Effect of a Particulate and a Putty-Like Tricalcium Phosphate-Based Bone-grafting Material on Bone Formation, Volume Stability and Osteogenic Marker Expression after Bilateral Sinus Floor Augmentation in Humans
Abstract
:1. Introduction
2. Materials und Methods
2.1. Test Materials
2.2. Patient Selection
2.3. Radiological Examination
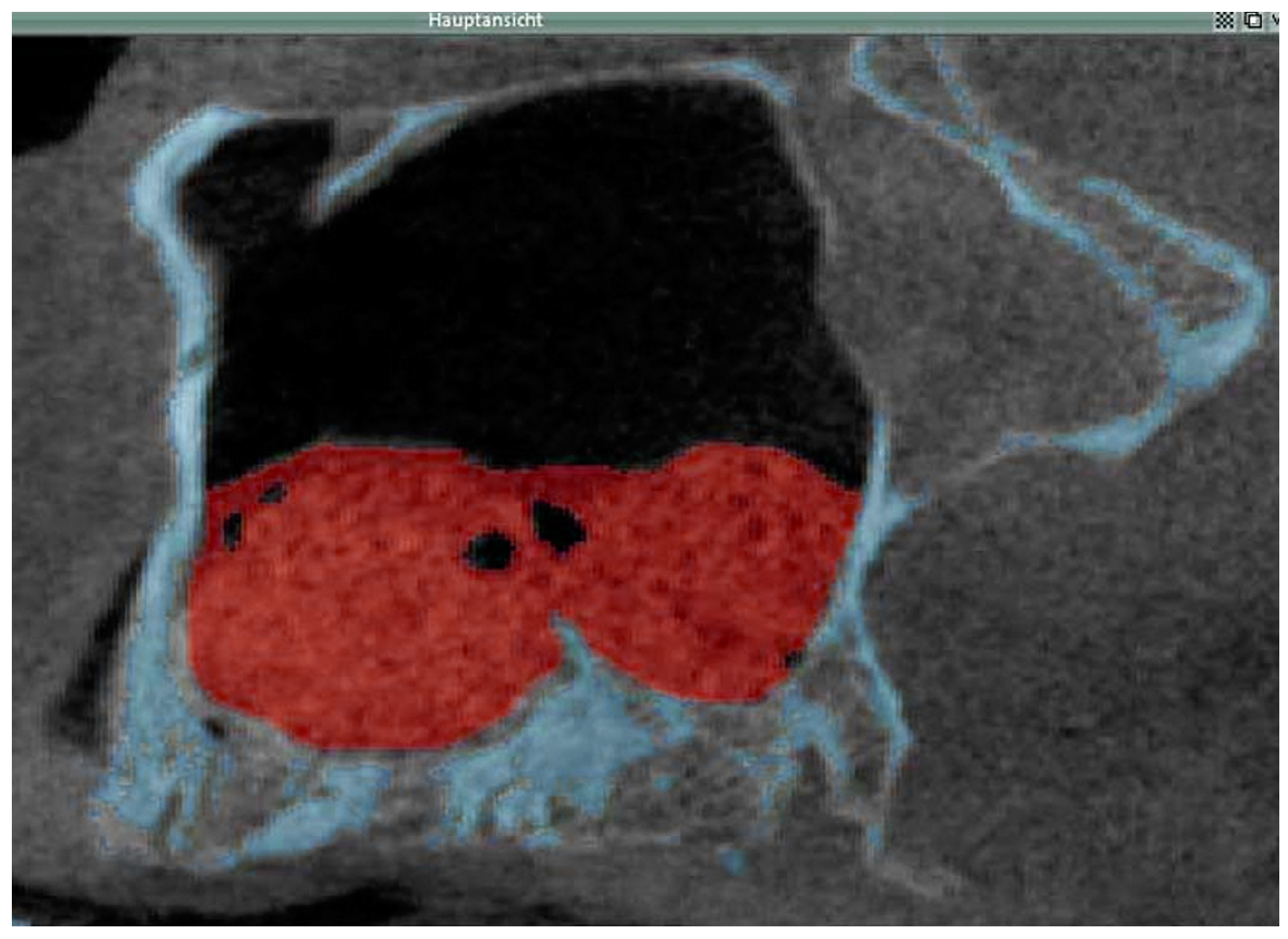
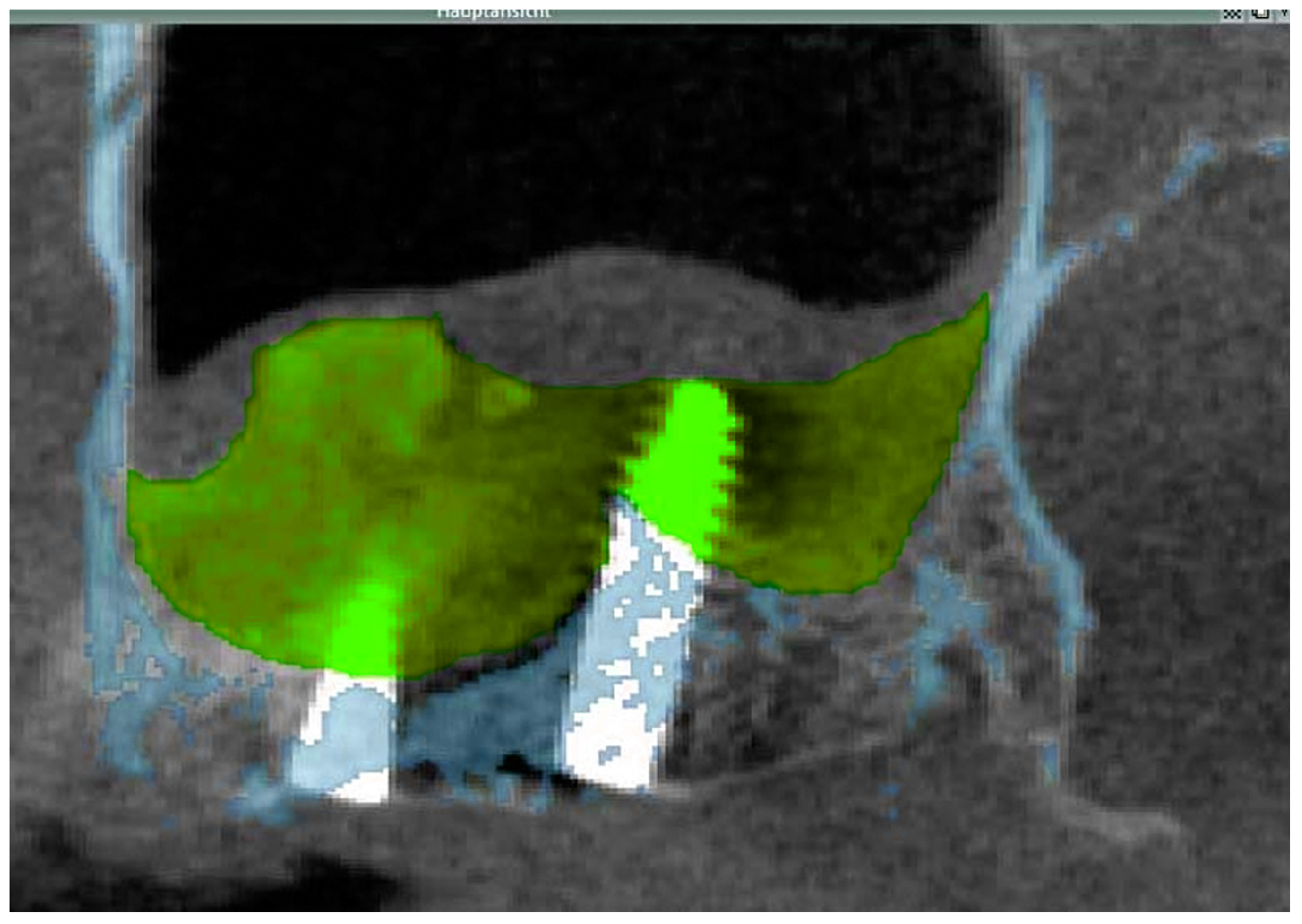
2.3.1. Cone Beam CT
2.3.2. Data Transfer, Analysis and Volume Determination
2.4. Sinus Floor Elevation
2.5. Dental Implant Surgery and Biopsy Specimen Retrieval
2.6. Preparation of Biopsy Specimens for Histomorphometry and Immunohistochemistry
2.7. Statistical Analysis
3. Results
3.1. Clinical Findings
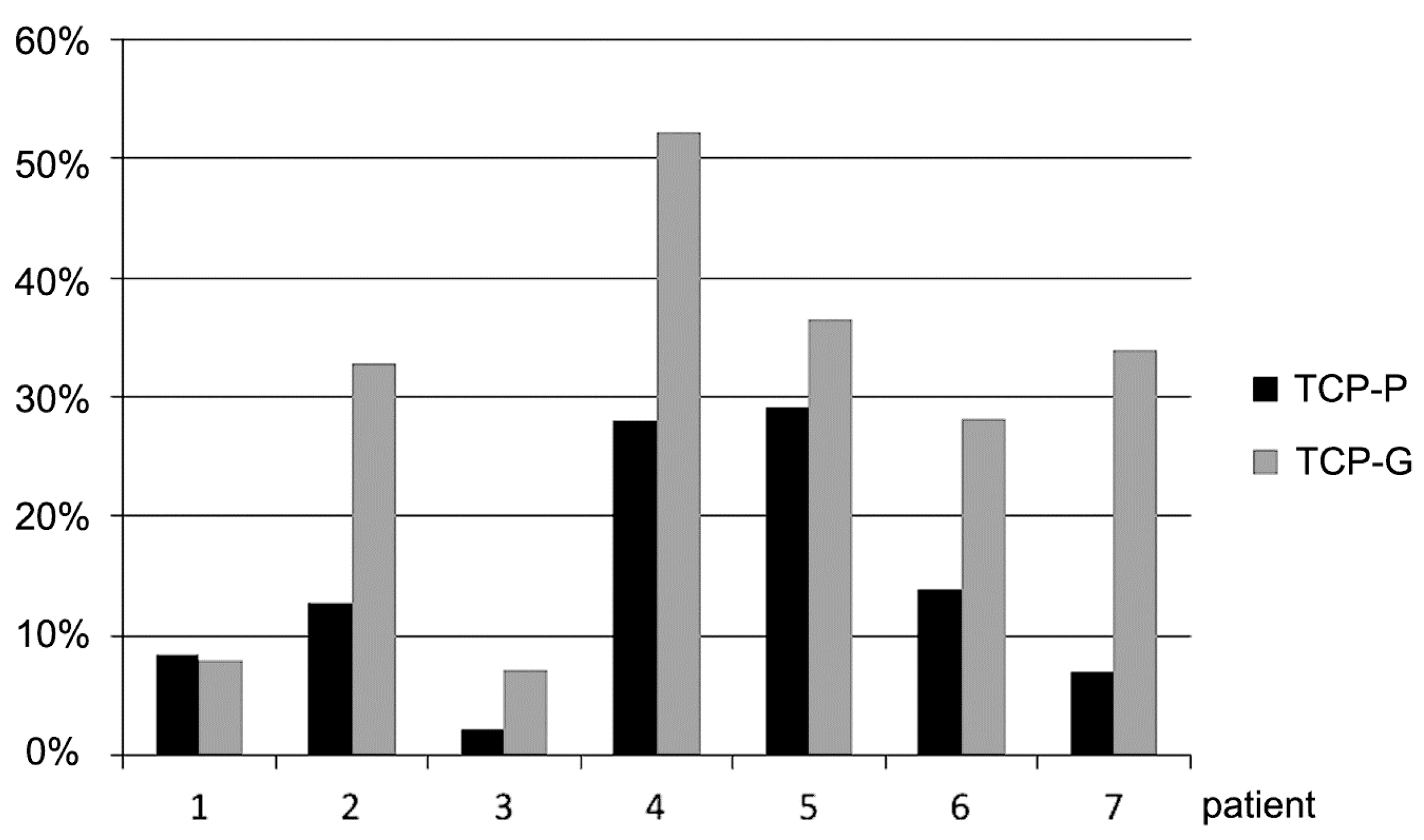
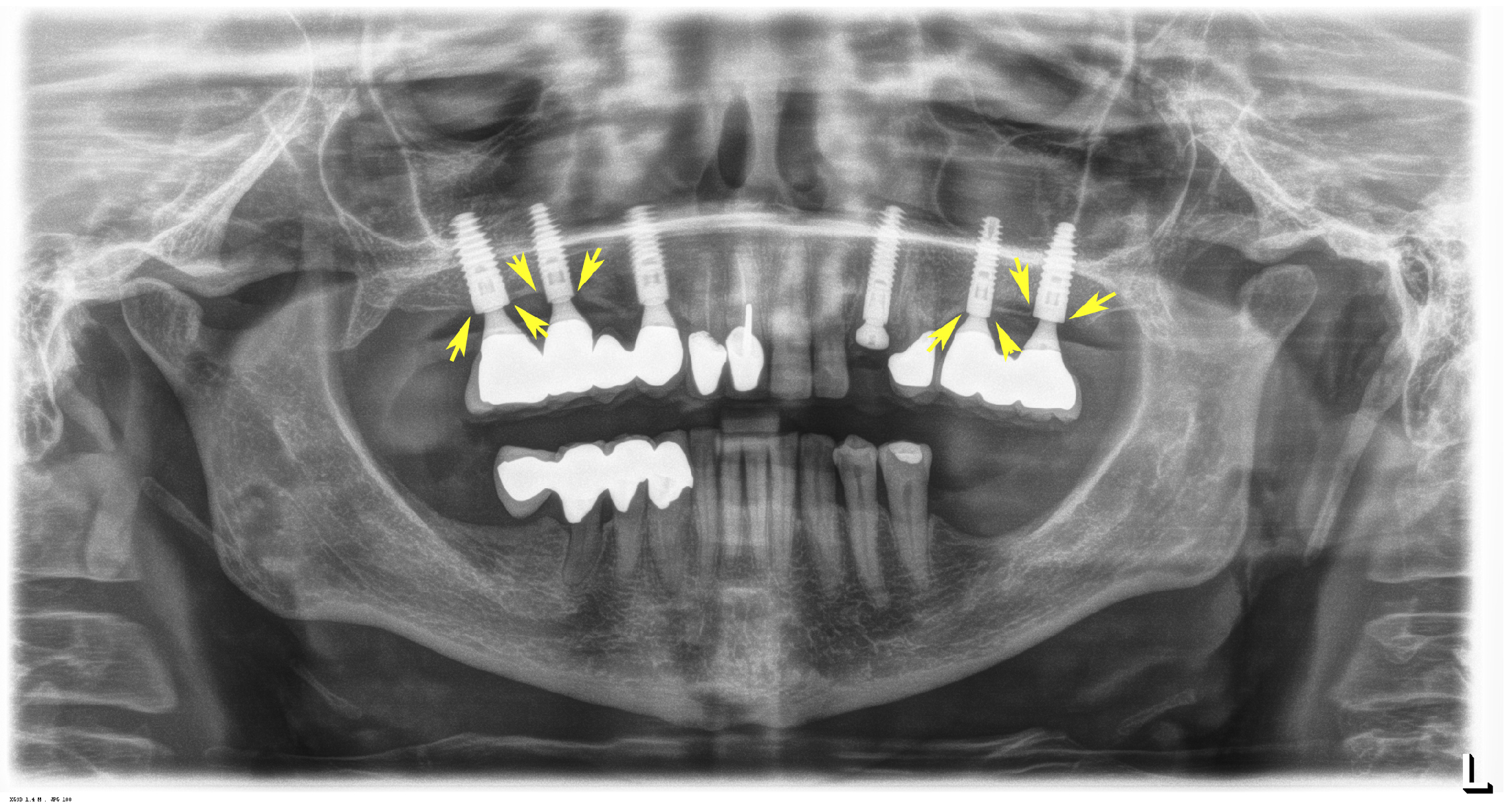
3.2. Radiological Results
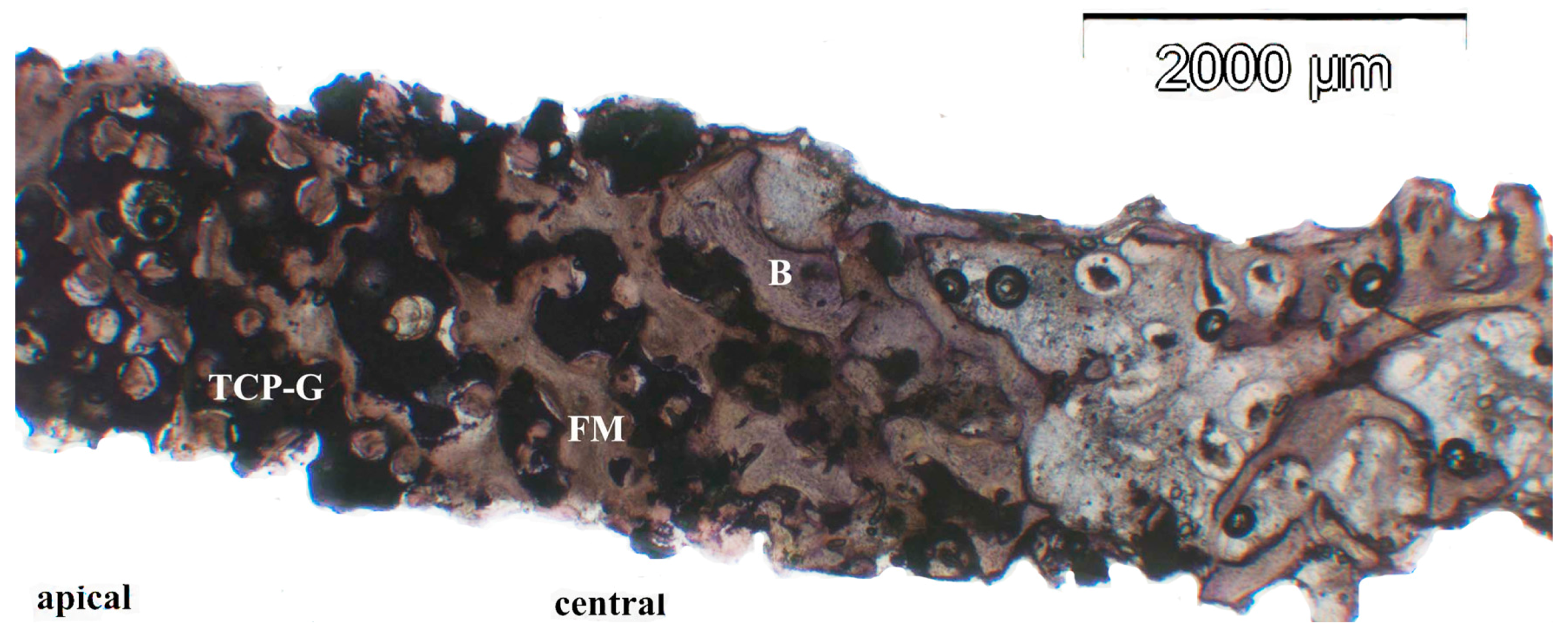
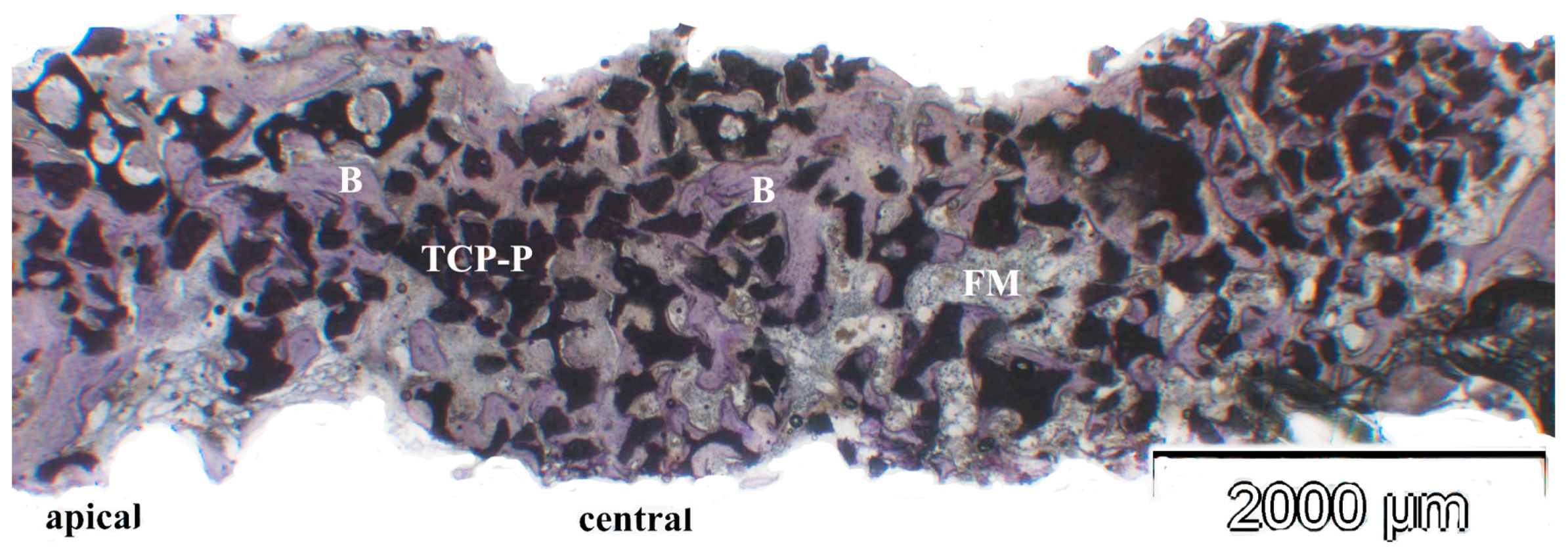
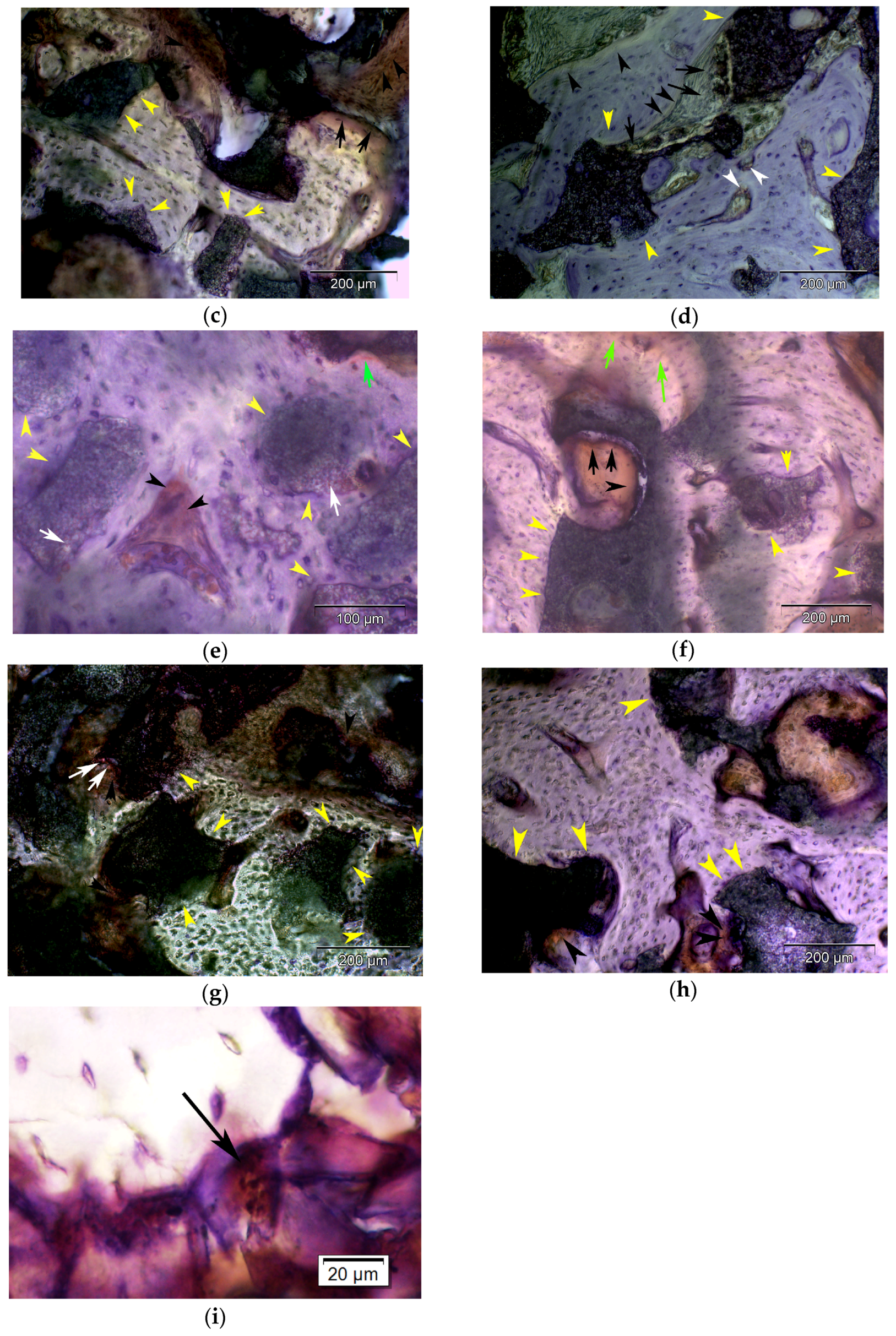
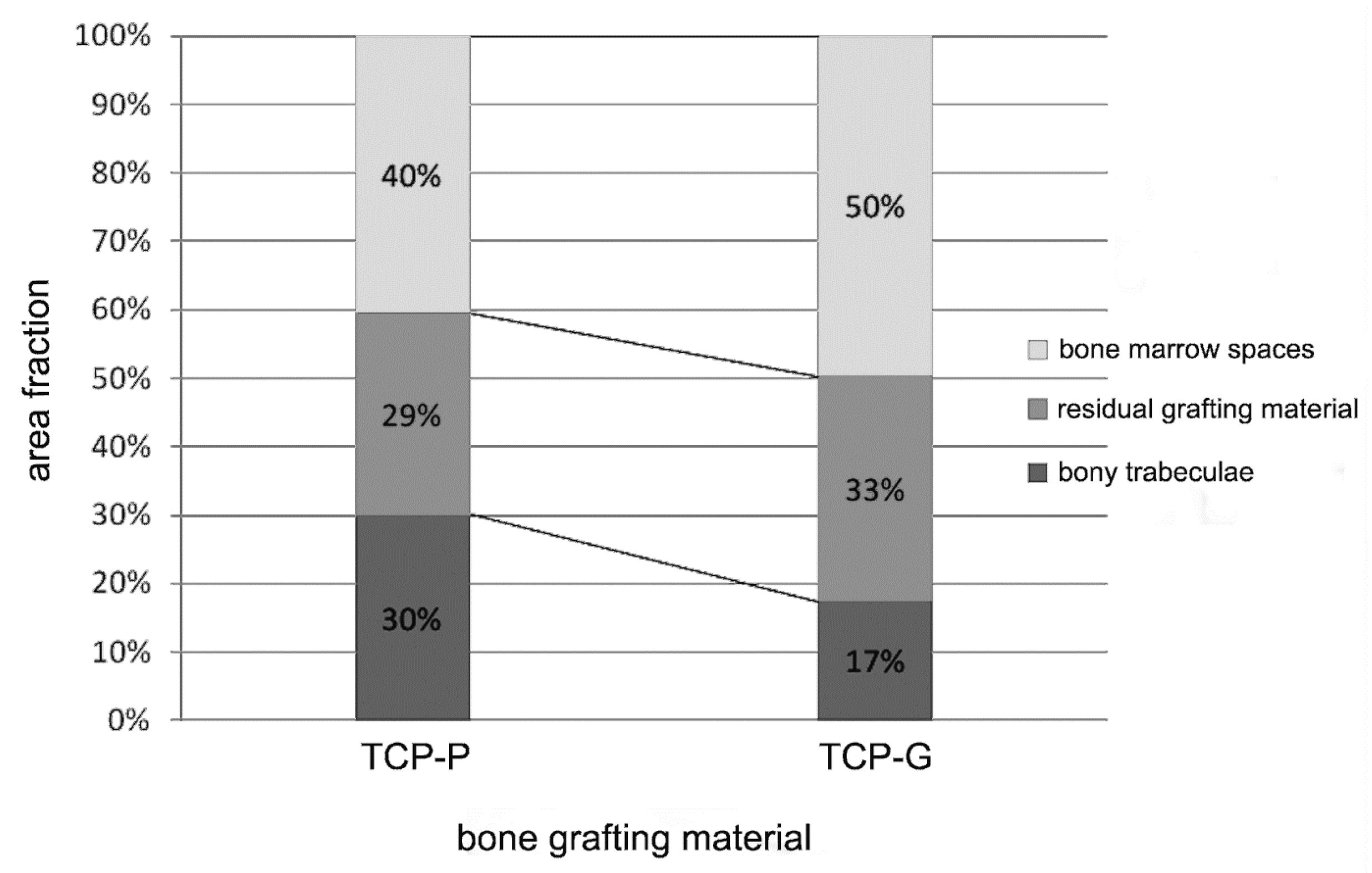
3.3. Results of Histologic, Histomorphometric and Immunohistochemical Analyses
3.4. Dental Implant Performance 6 Years after Placement
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of interest
Ethical Considerations
References
- Aghaloo, T.L.; Moy, P.K. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral Maxillofac. Implant. 2007, 22, 49–70. [Google Scholar]
- Knabe, C.; Koch, C.; Rack, A.; Stiller, M. Effect of beta-tricalcium phosphate particles with varying porosity on osteogenesis after sinus floor augmentation in humans. Biomaterials 2008, 29, 2249–2258. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J. Clin. Periodontol. 2008, 35, 216–240. [Google Scholar] [CrossRef] [PubMed]
- Kalk, W.W.; Raghoebar, G.M.; Jansma, J.; Boering, G. Morbidity from iliac crest bone harvesting. J. Oral Maxillofac. Surg. 1996, 54, 1424–1429. [Google Scholar] [CrossRef]
- Wheeler, S.L. Sinus augmentation for dental implants: The use of alloplastic materials. J. Oral Maxillofac. Surg. 1997, 55, 1287–1293. [Google Scholar] [CrossRef]
- Zijderveld, S.A.; Zerbo, I.R.; van den Bergh, J.P.; Schulten, E.A.; ten Bruggenkate, C.M. Maxillary sinus floor augmentation using a beta-tricalcium phosphate (Cerasorb) alone compared to autogenous bone grafts. Int. J. Oral Maxillofac. Implant. 2005, 20, 432–440. [Google Scholar]
