Adhesion of Diarrheagenic Escherichia coli and Inhibition by Glycocompounds Engaged in the Mucosal Innate Immunity
Abstract
:1. The Discovery of Diarrheagenic Categories of Escherichia coli
| Pathotype | Histopathological feature | Major adhesion factors | Host cell receptor (adhesin) | Preferential gut site | Reference |
|---|---|---|---|---|---|
| Enterotoxigenic E. coli (ETEC) | Colonization factor antigens (CFA I, II and IV) | Sialoglycoprotein (CFA/I) Asialo ganglioside GM1 (CFA/II) Glycosphingolipid sulphatide (CFA/IV) | - Jejunal and duodenal mucosa | [16] | |
| Enteropathogenic E. coli (EPEC) | - Localized adherence - Attachment-and-effacement lesion | Intimin α Bundle-forming pilus | β1-integrins (intimin α) | - Proximal and distal small intestine - Follicle associated epithelium of ileal Peyer’s patches | [17,18,19] |
| Enterohemorrhagic E. coli (EHEC) | - Attachment-and-effacement lesion | Intimin γ Long polar fimbriae (LPF) | β1-integrins (intimin γ) Fibronectin, laminin and collagen IV (LPF) | - Follicle associated epithelium of ileal Peyer’s patches | [17,18,19,20] |
| Enteroaggregative E. coli (EAEC) | - Aggregative adherence - Vesiculation of colonic microvilli | Aggregative adherence fimbriae (AAF-I to IV) | Glycoproteins (AAF-II): - thrombospondin-1—TSP1. - fibronectin - epidermal growth factor receptor—EGFR - endoplasmin—GRP-94/Gp96 | - Ileal and colonic mucosa avoiding intestinal crypts | [21,22] |
| Diffusely adhering E. coli (DAEC) | - Diffuse adherence - Elongation of microvilli | Afa/Dr adhesins (AfaE alleles and F1845) | Glycosylphosphatidylinositol-anchored protein DAF (AfaE-I to IV and F1845) CEA-related cell adhesion molecule (AfaE-III and F1854) | [23,24,25] |
2. Diarrheagenic Categories of E. coli Exploit Different Adhesins
2.1. Adhesins of Enterotoxigenic Escherichia coli
| Biotype | Coli surface antigen | Colonization factor antigen | Morphology | Receptor | Reference |
|---|---|---|---|---|---|
| CFA/I | CfaB | CFA/I | Fimbrial | Sialoglycoprotein Nonacid glycosphingolipids | [34,35,36] |
| CFA/II | CS1 | CS1 | Fimbrial | Asialo ganglioside GM1 | [37,38] |
| CFA/II | CS2 | CS2 | Fimbrial | Asialo ganglioside GM1 | [31,38] |
| CFA/II | CS3 | CS3 | Fibrillar | Asialo ganglioside GM1 | [37,38] |
| CFA/III | CS8 | CFA/III | Fimbrial | [16] | |
| CFA/IV | CS4 | CS4 | Fimbrial | Asialo ganglioside GM1 | [16,38] |
| CFA/IV | CS5 | CS5 | Fimbrial (double-helical fibrils) | [16] | |
| CFA/IV | CS6 | CS6 | Fibrillar, fimbrial or nonfimbrial | Fibronectin Glycosphingolipid sulphatide | [16,39,40] |
2.2. Adhesins in A/E Lesion-Inducing E. coli Pathotypes
2.3. Adhesins in Enteroaggregative E. coli
2.4. Adhesins in Diffusely Adhering E. coli
3. Impairing Virulence by Targeting E. coli Adhesins
| Innate immune factor | Target E. coli pathotype | Inhibited adhesion/colonization processes | Interactions with adhesins | Reference |
|---|---|---|---|---|
| Lactoferrin | ETEC | - Inhibition of CFA-I-mediated hemagglutination - Inhibition of the ETEC adherence to epithelial cells - Inhibition of the gut colonization | - Binds to the CFA-I but do not to CFA-II | [82,85,90] |
| EPEC | - Inhibition of EPEC adhesion to epithelial cells - Inhibition of the A/E lesion - Inhibition of EPEC-induced hemolysis | - Binds to EspA and EspB promoting proteolytic degradation | [86,87,88,91] | |
| EHEC | - Inhibition of the gut colonization and of the spreading toward the kidney (mouse infection model) | [92] | ||
| EAEC | - Inhibition of EAEC adhesion to epithelial cells - Inhibition of biofilm formation | - Promotes release of AAF-II and its degradation | [89,93] | |
| DAEC | - Inhibition of adhesion to epithelial cells displayed by DAEC harboring F1845 | [89] | ||
