1. Introduction
Electronic Fetal Monitoring (EFM) is an essential requirement when assessing the health state of the fetus and its overall growth and development inside the uterus during pregnancy and labor [
1]. In high-risk conditions like an Intra-Uterine Growth Retarded (IUGR) fetus or pregnancies complicated by pathologies like diabetes, infections, pre-eclampsia or placental abruption, etc., long-term fetal monitoring is required [
2]. Fetal Heart Rate (FHR) analysis using the Cardiotocograph (CTG) or by direct fetal scalp ECG are the most effective techniques for fetal well-being assessment [
3]. However, CTG is not suitable for long-term monitoring and requires highly experienced medical personnel for the interpretation of FHR traces. Fetal scalp Electrocardiogram (ECG) recordings are considered to be the gold standard in FHR monitoring, but can only be applied when the membrane has been ruptured [
4]. Considering the above limitations, a non-invasive alternative for FHR monitoring is abdominal ECG (aECG) recordings. In the aECG method, electrodes are placed on the mother’s abdomen, which acquire a composite ECG signal, which consists of both fetal ECG (fECG) and maternal ECG (mECG) [
5] along with other artifacts like muscle contraction noise, power line interferences, various electrical noise, fetal movement and uterine contractions [
6]. The interpretation of morphology, magnitude and frequency of fECG helps physicians to identify overall fetal health state [
7]; however, the magnitude of fECG signals is usually overwhelmed by the magnitude of mECG signals, and significant frequency overlaps with other artifacts make the Signal to Noise Ratio (SNR) of the fECG signal very low. Therefore, advanced signal processing techniques are required for the extraction of fECG from the aECG signal [
8].
Researchers have been working in this direction and successfully evaluated various advanced signal processing methods. Kanjilal et al. proposed a method based on Singular Value Decomposition (SVD) for extraction of fECG from the single channel aECG signal by decomposing it into orthogonal modes and then selecting the most dominant periodic component by Singular Value Ratio (SVR) spectrum analysis [
9]. Based on the Artificial Neural Network (ANN) technique, Hasan et al. used the supervised Multilayer Perception (MLP) network [
10]; Jia et al. used the adaptive linear neural network [
11]; and Golzan et al. used the multi-layer perceptron neural network model for extraction of fECG [
12]. Based on the Adaptive Noise Cancellation (ANC) technique, Zhang et al. used a combination of SVD and Smooth Window (SW) techniques to build a reference signal in an ANC, which is done to eliminate the limitation of having a similar thoracic mECG waveform as that present in acquired the aECG waveform [
13], and Zeng et al. proposed a Recursive Least Squares (RLS)-based ANC approach for fECG extraction by elimination of the mECG signal [
14]. Based on Principal Component Analysis (PCA), Rahmati et al. detected morphological ECG features like FHR, fetal R-peaks and RR interval from maternal aECG recordings collected from the PhysioNet/Computing in Cardiology Challenge 2013 (CinC2013) [
15], Lipponen et al. also used the principal component model for removing the maternal ECG from aECG recordings for the purpose of fetal QRS detection [
16], and Petrolis et al. used multistage PCA for the subtraction of mECG from aECG signals, leaving behind a signal with a higher energy of fECG components; they also tested their methodology on the database collected from PhysioNet/CinC2013 [
17]. Based on the Blind Source Separation (BSS) technique, He et al. proposed a method of mECG and fECG separation from a single channel abdominal signal. They also used the Empirical Mode Decomposition (EMD) method to decompose the collected single channel signal into multiple Intrinsic Mode Function (IMF) mapping single channels [
18]. Ghazdali et al. proposed an approach for denoising of the observed ECG signals using a Bilateral Total Variation (BTV) filter and then minimizing the Kullback–Leibler divergence [
19] between copula densities to separate the fECG signal from the mECG [
20]. Sato et al. proposed a modified blind source separation with the reference signal (BSSR) for fECG extraction by cancellation of the mECG component [
21]. Zarzoso et al. tested three methods for fECG extraction PCA, Higher-Order Singular-Value Decomposition (HOSVD) and Higher-Order Eigenvalue Decomposition (HOEVD) and found that HOEVD was the best amongst them [
22]; in a consecutive study, they implemented higher-order statistics and Widrow’s multireference ANC approach for more robust BSS performance in the fECG extraction problem [
23]. Based on the Adaptive Neuro-Fuzzy Inference System (ANFIS), Assaleh et al. demonstrated the use of the ANFIS network to identify the nonlinear relationship that exists between the mECG signal acquired from thorax and the mECG component derived from the aECG signal, thus helping in the fECG extraction process by subtracting the aligned version of the mECG signal from the aECG signal [
24]. Panigrahy et al. implemented ANFIS along with the Differential Evolution (DE) algorithm and the Extended Kalman Smoother (EKS) for fECG extraction, requiring some degree of operator interaction for assigning the parameters and the EKS state equations [
25]. Su et al. applied a nonlinear time-frequency analysis technique called de-shape Short Time Fourier Transform (STFT) on PhysioNet (adfecgdb) database and CinC2013 database for fECG extraction [
26]. Almeida et al. validated the Wavelet Transform (WT)-based QRS algorithm for localization of the fetal QRS complex in aECG signals acquired from the PhysioNet database [
27].
