Emotions and Emotion Regulation in Breast Cancer Survivorship
Abstract
:1. Introduction
2. Emotional Response to Cancer: What We Know Now
2.1. What Types of Emotions Do Cancer Patients Experience?
2.2. How Prevalent Are Negative Emotions among Cancer Patients?
2.3. Following Treatment, Do Patients’ Emotional Experiences Improve?
3. Emotion Regulation: Basic Principles from Affective Science
3.1. What is Emotion Regulation?
3.2. How Is Emotion Regulation Measured?
3.2.1. Self-Report Measures
3.2.2. Observational Methods
3.3. Does Emotion Regulation Affect Psychological Health?
3.4. Does Emotion Regulation Affect Physical Health?
4. Emotion Regulation in the Context of Cancer: Emerging Evidence
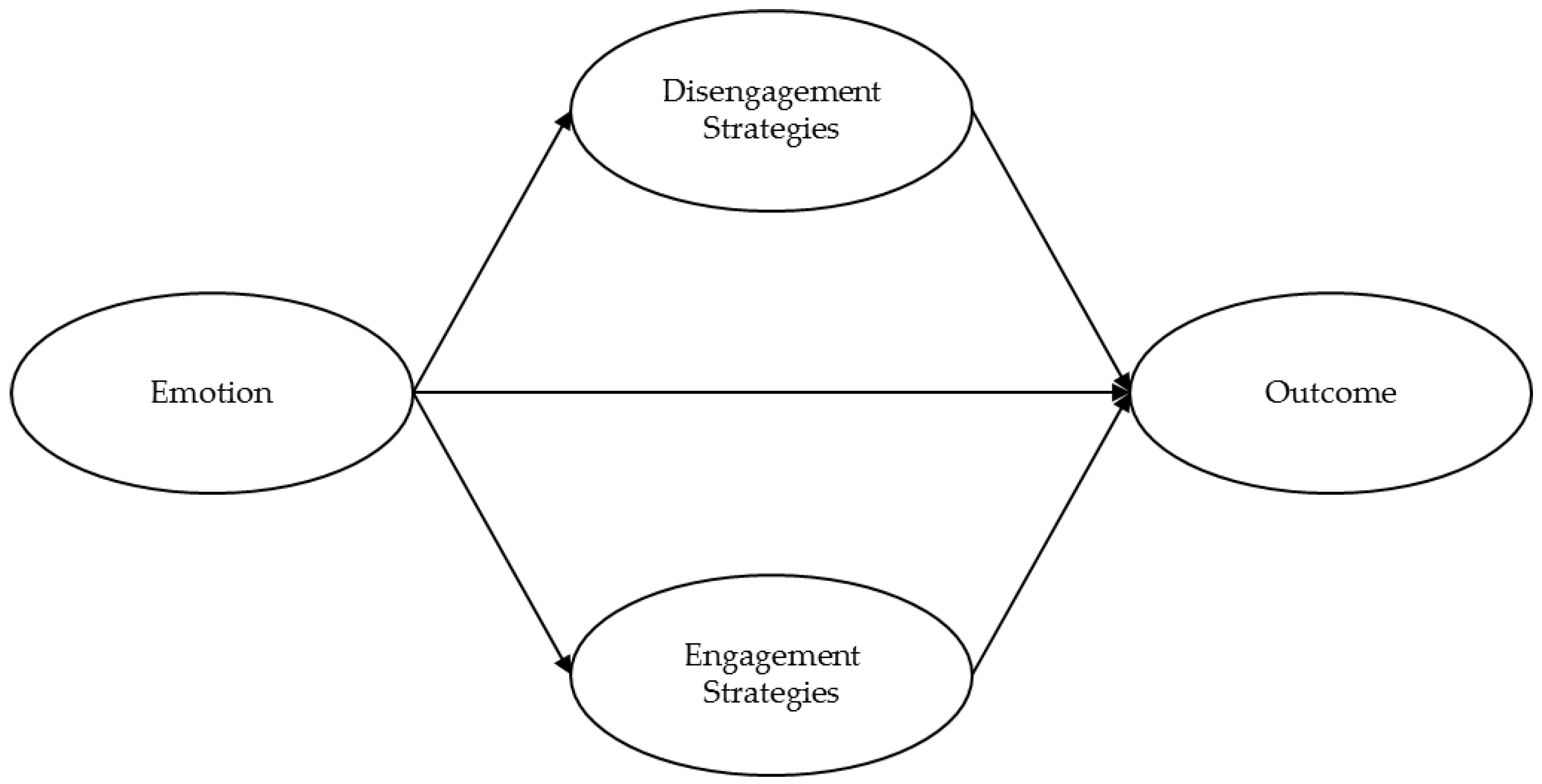
5. Putting It All Together: A Guiding Emotion Regulation Model
6. New Findings: Emotion Regulation in Recurrent Breast Cancer
6.1. Methods
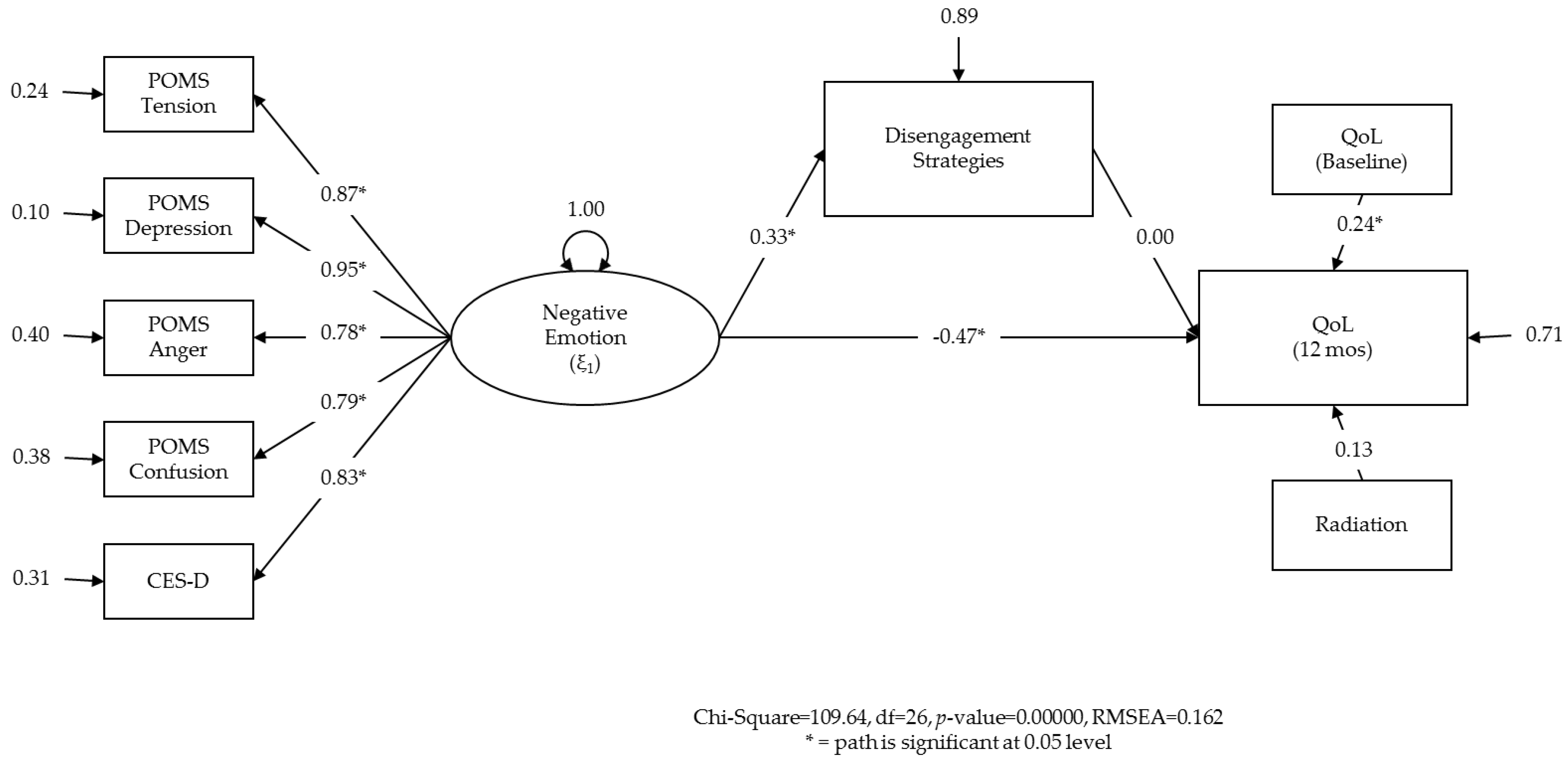
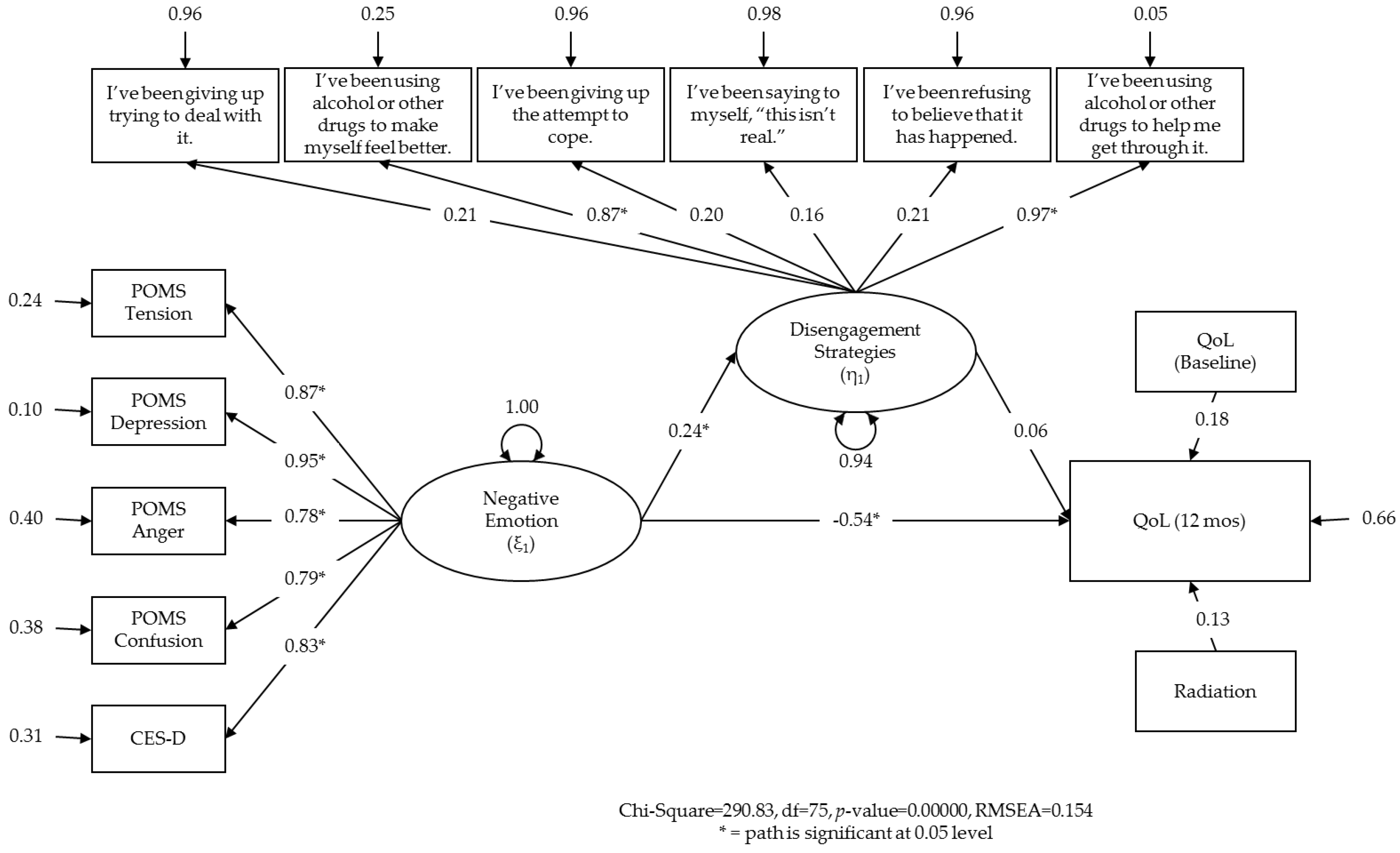
6.2. Results
6.3. Discussion
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ER | emotion regulation |
| QoL | quality of life |
Appendix
| ER Domains | Strategy | Description | Examples |
|---|---|---|---|
| Engagement Strategies | Acceptance | Assent to the reality of a situation, without attempting to change it. | “I’ve been accepting the reality of it.” |