| Secretory component | ETEC | - Inhibition of CFA-I-mediated hemagglutination | - Binds to the CFA-I and CFA-II | [82,85] |
| EPEC | - Inhibition of EPEC adhesion to epithelial cells - Inhibition of the A/E lesion | - Binds to intimin α | [86,94] | |
| Sialyl (acid)-oligosaccharide | ETEC | - Inhibition of CFA-I- and CFA-II-mediated hemagglutination | [88] | |
| EPEC | - Inhibition of EPEC adhesion to Caco-2 cells | [84] | ||
| Neutral oligosaccharide | EPEC | - Inhibition of EPEC adhesion to Caco-2 cells | [84] |
3.1. Inhibition of Diarrheagenic E. coli by Lactoferrin
3.2. Inhibition of E. coli Adhesion by Free Secretory Component (FSC)
3.3. Inhibition of E. coli Adhesion by Human Milk Oligosaccharides
4. Conclusions
Conflict of Interest
Acknowledgements
References
- Kaper, J.B.; Nataro, J.P.; Mobley, H.L. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2004, 2, 123–140. [Google Scholar] [CrossRef]
- Sekirov, I.; Russell, S.L.; Antunes, L.C.; Finlay, B.B. Gut microbiota in health and disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef]
- Fanaro, S.; Chierici, R.; Guerrini, P.; Vigi, V. Intestinal microflora in early infancy: Composition and development. Acta Paediatr. Suppl. 2003, 91, 48–55. [Google Scholar]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef] [Green Version]
- Nataro, J.P.; Kaper, J.B. Diarrheagenic Escherichia coli. Clin. Microbiol. Rev. 1998, 11, 142–201. [Google Scholar]
- Orskov, F. On the occurrence of E. coli belonging to O-group 26 in cases of infantile diarrhoea and white scours. Acta Pathol. Microbiol. Scand. 1951, 29, 373–378. [Google Scholar] [CrossRef]
- Ewing, W.H.; Tanner, K.E.; Tatum, H.W. A new serotype of Escherichia coli associated with infantile diarrhea. Public Health Rep. 1955, 70, 107–114. [Google Scholar] [CrossRef]
- Evans, D.G.; Silver, R.P.; Evans, D.J., Jr.; Chase, D.G.; Gorbach, S.L. Plasmid-controlled colonization factor associated with virulence in Esherichia coli enterotoxigenic for humans. Infect. Immun. 1975, 12, 656–667. [Google Scholar]
- Evans, D.G.; Evans, D.J., Jr. New surface-associated heat-labile colonization factor antigen (CFA/II) produced by enterotoxigenic Esherichia coli of serogroups O6 and O8. Infect. Immun. 1978, 21, 638–647. [Google Scholar]
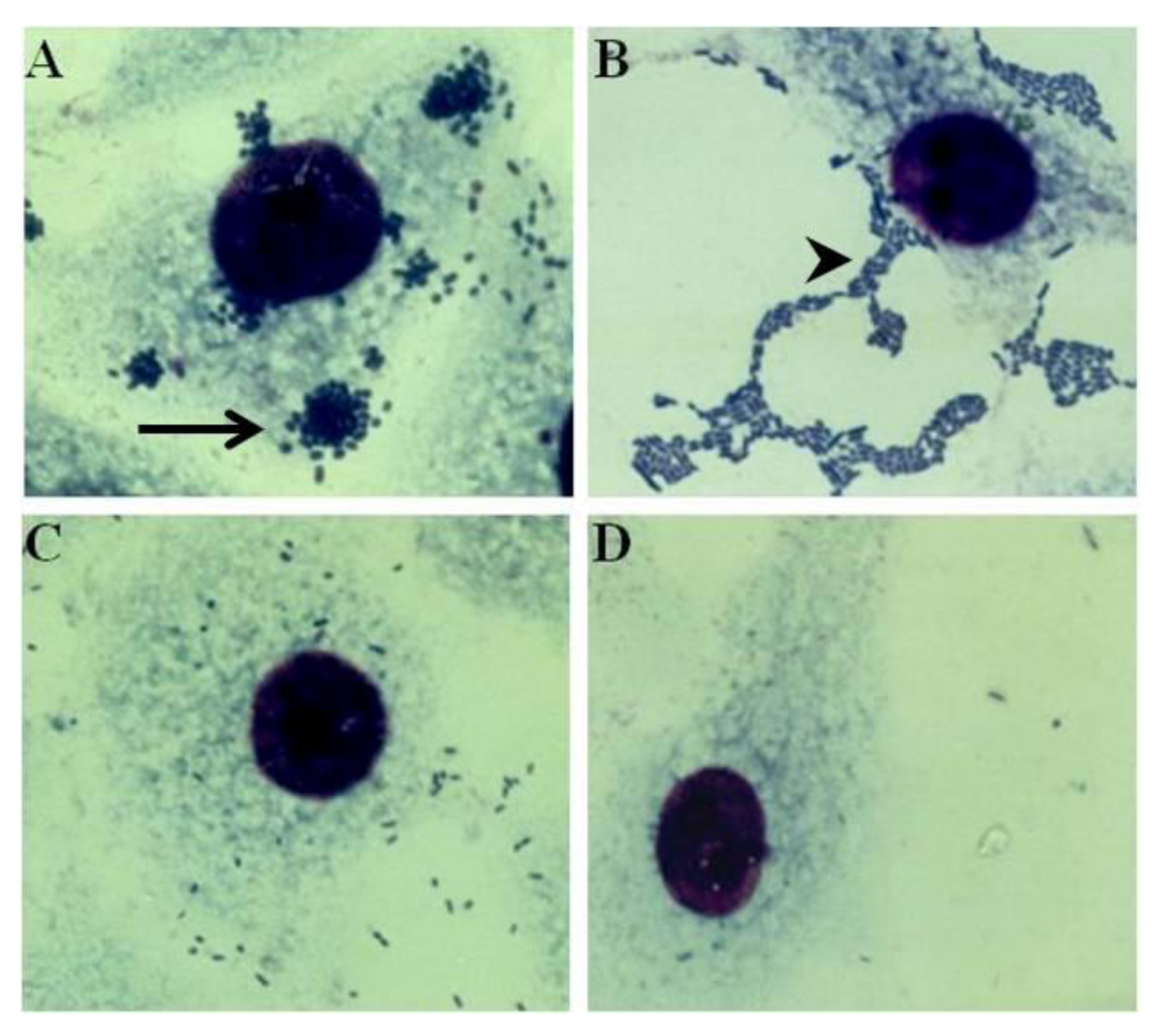
- Scaletsky, I.C.; Silva, M.L.; Trabulsi, L.R. Distinctive patterns of adherence of enteropathogenic Esherichia coli to HeLa cells. Infect. Immun. 1984, 45, 534–536. [Google Scholar]
- Nataro, J.P.; Scaletsky, I.C.; Kaper, J.B.; Levine, M.M.; Trabulsi, L.R. Plasmid-mediated factors conferring diffuse and localized adherence of enteropathogenic Esherichia coli. Infect. Immun. 1985, 48, 378–383. [Google Scholar]
- Giron, J.A.; Ho, A.S.; Schoolnik, G.K. An inducible bundle-forming pilus of enteropathogenic Esherichia coli. Science 1991, 254, 710–713. [Google Scholar]
- Giron, J.A.; Ho, A.S.; Schoolnik, G.K. Characterization of fimbriae produced by enteropathogenic Esherichia coli. J. Bacteriol. 1993, 175, 7391–7403. [Google Scholar]
- Nataro, J.P.; Deng, Y.; Maneval, D.R.; German, A.L.; Martin, W.C.; Levine, M.M. Aggregative adherence fimbriae I of enteroaggregative Esherichia coli mediate adherence to HEp-2 cells and hemagglutination of human erythrocytes. Infect. Immun. 1992, 60, 2297–2304. [Google Scholar]
- Bilge, S.S.; Clausen, C.R.; Lau, W.; Moseley, S.L. Molecular characterization of a fimbrial adhesin, F1845, mediating diffuse adherence of diarrhea-associated Esherichia coli to HEp-2 cells. J. Bacteriol. 1989, 171, 4281–4289. [Google Scholar]
- Knutton, S.; McConnell, M.M.; Rowe, B.; McNeish, A.S. Adhesion and ultrastructural properties of human enterotoxigenic Esherichia coli producing colonization factor antigens III and IV. Infect. Immun. 1989, 57, 3364–3371. [Google Scholar]