- Bohner, M. Design of ceramic-based cements and putties for bone graft substitution. Eur. Cell. Mater. 2010, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Suba, Z.; Takacs, D.; Matusovits, D.; Barabas, J.; Fazekas, A.; Szabo, G. Maxillary sinus floor grafting with beta-tricalcium phosphate in humans: Density and microarchitecture of the newly formed bone. Clin. Oral Implants Res. 2006, 17, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Szabo, G.; Huys, L.; Coulthard, P.; Maiorana, C.; Garagiola, U.; Barabas, J.; Németh, Z.; Hrabák, K.; Suba, Z. A prospective multicenter randomized clinical trial of autogenous bone versus beta-tricalcium phosphate graft alone for bilateral sinus elevation: Histologic and histomorphometric evaluation. Int. J. Oral Maxillofac. Implant. 2005, 20, 371–381. [Google Scholar]
- Zerbo, I.R.; Bronckers, A.L.; de Lange, G.; Burger, E.H. Localisation of osteogenic and osteoclastic cells in porous beta-tricalcium phosphate particles used for human maxillary sinus floor elevation. Biomaterials 2005, 26, 1445–1451. [Google Scholar] [CrossRef] [PubMed]
- Zerbo, I.R.; Zijderveld, S.A.; de Boer, A.; Bronckers, A.L.; de Lange, G.; ten Bruggenkate, C.M.; Burger, E.H. Histomorphometry of human sinus floor augmentation using a porous beta-tricalcium phosphate: A prospective study. Clin. Oral Implants Res. 2004, 15, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Zijderveld, S.A.; Schulten, E.A.; Aartman, I.H.; ten Bruggenkate, C.M. Long-term changes in graft height after maxillary sinus floor elevation with different grafting materials: Radiographic evaluation with a minimum follow-up of 4.5 years. Clin. Oral Implants Res. 2009, 20, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Chazono, M.; Tanaka, T.; Komaki, H.; Fujii, K. Bone formation and bioresorption after implantation of injectable beta-tricalcium phosphate granules-hyaluronate complex in rabbit bone defects. J. Biomed. Mater. Res. A 2004, 70, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Stiller, M.; Rack, A.; Zabler, S.; Goebbels, J.; Dalugge, O.; Jonscher, S.; Knabe, C. Quantification of bone tissue regeneration employing beta-tricalcium phosphate by three-dimensional non-invasive synchrotron micro-tomography—A comparative examination with histomorphometry. Bone 2009, 44, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Peters, F.; Reif, D. Functional materials for bone regeneration from β-tricalcium phosphate. Materwiss. Werksttech. 2004, 35, 203–207. [Google Scholar] [CrossRef]