| “I’ve been learning to live with it.” | |||
| Active coping | Taking active steps to remove/circumvent the emotional stimulus or to minimize its effects. | “I’ve been trying to do something about it.” | |
| “I’ve been taking action to improve the situation.” | |||
| Cognitive reappraisal | Construing an emotional stimulus in different terms. Also known as reframing. | “I’ve been trying to see it in a different light.” | |
| “I’ve been looking for the good in the situation.” | |||
| Problem solving | Discovering, analyzing, and finding a solution that best resolves the issue (does NOT include taking active steps toward a solution). | “I’ve been thinking about a strategy for action.” | |
| “I’ve been thinking about what steps to take.” | |||
| Seeking instrumental support | Seeking advice, assistance, or information from others. | “I’ve been getting help and advice from others.” | |
| Disengagement Strategies | Behavioral avoidance | Reducing one’s effort to deal with the emotional stimulus or attain related goals. | “I’ve been giving up trying to deal with it.” |
| “I’ve been giving up the attempt to cope.” | |||
| Cognitive avoidance | Using distraction to prevent oneself from thinking about the emotional stimulus and/or related goals. | “I’ve been trying to take my mind off things.” | |
| “I’ve been doing something to think about it less.” | |||
| Denial | The refusal to accept reality or fact, acting as if an emotional stimulus did not exist. | “I’ve been thinking that this can’t be real.” | |
| “I refuse to believe that it has happened.” | |||
| Substance use | Using drugs or alcohol to disengage from or numb an emotional stimulus. | “I’ve been using alcohol or other drugs to make myself feel better.” | |
| Suppression | Actively trying to put thoughts or feelings about the emotional stimulus out of one’s mind (does NOT include replacing those thoughts with a distractor). | “I tried to put it out of my mind.” | |
| “I tried to avoid thoughts about it.” |
| Scale | Constructs Measured | Number of Items | Internal Consistency | General or Strategies? | Overlap w/Emotions? | Overlap w/Outcomes? |
|---|---|---|---|---|---|---|
| Cognitive Emotion Regulation Questionnaire (CERQ) [57] | Self-blame; Other-blame; Rumination; Catastrophizing; Putting into Perspective; Positive Refocusing; Positive Reappraisal; Acceptance; Refocus on Planning | 36 | Subscales: 0.59–0.84 | Strategies | No | No |
