exercise correctly, the patient must alternate the load on the lower left and right limbs without compensating the movement by shifting the upper part of the body. This erroneous strategy can be detected by computing the difference between and (Figure 9c):
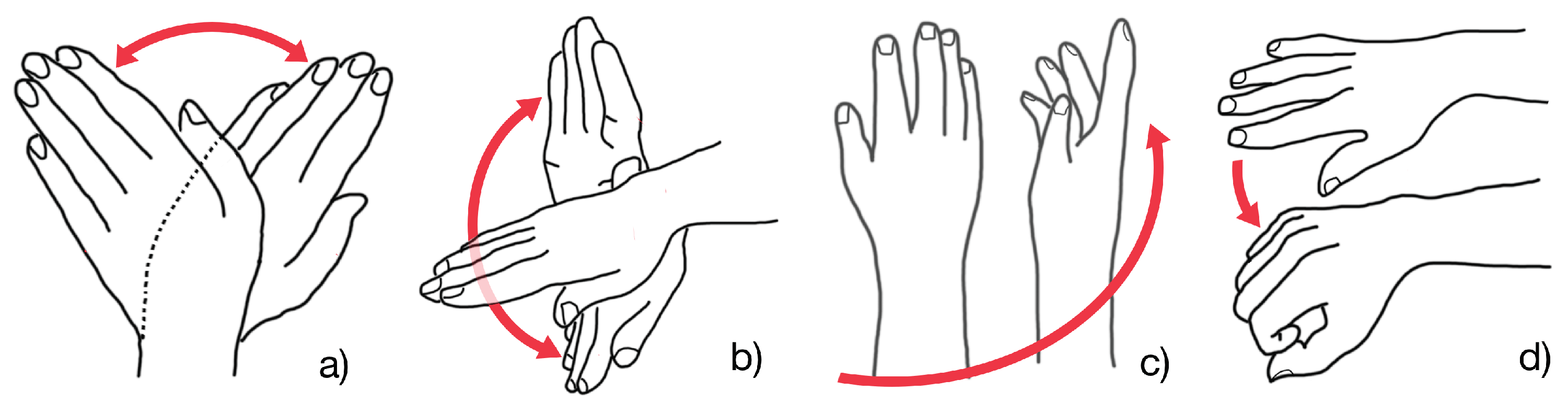
3.6. Hand Movements
- Repetition rate: same as previous activities.
- Maximum angle: maximum angle reached in each of the proposed movement (corresponding to yaw, pitch, and roll). These values are tracked, respectively, in EndlessZig, CityCar, and WineBottle games.
- Grab strength: evaluation of the grasping exercise with Grab strength function provided by Leap Motion SDK that returns values between 0 and 1 respectively when the hand is open or when it is closed in a grabbing pose. This feature is currently tracked in the FloatingTrap serious game.