- Puppi, D.; Chiellini, F.; Piras, A.M.; Chiellini, E. Polymeric materials for bone and cartilage repair. Prog. Polym. Sci. 2010, 35, 403–440. [Google Scholar] [CrossRef]
- West, D.C.; Hampson, I.N.; Arnold, F.; Kumar, S. Angiogenesis induced by degradation products of hyaluronic acid. Science 1985, 228, 1324–1326. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.E.; Lussier, A.J.; Peyron, J.G. A risk-benefit assessment of injections of hyaluronan and its derivatives in the treatment of osteoarthritis of the knee. Drug Saf. 2000, 231, 15–30. [Google Scholar] [CrossRef]
- Liao, Y.H.; Jones, S.A.; Forbes, B.; Martin, G.P.; Brown, M.B. Hyaluronan: Pharmaceutical characterization and drug delivery. Drug Deliv. 2005, 12, 327–342. [Google Scholar] [CrossRef] [PubMed]
- Moreland, L.W. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: Mechanisms of action. Arthritis Res. Ther. 2003, 5, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Yamaguchi, M.; Sumitomo, S.; Takai, Y. Hyaluronan-based biomaterials in tissue engineering. Acta Histochem. Cytochem. 2004, 37, 1–5. [Google Scholar] [CrossRef]
- Smiler, D.G. The sinus lift graft: Basic technique and variantions. Pract. Periodont. Aesthet. Dent. 1997, 9, 885–893. [Google Scholar]
- Tatum, H.J. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [PubMed]
- Becker, S.T.; Terheyden, H.; Steinriede, A.; Behrens, E.; Springer, I.; Wiltfang, J. Prospective observation of 41 perforations of the Schneiderian membrane during sinus floor elevation. Clin. Oral Implant. Res. 2008, 19, 1285–1289. [Google Scholar] [CrossRef] [PubMed]
- Pommer, B.; Unger, E.; Suto, D.; Hack, N.; Watzek, G. Mechanical properties of the Schneiderian membrane in vitro. Clin. Oral Implant. Res. 2009, 20, 633–637. [Google Scholar]
- Waisbrod, H.; Gerbershagen, H.U. A pilot study of the value of ceramics for bone replacement. Arch. Orthop. Trauma Surg. 1986, 105, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Geret, V.; Mueller, W.; Tepic, M.; Rahn, B.A.; Perren, S.M. Comparison of calciumhydroxyapatite (Ceros 80) and beta-tricalciumphosphate (Ceros 82) in vivo with soft tissue interface. In Biomaterials and Clinical Applications; Pizzoferrato, A., Marchetti, P.G., Ravaglioli, A., Lee, A.J.C., Eds.; Elsevier: Amsterdam, The Netherlands, 1987; pp. 627–631. [Google Scholar]