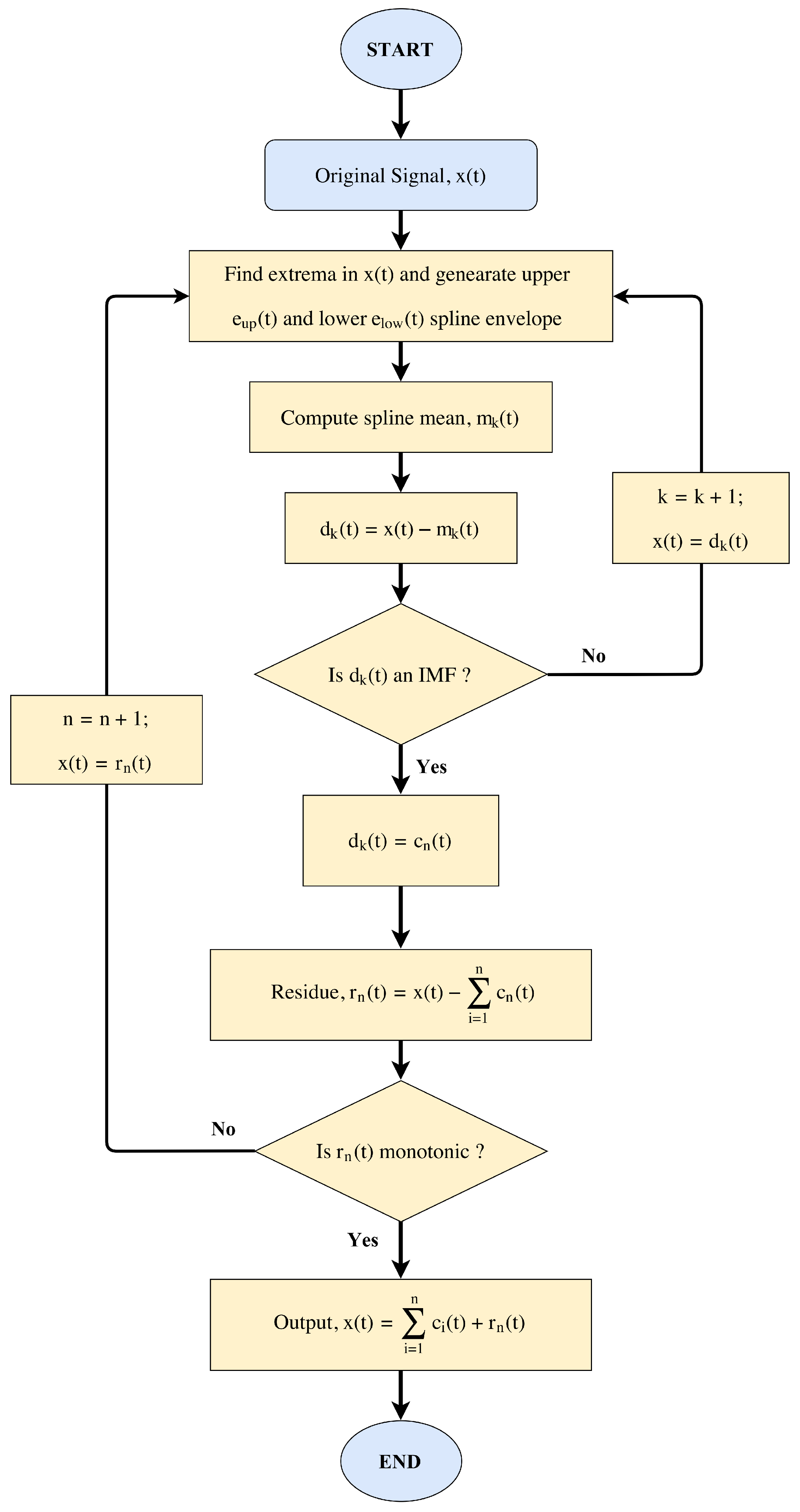
Recently, researchers have been involved in techniques like Empirical Mode Decomposition (EMD) for denoising of ECG signals [
28,
29], baseline wander removal [
30], Power Line Interference (PLI) removal [
31,
32,
33], QRS complex detection [
34,
35], extraction of the respiratory signal from ECG recordings [
36,
37], etc. EMD has emerged to be an essential tool for decomposing a nonlinear and non-stationary signal into its constituent frequency components with higher temporal and spatial resolution as compared to Fourier-based and wavelet-based time-frequency methods. Several improvements in basic EMD have been proposed like Ensemble Empirical Mode Decomposition (EEMD) [
38] and Complete Ensemble Empirical Mode Decomposition with Adaptive Noise (CEEMDAN) [
39] for minimizing the limitations of basic EMD like the “end-effect” and “mode-mixing”. However, very limited research has been done on the topic of the extraction of fetal heart rate information from the aECG signal using EMD [
40,
41,
42].