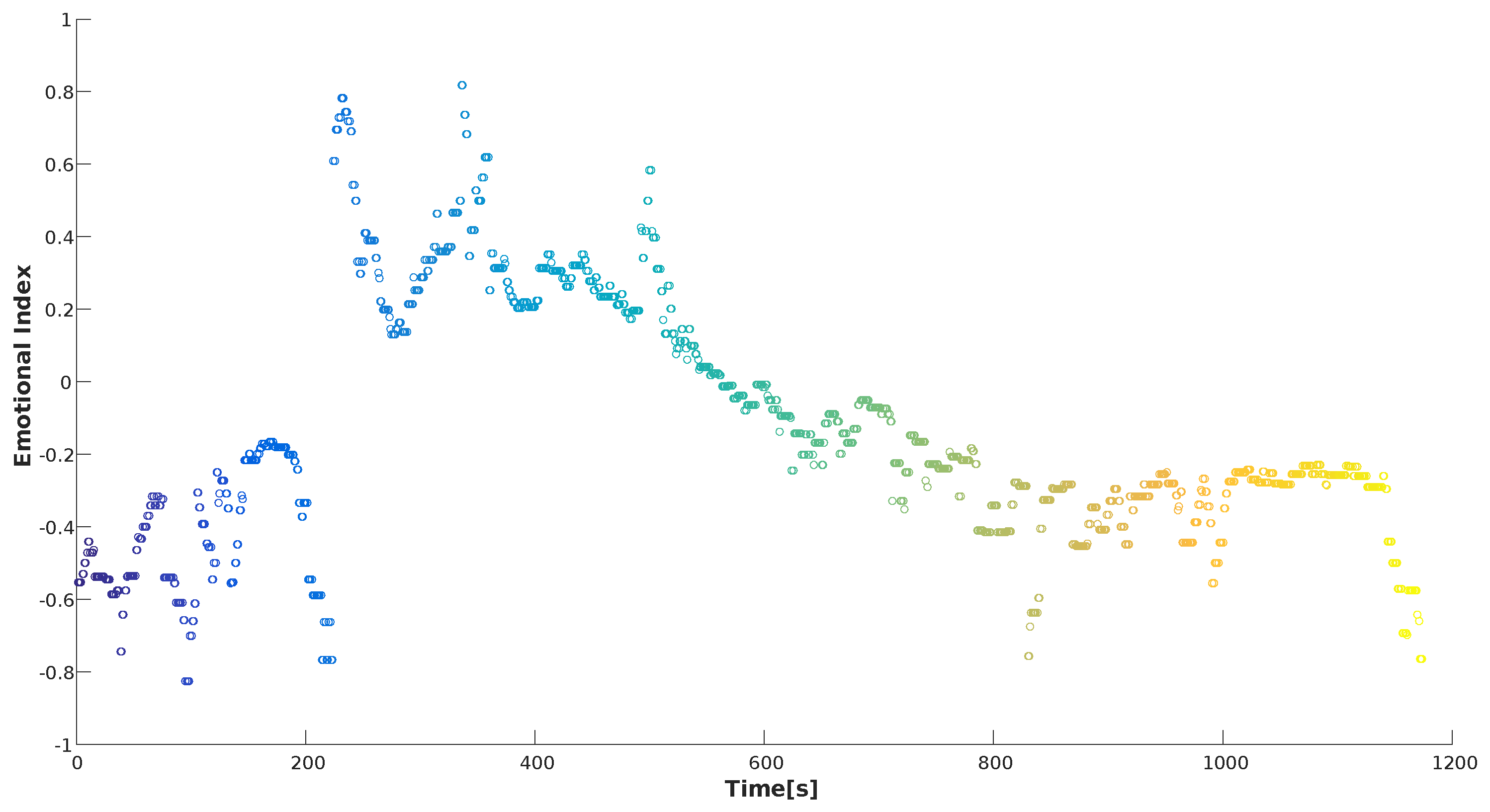
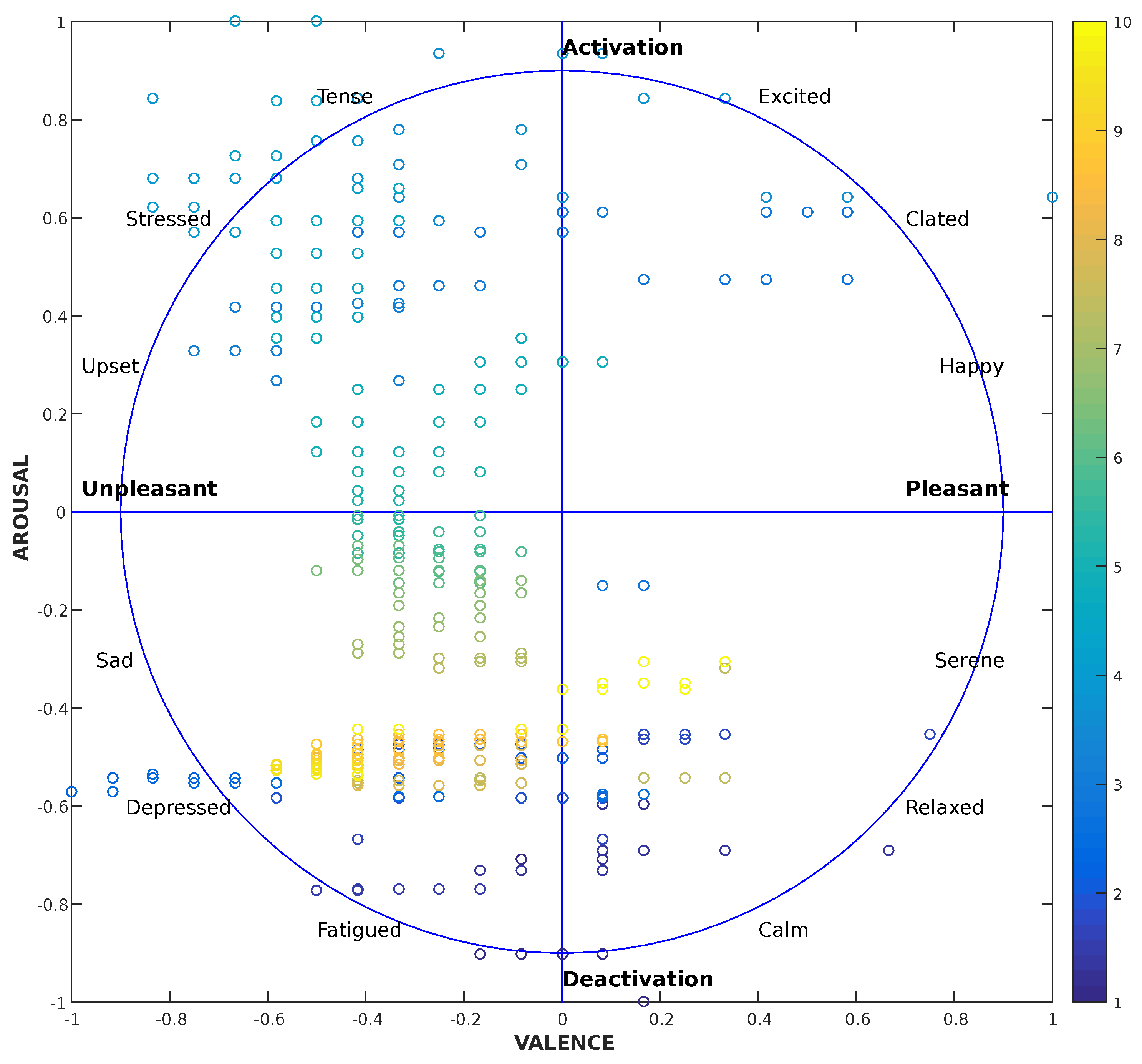
3.7. Heart Rate and Electrodermal Activity
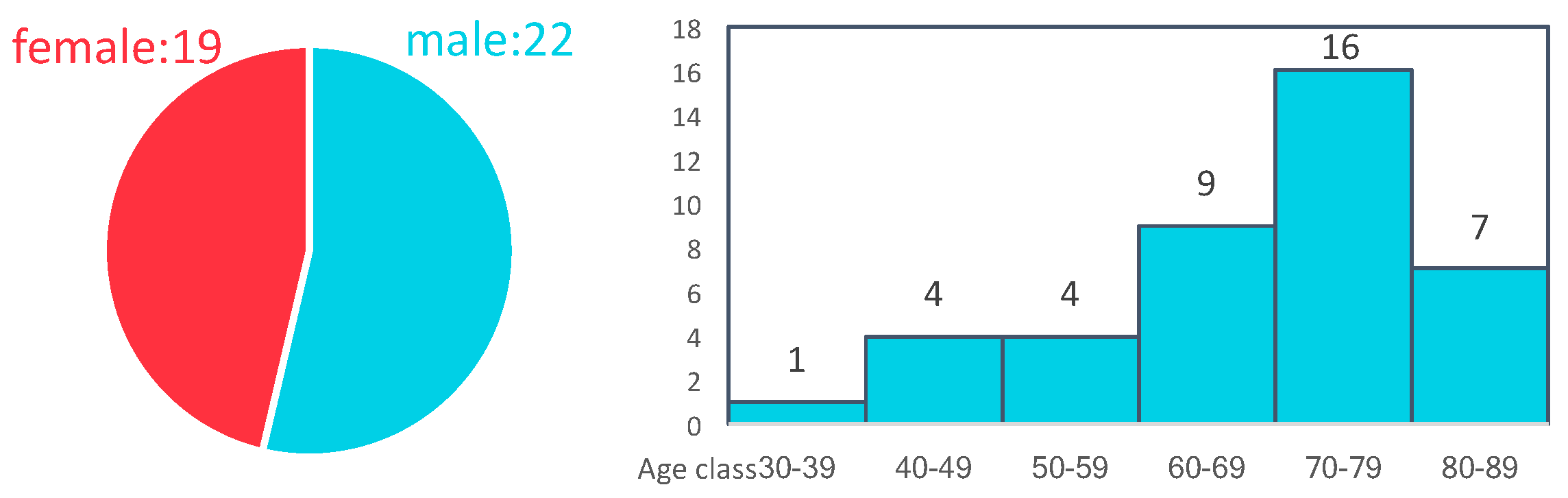
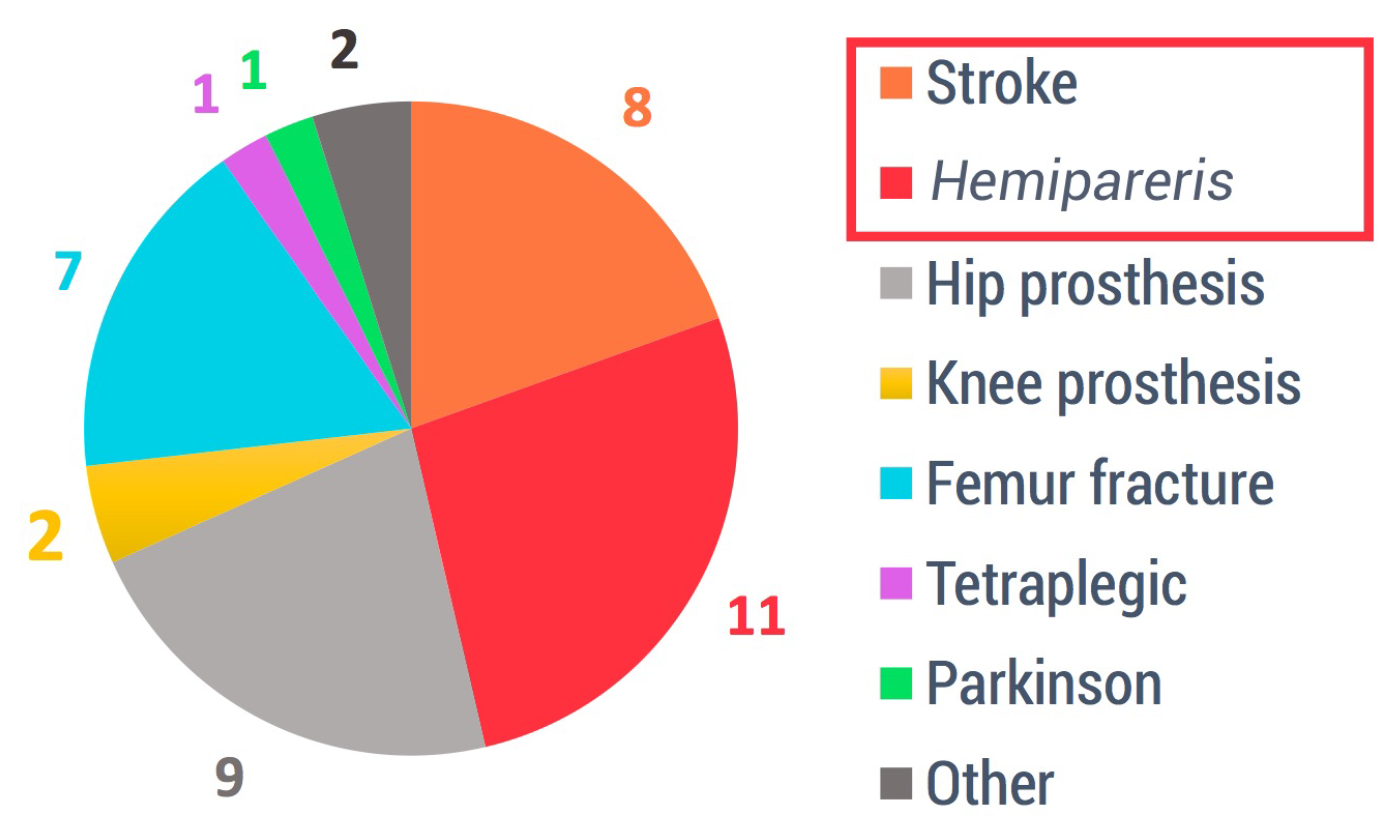
4. Results
- Determine the training examples. We have decided which features are going to be used as training set for each of our serious games.
- Gather a training set. Thus, a set of input objects is gathered and corresponding outputs are also gathered according to care providers. In detail, “labelled” information consist of flagged data by the therapist as “Good” when the patient performance is valid, and “Other” when the patient carried out the exercise erroneously/inadequately.
5. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maule, J.; Chestnutt, L. Telemedicine in the 21st Century, Opportunities for Citizens, Society and