- Eggli, P.S.; Mueller, W.; Schenk, R.K. The role of pore size on bone ingrowth and implant substitution in Hydroxylapatit and Tricalcium phosphat ceramics. A histologic and morphometric study in rabbits. In Biomaterials and Clinical Applications; Pizzoferrato, A., Marchetti, P.G., Ravaglioli, A., Lee, A.J.C., Eds.; Elsevier: Amsterdam, The Netherlands, 1987; pp. 53–56. [Google Scholar]
- Eggli, P.S.; Mueller, W.; Schenk, R.K. Porous hydroxyapatite and tricalciumphosphate cylinders with two different pore size ranges implanted in the cancellous bone of rabbits: A comparative histomorphometric and histologic study of bony ingrowth and implant substitution. Clin. Orthop. Relat. Res. 1988, 232, 127–138. [Google Scholar]
- Gatti, A.M.; Zaffe, D.; Poli, G.P. Behavior of tricalcium phosphate and hydroxyapatite granules in sheep bone defects. Biomaterials 1990, 11, 513–517. [Google Scholar] [CrossRef]
- Buser, D.; Hoffmann, B.; Bernard, J.P.; Lussi, A.; Mettler, D.; Schenk, R.K. Evaluation of filling materials in membrane protected bone defects. A comparative histomorphometric study in mandible of miniature pigs. Clin. Oral Implant. Res. 1998, 9, 137–150. [Google Scholar] [CrossRef]
- Lu, J.X.; Flautre, B.; Anselme, K.; Hardouin, P.; Gallur, A.; Descamps, M.; Thierry, B. Role of interconnections bioceramics on bone recolonization in vitro and in vivo. J. Mate. Sci. Mater. Med. 1999, 10, 111–120. [Google Scholar] [CrossRef]
- Lindenmüller, I.H.; Lambrecht, J.H. Sinusbodenelevation und Implantation—Eine Retrospektive Untersuchung. Schweiz. Monatsschr. Zahnmed. 2006, 2, 142–149. [Google Scholar]
- Njensen, S.S.; Broggini, N.; Hjorting-Hansen, E.; Schenk, R.; Buser, D. Bone healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clin. Oral Implant. Res. 2006, 17, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.; Maissen, O.; Ponomarev, I.; Stoll, T.; Rahn, B.; Wilke, I. Osteopromotion by a beta-tricalcium phosphate/bone marrow hybrid implant for use in spine surgery. Spine 2006, 31, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Walsh, W.R.; Vizesi, F.; Michael, D.; Auld, J.; Langdown, A.; Oliver, R.; Yu, Y.; Irie, H.; Bruce, W. Beta-TCP bone graft substitutes in a bilateral rabbit tibial defect model. Biomaterials 2008, 29, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Knabe, C.; Kraska, B.; Koch, C.; Gross, U.; Zreiqat, H.; Stiller, M. A method for immunohistochemical detection of osteogenic markers in undecalcified bone sections. Biotech. Histochem. 