MOOC Learners’ Engagement with Two Variants of Virtual Patients: A Randomised Trial
Abstract
:1. Introduction
2. Methods
2.1. Study Context
2.2. Study Design
2.3. Participants
2.4. Data Collection
2.5. Data Analysis
2.6. Ethics
3. Results
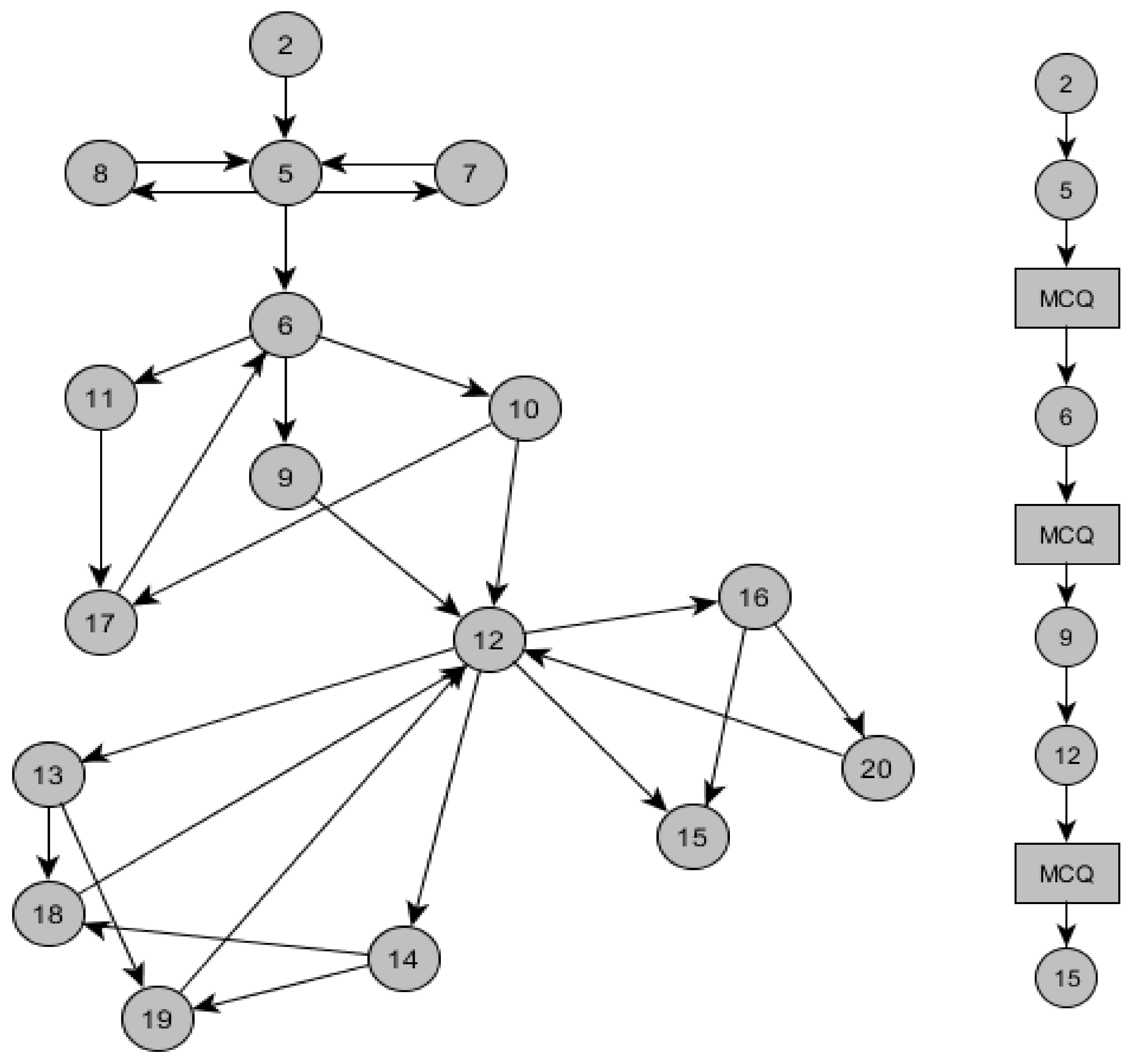
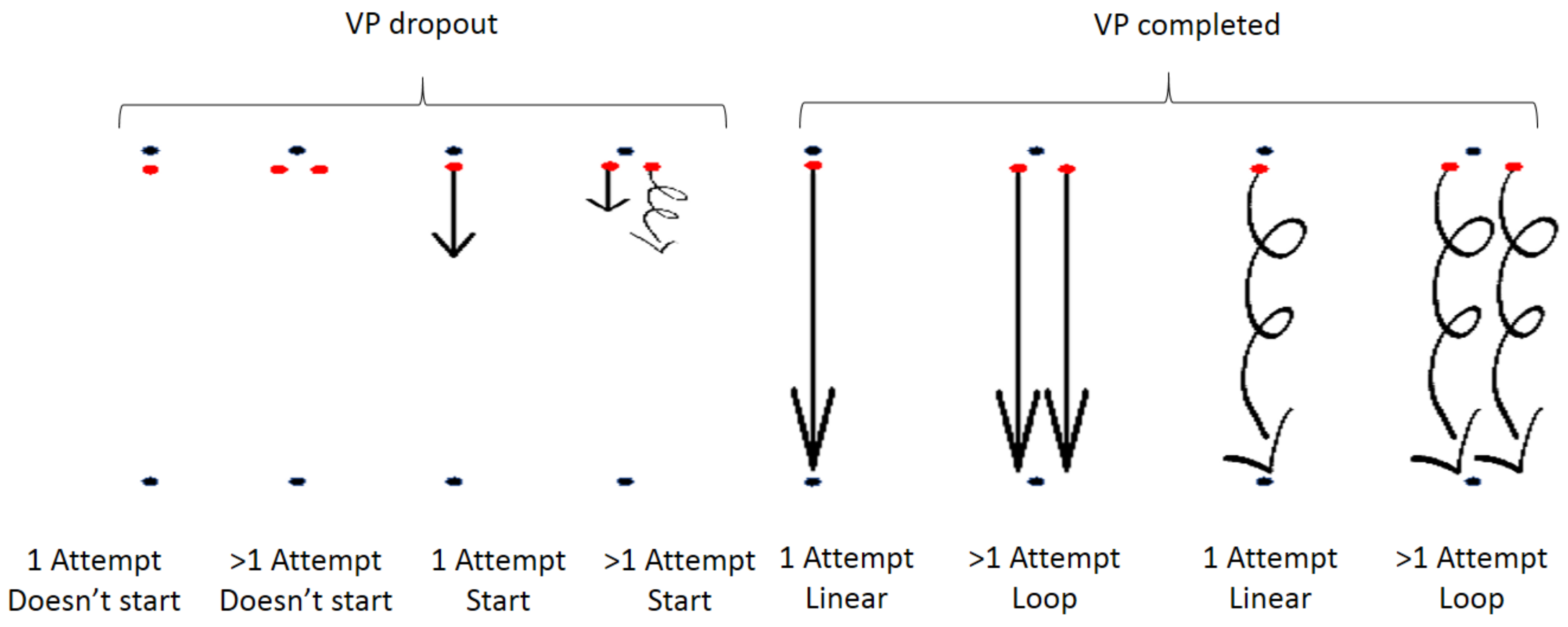
3.1. Learners’ Interaction Patterns with VPs in MOOCs
- Distance between the black dots: length of VP case;
- Red dots: introduction page of VP case;
- Initiated line: user has loaded VP scenario;
- Straight line: linear behaviour in VP scenario;
- Loop line: loop behaviour in VP scenario;
- Multiple straight and loop lines: multiple linear and loop behaviours in VP scenario respectively;
- Incomplete line: dropout from VP scenario;
- Line reaching end dots (Straight or loop): completed VP scenario.
- Attempt: the act of loading the VP introduction page but not starting the VP scenario.
- Start: act of loading the VP scenario after the VP introduction page.
3.2. Influence of Branching Points in a VP Case on the Drop-Out Rate of Learners
4. Discussion
Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Liyanagunawardena, T.; Adams, A.; Williams, S. MOOCs: A Systematic Study of the Published Literature 2008–2012. Int. Rev. Res. Open Distrib. Learn. 2013, 14, 202–227. [Google Scholar] [CrossRef]
- Isaac, C.; Andrew, H. HarvardX and MITx: Four Years of Open Online Courses—Fall 2012–Summer 2016. SSRN. 2016. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2889436 (accessed on 29 March 2018).
- Kearney, R.C.; Premaraj, S.; Smith, B.M.; Olson, G.W.; Williamson, A.E.; Romanos, G. Massive Open Online Courses in Dental Education: Two Viewpoints: Viewpoint 1: Massive Open Online Courses Offer Transformative Technology for Dental Education and Viewpoint 2: Massive Open Online Courses Are Not Ready for Primetime. J. Dent. Educ. 2016, 80, 121–127. [Google Scholar] [PubMed]
- Akyol, Z.; Vaughan, N.; Garrison, D.R. The impact of course duration on the development of a community of inquiry. Interact. Learn. Environ. 2011, 19, 231–246. [Google Scholar] [CrossRef]
- Ebben, M.; Murphy, J.S. Unpacking MOOC scholarly discourse: A review of nascent MOOC scholarship. Learn. Media Technol. 2014, 39, 328–345. [Google Scholar] [CrossRef]
- Laurillard, D. Multimedia and the changing experience of the learner. Br. J. Educ. Technol. 1995, 26, 179–189. [Google Scholar] [CrossRef]