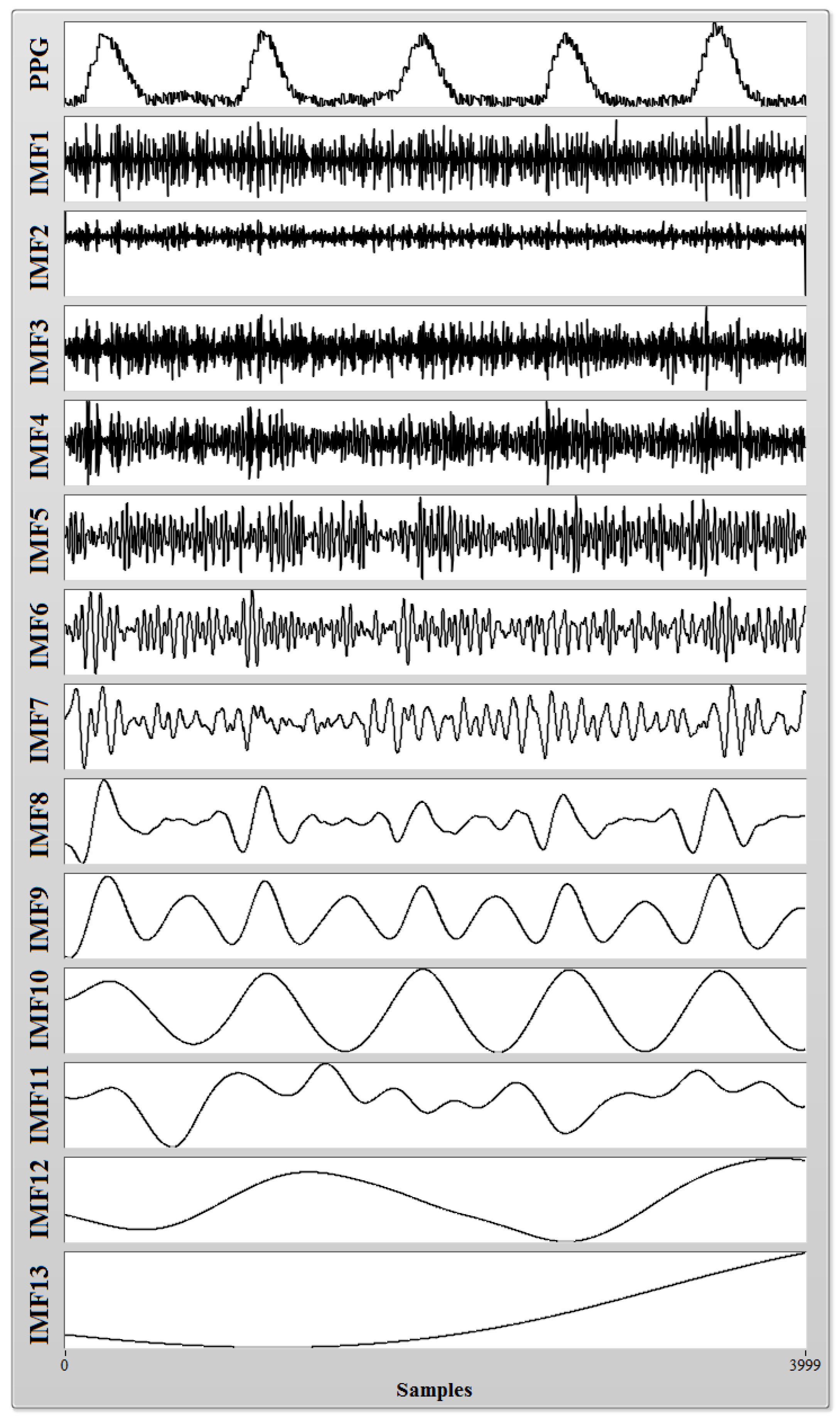
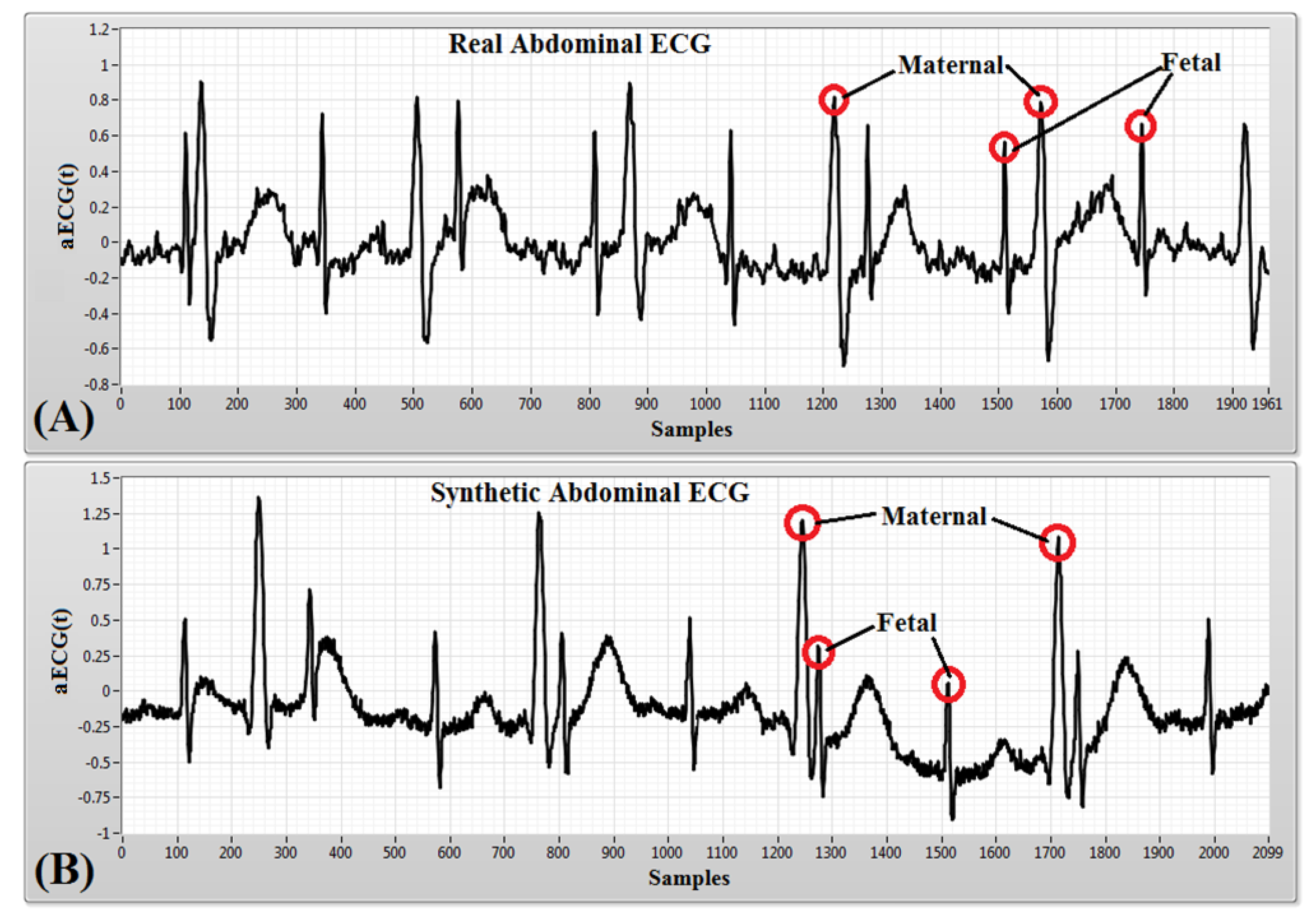
In this paper, we propose the CEEMDAN-based method for reliable extraction of both maternal and fetal heart rate information from the composite aECG signal. The aECG signal datasets used in this research are acquired from three different publicly available online sources. The CEEMDAN technique decomposes the composite aECG signal into a finite number of components separated by instantaneous frequencies called modes [
43,
44]. Careful selection of the modes according to both maternal and fetal components and post-processing for valid R-peak detection results in the extraction of FHR, MHR and their Heart Rate Variability (HRV). Feto-maternal HRV analysis helps the clinician to predict the overall health state of the fetus along with the cardiac autonomic regulation of the fetal heart.
The remainder of the paper is structured as follows: In
Section 2, the review of the EMD technique and its improved versions like EEMD and CEEMDAN is presented. The datasets and proposed methodology are described in
Section 3. In
Section 4, experimental results are presented. In
Section 5, the discussion about the results is presented, and finally, in
Section 6, the main conclusions are pointed out.
4. Experiment and Results
We have used the PhysioNet aECG dataset, as well as the synthetic aECG dataset to evaluate the performance of CEEMDAN for the process of maternal and fetal heart rate extraction from a composite aECG signal. The performance of the proposed method was evaluated by the following measures:
where
FN (False Negative) indicates that the proposed method failed to detect a real heart beat,
FP (False Positive) indicates that the proposed method detects a heart beat when their is no actual beat present,