Industry. In Proceedings of the an International Space University Workshop, Strasbourg, France, 4–5 November 1999. [Google Scholar]
- Ferrara, E.; Nardotto, S.; Ponte, S.; Dellepiane, S.G. Infrastructure for data management and user centered rehabilitation in Rehab@Home project. In Proceedings of the 7th International Conference on PErvasive Technologies Related to Assistive Environments, Island of Rhodes, Greece, 27–30 May 2014; p. 21. [Google Scholar]
- Deutsch, J.E.; Brettler, A.; Smith, C.; Welsh, J.; John, R.; Guarrera-Bowlby, P.; Kafri, M. Nintendo Wii Sports and Wii Fit Game Analysis, Validation, and Application to Stroke Rehabilitation. Top. Stroke Rehabil. 2011, 18, 701–719. [Google Scholar] [CrossRef] [PubMed]
- Mouawad, M.R.; Doust, C.G.; Max, M.D.; McNulty, P.A. Wii-based movement therapy to promote improved upper extremity function post-stroke: A pilot study. J. Rehabil. Med. 2011, 43, 527–533. [Google Scholar] [PubMed]
- Ponte, S.; Gabrielli, S.; Jonsdottir, J.; Morando, M.; Dellepiane, S. Monitoring game-based motor rehabilitation of patients at home for better plans of care and quality of life. In Proceedings of the 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 3941–3944. [Google Scholar]
- Vamsikrishna, K.; Dogra, D.P.; Desarkar, M.S. Computer-vision-assisted palm rehabilitation with supervised learning. IEEE Trans. Biomed. Eng. 2016, 63, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Cary, F.; Postolache, O.; Girao, P.S. Kinect based system and artificial neural networks classifiers for physiotherapy assessment. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lisboa, Portugal, 11–12 June 2014; pp. 1–6. [Google Scholar]
- Bragaglia, S.; Di Monte, S.; Mello, P. A distributed system using MS kinect and event calculus for adaptive physiotherapist rehabilitation. In Proceedings of the Eighth International Conference on Complex, Intelligent and Software Intensive Systems (CISIS), Birmingham, UK, 2–4 July 2014; pp. 531–538. [Google Scholar]
- Wattanasoontorn, V.; Boada, I.; García, R.; Sbert, M. Serious games for health. Entertain. Comput. 2013, 4, 231–247. [Google Scholar] [CrossRef]
- Morando, M.; Ponte, S.; Ferrara, E.; Dellepiane, S. Biophysical and Motion Features Extraction for an Effective Home-Based Rehabilitation. In Proceedings of the International Conference on Bioinformatics Research and Applications ICBRA 2017, Barcelona, Spain, 8–10 December 2017; pp. 79–85. [Google Scholar]
- Pixabay Home Page. Available online: https://pixabay.com (accessed on 20 April 2018).