- Fitzhenry, R.J.; Pickard, D.J.; Hartland, E.L.; Reece, S.; Dougan, G.; Phillips, A.D.; Frankel, G. Intimin type influences the site of human intestinal mucosal colonisation by enterohaemorrhagic Esherichia coli O157:H7. Gut 2002, 50, 180–185. [Google Scholar] [CrossRef]
- Phillips, A.D.; Frankel, G. Intimin-mediated tissue specificity in enteropathogenic Esherichia coli interaction with human intestinal organ cultures. J. Infect. Dis. 2000, 181, 1496–1500. [Google Scholar] [CrossRef]
- Frankel, G.; Lider, O.; Hershkoviz, R.; Mould, A.P.; Kachalsky, S.G.; Candy, D.C.; Cahalon, L.; Humphries, M.J.; Dougan, G. The cell-binding domain of intimin from enteropathogenic Esherichia coli binds to beta1 integrins. J. Biol. Chem. 1996, 271, 20359–20364. [Google Scholar] [CrossRef]
- Farfan, M.J.; Cantero, L.; Vidal, R.; Botkin, D.J.; Torres, A.G. Long polar fimbriae of enterohemorrhagic Esherichia coli O157:H7 bind to extracellular matrix proteins. Infect. Immun. 2011, 79, 3744–3750. [Google Scholar] [CrossRef]
- Hicks, S.; Candy, D.C.; Phillips, A.D. Adhesion of enteroaggregative Esherichia coli to pediatric intestinal mucosa in vitro. Infect. Immun. 1996, 64, 4751–4760. [Google Scholar]
- Knutton, S.; Shaw, R.K.; Bhan, M.K.; Smith, H.R.; McConnell, M.M.; Cheasty, T.; Williams, P.H.; Baldwin, T.J. Ability of enteroaggregative Esherichia coli strains to adhere in vitro to human intestinal mucosa. Infect. Immun. 1992, 60, 2083–2091. [Google Scholar]
- Le, B.C.; Servin, A.L. Diffusely adherent Esherichia coli strains expressing Afa/Dr adhesins (Afa/Dr DAEC): hitherto unrecognized pathogens. FEMS Microbiol. Lett. 2006, 256, 185–194. [Google Scholar] [CrossRef]
- Peiffer, I.; Servin, A.L.; Bernet-Camard, M.F. Piracy of decay-accelerating factor (CD55) signal transduction by the diffusely adhering strain Esherichia coli C1845 promotes cytoskeletal F-actin rearrangements in cultured human intestinal INT407 cells. Infect. Immun. 1998, 66, 4036–4042. [Google Scholar]
- Bernet-Camard, M.F.; Coconnier, M.H.; Hudault, S.; Servin, A.L. Pathogenicity of the diffusely adhering strain Esherichia coli C1845: F1845 adhesin-decay accelerating factor interaction, brush border microvillus injury, and actin disassembly in cultured human intestinal epithelial cells. Infect. Immun. 1996, 64, 1918–1928. [Google Scholar]
- Lan, R.; Alles, M.C.; Donohoe, K.; Martinez, M.B.; Reeves, P.R. Molecular evolutionary relationships of enteroinvasive Esherichia coli and Shigella spp. Infect. Immun. 2004, 72, 5080–5088. [Google Scholar] [CrossRef]
- Parsot, C. Shigella spp. and enteroinvasive Esherichia coli pathogenicity factors. FEMS Microbiol. Lett. 2005, 252, 11–18. [Google Scholar] [CrossRef]
- Sansonetti, P. Host-pathogen interactions: The seduction of molecular cross talk. Gut 2002, 50, III2–III8. [Google Scholar] [CrossRef]
- Sansonetti, P.J. Rupture, invasion and inflammatory destruction of the intestinal barrier by Shigella, making sense of prokaryote-eukaryote cross-talks. FEMS Microbiol. Rev. 2001, 25, 3–14. [Google Scholar]
- Sansonetti, P.J.; D’Hauteville, H.; Ecobichon, C.; Pourcel, C. Molecular comparison of virulence plasmids in Shigella and enteroinvasive Esherichia coli. Ann. Microbiol. (Paris) 1983, 134A, 295–318. [Google Scholar]
- Honda, T.; Cakir, N.; Arita, M.; Miwatani, T. Purification and characterization of the CS2 pili of colonization factor antigen II produced by human enterotoxigenic Esherichia coli. Microbiol. Immunol. 1989, 33, 265–275. [Google Scholar]
- Isidean, S.D.; Riddle, M.S.; Savarino, S.J.; Porter, C.K. A systematic review of ETEC epidemiology focusing on colonization factor and toxin expression. Vaccine 2011, 29, 6167–6178. [Google Scholar]
