A Novel Impedance Biosensor for Measurement of Trans-Epithelial Resistance in Cells Cultured on Nanofiber Scaffolds
Abstract
:1. Introduction
2. Materials and Methods
2.1. Nanoscaffold Transwell Assembly
2.2. SIMS Cell Studies
2.3. ECIS-TEER Measurement
2.4. Immunocytochemistry Staining and Quantification
3. Results and Discussion
3.1. Transwell Nanofiber Membrane Integration
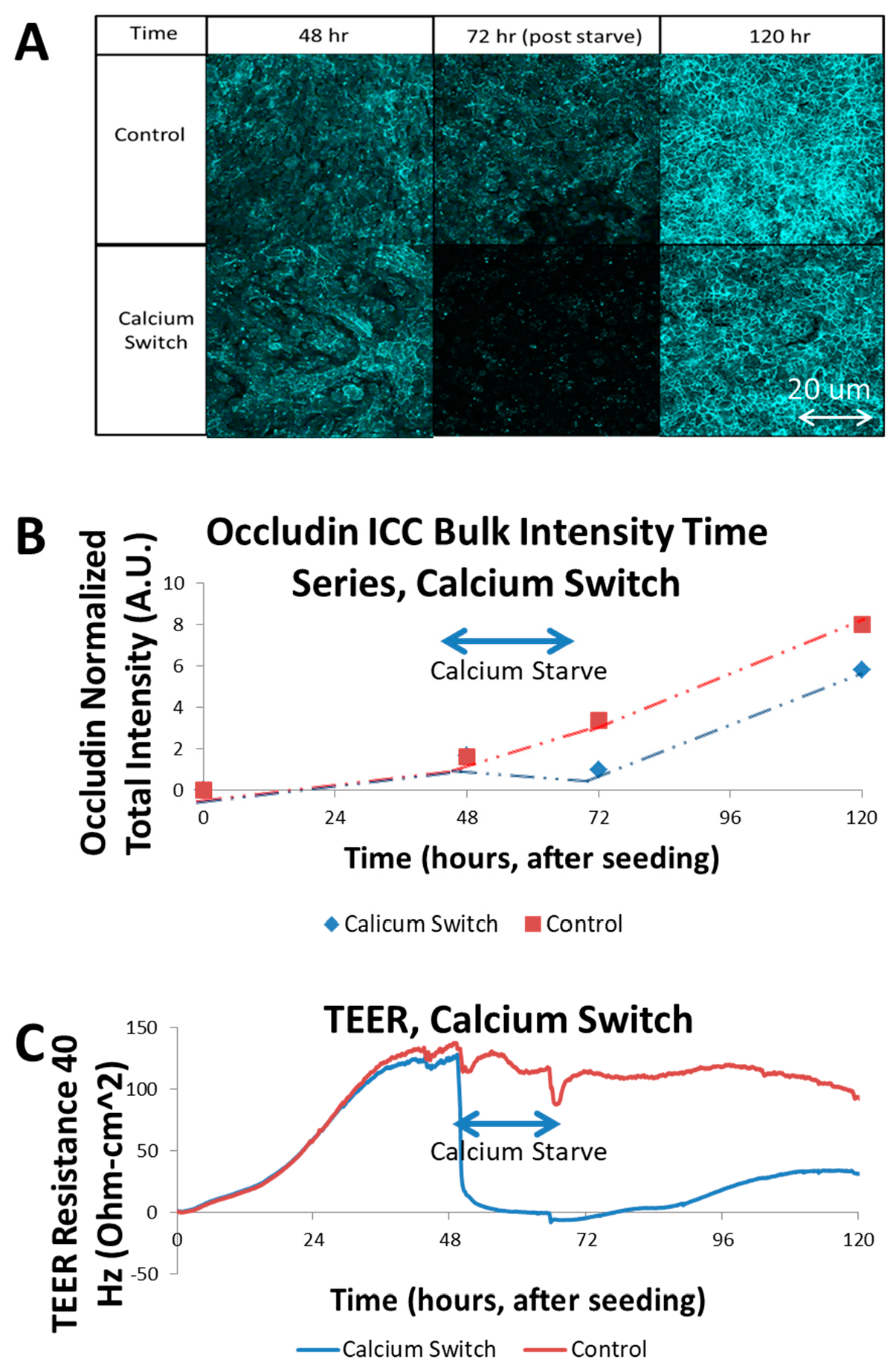
3.2. Calcium Switch of SIMS Cells and Effect on TEER
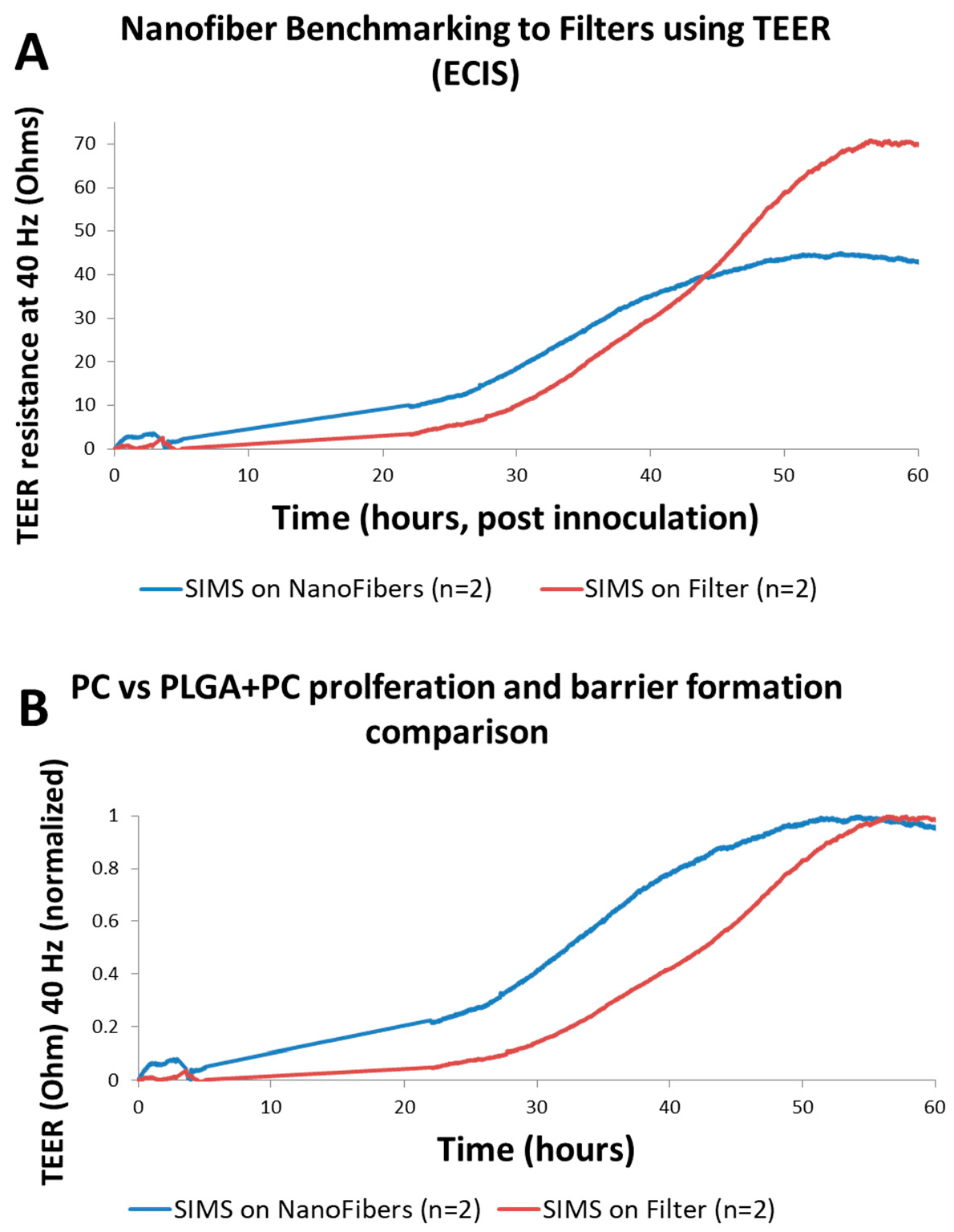
3.3. TEER Measurements on Engineered Nanofiber Scaffold
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Giaever, I.; Keese, C.R. Micromotion of mammalian cells measured electrically. Proc. Natl. Acad. Sci. USA 1991, 88, 7896–7900. [Google Scholar] [CrossRef] [PubMed]
- Freed, L.E.; Vunjak-Novakovic, G.; Biron, R.J.; Eagles, D.B.; Lesnoy, D.C.; Barlow, S.K.; Langer, R. Biodegradable polymer scaffolds for tissue engineering. Biotechnology 1994, 12, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Torrejon, K.Y.; Papke, E.L.; Halman, J.R.; Stolwijk, J.; Dautriche, C.N.; Bergkvist, M.; Danias, J.; Sharfstein, S.T.; Xie, Y. Bioengineered glaucomatous 3D human trabecular meshwork as an in vitro disease model. Biotechnol. Bioeng. 2016, 113, 1357–1368. [Google Scholar] [CrossRef] [PubMed]
- Soscia, D.; Sequeira, S.J.; Schramm, R.; Jayarathanam, K.; Cantara, S.I.; Larsen, M.; Castracane, J. Salivary gland cell differentiation and organization on micropatterned PLGA nanofiber craters. Biomaterials 2013, 34, 6773–6784. [Google Scholar] [CrossRef] [PubMed]