- Khalil, H.; Ebner, M. MOOCs Completion Rates and Possible Methods to Improve Retention—A Literature Review. In Proceedings of the World Conference on Educational Multimedia, Hypermedia and Telecommunications, Tampere, Finland, 23 June 2014; pp. 1236–1244. [Google Scholar]
- Ellaway, R.; Candler, C.; Greene, P.; Smothers, V. An Architectural Model for MedBiquitous Virtual Patients; Technical Report; MedBiquitous: Baltimore, MD, USA, 2006. [Google Scholar]
- Stathakarou, N.; Zary, N.; Kononowicz, A.A. Virtual Patients in Massive Open Online Courses-Design Implications and Integration Strategies. Stud. Health Technol. Inform. 2014, 205, 793–797. [Google Scholar] [PubMed]
- Stathakarou, N.; Zary, N.; Kononowicz, A.A. Beyond xMOOCs in healthcare education: Study of the feasibility in integrating virtual patient systems and MOOC platforms. PeerJ 2014, 2, e672. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.H.; Biguet, G.; Stathakarou, N.; Westin-Hägglöf, B.; Jeding, K.; McGrath, C.; Zary, N.; Kononowicz, A.A. Virtual Patients in a Behavioral Medicine Massive Open Online Course (MOOC): A Qualitative and Quantitative Analysis of Participants’ Perceptions. Acad. Psychiatry 2017, 41, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Henningsohn, L.; Dastaviz, N.; Stathakarou, N.; McGrath, C. KIUrologyX: Urology as You Like It—A Massive Open Online Course for Medical Students, Professionals, Patients, and Laypeople Alike. Eur. Urol. 2017, 72, 321–322. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.; Triola, M. Virtual patients: A critical review and proposed next steps. Med. Educ. 2009, 43, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, R.; Poulton, T.; Fors, U.; McGee, J.B.; Albright, S. Building a virtual patient commons. Med. Teach. 2008, 30, 170–174. [Google Scholar] [CrossRef] [PubMed]
- McGaghie, W.C.; Issenberg, S.B.; Petrusa, E.R.; Scalese, R.J. A critical review of simulation-based medical education research: 2003–2009. Med. Educ. 2010, 44, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.A.; Erwin, P.J.; Triola, M.M. Computerized virtual patients in health professions education: A systematic review and meta-analysis. Acad. Med. 2010, 85, 1589–1602. [Google Scholar] [CrossRef] [PubMed]
- Narciss, S. Feedback Strategies for Interactive Learning Tasks. In Handbook of Research on Educational Communications and Technology; Spector, J.M., Merrill, M.D., van Merriënboer, J., Driscoll, M.P., Eds.; Routledge: Abingdon, UK, 2007. [Google Scholar]
