The Feasibility and Functional Performance of Ternary Borate-Filled Hydrophilic Bone Cements: Targeting Therapeutic Release Thresholds for Strontium
Abstract
:1. Introduction
2. Results
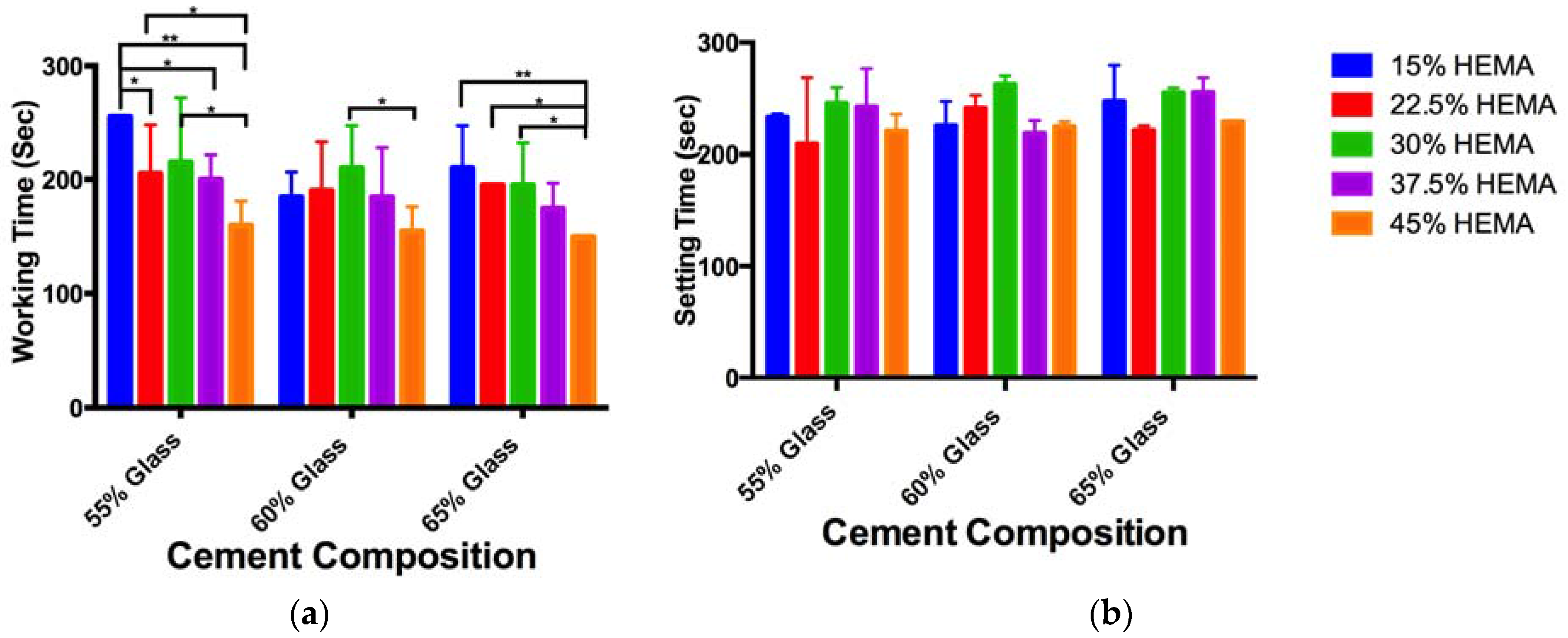
2.1. Cement Handling Properties
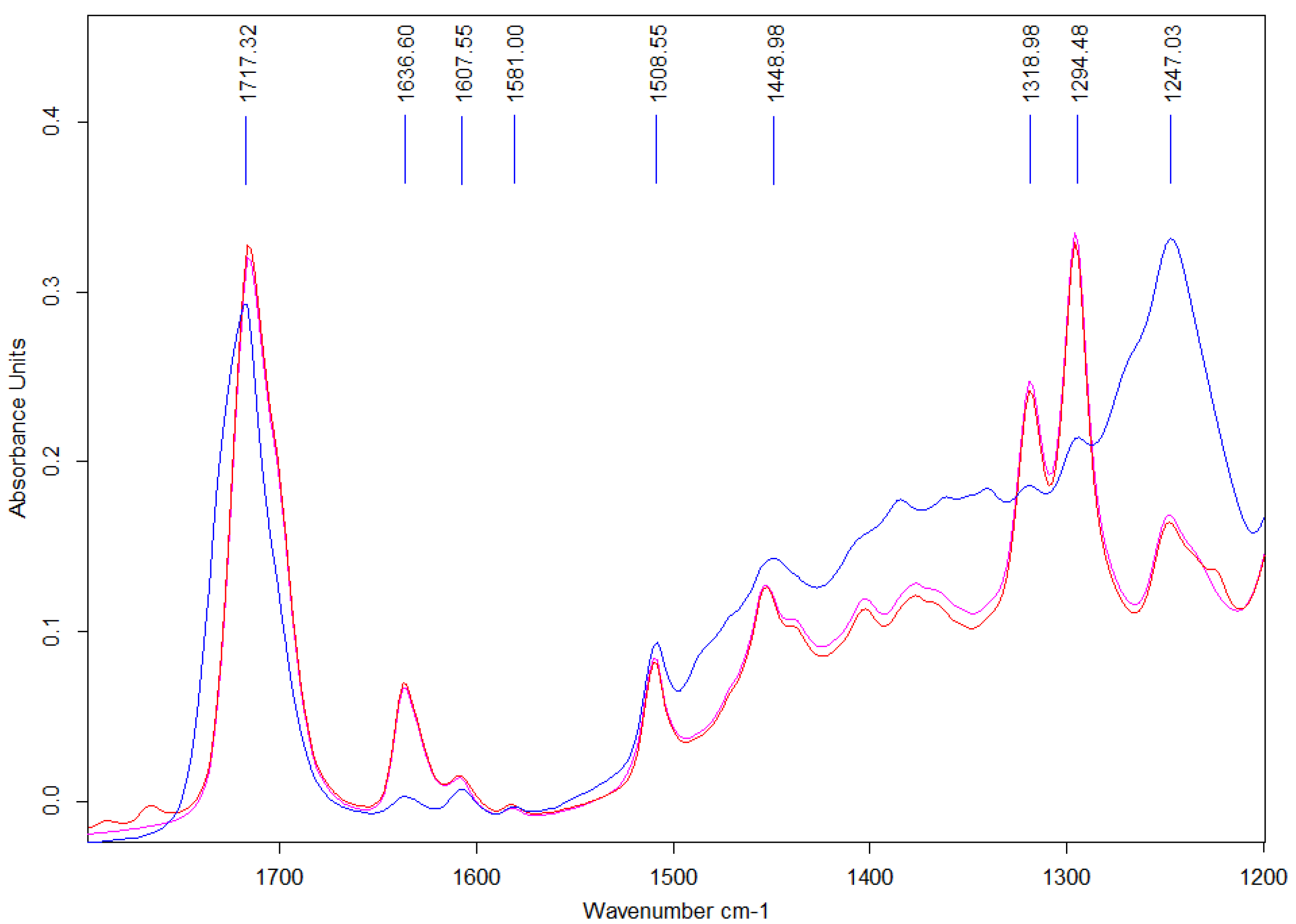
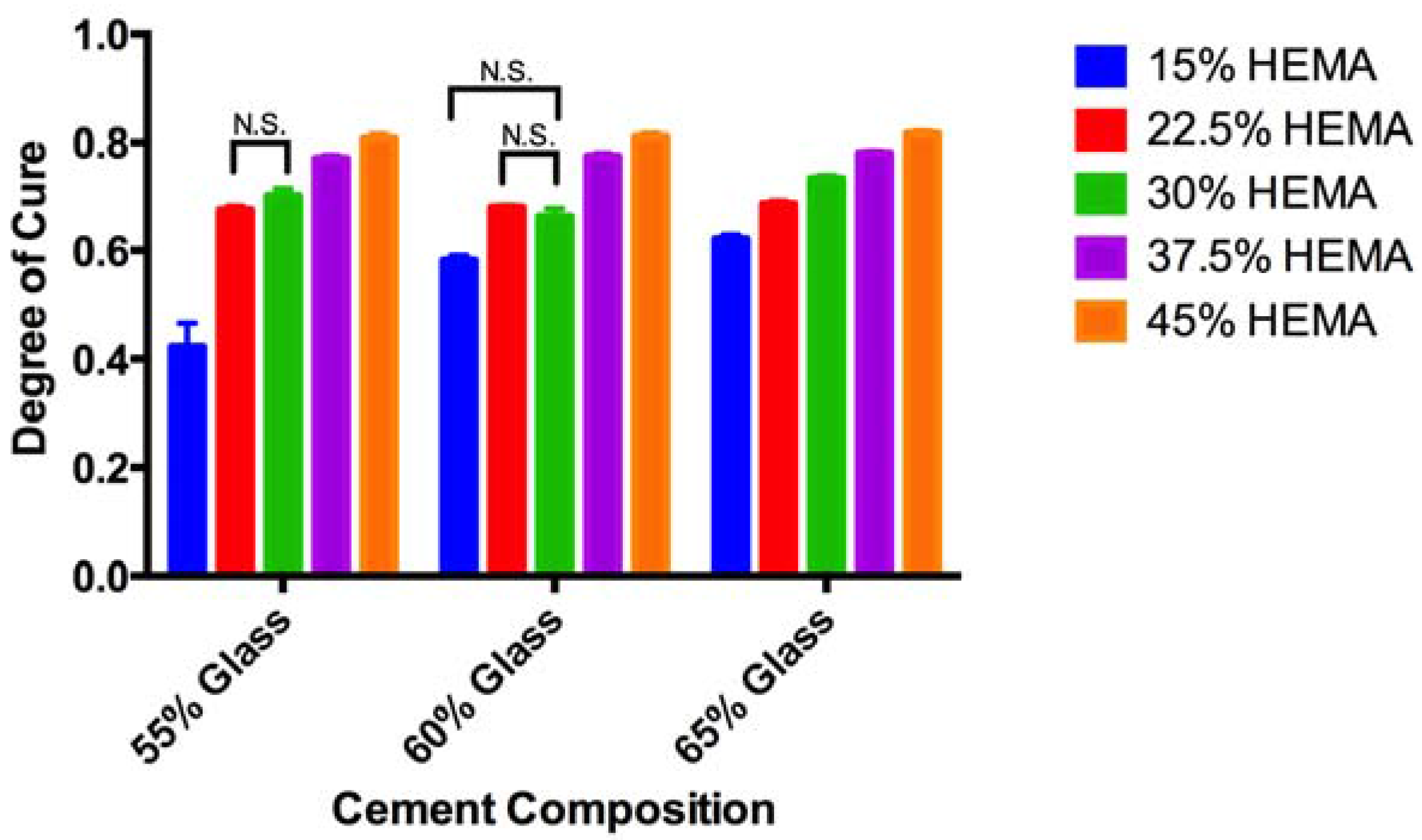
2.2. ATR-FTIR Degree of Conversion
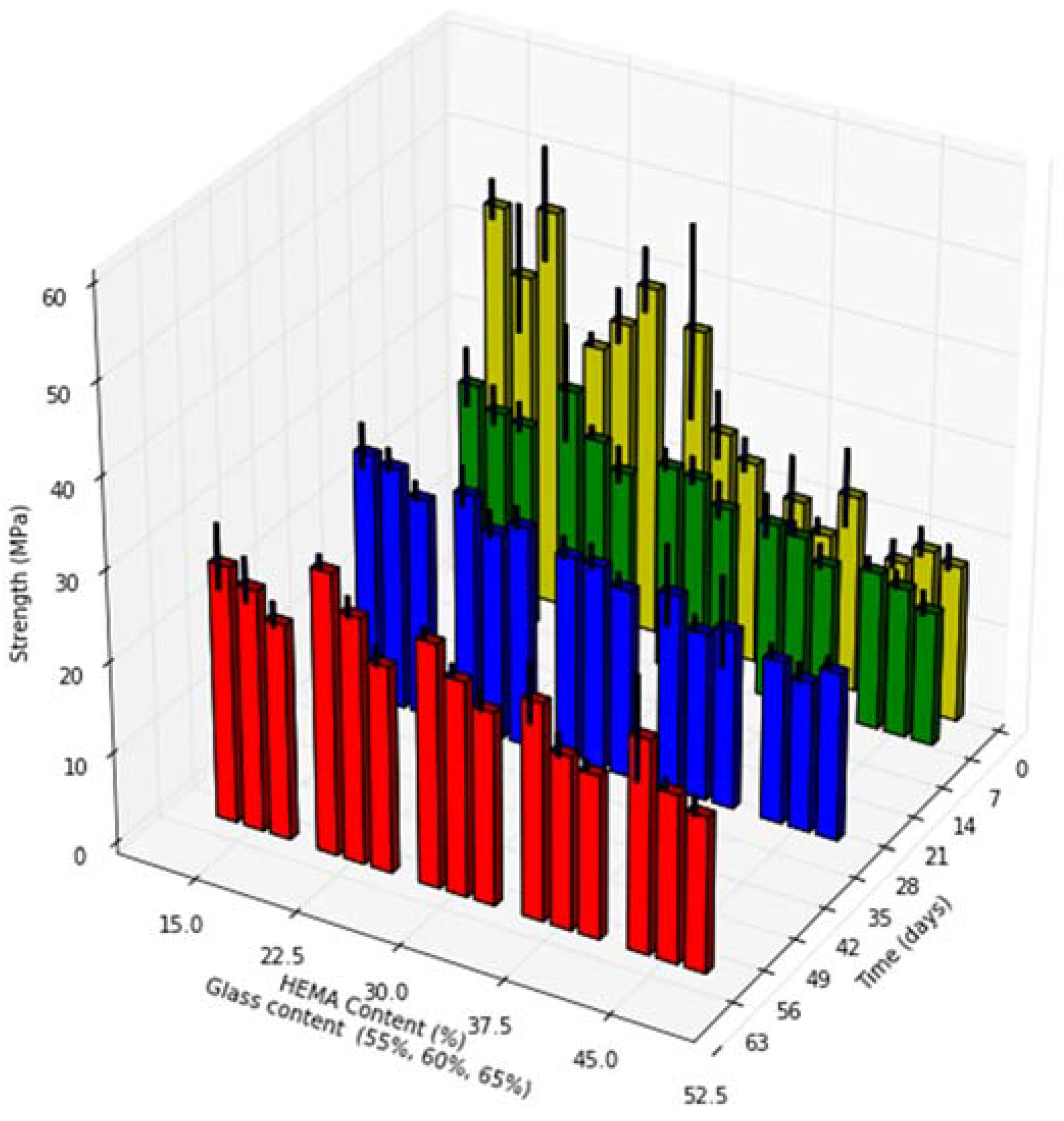
2.3. Biaxial Flexural Strength
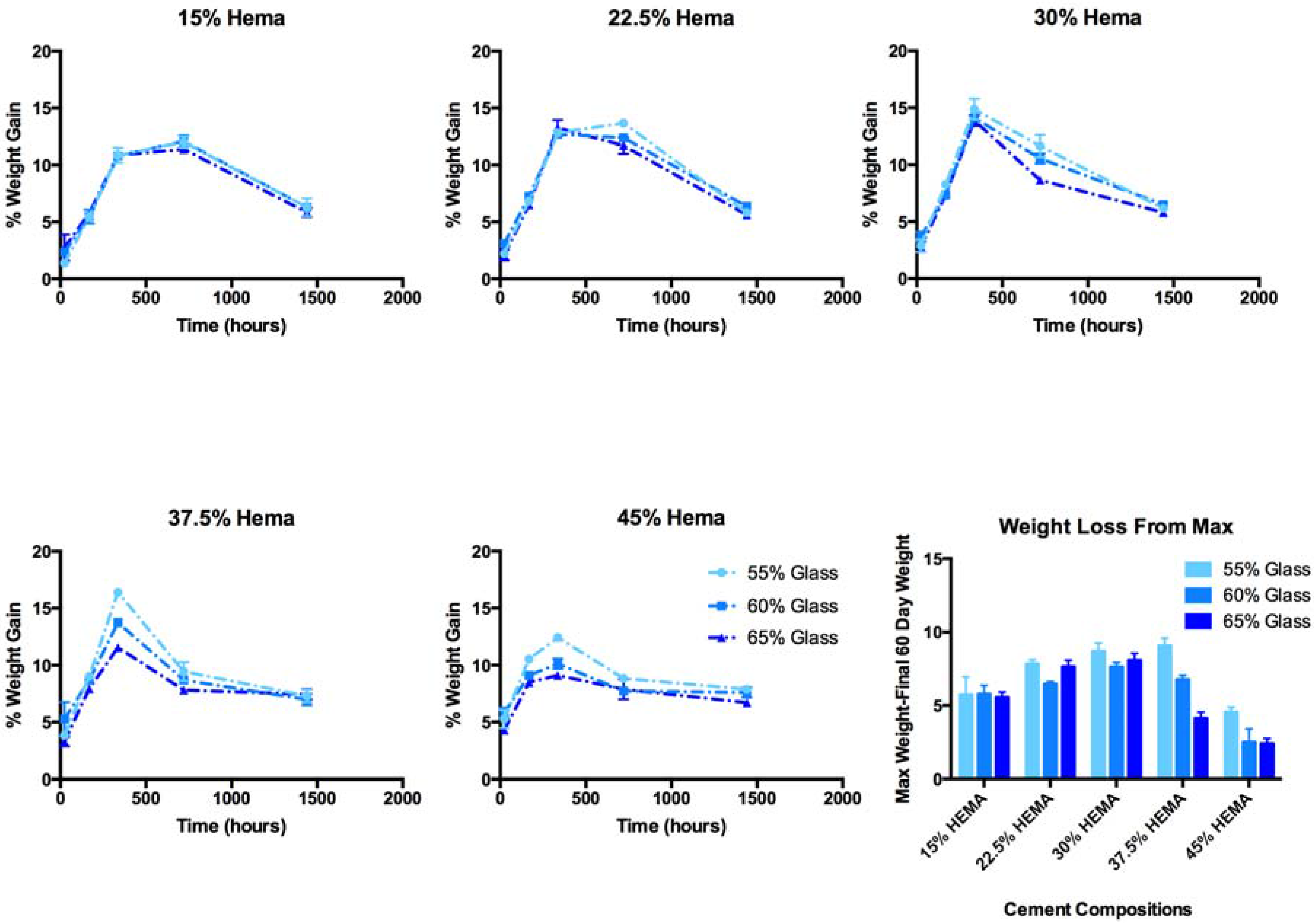
2.4. Cement Water Sorption and Weight Loss
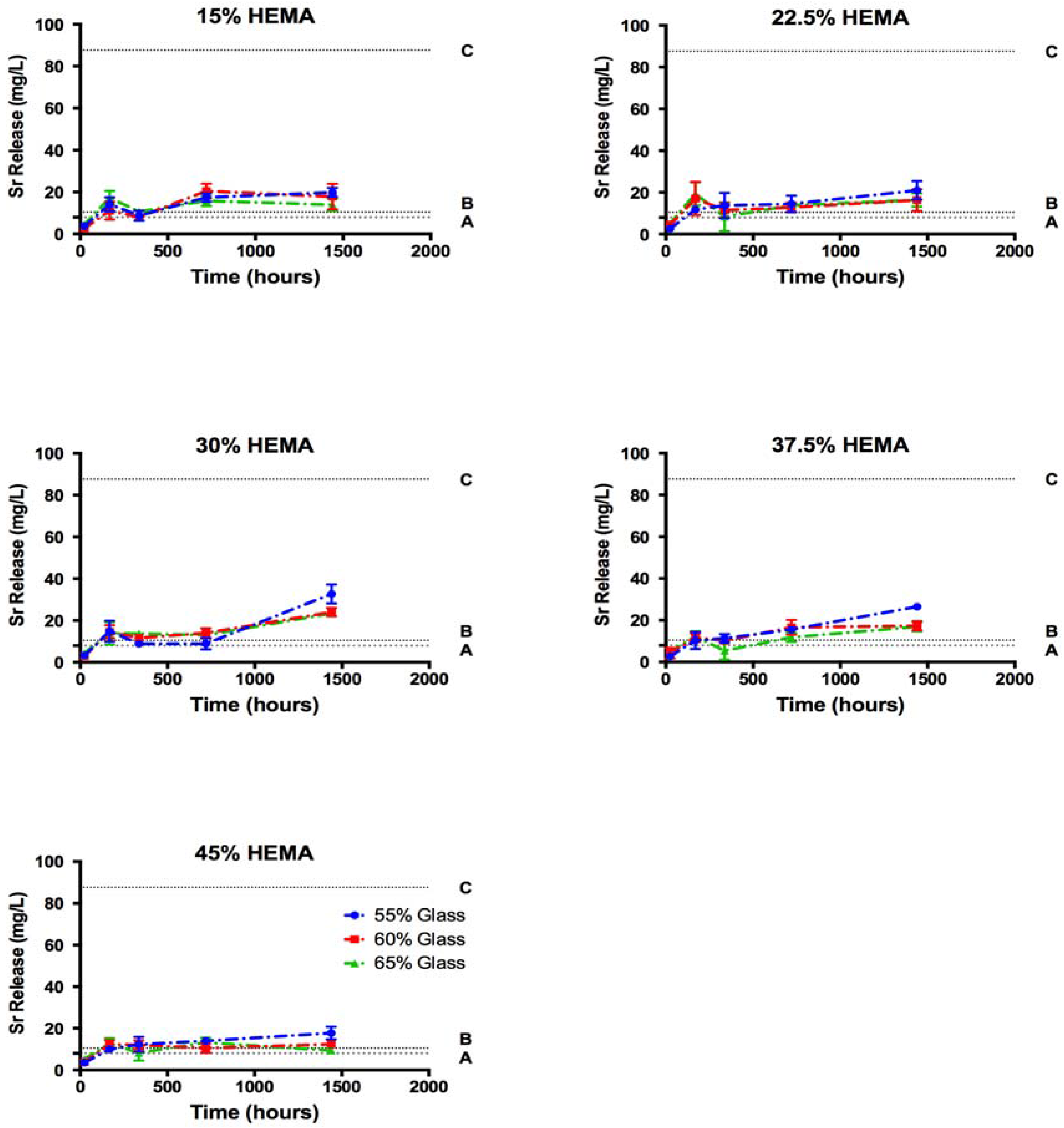
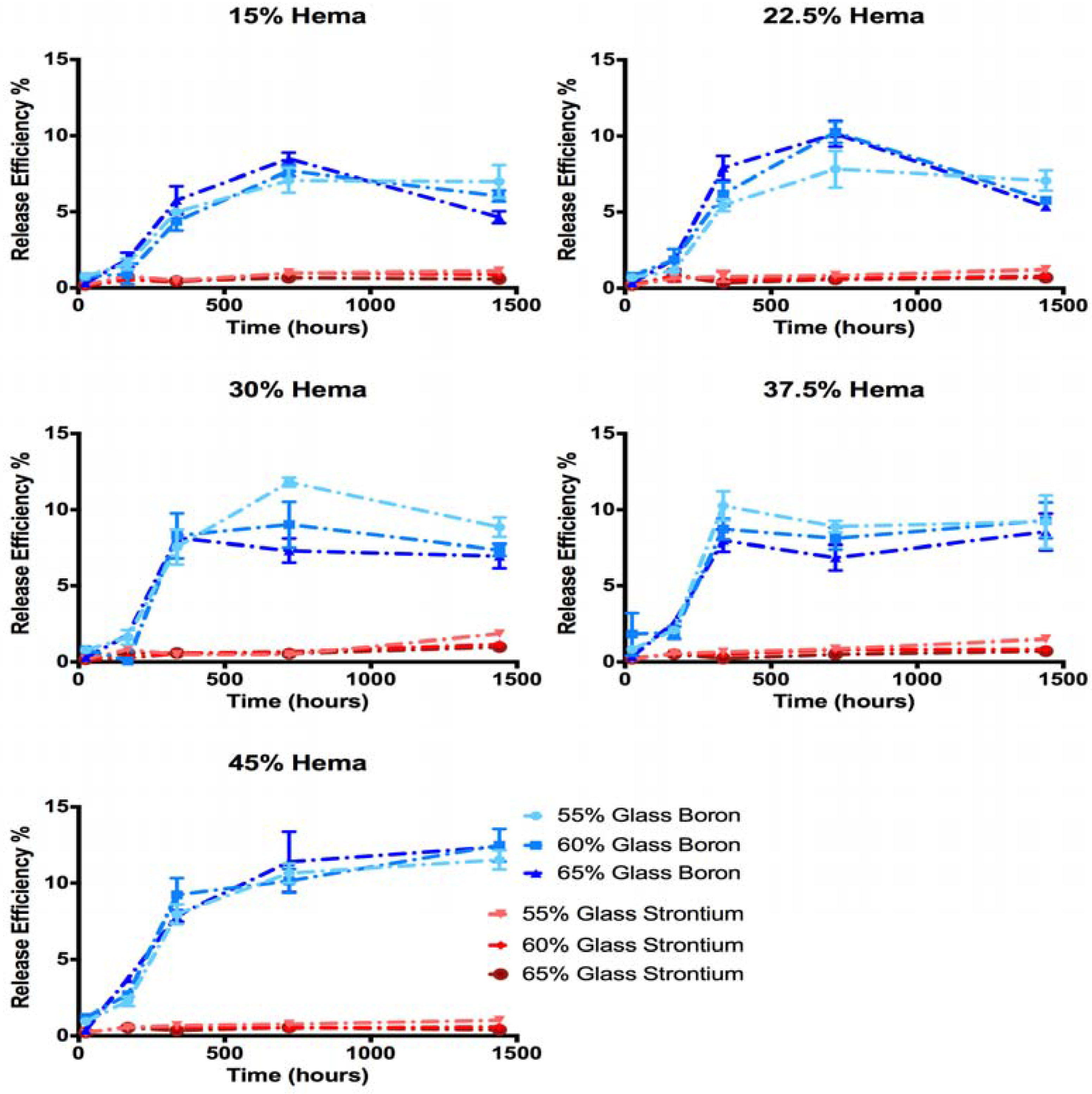
2.5. Ion Release
3. Discussion
4. Materials and Methods
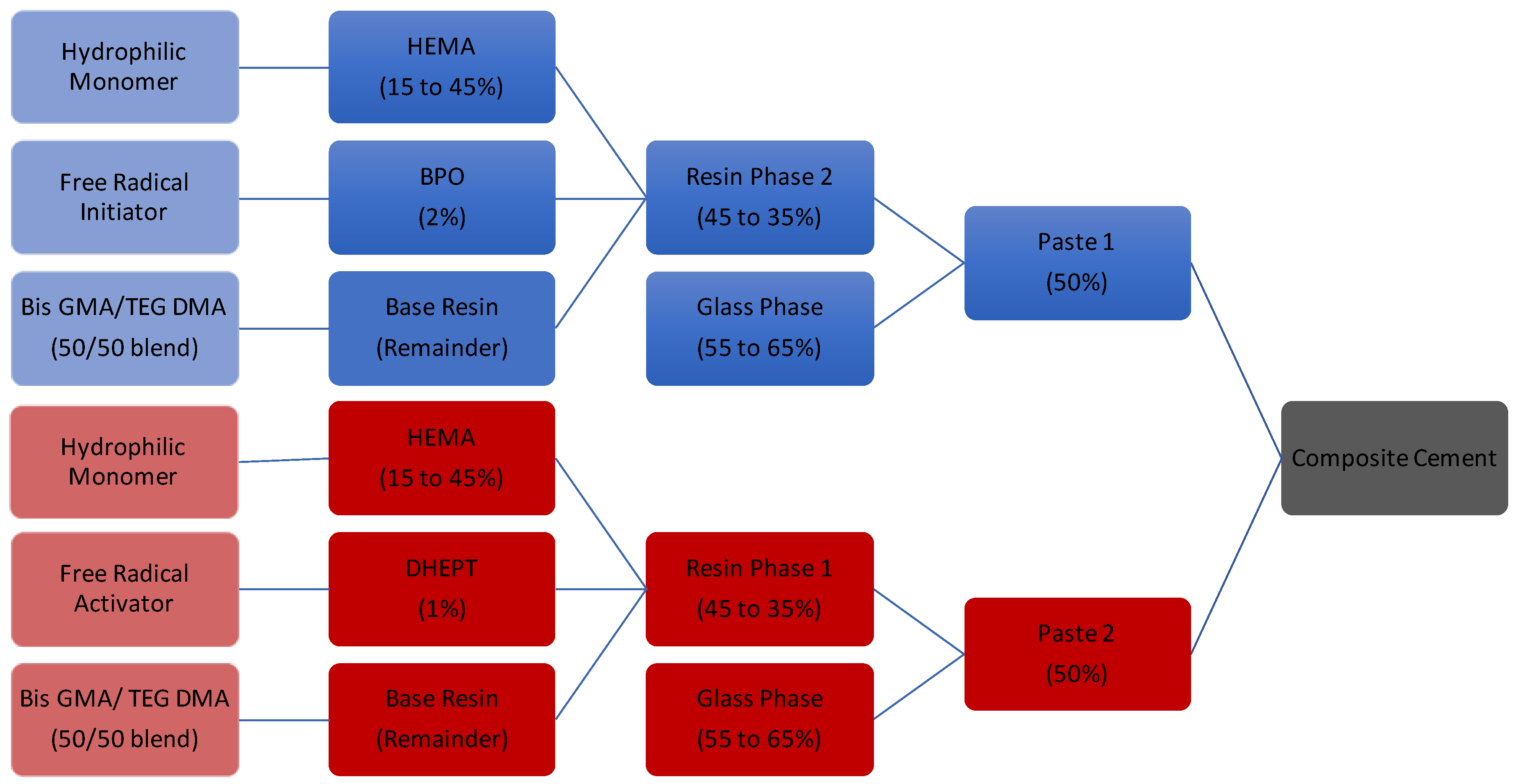
4.1. Cement Fabrication
4.2. Cement Handling Characteristics