TP (True Positive) indicates that the real heart beat was detected accurately and
N is the total number of the actual QRS complexes present in the reference signal. The F1 score is calculated based on sensitivity and positive diagnostic value and varies between [0,1]. A value of “1” represents the optimal recognition capability of the proposed method, and a value of “0” represents that the proposed method is incapable of recognition.
Table 4 and
Table 5 present the values of performance measures obtained after applying the proposed CEEMDAN-based feto-maternal heart rate extraction algorithm on all collected aECG datasets. For PhysioNet datasets, we assumed that a maternal R-wave and a fetal R-wave are considered to be True Positives (
TP) if they are detected within ±10 ms from the reference peak. At a sampling rate of 1000 Hz, ±10 ms corresponds to a difference of 10 samples between the reference peak and the detected peaks. For the synthetic database, we have considered a
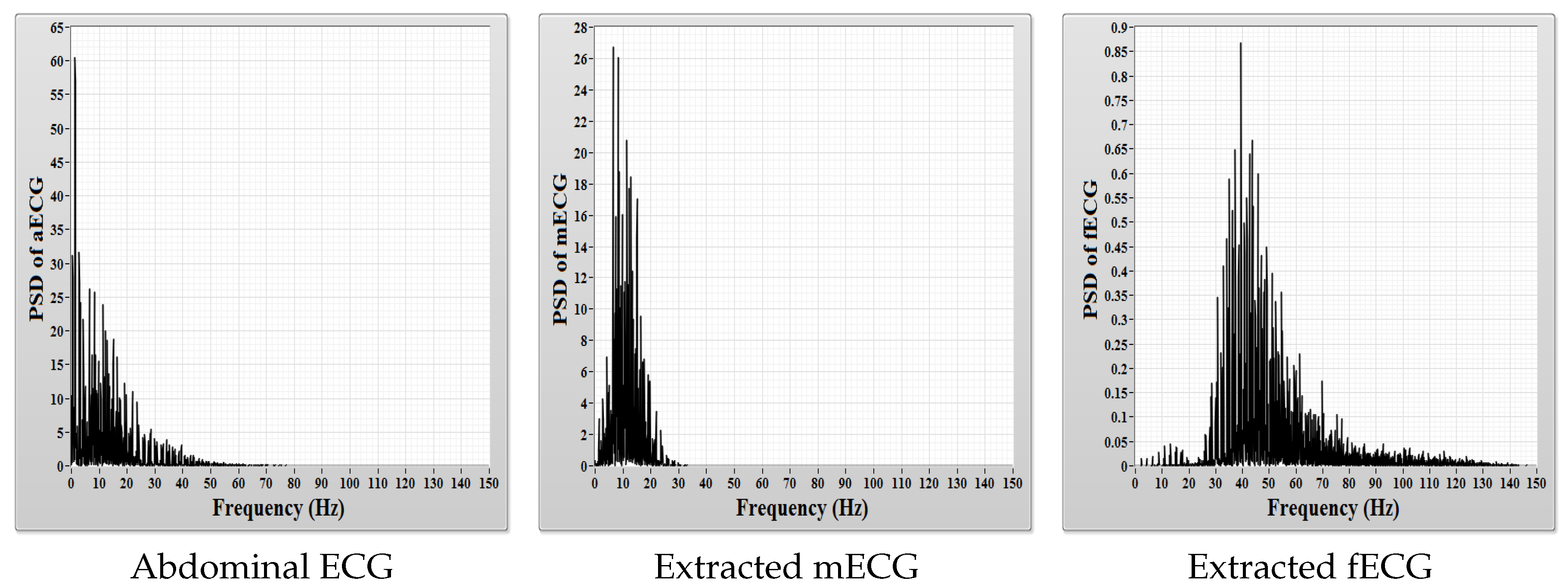
TP case when a peak is detected within a difference of five samples between the reference peak and the detected peaks. The quality of feto-maternal heart rate separation depends on the overlap between their frequency spectrum in the composite abdominal ECG signal. Less frequency overlap means that it is easier to extract feto-maternal heart rate information from aECG signal using decomposition techniques like CEEMDAN. A comparison between the power spectral density of the aECG, mECG and fECG signals is shown in
Figure 10, and the difference between the magnitude of power contained within the mECG signal and within the fECG signal can clearly be observed.