- Bing-You, R.; Hayes, V.; Varaklis, K.; Trowbridge, R.; Kemp, H.; McKelvy, D. Feedback for learners in medical education: What is known? A scoping review. Acad. Med. 2017, 92, 1346–1354. [Google Scholar] [CrossRef]
- Clark, R.C.; Mayer, R.E. Scenario-Based e-Learning: Evidence-Based Guidelines for Online Workforce Learning; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development; FT Press: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Huwendiek, S.; Reichert, F.; Bosse, H.M.; De Leng, B.A.; Van Der Vleuten, C.P.; Haag, M.; Tönshoff, B. Design principles for virtual patients: A focus group study among students. Med. Educ. 2009, 43, 580–588. [Google Scholar] [CrossRef] [PubMed]
- OpenLabyrinth—Virtual Scenarios and Education Research. Available online: http://openlabyrinth.ca/ (accessed on 26 February 2018).
- Poulton, T.; Ellaway, R.H.; Round, J.; Jivram, T.; Kavia, S. Exploring the efficacy of replacing linear paper-based patient cases in problem-based learning with dynamic Web-based virtual patients: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e240. [Google Scholar] [CrossRef] [PubMed]
| Learner Interaction Patterns | Total (n = 378) | ||
|---|---|---|---|
| VP dropout | 1 Attempt | Does not Start | 51 |
| Start | 14 | ||
| >1 Attempt | Does not Start | 3 | |
| Start | 3 | ||
| Completed | 1 Attempt | Linear behaviour | 209 |
| Loop behaviour | 46 | ||
| >1 Attempt | Linear behaviour | 36 | |
| Loop behaviour | 16 | ||
| VP Design | Dropout | |
|---|---|---|
| Yes | No | |
| VP1 | 16 (9) | 149 (156) |
| VP2 | 1 (8) | 158 (151) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stathakarou, N.; Scully, M.L.; Kononowicz, A.A.; Henningsohn, L.; Zary, N.; McGrath, C. MOOC Learners’ Engagement with Two Variants of Virtual Patients: A Randomised Trial. Educ. Sci. 2018, 8, 44. https://doi.org/10.3390/educsci8020044
Stathakarou N, Scully ML, Kononowicz AA, Henningsohn L, Zary N, McGrath C. MOOC Learners’ Engagement with Two Variants of Virtual Patients: A Randomised Trial. Education Sciences. 2018; 8(2):44. https://doi.org/10.3390/educsci8020044
Chicago/Turabian StyleStathakarou, Natalia, Marcel Leon Scully, Andrzej A. Kononowicz, Lars Henningsohn, Nabil Zary, and Cormac McGrath. 2018. "MOOC Learners’ Engagement with Two Variants of Virtual Patients: A Randomised Trial" Education Sciences 8, no. 2: 44. https://doi.org/10.3390/educsci8020044