2006, 81, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Knabe, C.; Mele, A.; Kann, P.H.; Peleska, B.; Adel-Khattab, D.; Renz, H.; Reuss, A.; Bohner, M.; Stiller, M. Effect of sex-hormone levels, sex, body mass index and other host factors on human craniofacial bone regeneration with bioactive tricalcium phosphate grafts. Biomaterials 2017, 123, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Fisher, L.W.; Stubbs, J.T., 3rd; Young, M.F. Antisera and cDNA probes to human and certain animal model bone matrix noncollagenous proteins. Acta. Orthop. Scand. Suppl. 1995, 266, 61–65. [Google Scholar] [PubMed]
- Goldberg, A.F.; Barka, T. Acid phosphatase activity in human blood cells. Nature 1962, 195, 297. [Google Scholar] [CrossRef] [PubMed]
- Farhadieh, R.D.; Gianoutsos, M.P.; Yu, Y.; Walsh, W.R. The role of bone morphogenetic proteins BMP-2 and BMP-4 and their related postreceptor signaling system (Smads) in distraction osteogenesis of the mandible. J. Craniofac. Surg. 2004, 15, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, K.; Yu, Y.; Shahidi, S.; Bonar, F.; Walsh, W.R.; Poole, M.D. Expression of growth factors in the mandibular distraction zone: A sheep study. Br. J. Plast. Surg. 1999, 52, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Gerstenfeld, L.C.; Wronski, T.J.; Hollinger, J.O.; Einhorn, T.A. Application of histomorphometric methods to the study of bone repair. J. Bone Miner. Res. 2005, 20, 1715–1722. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, R.; Osborne, R.H.; Ebeling, P.R.; Wark, J.D.; Mitchell, P.; Wriedt, C.; Graves, S.; Staples, M.P.; Murphy, B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N. Engl. J. Med. 2009, 361, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.F.; De Giacomo, A.; Gerstenfeld, L.C. Overview of skeletal repair (fracture healing and its assessment). Methods Mol. Biol. 2014, 1130, 13–31. [Google Scholar] [PubMed]