In the case of fetal heart rate detection, from among a total number of 727 maternal QRS complexes recognized in the reference signals, 718 complexes were detected accurately, only nine complexes (1.24%) were missed, whereas the number of detected false complexes was only 16 (2.2%). The mean sensitivity of 98.83%, positive diagnostic value of 97.97%, accuracy of 96.93%, performance index of 96.75% and F1 score of 0.98 were obtained while detecting the maternal QRS complexes after the application of the proposed methodology as shown in
Table 4.
In the case of fetal heart rate detection, from among a total number of 1231 fetal QRS complexes recognized in the reference signals, 1210 complexes were detected accurately, only 21 complexes (1.71%) were missed, whereas the number of detected false complexes was only 28 (2.28%). The mean sensitivity of 98.13%, positive diagnostic value of 97.62%, accuracy of 95.91%, performance index of 95.69% and F1 score of 0.98 were obtained as shown in
Table 5.
We further studied the HRV analysis of the corresponding maternal and fetal heart rate intervals (RR intervals) determined from reference R-peaks and detected R-peaks after the CEEMDAN process.
Table 6, presents the time domain results, while
Table 7 and
Table 8 present the frequency domain results.
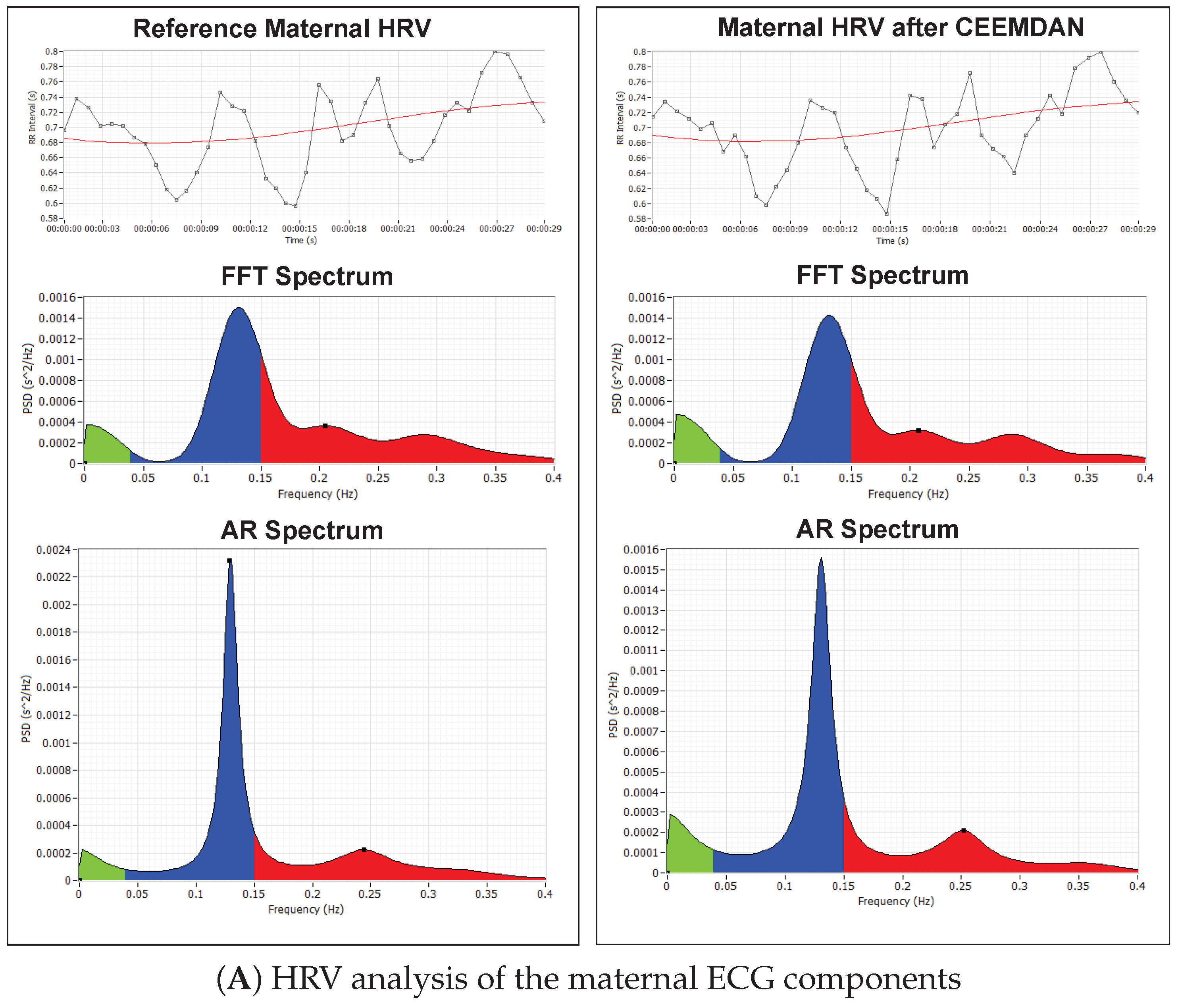
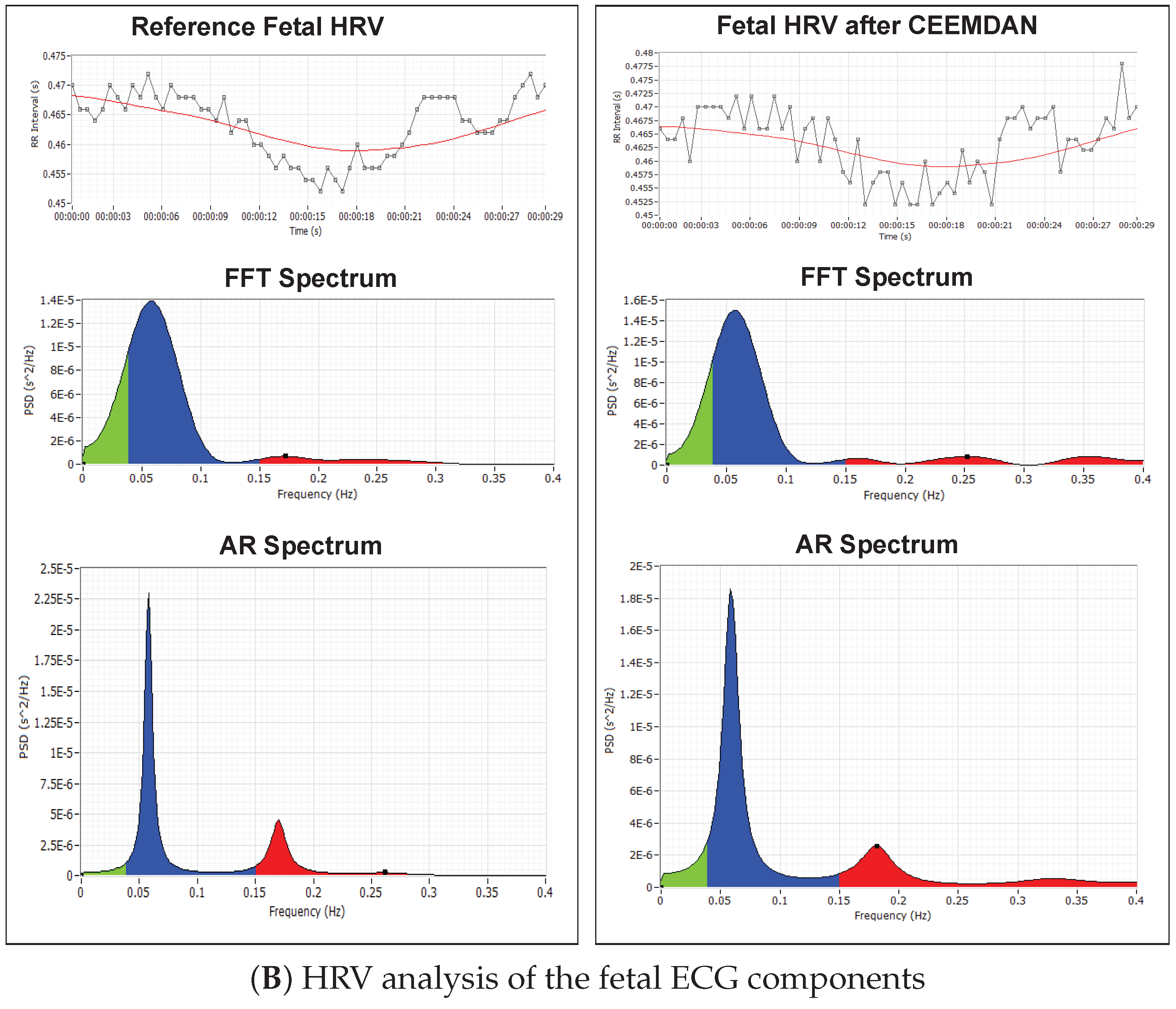
Figure 11 shows the RR intervals plot (tachogram) for both MHR signals and FHR signals derived from the reference signal and the signal obtained after the CEEMDAN process.
Figure 11A shows the RR-tachogram obtained from the reference mECG signal and extracted mECG signal and their corresponding Fast Fourier transform (FFT) spectrum and Autoregressive (AR) power spectrum plots. Various studies in the past have been done to evaluate the relationship between maternal HRV and fetal HRV during pregnancy-related pathologies like hypertension and pre-eclampsia [
56,
57]. The influence of maternal Respiratory Sinus Arrhythmia (RSA) on maternal HRV and fetal autonomic nervous regulation in normal gestation is also investigated by researchers [
57].