- Wolf, M.K. Occurrence, distribution, and associations of O and H serogroups, colonization factor antigens, and toxins of enterotoxigenic Esherichia coli. Clin. Microbiol. Rev. 1997, 10, 569–584. [Google Scholar]
- Mu, X.Q.; Savarino, S.J.; Bullitt, E. The three-dimensional structure of CFA/I adhesion pili: Traveler’s diarrhea bacteria hang on by a spring. J. Mol. Biol. 2008, 376, 614–620. [Google Scholar] [CrossRef]
- Pieroni, P.; Worobec, E.A.; Paranchych, W.; Armstrong, G.D. Identification of a human erythrocyte receptor for colonization factor antigen I pili expressed by H10407 enterotoxigenic Esherichia coli. Infect. Immun. 1988, 56, 1334–1340. [Google Scholar]
- Jansson, L.; Tobias, J.; Lebens, M.; Svennerholm, A.M.; Teneberg, S. The major subunit, CfaB, of colonization factor antigen i from enterotoxigenic Esherichia coli is a glycosphingolipid binding protein. Infect. Immun. 2006, 74, 3488–3497. [Google Scholar] [CrossRef]
- Levine, M.M.; Ristaino, P.; Sack, R.B.; Kaper, J.B.; Orskov, F.; Orskov, I. Colonization factor antigens I and II and type 1 somatic pili in enterotoxigenic Esherichia coli: Relation to enterotoxin type. Infect. Immun. 1983, 39, 889–897. [Google Scholar]
- Oro, H.S.; Kolsto, A.B.; Wenneras, C.; Svennerholm, A.M. Identification of asialo GM1 as a binding structure for Esherichia coli colonization factor antigens. FEMS Microbiol. Lett. 1990, 60, 289–292. [Google Scholar]
- Roy, S.P.; Rahman, M.M.; Yu, X.D.; Tuittila, M.; Knight, S.D.; Zavialov, A.V. Crystal structure of enterotoxigenic Esherichia coli colonization factor CS6 reveals a novel type of functional assembly. Mol. Microbiol. 2012, 86, 1100–1115. [Google Scholar]
- Jansson, L.; Tobias, J.; Jarefjall, C.; Lebens, M.; Svennerholm, A.M.; Teneberg, S. Sulfatide recognition by colonization factor antigen CS6 from enterotoxigenic Esherichia coli. PLoS One 2009, 4, e4487. [Google Scholar]
- Li, Y.F.; Poole, S.; Nishio, K.; Jang, K.; Rasulova, F.; McVeigh, A.; Savarino, S.J.; Xia, D.; Bullitt, E. Structure of CFA/I fimbriae from enterotoxigenic Esherichia coli. Proc. Natl. Acad. Sci. USA 2009, 106, 10793–10798. [Google Scholar] [CrossRef]
- Thomas, L.V.; McConnell, M.M.; Rowe, B.; Field, A.M. The possession of three novel coli surface antigens by enterotoxigenic Esherichia coli strains positive for the putative colonization factor PCF8775. J. Gen. Microbiol. 1985, 131, 2319–2326. [Google Scholar]
- Wolf, M.K.; de Haan, L.A.; Cassels, F.J.; Willshaw, G.A.; Warren, R.; Boedeker, E.C.; Gaastra, W. The CS6 colonization factor of human enterotoxigenic Esherichia coli contains two heterologous major subunits. FEMS Microbiol. Lett. 1997, 148, 35–42. [Google Scholar] [CrossRef]
- Ghosal, A.; Bhowmick, R.; Banerjee, R.; Ganguly, S.; Yamasaki, S.; Ramamurthy, T.; Hamabata, T.; Chatterjee, N.S. Characterization and studies of the cellular interaction of native colonization factor CS6 purified from a clinical isolate of enterotoxigenic Esherichia coli. Infect. Immun. 2009, 77, 2125–2135. [Google Scholar] [CrossRef]
- Tobias, J.; Lebens, M.; Kallgard, S.; Nicklasson, M.; Svennerholm, A.M. Role of different genes in the CS6 operon for surface expression of Enterotoxigenic Esherichia coli colonization factor CS6. Vaccine 2008, 26, 5373–5380. [Google Scholar] [CrossRef]
- Tobe, T.; Sasakawa, C. Role of bundle-forming pilus of enteropathogenic Esherichia coli in host cell adherence and in microcolony development. Cell Microbiol. 2001, 3, 579–585. [Google Scholar] [CrossRef]
- Tobe, T.; Sasakawa, C. Species-specific cell adhesion of enteropathogenic Esherichia coli is mediated by type IV bundle-forming pili. Cell Microbiol. 2002, 4, 29–42. [Google Scholar] [CrossRef]
- Cleary, J.; Lai, L.C.; Shaw, R.K.; Straatman-Iwanowska, A.; Donnenberg, M.S.; Frankel, G.; Knutton, S. Enteropathogenic Esherichia coli (EPEC) adhesion to intestinal epithelial cells: Role of bundle-forming pili (BFP), EspA filaments and intimin. Microbiology 2004, 150, 527–538. [Google Scholar] [CrossRef]