4.3. Degree of Conversion
4.4. Biaxial Flexural Strength
4.5. Cement Water Sorption and Weight Loss
4.6. Ion Release Profiles
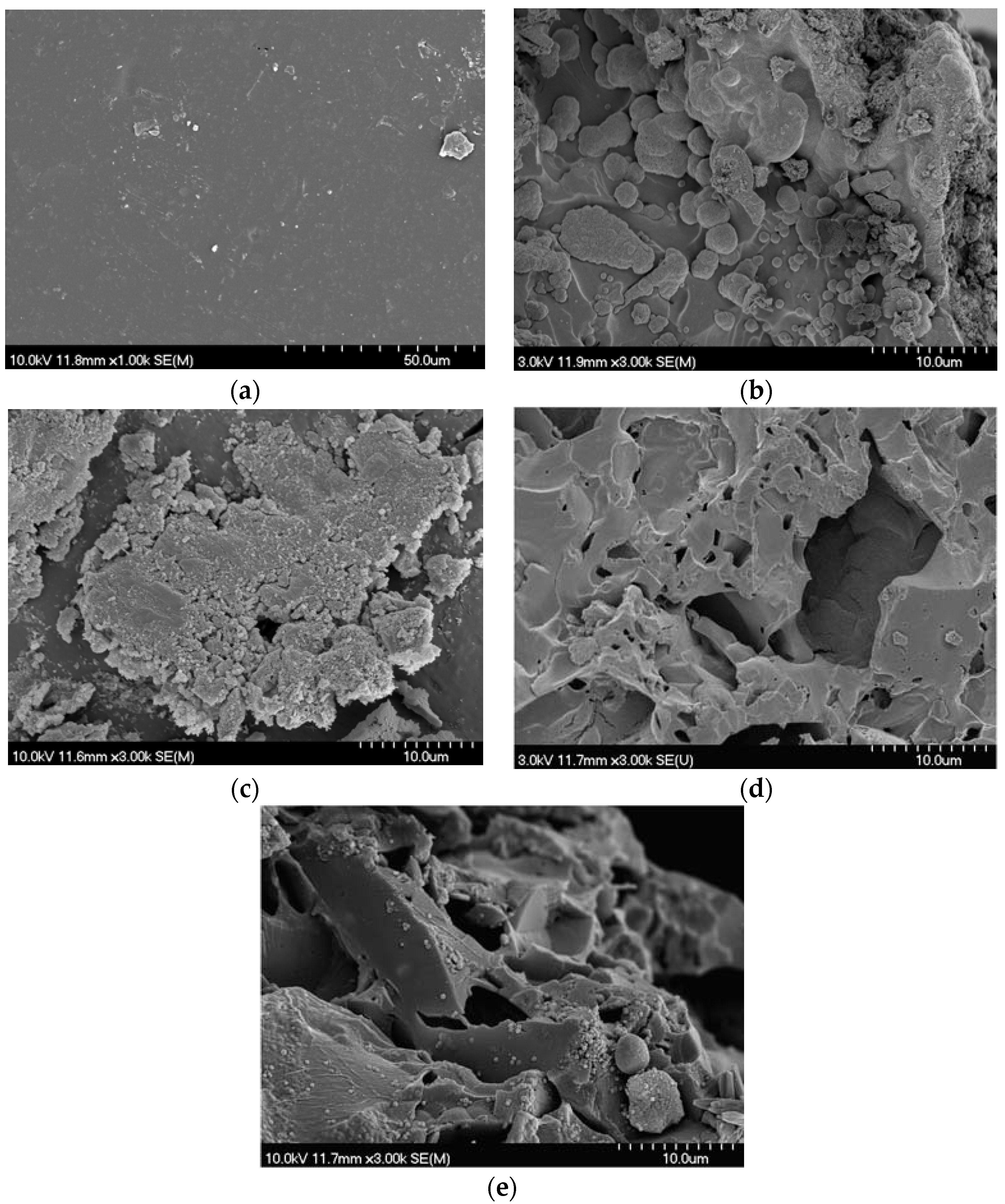
4.7. SEM Analysis of Weight Loss Samples
4.8. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Grynpas, M.; Marie, P. Effects of low doses of strontium on bone quality and quantity in rats. Bone 1990, 11, 313–319. [Google Scholar] [CrossRef]
- Ammann, P.; Shen, V.; Robin, B.; Mauras, Y.; Bonjour, J.; Rizzoli, R. Strontium ranelate improves bone resistance by increasing bone mass and improving architecture in intact female rats. J. Bone Miner. Res. 2004, 19, 2012–2020. [Google Scholar] [CrossRef] [PubMed]
- Marie, P.J. Mechanisms of action and therapeutic potential of strontium in bone. Calcif. Tissue Int. 2001, 69, 121. [Google Scholar] [CrossRef] [PubMed]