Figure 11B shows the RR-tachogram obtained from the reference fECG signal and extracted fECG signal and their corresponding FFT spectrum and Autoregressive (AR) power spectrum plots. The energy content in the frequency range of up to 0.2 Hz indicates the long-term variability, and the frequency range up to 1.5 Hz indicates the short-term variability. Long-term and short-term FHR variability are often related to fetal conditions [
58,
59]. Fetuses also exhibit HRV analogous to an adult subject [
60]; therefore, detailed analysis of fetal HRV can give sensitive information about the autonomic nervous system and cardiovascular system development of the fetus [
60].
6. Conclusions
Monitoring of fetal and maternal heart rate variability provides critical diagnostic information about the health state of the mother and her fetus. Long-term FHR monitoring is crucial in high-risk pregnancies, which can be accomplished only by a non-invasive method like aECG. Although CTG and ultrasound are extensively employed diagnostic tools for non-invasive monitoring of various physiological and morphological parameters of the fetus inside the uterus, it is not preferred for long-term bedside monitoring due to some degree of inconvenience to the patient and the need for frequent attendance by an experienced medical professional.
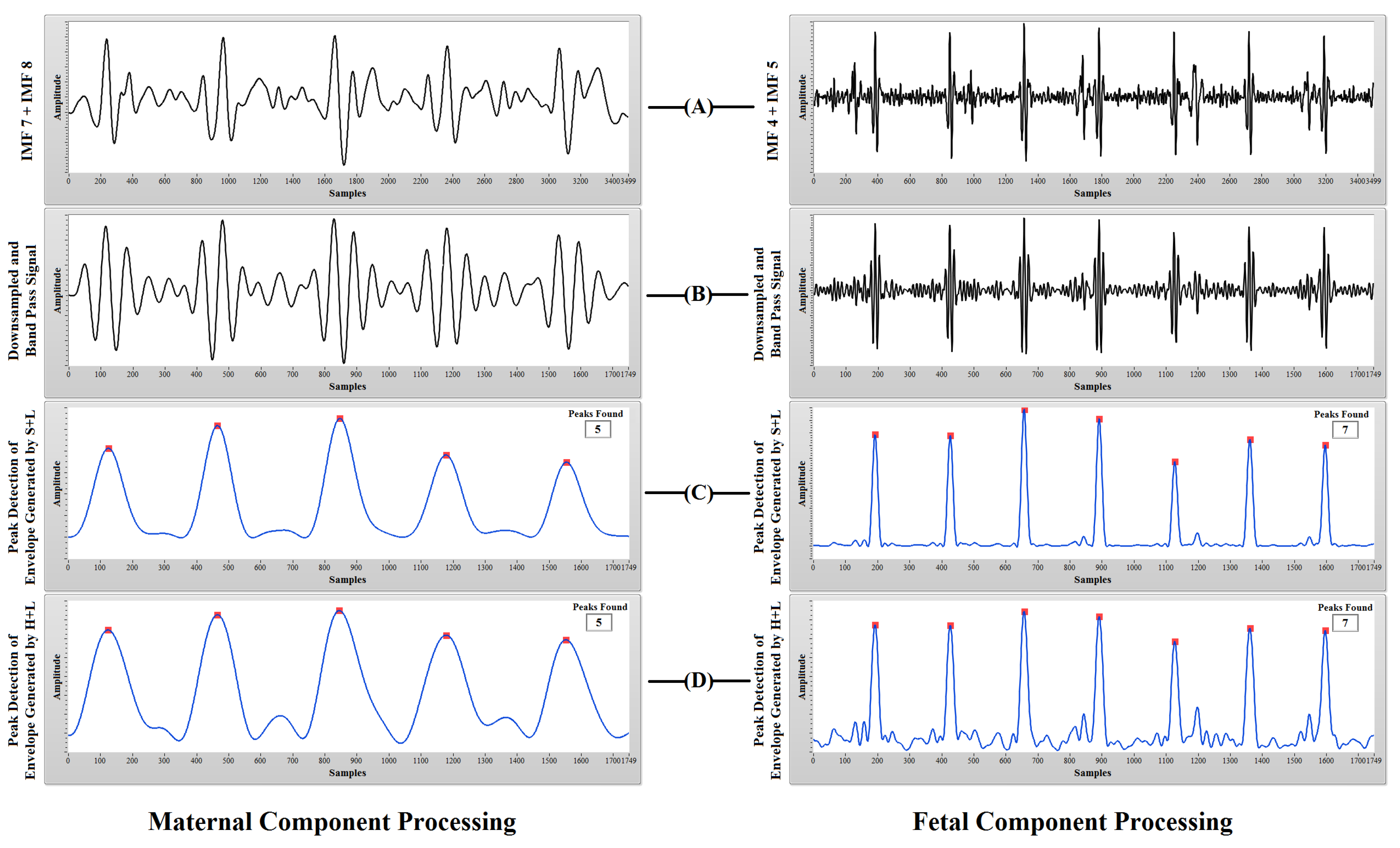
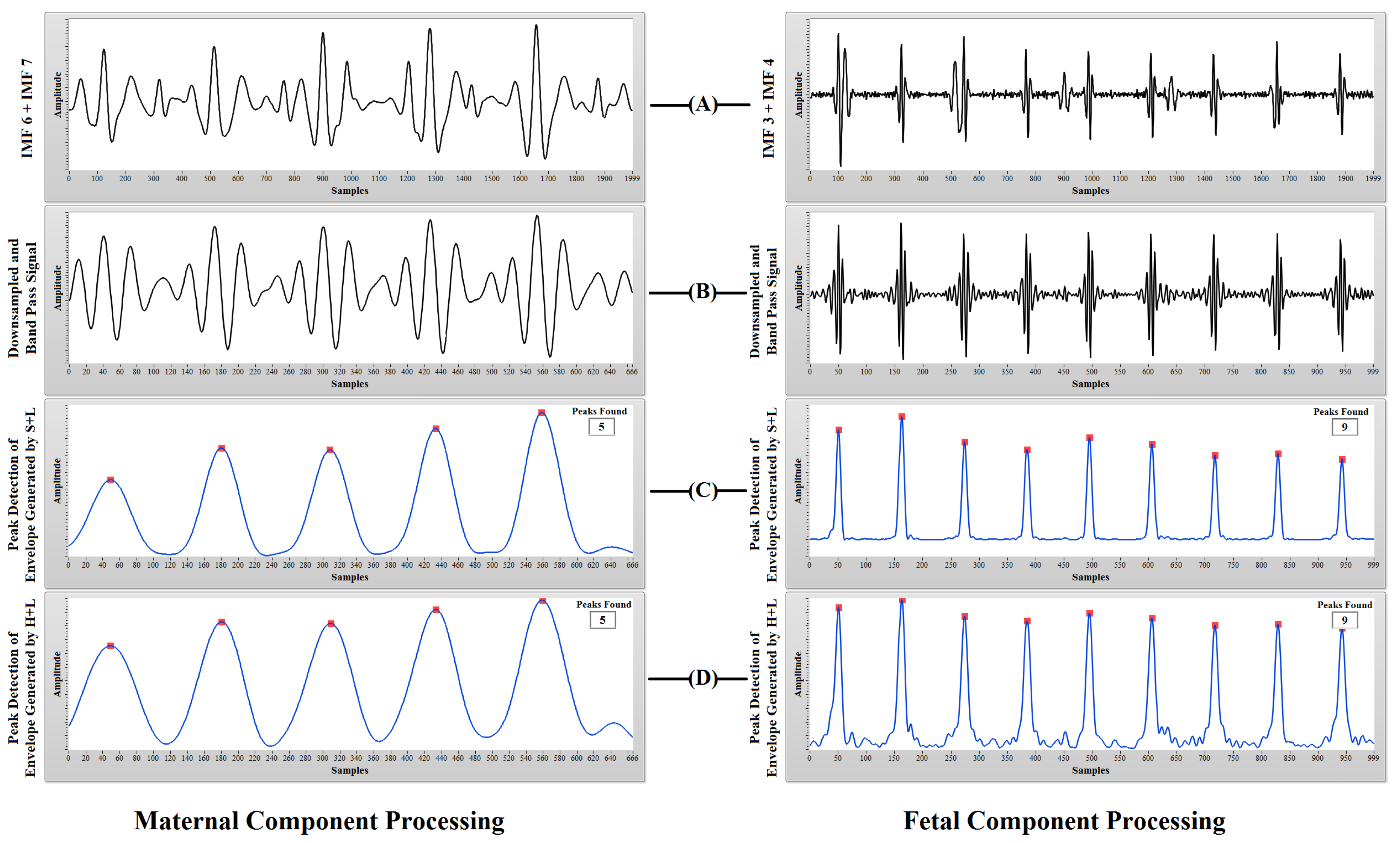
A CEEMDAN-based approach for extraction of both fetal and maternal heart rates from composite aECG recordings is presented in this research. The proposed method is based on the fact that in most of the cases, there is a frequency difference between maternal ECG components and fetal ECG components. CEEMDAN is a robust technique to decompose a composite signal into its respective frequency components called IMFs. CEEMDAN decomposition of the aECG signal