- Cawood, J.I.; Stoelinga, P.J. International Research Group on Reconstructive Preprosthetic Surgery. Consensus report. Int. J. Oral Maxillofac. Surg. 2000, 29, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Cawood, J.I.; Stoelinga, P.J. International academy for oral and facial rehabilitation—Consensus Report. Int. J. Oral Maxillofac. Surg. 2006, 35, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Stoelinga, P.J.; Cawood, J.I. Report of the International Research Group on Reconstructive Preprosthetic Surgery: The history of the Consensus Conference on Reconstructive Preprosthetic Surgery. Int. J. Oral Maxillofac. Surg. 1996, 25, 81–84. [Google Scholar] [PubMed]
- Jung, J.; Yim, J.H.; Kwon, Y.D.; Al-Nawas, B.; Kim, G.T.; Choi, B.J.; Lee, D.W. A radiographic study of the position and prevalence of the maxillary arterial endosseous anastomosis using cone beam computed tomography. Int. J. Oral Maxillofac. Implant. 2011, 26, 1273–1278. [Google Scholar]
- Platzer, S.; Wildburger, A.; Lorenzoni, M.; Jakse, N.; Riedl, R.; Weiglein, A.; Wegscheider, W.; Kirmeier, R. Human cadaver study evaluating a new measurement technique for graft volumes after sinus floor elevation. Clin. Implant. Dent. Relat. Res. 2014, 16, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M. Resorbable biomaterials as bone graft substitutes. Mater. Today 2010, 13, 24–30. [Google Scholar] [CrossRef]
- Fraser, J.R.; Laurent, T.C.; Laurent, U.B. Hyaluronan: Its nature, distribution, functions and turnover. J. Intern. Med. 1997, 242, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lebel, L.; Fraser, J.R.; Kimpton, W.S.; Gabrielsson, J.; Gerdin, B.; Laurent, T.C. A pharmacokinetic model of intravenously administered hyaluronan in sheep. Pharm Res. 1989, 6, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Zhong, S.P.; Campoccia, D.; Doherty, P.J.; Williams, R.L.; Benedetti, L.; Williams, D.F. Biodegradation of hyaluronic acid derivatives by hyaluronidase. Biomaterials 1994, 15, 359–365. [Google Scholar] [CrossRef]
- Aslan, M.; Simsek, G.; Dayi, E. The effect of hyaluronic acid-supplemented bone graft in bone healing: Experimental study in rabbits. J. Biomater. Appl. 2006, 20, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Cheng, Y.Y.; Koo, P.L.; Lee, K.M.; Qin, L.; Cheng, J.C.; et al. The effect of hyaluronan on osteoblast proliferation and differentiation in rat calvarial-derived cell cultures. J. Biomed. Mater. Res. A. 2003, 66, 880–884. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Watanabe, C. Stimulation of osteoinduction in bone wound healing by high-molecular hyaluronic acid. Bone 1995, 16, 9–15. [Google Scholar] [CrossRef]