- Bieber, D.; Ramer, S.W.; Wu, C.Y.; Murray, W.J.; Tobe, T.; Fernandez, R.; Schoolnik, G.K. Type IV pili, transient bacterial aggregates, and virulence of enteropathogenic Esherichia coli. Science 1998, 280, 2114–2118. [Google Scholar] [CrossRef]
- Oswald, E.; Schmidt, H.; Morabito, S.; Karch, H.; Marches, O.; Caprioli, A. Typing of intimin genes in human and animal enterohemorrhagic and enteropathogenic Esherichia coli: Characterization of a new intimin variant. Infect. Immun. 2000, 68, 64–71. [Google Scholar] [CrossRef]
- Kelly, G.; Prasannan, S.; Daniell, S.; Fleming, K.; Frankel, G.; Dougan, G.; Connerton, I.; Matthews, S. Structure of the cell-adhesion fragment of intimin from enteropathogenic Esherichia coli. Nat. Struct. Biol. 1999, 6, 313–318. [Google Scholar] [CrossRef]
- Frankel, G.; Candy, D.C.; Fabiani, E.; du-Bobie, J.; Gil, S.; Novakova, M.; Phillips, A.D.; Dougan, G. Molecular characterization of a carboxy-terminal eukaryotic-cell-binding domain of intimin from enteropathogenic Esherichia coli. Infect. Immun. 1995, 63, 4323–4328. [Google Scholar]
- Muza-Moons, M.M.; Koutsouris, A.; Hecht, G. Disruption of cell polarity by enteropathogenic Esherichia coli enables basolateral membrane proteins to migrate apically and to potentiate physiological consequences. Infect. Immun. 2003, 71, 7069–7078. [Google Scholar] [CrossRef]
- Torres, A.G.; Giron, J.A.; Perna, N.T.; Burland, V.; Blattner, F.R.; velino-Flores, F.; Kaper, J.B. Identification and characterization of lpfABCC'DE, a fimbrial operon of enterohemorrhagic Esherichia coli O157:H7. Infect. Immun. 2002, 70, 5416–5427. [Google Scholar]
- Torres, A.G.; Kanack, K.J.; Tutt, C.B.; Popov, V.; Kaper, J.B. Characterization of the second long polar (LP) fimbriae of Esherichia coli O157:H7 and distribution of LP fimbriae in other pathogenic E. coli strains. FEMS Microbiol. Lett. 2004, 238, 333–344. [Google Scholar]
- Fitzhenry, R.; Dahan, S.; Torres, A.G.; Chong, Y.; Heuschkel, R.; Murch, S.H.; Thomson, M.; Kaper, J.B.; Frankel, G.; Phillips, A.D. Long polar fimbriae and tissue tropism in Esherichia coli O157:H7. Microb. Infect. 2006, 8, 1741–1749. [Google Scholar] [CrossRef]
- Jordan, D.M.; Cornick, N.; Torres, A.G.; an-Nystrom, E.A.; Kaper, J.B.; Moon, H.W. Long polar fimbriae contribute to colonization by Esherichia coli O157:H7 in vivo. Infect. Immun. 2004, 72, 6168–6171. [Google Scholar]
- Czeczulin, J.R.; Balepur, S.; Hicks, S.; Phillips, A.; Hall, R.; Kothary, M.H.; Navarro-Garcia, F.; Nataro, J.P. Aggregative adherence fimbria II, a second fimbrial antigen mediating aggregative adherence in enteroaggregative Esherichia coli. Infect. Immun. 1997, 65, 4135–4145. [Google Scholar]
- Bernier, C.; Gounon, P.; Le, B.C. Identification of an aggregative adhesion fimbria (AAF) type III-encoding operon in enteroaggregative Esherichia coli as a sensitive probe for detecting the AAF-encoding operon family. Infect. Immun. 2002, 70, 4302–4311. [Google Scholar] [CrossRef]
- Boisen, N.; Struve, C.; Scheutz, F.; Krogfelt, K.A.; Nataro, J.P. New adhesin of enteroaggregative Esherichia coli related to the Afa/Dr/AAF family. Infect. Immun. 2008, 76, 3281–3292. [Google Scholar] [CrossRef]
- Boll, E.J.; Struve, C.; Sander, A.; Demma, Z.; Nataro, J.P.; McCormick, B.A.; Krogfelt, K.A. The fimbriae of enteroaggregative Esherichia coli induce epithelial inflammation in vitro and in a human intestinal xenograft model. J. Infect. Dis. 2012, 206, 714–722. [Google Scholar] [CrossRef]
- Konar, M.; Sachin, O.; Priya, A.; Ghosh, S. Identification of key proteins of cultured human intestinal cells involved in interaction with enteroaggregative Esherichia coli. FEMS Immunol. Med. Microbiol. 2012, 66, 177–190. [Google Scholar] [CrossRef]