produces IMFs in which the lower order IMFs contain higher frequency components (fetal ECG) and higher order IMFs contain lower frequency components (maternal ECG). Manually selecting the IMFs according to probable maternal and fetal components and taking the summation of theses components produces a signal for further post-processing. Post-processing involves downsampling, band pass filtering, envelope generation and peak detection. The detected peaks for both maternal and fetal cases were compared with the reference peaks for identifying TP, FP and FN cases. A TP case is considered when a detected R-peak is within ±10 ms from the reference R-peak. An overall sensitivity of 98.83%, a positive diagnostic value of 97.97%, an accuracy of 96.93% and a performance index of 96.75% were obtained in the case of MHR quantification, and an overall sensitivity of 98.13%, a positive diagnostic value of 97.62%, an accuracy of 95.91% and a performance index of 95.69% were obtained in the case of FHR quantification. The obtained results prove that the proposed CEEMDAN-based methodology is a very robust way of separating maternal and fetal components with good accuracy and sensitivity. It also confirms that an abdominal ECG recording is indeed a very useful technique for fetal heart rate extraction when long-term monitoring of a pregnant woman is required. Furthermore, the CEEMDAN method produces the best results when there is less overlap between the spectral components to be separated. Some limitations like manual selection of IMFs and time consumption during the decomposition process limit the usage of the proposed CEEMDAN-based methodology in a real-time environment. In the future, patient-specific modification of the proposed methodology can eliminate these limitations and can be used in real-time feto-maternal heart rate assessment applications.