- Lachat, E.; Macher, H.; Landes, T.; Grussenmeyer, P. Assessment and calibration of a RGB-D camera (kinect v2 sensor) towards a potential use for close-range 3D modeling. Remote Sens. 2015, 7, 13070–13097. [Google Scholar] [CrossRef]
- Geerse, D.J.; Coolen, B.H.; Roerdink, M. Kinematic validation of a multi-Kinect v2 instrumented 10-m walkway for quantitative gait assessments. PloS ONE 2015, 10, e0139913. [Google Scholar] [CrossRef] [PubMed]
- Pöhlmann, S.T.; Harkness, E.F.; Taylor, C.J.; Astley, S.M. Evaluation of Kinect 3d sensor for healthcare imaging. J. Med. Biol. Eng. 2016, 36, 857–870. [Google Scholar] [CrossRef] [PubMed]
- Weichert, F.; Bachmann, D.; Rudak, B.; Fisseler, D. Analysis of the accuracy and robustness of the leap motion controller. Sensors 2013, 13, 6380–6393. [Google Scholar] [CrossRef] [PubMed]
- Khademi, M.; Mousavi Hondori, H.; McKenzie, A.; Dodakian, L.; Lopes, C.V.; Cramer, S.C. Free-hand interaction with leap motion controller for stroke rehabilitation. In Proceedings of the CHI’14 Extended Abstracts on Human Factors in Computing Systems, Toronto, ON, Canada, 26 April–1 May 2014; pp. 1663–1668. [Google Scholar]
- Bassily, D.; Georgoulas, C.; Guettler, J.; Linner, T.; Bock, T. Intuitive and adaptive robotic arm manipulation using the leap motion controller. In Proceedings of the ISR/robotik 2014, 41st International Symposium on Robotics, Munich, Germany, 2–3 June 2014; pp. 1–7. [Google Scholar]
- Al-Naffakh, N.; Clarke, N.; Dowland, P.; Li, F. Activity Recognition using wearable computing. In Proceedings of the 2016 11th International Conference on Internet Technology and Secured Transactions (ICITST), Barcelona, Spain, 5–7 December 2016; pp. 189–195. [Google Scholar]
- Britton, E.; Harris, N.; Turton, A. An exploratory randomized controlled trial of assisted practice for improving sit-to-stand in stroke patients in the hospital setting. Clin. Rehabil. 2008, 22, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Bryant, A.L.; Pua, Y.; McCrory, P.; Bennell, K.; Hunt, M. Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait Posture 2010, 31, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, H.L.; Ting, L.H.; Bingham, J.T. Accuracy of force and center of pressure measures of the Wii Balance Board. Gait Posture 2014, 39, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Ponte, S.; Ferrara, E.; Dellepiane, S. Home-based system for rehabilitation: improving quality of life through engineering solutions. In Proceedings of the Engineering 4 Society, Raising Awareness for the Societal and Environmental Role of Engineering and (Re)training Engineers for Participatory Design, Leuven, Belgium, 18–19 June 2015; pp. 126–130. [Google Scholar]
- Hamdi, H.; Richard, P.; Suteau, A.; Allain, P. Emotion assessment for affective computing based on physiological responses. In Proceedings of the 2012 IEEE International Conference on Fuzzy Systems (FUZZ-IEEE), Brisbane, Australia, 10–15 June 2012; pp. 1–8. [Google Scholar]
- Gu, Y.; Wong, K.J.; Tan, S.L. Analysis of physiological responses from multiple subjects for emotion recognition. In Proceedings of the 2012 IEEE 14th International Conference on e-Health Networking, Applications and Services (Healthcom), Beijing, China, 10–13 October 2012; pp. 178–183. [Google Scholar]