- Piva, I.C.; Pereira, A.L.; Ferraz, L.R.; Silva, R.S.; Vieira, A.C.; Blanco, J.E.; Blanco, M.; Blanco, J.; Giugliano, L.G. Virulence markers of enteroaggregative Esherichia coli isolated from children and adults with diarrhea in Brasilia, Brazil. J. Clin. Microbiol. 2003, 41, 1827–1832. [Google Scholar] [CrossRef]
- Pereira, A.L.; Ferraz, L.R.; Silva, R.S.; Giugliano, L.G. Enteroaggregative Esherichia coli virulence markers: Positive association with distinct clinical characteristics and segregation into 3 enteropathogenic E. coli serogroups. J. Infect. Dis. 2007, 195, 366–374. [Google Scholar] [CrossRef]
- Boisen, N.; Scheutz, F.; Rasko, D.A.; Redman, J.C.; Persson, S.; Simon, J.; Kotloff, K.L.; Levine, M.M.; Sow, S.; Tamboura, B.; et al. Genomic characterization of enteroaggregative Esherichia coli from children in Mali. J. Infect. Dis. 2012, 205, 431–444. [Google Scholar] [CrossRef]
- Monteiro-Neto, V.; Bando, S.Y.; Moreira-Filho, C.A.; Giron, J.A. Characterization of an outer membrane protein associated with haemagglutination and adhesive properties of enteroaggregative Esherichia coli O111:H12. Cell Microbiol. 2003, 5, 533–547. [Google Scholar] [CrossRef]
- Dudley, E.G.; Abe, C.; Ghigo, J.M.; Latour-Lambert, P.; Hormazabal, J.C.; Nataro, J.P. An IncI1 plasmid contributes to the adherence of the atypical enteroaggregative Esherichia coli strain C1096 to cultured cells and abiotic surfaces. Infect. Immun. 2006, 74, 2102–2114. [Google Scholar] [CrossRef]
- Pereira, A.L.; Silva, T.N.; Gomes, A.C.; Araujo, A.C.; Giugliano, L.G. Diarrhea-associated biofilm formed by enteroaggregative Esherichia coli and aggregative Citrobacter freundii: A consortium mediated by putative F pili. BMC Microbiol. 2010, 10, 57. [Google Scholar] [CrossRef]
- Tacket, C.O.; Moseley, S.L.; Kay, B.; Losonsky, G.; Levine, M.M. Challenge studies in volunteers using Esherichia coli strains with diffuse adherence to HEp-2 cells. J. Infect. Dis. 1990, 162, 550–552. [Google Scholar] [CrossRef]
- Mansan-Almeida, R.; Pereira, A.L.; Giugliano, L.G. Diffusely adherent Esherichia coli strains isolated from children and adults constitute two different populations. BMC Microbiol. 2013, 13, 22. [Google Scholar] [CrossRef]
- Arikawa, K.; Meraz, I.M.; Nishikawa, Y.; Ogasawara, J.; Hase, A. Interleukin-8 secretion by epithelial cells infected with diffusely adherent Esherichia coli possessing Afa adhesin-coding genes. Microbiol. Immunol. 2005, 49, 493–503. [Google Scholar]
- Fujihara, S.; Arikawa, K.; Aota, T.; Tanaka, H.; Nakamura, H.; Wada, T.; Hase, A.; Nishikawa, Y. Prevalence and properties of diarrheagenic Esherichia coli among healthy individuals in Osaka City, Japan. Jpn. J. Infect. Dis. 2009, 62, 318–323. [Google Scholar]
- Servin, A.L. Pathogenesis of Afa/Dr diffusely adhering Esherichia coli. Clin. Microbiol. Rev. 2005, 18, 264–292. [Google Scholar] [CrossRef]
- Baranov, V.; Hammarstrom, S. Carcinoembryonic antigen (CEA) and CEA-related cell adhesion molecule 1 (CEACAM1), apically expressed on human colonic M cells, are potential receptors for microbial adhesion. Histochem. Cell Biol. 2004, 121, 83–89. [Google Scholar] [CrossRef]
- Guignot, J.; Peiffer, I.; Bernet-Camard, M.F.; Lublin, D.M.; Carnoy, C.; Moseley, S.L.; Servin, A.L. Recruitment of CD55 and CD66e brush border-associated glycosylphosphatidylinositol-anchored proteins by members of the Afa/Dr diffusely adhering family of Esherichia coli that infect the human polarized intestinal Caco-2/TC7 cells. Infect. Immun. 2000, 68, 3554–3563. [Google Scholar]
- O'Ryan, M.; Prado, V.; Pickering, L.K. A millennium update on pediatric diarrheal illness in the developing world. Semin. Pediatr. Infect. Dis. 2005, 16, 125–136. [Google Scholar] [CrossRef]