| COPE Inventory [58,59] | Engagement; Disengagement | 60 (Brief = 28) | Subscales: 0.54–0.98 | Strategies | No | No |
| Courtauld Emotional Control Scale (CECS) [55] | Control of Anger; Control of Depressed Mood; Control of Anxiety | 21 | Subscales: 0.79–0.93; Total score: 0.84–0.95 | Both | No | Yes |
| Difficulties in Emotion Regulation Scale (DERS) [56] | Non-acceptance of Emotions; Difficulties in Goal-directed Behavior; Impulse Control; Lack of Emotional Awareness; Limited Emotion Regulation Strategies; Lack of Emotional Clarity | 36 | Subscales: 0.80–0.89; Total score: 0.93 | Both | Yes | Yes |
| Emotion Regulation Questionnaire (ERQ) [61] | Cognitive Reappraisal; Expressive Suppression | 10 | Subscales: 0.68–0.82 | Strategies | No | No |
| Emotional Approach Coping Scale (EACS) [60] | Emotional Expression; Emotional Processing | 8 | Subscales: 0.32–0.93 | Strategies | Yes | No |
| Ways of Coping Questionnaire (WCQ) [121,122] | Expressing Emotion; Suppression; Avoidance; Wishful Thinking; Problem-Solving; Positive Reappraisal; Escapism | 28 | Subscales: 0.80–0.81 | Strategies | Yes | No |
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Soerjomataram, I.; Ervik, M.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide in 2012. Available online: http://globocan.iarc.fr (accessed on 26 May 2016).