- Larsen, M.; Jean-Gilles, R.; Soscia, D.; Sequeira, S.; Melfi, M.; Gadre, A.; Castracane, J. Development of Nanofiber Scaffolds for Engineering an Artificial Salivary Gland. In Proceedings of the ASME. Global Congress on NanoEngineering for Medicine and Biology, ASME 2010 First Global Congress on NanoEngineering for Medicine and Biology, Houston, TX, USA, 7–10 February 2010; pp. 185–186. [Google Scholar]
- Cantara, S.I.; Soscia, D.; Sequeira, S.J.; Jean-Gilles, R.P.; Castracane, J.; Larsen, M. Selective functionalization of nanofiber scaffolds to regulate salivary gland epithelial cell proliferation and polarity. Biomaterials 2012, 33, 8372–8382. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.; Hussain, M.; Mao, J.J. Continuing differentiation of human mesenchymal stem cells and induced chondrogenic and osteogenic lineages in electrospun PLGA nanofiber scaffold. Biomaterials 2007, 28, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Sequeira, S.J.; Soscia, D.A.; Oztan, B.; Mosier, A.P.; Jean-Gilles, R.; Gadre, A.; Larsen, M. The regulation of focal adhesion complex formation and salivary gland epithelial cell organization by nanofibrous PLGA scaffolds. Biomaterials 2012, 33, 3175–3186. [Google Scholar] [CrossRef] [PubMed]
- Sfakis, L.; Sharikova, A.; Tuschel, D.; Costa, F.X.; Larsen, M.; Khmaladze, A.; Castracane, J. Core/shell nanofiber characterization by Raman scanning microscopy. Biomed. Opt. Express 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Laoide, B.M.; Courty, Y.; Gastinne, I.; Thibaut, C.; Kellermann, O.; Rougeon, F. Immortalised mouse submandibular epithelial cell lines retain polarised structural and functional properties. J. Cell Sci. 1996, 109, 2789–2800. [Google Scholar] [PubMed]