- Lamberti, L.M.; Fischer Walker, C.L.; Noiman, A.; Victora, C.; Black, R.E. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health 2011, 11, S15. [Google Scholar]
- Svennerholm, A.M.; Tobias, J. Vaccines against enterotoxigenic Esherichia coli. Exp. Rev. Vaccines. 2008, 7, 795–804. [Google Scholar] [CrossRef]
- Tobias, J.; Svennerholm, A.M. Strategies to overexpress enterotoxigenic Esherichia coli (ETEC) colonization factors for the construction of oral whole-cell inactivated ETEC vaccine candidates. Appl. Microbiol. Biotechnol. 2012, 93, 2291–2300. [Google Scholar] [CrossRef]
- Work Group on Breastfeeding. Breastfeeding and the use of human milk—American Academy of Pediatrics. Pediatrics 1997, 100, 1035–1039. [CrossRef]
- Gartner, L.M.; Morton, J.; Lawrence, R.A.; Naylor, A.J.; O’Hare, D.; Schanler, R.J.; Eidelman, A.I. Breastfeeding and the use of human milk. Pediatrics 2005, 115, 496–506. [Google Scholar] [CrossRef]
- Giugliano, L.G.; Ribeiro, S.T.; Vainstein, M.H.; Ulhoa, C.J. Free secretory component and lactoferrin of human milk inhibit the adhesion of enterotoxigenic Esherichia coli. J. Med. Microbiol. 1995, 42, 3–9. [Google Scholar] [CrossRef]
- Morrow, A.L.; Ruiz-Palacios, G.M.; Jiang, X.; Newburg, D.S. Human-milk glycans that inhibit pathogen binding protect breast-feeding infants against infectious diarrhea. J. Nutr. 2005, 135, 1304–1307. [Google Scholar]
- Coppa, G.V.; Zampini, L.; Galeazzi, T.; Facinelli, B.; Ferrante, L.; Capretti, R.; Orazio, G. Human milk oligosaccharides inhibit the adhesion to Caco-2 cells of diarrheal pathogens: Esherichia coli, Vibrio cholerae, and Salmonella fyris. Pediatr. Res. 2006, 59, 377–382. [Google Scholar] [CrossRef]
- Oliveira, I.R.; de Araujo, A.N.; Bao, S.N.; Giugliano, L.G. Binding of lactoferrin and free secretory component to enterotoxigenic Esherichia coli. FEMS Microbiol. Lett. 2001, 203, 29–33. [Google Scholar]
- De Araujo, A.N.; Giugliano, L.G. Lactoferrin and free secretory component of human milk inhibit the adhesion of enteropathogenic Esherichia coli to HeLa cells. BMC Microbiol. 2001, 1, 25. [Google Scholar] [CrossRef]
- Ochoa, T.J.; Noguera-Obenza, M.; Ebel, F.; Guzman, C.A.; Gomez, H.F.; Cleary, T.G. Lactoferrin impairs type III secretory system function in enteropathogenic Esherichia coli. Infect. Immun. 2003, 71, 5149–5155. [Google Scholar] [CrossRef]
- Martin-Sosa, S.; Martin, M.J.; Hueso, P. The sialylated fraction of milk oligosaccharides is partially responsible for binding to enterotoxigenic and uropathogenic Esherichia coli human strains. J. Nutr. 2002, 132, 3067–3072. [Google Scholar]
- Nascimento de, A.A.; Giugliano, L.G. Human milk fractions inhibit the adherence of diffusely adherent Esherichia coli (DAEC) and enteroaggregative E. coli (EAEC) to HeLa cells. FEMS Microbiol. Lett. 2000, 184, 91–94. [Google Scholar]
- Kawasaki, Y.; Tazume, S.; Shimizu, K.; Matsuzawa, H.; Dosako, S.; Isoda, H.; Tsukiji, M.; Fujimura, R.; Muranaka, Y.; Isihida, H. Inhibitory effects of bovine lactoferrin on the adherence of enterotoxigenic Esherichia coli to host cells. Biosci. Biotechnol. Biochem. 2000, 64, 348–354. [Google Scholar] [CrossRef]
- Flores-Villasenor, H.; Canizalez-Roman, A.; de la, G.M.; Nazmi, K.; Bolscher, J.G.; Leon-Sicairos, N. Lactoferrin and lactoferrin chimera inhibit damage caused by enteropathogenic Esherichia coli in HEp-2 cells. Biochimie 2012, 94, 1935–1942. [Google Scholar] [CrossRef]
- Flores-Villasenor, H.; Canizalez-Roman, A.; Velazquez-Roman, J.; Nazmi, K.; Bolscher, J.G.; Leon-Sicairos, N. Protective effects of lactoferrin chimera and bovine lactoferrin in a mouse model of enterohaemorrhagic Esherichia coli O157:H7 infection. Biochem. Cell Biol. 2012, 90, 405–411. [Google Scholar] [CrossRef]