- Centers for Disease Control and Prevention. Global Cancer Statistics. 2015. Available online: http://www.cdc.gov/cancer/international/statistics.htm (accessed on 26 May 2016). [Google Scholar]
- Edwards, B.K.; Howe, H.L.; Ries, L.A.; Thun, M.J.; Rosenberg, H.M.; Yancik, R.; Wingo, P.A.; Jemal, A.; Feigal, E.G. Annual report to the nation on the status of cancer, 1973–1999, featuring implications of age and aging on US cancer burden. Cancer 2002, 94, 2766–2792. [Google Scholar] [CrossRef] [PubMed]
- Henselmans, I.; Helgeson, V.S.; Seltman, H.; de Vries, J.; Sanderman, R.; Ranchor, A.V. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol. 2010, 29, 160–168. [Google Scholar] [CrossRef] [PubMed]
- White, K.; D’Abrew, N.; Katris, P.; O’Connor, M.; Emery, L. Mapping the psychosocial and practical support needs of cancer patients in Western Australia. Eur. J. Cancer Care 2012, 21, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Thorne, S.; Hislop, T.G.; Kim-Sing, C.; Oglov, V.; Oliffe, J.L.; Kelli, I. StajduharChanging communication needs and preferences across the cancer care trajectory: Insights from the patient perspective. Support. Care Cancer 2014, 22, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Bultz, B.D.; Carlson, L.E. Emotional distress: The sixth vital sign in cancer care. J. Clin. Oncol. 2005, 23, 6440–6441. [Google Scholar] [CrossRef] [PubMed]
- DiMatteo, M.R.; Lepper, H.S.; Croghan, T.W. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch. Int. Med. 2000, 160, 2101–2107. [Google Scholar] [CrossRef]
- Greer, J.A.; Pirl, W.F.; Park, E.R.; Lynch, T.J.; Jennifer, S. TemelBehavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. J. Psychosom. Res. 2008, 65, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Duberstein, P.R. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797–1810. [Google Scholar] [CrossRef] [PubMed]
- Satin, J.R.; Linden, W.; Phillips, M.J. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer 2009, 115, 5349–5361. [Google Scholar] [CrossRef] [PubMed]
- Andersen, B.L.; Rowland, J.H.; Somerfield, M.R. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. J. Clin. Oncol. 2015, 11, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.J.; Barrett, L.F. Emotion generation and emotion regulation: One or two depends on your point of view. Emot. Rev. 2011, 3, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Burton, C.L. Regulatory flexibility an individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 2013, 8, 591–612. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.J. The emerging field of emotion regulation: An integrative review. Rev. General Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Spencer, S.; Carver, C.S.; Price, A. Psychological and social factors in adaptation. Psycho-Oncol. 1998, 2, 211–222. [Google Scholar]
- Sears, S.R.; Stanton, A.L.; Danoff-Burg, S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol. 2003, 22, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Sanatani, M.; Schreier, G.; Stitt, L. Level and direction of hope in cancer patients: An exploratory longitudinal study. Support. Care Cancer 2008, 16, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.E.; Page, A.E. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs; National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Ness, S.; Kokal, J.; Fee-Schroeder, K.; Novotny, P.; Satele, D.; Barton, D. Concerns across the survivorship trajectory: Results from a survey of cancer survivors. Oncol. Nurs. Forum 2013, 40, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Boyes, A.W.; Girgis, A.; D’Este, C.A.; Zucca, A.C.; Lecathelinais, C.; Carey, M.L. Prevalence and predictors of the short-term trajectory of anxiety and depression in the first year after a cancer diagnosis: A population-based longitudinal study. J. Clin. Oncol. 2013, 31, 2724–2729. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; Vodermaier, A.; MacKenzieb, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Trudel-Fitzgerald, C.; Savard, J.; Ivers, H. Which symptoms come first? Exploration of temporal relationships between cancer-related symptoms over an 18-month period. Ann. Behav. Med. 2013, 45, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Neilson, K.; Pollard, A.; Boonzaier, A.; Corry, J.; Castle, D.; Smith, D.; Trauer, T.; Couper, J. A longitudinal study of distress (depression and anxiety) up to 18 months after radiotherapy for head and neck cancer. Psycho-Oncol. 2013, 22, 1843–1848. [Google Scholar] [CrossRef] [PubMed]