- Fleureau, J.; Guillotel, P.; Huynh-Thu, Q. Physiological-based affect event detector for entertainment video applications. IEEE Trans. Affect. Comput. 2012, 3, 379–385. [Google Scholar] [CrossRef]
- Boucsein, W. Electrodermal Activity; Springer: Boston, MA, USA, 2012. [Google Scholar]
- Moore, M.M.; Dua, U. A Galvanic Skin Response Interface for People with Severe Motor Disabilities. SIGACCESS Access. Comput. 2003, 48–54. [Google Scholar] [CrossRef]
- Egan, D.; Brennan, S.; Barrett, J.; Qiao, Y.; Timmerer, C.; Murray, N. An evaluation of Heart Rate and Electrodermal Activity as an objective QoE evaluation method for immersive virtual reality environments. In Proceedings of the 2016 Eighth International Conference on Quality of Multimedia Experience (QoMEX), Lisbon, Portugal, 6–8 June 2016; pp. 1–6. [Google Scholar]



| Description | Unit | Range | Data Type | Notes |
|---|---|---|---|---|
| Heart Rate | seconds | from 2 to 0.24 | float: 5 dec. | inter-beat interval |
| Electrodermal activity | kohms | from 0 to INF | integer | |
| Score | integer | |||
| Joint position | meters | from −5 to +5 | float: 7 dec. | for each X, Y, Z coordinates |
| Yaw, roll, pitch | radians | from 0 to 2 | float: 7 dec. | |
| Grab strength | from 0 to 1 | float: 7 dec. | 0 palm open, 1 hand closed |
| Activity Name | Activity Purpose | Devices | Performance Indicators |
|---|---|---|---|
| BreathBall | Relaxation | Microsoft Band 2 | Heart Rate, Angular coefficient |
| OwlNest | Upper limb rehab | Microsoft Kinect V2 | Score, Compensation, Barycenter, Target position |
| ShelfCans | Upper limb rehab | Microsoft Kinect V2 | Score, Compensation, Hand trajectory |
| FlappyCloud | Lower limb rehab | Microsoft Kinect V2 | Score, Compensation, Elevation |
| EquilibriumPaint | Sit to Stand | Microsoft Kinect V2 | Repetition rate, Repetition trend, Coronal shift, Shoulder shift |
| HotAir | Balance shift | Microsoft Kinect V2 | Score, CoP variation, Compensation |
| EndlessZig | Hand rehab | Leap Motion | Score, Repetition rate, Range of Motion: yaw |
| CityCar | Hand rehab | Leap Motion | Score, Repetition rate, Range of Motion: pitch |
| WineBottle | Hand rehab | Leap Motion | Score, Repetition rate, Range of Motion: roll |
| FloatingTrap | Hand rehab | Leap Motion | Score, Repetition rate, Grab strength |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morando, M.; Ponte, S.; Ferrara, E.; Dellepiane, S. Definition of Motion and Biophysical Indicators for Home-Based Rehabilitation through Serious Games. Information 2018, 9, 105. https://doi.org/10.3390/info9050105
Morando M, Ponte S, Ferrara E, Dellepiane S. Definition of Motion and Biophysical Indicators for Home-Based Rehabilitation through Serious Games. Information. 2018; 9(5):105. https://doi.org/10.3390/info9050105
Chicago/Turabian StyleMorando, Matteo, Serena Ponte, Elisa Ferrara, and Silvana Dellepiane. 2018. "Definition of Motion and Biophysical Indicators for Home-Based Rehabilitation through Serious Games" Information 9, no. 5: 105. https://doi.org/10.3390/info9050105