- Meunier, P.J.; Roux, C.; Seeman, E.; Ortolani, S.; Badurski, J.E.; Spector, T.D.; Cannata, J.; Balogh, A.; Lemmel, E.; Pors-Nielsen, S.; Rizzoli, R.; Genant, H.K.; Reginster, J. The Effects of Strontium Ranelate on the Risk of Vertebral Fracture in Women with Postmenopausal Osteoporosis. N. Engl. J. Med. 2004, 350, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Stepan, J.J. Strontium ranelate: In search for the mechanism of action. J. Bone Miner. Metab. 2013, 31, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Bonnelye, E.; Chabadel, A.; Saltel, F.; Jurdic, P. Dual effect of strontium ranelate: Stimulation of osteoblast differentiation and inhibition of osteoclast formation and resorption in vitro. Bone 2008, 42, 129–138. [Google Scholar] [PubMed]
- Marie, P.J. Signaling pathways affecting skeletal health. Curr. Osteoporos. Rep. 2012, 10, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Marie, P.; Felsenberg, D.; Brandi, M. How strontium ranelate, via opposite effects on bone resorption and formation, prevents osteoporosis. Osteoporos. Int. 2011, 22, 1659–1667. [Google Scholar] [CrossRef] [PubMed]
- Blake, G.M.; Lewiecki, E.M.; Kendler, D.L.; Fogelman, I. A review of strontium ranelate and its effect on DXA scans. J. Clin. Densitom. 2007, 10, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Saidak, Z.; Marie, P.J. Strontium signaling: Molecular mechanisms and therapeutic implications in osteoporosis. Pharmacol. Ther. 2012, 136, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Alkhraisat, M.H.; Rueda, C.; Cabrejos-Azama, J.; Lucas-Aparicio, J.; Mariño, F.T.; Torres García-Denche, J.; Jerez, L.B.; Gbureck, U.; Cabarcos, E.L. Loading and release of doxycycline hyclate from strontium-substituted calcium phosphate cement. Acta Biomater. 2010, 6, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Chen, F.; Song, W.; Song, Y.; Chen, Y.; Wan, C.; Yu, X.; Zhang, X. In vivo study of porous strontium-doped calcium polyphosphate scaffolds for bone substitute applications. J. Mater. Sci. Mater. Med. 2009, 20, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Reginster, J.; Deroisy, R.; Jupsin, I. Strontium ranelate: A new paradigm in the treatment of osteoporosis. Drugs Today 2003, 39, 89–101. [Google Scholar] [CrossRef] [PubMed]
- Wornham, D.; Hajjawi, M.; Orriss, I.; Arnett, T. Strontium potently inhibits mineralisation in bone-forming primary rat osteoblast cultures and reduces numbers of osteoclasts in mouse marrow cultures. Osteoporos. Int. 2014, 25, 2477–2484. [Google Scholar] [CrossRef] [PubMed]
- Hurtel-Lemaire, A.S.; Mentaverri, R.; Caudrillier, A.; Cournarie, F.; Wattel, A.; Kamel, S.; Terwilliger, E.F.; Brown, E.M.; Brazier, M. The calcium-sensing receptor is involved in strontium ranelate-induced osteoclast apoptosis. New insights into the associated signaling pathways. J. Biol. Chem. 2009, 284, 575–584. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services Toxicological Profile for Strontium; Public Health Service, Agency for Toxic Substances and Disease Registry: Atlanta, GA, USA, 2004.