- Lo, C.M.; Keese, C.R.; Giaever, I. Cell-substrate contact: Another factor may influence transepithelial electrical resistance of cell layers cultured on permeable filters. Exp. Cell Res. 1999, 250, 576–580. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.I.; Dodelet-devillers, A.; Kebir, H.; Ifergan, I.; Fabre, P.J.; Terouz, S.; Sabbagh, M.; Wosik, K.; Bourbonnière, L.; Bernard, M.; et al. The Hedgehog Pathway Promotes Blood-Brain Barrier Integrity and CNS Immune Quiescence. Science 2011, 334, 1727–1731. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schramm, R.A.; Koslow, M.H.; Nelson, D.A.; Larsen, M.; Castracane, J. A Novel Impedance Biosensor for Measurement of Trans-Epithelial Resistance in Cells Cultured on Nanofiber Scaffolds. Biosensors 2017, 7, 35. https://doi.org/10.3390/bios7030035
Schramm RA, Koslow MH, Nelson DA, Larsen M, Castracane J. A Novel Impedance Biosensor for Measurement of Trans-Epithelial Resistance in Cells Cultured on Nanofiber Scaffolds. Biosensors. 2017; 7(3):35. https://doi.org/10.3390/bios7030035
Chicago/Turabian StyleSchramm, Robert A., Matthew H. Koslow, Deirdre A. Nelson, Melinda Larsen, and James Castracane. 2017. "A Novel Impedance Biosensor for Measurement of Trans-Epithelial Resistance in Cells Cultured on Nanofiber Scaffolds" Biosensors 7, no. 3: 35. https://doi.org/10.3390/bios7030035