- Ochoa, T.J.; Brown, E.L.; Guion, C.E.; Chen, J.Z.; McMahon, R.J.; Cleary, T.G. Effect of lactoferrin on enteroaggregative E. coli (EAEC). Biochem. Cell Biol. 2006, 84, 369–376. [Google Scholar] [CrossRef]
- Perrier, C.; Sprenger, N.; Corthesy, B. Glycans on secretory component participate in innate protection against mucosal pathogens. J. Biol. Chem. 2006, 281, 14280–14287. [Google Scholar] [CrossRef]
- Gonzalez-Chavez, S.A.; Arevalo-Gallegos, S.; Rascon-Cruz, Q. Lactoferrin: Structure, function and applications. Int. J. Antimicrob. Agents 2009, 33, 301–308. [Google Scholar]
- Vogel, H.J. Lactoferrin, a bird's eye view. Biochem. Cell Biol. 2012, 90, 233–244. [Google Scholar] [CrossRef]
- Steiner, T.S.; Lima, A.A.; Nataro, J.P.; Guerrant, R.L. Enteroaggregative Esherichia coli produce intestinal inflammation and growth impairment and cause interleukin-8 release from intestinal epithelial cells. J. Infect. Dis. 1998, 177, 88–96. [Google Scholar] [CrossRef]
- Greenberg, D.E.; Jiang, Z.D.; Steffen, R.; Verenker, M.P.; DuPont, H.L. Markers of inflammation in bacterial diarrhea among travelers, with a focus on enteroaggregative Esherichia coli pathogenicity. J. Infect. Dis. 2002, 185, 944–949. [Google Scholar] [CrossRef]
- Snoeck, V.; Peters, I.R.; Cox, E. The IgA system: A comparison of structure and function in different species. Vet. Res. 2006, 37, 455–467. [Google Scholar] [CrossRef]
- Phalipon, A.; Corthesy, B. Novel functions of the polymeric Ig receptor: Well beyond transport of immunoglobulins. Trends Immunol. 2003, 24, 55–58. [Google Scholar] [CrossRef]
- Newburg, D.S. Oligosaccharides in human milk and bacterial colonization. J. Pediatr. Gastroenterol. Nutr. 2000, 30, S8–S17. [Google Scholar] [CrossRef]
- Cravioto, A.; Tello, A.; Villafan, H.; Ruiz, J.; del, V.S.; Neeser, J.R. Inhibition of localized adhesion of enteropathogenic Esherichia coli to HEp-2 cells by immunoglobulin and oligosaccharide fractions of human colostrum and breast milk. J. Infect. Dis. 1991, 163, 1247–1255. [Google Scholar] [CrossRef]
- Mata, L.J.; Wyatt, R.G. The uniqueness of human milk. Host resistance to infection. Am. J. Clin. Nutr. 1971, 24, 976–986. [Google Scholar]
- Caceres, A.; Mata, L.J. Indirect hemagglutination for the study of antibodies to enterobacteriaceae. Rev. Latinoam. Microbiol. 1970, 12, 137–144. [Google Scholar]
- Hanson, L.A.; Winberg, J. Breast milk and defence against infection in the newborn. Arch. Dis. Child 1972, 47, 845–848. [Google Scholar] [CrossRef]
- Jelliffe, D.B. Active anti-infective properties of human milk. Lancet 1971, 2, 167–168. [Google Scholar] [CrossRef]
- Bessler, H.C.; de Oliveira, I.R.; Giugliano, L.G. Human milk glycoproteins inhibit the adherence of Salmonella typhimurium to HeLa cells. Microbiol. Immunol. 2006, 50, 877–882. [Google Scholar]
- Willer, E.M.; Lima, R.L.; Giugliano, L.G. In vitro adhesion and invasion inhibition of Shigella dysenteriae, Shigella flexneri and Shigella sonnei clinical strains by human milk proteins. BMC Microbiol. 2004, 4, 18. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Pereira, A.L.; Giugliano, L.G. Adhesion of Diarrheagenic Escherichia coli and Inhibition by Glycocompounds Engaged in the Mucosal Innate Immunity. Biology 2013, 2, 810-831. https://doi.org/10.3390/biology2020810
Pereira AL, Giugliano LG. Adhesion of Diarrheagenic Escherichia coli and Inhibition by Glycocompounds Engaged in the Mucosal Innate Immunity. Biology. 2013; 2(2):810-831. https://doi.org/10.3390/biology2020810
Chicago/Turabian StylePereira, Alex L., and Loreny G. Giugliano. 2013. "Adhesion of Diarrheagenic Escherichia coli and Inhibition by Glycocompounds Engaged in the Mucosal Innate Immunity" Biology 2, no. 2: 810-831. https://doi.org/10.3390/biology2020810