- Er, K. Cytotoxicity analysis of strontium ranelate on cultured human periodontal ligament fibroblasts: A preliminary report. J. Formosan Med. Assoc. 2008, 107, 609–615. [Google Scholar] [CrossRef]
- Panzavolta, S.; Torricelli, P.; Sturba, L.; Bracci, B.; Giardino, R.; Bigi, A. Setting properties and in vitro bioactivity of strontium-enriched gelatin–calcium phosphate bone cements. J. Biomed. Mater. Res. Part A 2008, 84, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.M.; FHKCOS, F.O.; Lu, W.W.; Wong, C.; Chan, D.; Shen, J.; Qiu, G.; Zheng, Z.; Li, C.; Liu, S. Vertebroplasty by Use of a Strontium-Containing Bioactive Bone Cement. Spine 2005, 30, S84–S91. [Google Scholar] [CrossRef] [PubMed]
- Guo, D. Development of a strontium-containing hydroxyapatite bone cement. Biomaterials 2005, 26, 4073–4083. [Google Scholar] [CrossRef] [PubMed]
- Johal, K.; Mendoza-Suarez, G.; Escalante-Garcia, J.; Hill, R.; Brook, I. In vivo response of strontium and zinc-based ionomeric cement implants in bone. J. Mater. Sci. Mater. Med. 2002, 13, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ye, J.; Wang, Y. Influence of a novel radiopacifier on the properties of an injectable calcium phosphate cement. Acta Biomater. 2007, 3, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.; Lu, W.; Luk, K.; Cheung, K.; Wong, C.; Leong, J.; Yao, K. Surface treatment of injectable strontium-containing bioactive bone cement for vertebroplasty. J. Biomed. Mater. Res. Part B 2004, 69, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Lam, W.; Pan, H.; Fong, M.; Cheung, W.; Wong, K.; Li, Z.; Luk, K.; Chan, W.; Wong, C.; Yang, C. In Vitro characterization of low modulus linoleic acid coated strontium-substituted hydroxyapatite containing PMMA bone cement. J. Biomed. Mater. Res. Part B 2011, 96, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Tadier, S.; Bareille, R.; Siadous, R.; Marsan, O.; Charvillat, C.; Cazalbou, S.; Amédée, J.; Rey, C.; Combes, C. Strontium-loaded mineral bone cements as sustained release systems: Compositions, release properties, and effects on human osteoprogenitor cells. J. Biomed. Mater. Res. Part B 2012, 100, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Leong, J.; Lu, W.; Luk, K.; Cheung, K.; Chiu, K.; Chow, S. A novel injectable bioactive bone cement for spinal surgery: A developmental and preclinical study. J. Biomed. Mater. Res. 2000, 52, 164–170. [Google Scholar] [CrossRef]
- Lewis, G. Injectable bone cements for use in vertebroplasty and kyphoplasty: State-of-the-art review. J. Biomed. Mater. Res. Part B 2006, 76, 456–468. [Google Scholar] [CrossRef] [PubMed]
- Erbe, E.M.; Clineff, T.D.; Gualtieri, G. Comparison of a new bisphenol-a-glycidyl dimethacrylate-based cortical bone void filler with polymethyl methacrylate. Eur. Spine J. 2001, 10 (Suppl. 2), S147–S152. [Google Scholar] [CrossRef] [PubMed]
- Vorndran, E.; Spohn, N.; Nies, B.; Rößler, S.; Storch, S.; Gbureck, U. Mechanical properties and drug release behavior of bioactivated PMMA cements. J. Biomater. Appl. 2012, 26, 581–594. [Google Scholar] [CrossRef] [PubMed]
- Frutos, P.; Diez-Pena, E.; Frutos, G.; Barrales-Rienda, J. Release of gentamicin sulphate from a modified commercial bone cement. Effect of (2-hydroxyethyl methacrylate) comonomer and poly (N-vinyl-2-pyrrolidone) additive on release mechanism and kinetics. Biomaterials 2002, 23, 3787–3797. [Google Scholar] [CrossRef]
- Chan, W.D.; Yang, L.; Wan, W.; Rizkalla, A.S. Fluoride release from dental cements and composites: A mechanistic study. Dent. Mater. 2006, 22, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Skrtic, D. Effect of the monomer and filler systems on the remineralizing potential of bioactive dental composites based on amorphous calcium phosphate. Polym. Adv. Technol. 2001, 12, 369–379. [Google Scholar] [CrossRef]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef] [PubMed]
- George, J.L. Dissolution of Borate Glasses and Precipitation of Phosphate Compounds. Ph.D. Thesis, Missouri University of Science and Technology, Rolla, MO, USA, 2015. [Google Scholar]
- MacDonald, K.; Hanson, M.A.; Boyd, D. Modulation of strontium release from a tertiary borate glass through substitution of alkali for alkali earth oxide. J. Non-Cryst. Solids. 2016, 443, 184–191. [Google Scholar] [CrossRef]
- Matinlinna, J.P.; Lassila, L.V.; Özcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 156–164. [Google Scholar]
- Collares, F.M.; Ogliari, F.A.; Zanchi, C.H.; Petzhold, C.L.; Piva, E.; Samuel, S.M. Influence of 2-hydroxyethyl methacrylate concentration on polymer network of adhesive resin. J. Adhes. Dent. 2011, 13, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, J.M.; Fowler, B.O.; Weir, M.D.; Skrtic, D.; Stansbury, J.W. Effect of ethyl-α-hydroxymethylacrylate on selected properties of copolymers and ACP resin composites. J. Mater. Sci. Mater. Med. 2008, 19, 3263–3271. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L.; Greener, E.H. Fourier transform infrared analysis of degree of polymerization in unfilled resins--methods comparison. J. Dent. Res. 1984, 63, 1093–1095. [Google Scholar] [CrossRef] [PubMed]
- Balachandera, L.; Ramadevudub, G.; Shareefuddina, M.; Sayannac, R.; Venudharc, Y. IR analysis of borate glasses containing three alkali oxides. ScienceAsia 2013, 39, 278. [Google Scholar] [CrossRef]
- Stein, S.E. “Infrared Spectra” by NIST Mass Spec Data Center. In NIST Chenistry WebBook NIST Standard Reference Database Number 69; Lindstrom, P.J., Mallard, W.G., Eds.; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2016. [Google Scholar]