- Mantegna, G.; Petrillo, M.; Fuoco, G.; Venditti, L.; Terzano, S.; Anchora, L.P.; Scambia, G.; Ferrandina, G. Long-term prospective longitudinal evaluation of emotional distress and quality of life in cervical cancer patients who remained disease-free 2-years from diagnosis. BMC Cancer 2013. [Google Scholar] [CrossRef] [PubMed]
- Ferrandina, G.; Petrillo, M.; Mantegna, G.; Fuoco, G.; Terzano, S.; Venditti, L.; Marcellusi, A.; De Vincenzo, R.; Scambia, G. Evaluation of quality of life and emotional distress in endometrial cancer patients: A 2-year prospective, longitudinal study. Gynecol. Oncol. 2014, 133, 518–525. [Google Scholar] [PubMed]
- Punnen, S.; Cowan, J.E.; Dunn, L.B.; Shumay, D.M.; Carroll, P.R.; Cooperberg, M.R. A longitudinal study of anxiety, depression and distress as predictors of sexual and urinary quality of life in men with prostate cancer. BJU Int. 2013, 112, E67–E75. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Int. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Schroevers, M.; Ranchor, A.V.; Sanderman, R. Adjustment to cancer in the 8 years following diagnosis: A longitudinal study comparing cancer survivors with healthy individuals. Soc. Sci. Med. 2006, 63, 598–610. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. State-Trait Anxiety Inventory (Self-Evaluation Questionnaire); Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Avis, N.E.; Levine, B.; Naughton, M.J.; Case, L.D.; Naftalis, E.; Van Zee, K.J. Age-related longitudinal changes in depressive symptoms following breast cancer diagnosis and treatment. Breast Cancer Res. Treat. 2013, 139, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Burgess, C.; Cornelius, V.; Love, S.; Graham, J.; Richards, M.; Ramirez, A. Depression and anxiety in women with early breast cancer: Five year observational cohort study. Br. Med. J. 2005, 330, 702–705. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; MacKenzie, R.; Rnic, K.; Marshall, C.; Vodermaier, A. Emotional adjustment over 1 year post-diagnosis in patients with cancer: Understanding and predicting adjustment trajectories. Support. Care Cancer 2015, 23, 1391–1399. [Google Scholar] [CrossRef] [PubMed]
- Andersen, B.; Goyal, N.G.; Westbrook, T.D.; Bishop, B.; Carson, W.E. Trajectories of stress, depressive symptoms, and immunity in cancer survivors: Diagnosis to 5 years. Clin. Cancer Res. 2016, 22. [Google Scholar] [CrossRef] [PubMed]
- Stanton, A.L. Psychosocial concerns and interventions for cancer survivors. J. Clin. Oncol. 2006, 24, 5132–5137. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef]
- Stanton, A.L. What happens now? Psychosocial care for cancer survivors after medical treatment completion. J. Clin. Oncol. 2012, 30, 1215–1220. [Google Scholar] [CrossRef] [PubMed]
- Vodermaier, A.; Linden, W.; McKenzie, R.; Greig, D.; Marshall, C. Post-diagnosis anxiety and depression: Contribution of disease stage and cancer site in four common types of cancer. Br. J. Cancer 2011, 105, 1814–1817. [Google Scholar] [CrossRef] [PubMed]
- Helgeson, V.S.; Snyder, P.; Seltman, H. Psychological and physical adjustment to breast cancer over 4 years: Identifying distinct trajectories of change. Health Psychol. 2004, 23, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.A. Emotion regulation: A theme in search of definition. Monogr. Soc. Res. Child Dev. 1994, 59, 25–52. [Google Scholar] [CrossRef] [PubMed]
- Kappas, A. Emotion and regulation are one! Emot. Rev. 2011, 3, 17–25. [Google Scholar] [CrossRef]
- Lewis, A.R.; Zinbarg, R.E.; Durbin, C.E. Advances, problems, and challenges in the study of emotion regulation: A commentary. J. Psychopathol. Behav. Assess. 2010, 32, 83–91. [Google Scholar] [CrossRef]
- Thompson, R.A. Emotion and emotion regulation: Two sides of the developing coin. Emot. Rev. 2011, 3, 53–61. [Google Scholar] [CrossRef]