- Knabe, C.; Ducheyne, P.; Adel-Khattab, D.; Stiller, M. 7.20 Dental Graft Materials. In Comprehensive Biomaterials II; Ducheyne, P., Grainger, D.W., Healy, K.E., Hutmacher, D.W., Kirkpatrick, C.J., Eds.; Elsevier: Oxford, UK, 2017; Volume 7, pp. 378–405. [Google Scholar]



| Patient | Age (Years) | Gender | CEROS®-TCP-Putty | CEROS®-TCP-Granules |
|---|---|---|---|---|
| 1 | 57 | F* | Right | Left |
| 2 | 63 | F | Right | Left |
| 3 | 70 | F | Left | Right |
| 4 | 72 | F | Right | Left |
| 5 | 66 | M | Left | Right |
| 6 | 67 | M* | Left | Right |
| 7 | 63 | F | Right | Left |
| Col I | Osteoblast | Osteocyte | Fibroblast | Fibrous Matrix of the Osteogenic Mesenchym | Bone Matrix | Osteoid | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| apical | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G |
| Mean ± SD | 0.85 ± 1 | 0.14 ± 0.3 | 0.71 ± 1.4 | 0.14 ± 0.3 | 2 ± 1.1 | 1.71 ± 1.4 | 1.42 ± 1.2 | 2.1 ± 1.54 | 1 ± 1.5 | 0.4 ± 1.1 | 1 ± 1.1 | 0.2 ± 0.75 |
| p-value | 0.03 | 0.35 | 0.6 | 0.23 | 0.17 | 0.03 | ||||||
| central | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G |
| Mean ± SD | 1.8 ± 1.4 | 2.1 ± 1.5 | 1.4 ± 1.8 | 0.57 ± 0.5 | 1.8 ± 2 | 1 ± 1.4 | 3.2 ± 1.3 | 3 ± 0.8 | 1.2 ± 1.3 | 1.4 ± 1.5 | 1 ± 0.5 | 2.2 ± 1.6 |
| p-value | 0.64 | 0.63 | 0.15 | 0.36 | 0.95 | 0.03 | ||||||
| ALP apical | Osteoblast | Osteocyte | Fibroblast | Fibrous matrix | Bone matrix | Osteoid | ||||||
| TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | |
| Mean ± SD | 1.5 ± 1.7 | 0.7 ± 1.4 | 0.14 ± 1.3 | 0.14 ± 0.3 | 1.4 ± 1.5 | 1 ± 1.1 | 2.8 ± 0.9 | 2.7 ± 1.9 | 0.14 ± 0.3 | 0 ± 0 | 1 ± 1.4 | 0.42 ± 0.7 |
| p-value | 0.18 | 0.59 | 0.47 | 0.65 | 0.48 | 0.18 | ||||||
| central | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G |
| Mean ± SD | 2.28 ± 1.6 | 2.1 ± 1.7 | 1.28 ± 1.6 | 0.85 ± 1.4 | 2.4 ± 1.7 | 2.7 ± 1.7 | 3.14 ± 0.9 | 3.8 ± 0.9 | 0.7 ± 1.1 | 0.4 ± 0.7 | 1.5 ± 1.5 | 1 ± 0.8 |
| p-value | 0.9 | 0.25 | 0.71 | 0.06 | 0.47 | 0.4 | ||||||
| OC apical | Osteoblast | Osteocyte | Fibroblast | Fibrous matrix | Bone matrix | Osteoid | ||||||
| TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | |
| Mean ± SD | 0.85 ± 1.4 | 0.57 ± 1.5 | 0.28 ± 0.4 | 0 ± 0 | 1.57 ± 1.9 | 0.57 ± 1.5 | 2.28 ± 1.6 | 2.28 ± 1.6 | 0.14 ± 0.3 | 0 ± 0 | 1.28 ± 1.3 | 0.42 ± 1.1 |
| p-value | 0.64 | 0.09 | 0.2 | 0.87 | 0.48 | 0.04 | ||||||
| central | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G |
| Mean ± SD | 2 ± 1.6 | 1.28 ± 1.6 | 0.85 ± 1.46 | 0.14 ± 0.3 | 1.7 ± 1.7 | 1.28 ± 1.8 | 3 ± 1.1 | 2.7 ± 1.4 | 0.42 ± 0.5 | 0.3 ± 0.4 | 1.14 ± 1 | 1 ± 0.8 |
| p-value | 0.3 | 0.12 | 0.66 | 0.52 | 0.69 | 0.86 | ||||||
| BSP apical | Osteoblast | Osteocyte | Fibroblast | Fibrous matrix | Bone matrix | Osteoid | ||||||
| TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | |
| Mean ± SD | 1.42 ± 1.8 | 0.14 ± 0.3 | 0.57 ± 1.1 | 0 ± 0 | 0.57 ± 1.1 | 0.42 ± 1.1 | 1.28 ± 1.6 | 1.28 ± 1.1 | 0 ± 0 | 0 ± 0 | 0.42 ± 0.7 | 0.28 ± 0.4 |
| p-value | 0.03 | 0.09 | 0.64 | 0.72 | 0.99 | 0.8 | ||||||
| Central | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G | TCP-P | TCP-G |
| Mean ± SD | 2.28 ± 1.7 | 0.85 ± 1 | 1.14 ± 1.3 | 0.14 ± 0.3 | 0.57 ± 1.1 | 1 ± 1 | 1.57 ± 1.7 | 2.7 ± 1.25 | 0.57 ± 0.5 | 0.3 ± 0.4 | 1.14 ± 1 | 1.2 ± 1.3 |
| p-value | 0.02 | 0.018 | 0.08 | 0.06 | 0.25 | 0.93 | ||||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knabe, C.; Khattab, D.A.; Kluk, E.; Struck, R.; Stiller, M. Effect of a Particulate and a Putty-Like Tricalcium Phosphate-Based Bone-grafting Material on Bone Formation, Volume Stability and Osteogenic Marker Expression after Bilateral Sinus Floor Augmentation in Humans. J. Funct. Biomater. 2017, 8, 31. https://doi.org/10.3390/jfb8030031
Knabe C, Khattab DA, Kluk E, Struck R, Stiller M. Effect of a Particulate and a Putty-Like Tricalcium Phosphate-Based Bone-grafting Material on Bone Formation, Volume Stability and Osteogenic Marker Expression after Bilateral Sinus Floor Augmentation in Humans. Journal of Functional Biomaterials. 2017; 8(3):31. https://doi.org/10.3390/jfb8030031
Chicago/Turabian StyleKnabe, Christine, Doaa Adel Khattab, Esther Kluk, Rainer Struck, and Michael Stiller. 2017. "Effect of a Particulate and a Putty-Like Tricalcium Phosphate-Based Bone-grafting Material on Bone Formation, Volume Stability and Osteogenic Marker Expression after Bilateral Sinus Floor Augmentation in Humans" Journal of Functional Biomaterials 8, no. 3: 31. https://doi.org/10.3390/jfb8030031