- Fleming, G.J.; Dowling, A.H.; Addison, O. The crushing truth about glass ionomer restoratives: Exposing the standard of the standard. J. Dent. 2012, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Pomrink, G.J.; DiCicco, M.P.; Clineff, T.D.; Erbe, E.M. Evaluation of the reaction kinetics of CORTOSS, a thermoset cortical bone void filler. Biomaterials 2003, 24, 1023–1031. [Google Scholar] [CrossRef]
- Lai, P.; Tai, C.; Chu, I.; Fu, T.; Chen, L.; Chen, W. Hypothermic manipulation of bone cement can extend the handling time during vertebroplasty. BMC Musculoskelet. Disord. 2012, 13, 198. [Google Scholar] [CrossRef] [PubMed]
- Bakopoulou, A.; Papadopoulos, T.; Garefis, P. Molecular toxicology of substances released from resin–based dental restorative materials. Int. J. Mol. Sci. 2009, 10, 3861–3899. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; McCabe, J.F.; Tarumi, H.; Ehara, A.; Ebisu, S. Degree of conversion of composites measured by DTA and FTIR. Dent. Mater. 2001, 17, 178–183. [Google Scholar] [CrossRef]
- Boyd, D.; Towler, M.; Wren, A.; Clarkin, O. Comparison of an experimental bone cement with surgical Simplex® P, Spineplex® and Cortoss®. J. Mater. Sci. Mater. Med. 2008, 19, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G. Properties of acrylic bone cement: State of the art review. J. Biomed. Mater. Res. 1997, 38, 155–182. [Google Scholar] [CrossRef]
- Goncalves, F.; Kawano, Y.; Pfeifer, C.; Stansbury, J.W.; Braga, R.R. Influence of BisGMA, TEGDMA, and BisEMA contents on viscosity, conversion, and flexural strength of experimental resins and composites. Eur. J. Oral Sci. 2009, 117, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Clarkin, O.; Boyd, D.; Madigan, S.; Towler, M. Comparison of an experimental bone cement with a commercial control, Hydroset™. J. Mater. Sci. Mater. Med. 2009, 20, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.; Yap, A.; Chandra, S.; Lim, C. Flexural strength of dental composite restoratives: Comparison of biaxial and three-point bending test. J. Biomed. Mater. Res. Part B 2004, 71, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Zainuddin, Z.; Hill, D.J.; Chirila, T.V.; Whittaker, A.K.; Kemp, A. Experimental calcification of HEMA-based hydrogels in the presence of albumin and a comparison to the in vivo calcification. Biomacromolecules 2006, 7, 1758–1765. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, M.; Lode, A.; Helth, A.; Gelinsky, M. A novel strontium (II)-modified calcium phosphate bone cement stimulates human-bone-marrow-derived mesenchymal stem cell proliferation and osteogenic differentiation in vitro. Acta. Biomater. 2013, 9, 9547–9557. [Google Scholar] [CrossRef] [PubMed]
- Powers, J.M.; Sakaguchi, R.L. Craig’s Restorative Dental Materials; Mosby: St. Louis, MO, USA, 2006. [Google Scholar]
- ISO. 9917–1: Dentistry-Water-Based Cements—Part 1: Powder/Liquid Acid–Base Cements; International Organization for Standardization: Geneva, Switzerland, 2007. [Google Scholar]
- ISO. 5833–2002. Implants for Surgery—Acrylic Resin Cements; International Standards Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Dickey, B.T.; Kehoe, S.; Boyd, D. Novel adaptations to zinc–silicate glass polyalkenoate cements: The unexpected influences of germanium based glasses on handling characteristics and mechanical properties. J. Mech. Behav. Biomed. Mater. 2013, 23, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Eliades, T.; Eliades, G.; Brantley, W.A.; Johnston, W.M. Polymerization efficiency of chemically cured and visible light-cured orthodontic adhesives: Degree of cure. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 294–301. [Google Scholar] [CrossRef]
| Composite | Group A | Group B | Group C | Group D | Group E | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | ||
| Resin Phase Part One | Bis-GMA | 41.474 | 37.725 | 33.975 | 30.225 | 26.475 | ||||||||||
| TEGDMA | 41.475 | 37.725 | 33.975 | 30.225 | 26.475 | |||||||||||
| HEMA | 15 | 22.5 | 30 | 37.5 | 45 | |||||||||||
| BPO | 2 | 2 | 2 | 2 | 2 | |||||||||||
| Resin Phase Part Two | Bis-GMA | 42 | 38.25 | 34.5 | 30.75 | 27 | ||||||||||
| TEGDMA | 42 | 38.25 | 34.5 | 30.75 | 27 | |||||||||||
| HEMA | 15 | 22.5 | 30 | 37.5 | 45 | |||||||||||
| DHEPT | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||||||||
| Glass | 55 | 60 | 65 | 55 | 60 | 65 | 55 | 60 | 65 | 55 | 60 | 65 | 55 | 60 | 65 | |
| Band Region (cm−1) | Cement Component | Functional Group | Reference |
|---|---|---|---|
| 1700–1720 | Resin | C=O and C=O hydrogen bonding | [38] |
| 1630–1640 | Resin | C=C double bonds | [39] |
| 1600–1610 | Resin | Aromatic Rings | [39] |
| 1500–1520 | Glass | Non Bridging oxygen stretching | [40] |
| 1280–1320 (2 peaks) | Glass | Boron-oxygen ring vibrations | [40] |
| 1240 | Glass | Ortho and Pyro borate asymmetric bond stretching | [40] |
| 1767 & 1790 | Initiator | Benzyl Peroxide Ring Vibration | [41] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
MacDonald, K.; Price, R.B.; Boyd, D. The Feasibility and Functional Performance of Ternary Borate-Filled Hydrophilic Bone Cements: Targeting Therapeutic Release Thresholds for Strontium. J. Funct. Biomater. 2017, 8, 28. https://doi.org/10.3390/jfb8030028
MacDonald K, Price RB, Boyd D. The Feasibility and Functional Performance of Ternary Borate-Filled Hydrophilic Bone Cements: Targeting Therapeutic Release Thresholds for Strontium. Journal of Functional Biomaterials. 2017; 8(3):28. https://doi.org/10.3390/jfb8030028
Chicago/Turabian StyleMacDonald, Kathleen, Richard B. Price, and Daniel Boyd. 2017. "The Feasibility and Functional Performance of Ternary Borate-Filled Hydrophilic Bone Cements: Targeting Therapeutic Release Thresholds for Strontium" Journal of Functional Biomaterials 8, no. 3: 28. https://doi.org/10.3390/jfb8030028