- Cisler, J.M.; Olatunji, B.O.; Feldner, M.T.; Forsyth, J.P. Emotion regulation and the anxiety disorders: An integrative review. J. Psychopathol. Behav. Assess. 2010, 32, 68–82. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Miles, E.; Sheeran, P. Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychol. Bull. 2012, 138, 775–808. [Google Scholar] [CrossRef] [PubMed]
- Kershaw, T.; Northouse, L.; Kritpracha, C.; Schafenacker, A.; Mood, D. Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol. Health 2004, 19, 139–155. [Google Scholar] [CrossRef]
- Perczek, R.E.; Burke, M.A.; Carver, C.S.; Krongrad, A.; Terris, M.K. Facing a prostate cancer diagnosis: Who is at risk for increased distress? Cancer 2002, 94, 2923–2929. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.-C.; Brothers, B.M.; Andersen, B.L. Stress and quality of life in breast cancer recurrence: Moderation or mediation of coping? Ann. Behav. Med. 2008, 35, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Bridges, L.J.; Denham, S.A.; Ganiban, J.M. Definitional issues in emotion regulation research. Child Dev. 2004, 75, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Treynor, W.; Gonzalez, R.; Nolen-Hoeksema, S. Rumination reconsidered: A psychometric analysis. Cogn. Ther. Res. 2003, 27, 247–259. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Brandão, T.; Tavares, R.; Schulz, M.S.; Matos, P.M. Measuring emotion regulation and emotional expression in breast cancer patients: A systematic review. Clin. Psychol. Rev. 2016, 43, 114–127. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.; Greer, S. Development of a questionnaire measure of emotional control. J. Psychosom. Res. 1983, 27, 299–305. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Garnefski, N.; Kraaij, V. The cognitive emotion regulation questionnaire. Eur. J. Psychol. Assess. 2007, 23, 141–149. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Stanton, A.L.; Kirk, S.B.; Cameron, C.L.; Danoff-Burg, S. Coping through emotional approach: Scale construction and validation. J. Personal. Soc. Psychol. 2000, 78, 1150–1169. [Google Scholar] [CrossRef]
- Gross, J.J.; John, O.P. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J. Personal. Soc. Psychol. 2003, 85, 348–362. [Google Scholar] [CrossRef]
- Robinson, M.D.; Clore, G.L. Episodic and semantic knowledge in emotional self-report: Evidence for two judgment processes. J. Personal. Soc. Psychol. 2002, 83, 198–215. [Google Scholar] [CrossRef]
- John, O.P.; Gross, J.J. Individual differences in emotion regulation. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007; pp. 351–372. [Google Scholar]
- Karademas, E.C.; Tsalikou, C.; Tallarou, M.-C. The impact of emotion regulation and illness-focused coping strategies on the relation of illness-related negative emotions to subjective health. J. Health Psychol. 2011, 16, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Wisco, B.E.; Lyubomirsky, S. Rethinking rumination. Perspect. Psychol. Sci. 2008, 3, 400–424. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.J.; Thompson, R.A. Emotion regulation: Conceptual foundations. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Mor, N.; Winquist, J. Self-focused attention and negative affect: A meta-analysis. Psychol. Bull. 2002, 128, 638–662. [Google Scholar] [CrossRef] [PubMed]
- Watkins, E. Appraisals and strategies associated with rumination and worry. Personal. Individ. Differ. 2004, 37, 679–694. [Google Scholar] [CrossRef]
- Abramowitz, J.S.; Tolin, D.F.; Street, G.P. Paradoxical effects of thought suppression: A meta-analysis of controlled studies. Clin. Psychol. Rev. 2001, 21, 683–703. [Google Scholar] [CrossRef]
- Demaree, H.A.; Robinson, J.L.; Pu, J.; Allen, J.J.B. Strategies actually employed during response-focused emotion regulation research: Affective and physiological consequences. Cogn. Emot. 2006, 20, 1248–1260. [Google Scholar] [CrossRef]
- John, O.P.; Gross, J.J. Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. J. Personal. 2004, 72, 1301–1334. [Google Scholar] [CrossRef] [PubMed]
- Goldin, P.R.; McRae, K.; Ramel, W.; Gross, J.J. The neural bases of emotion regulation: Reappraisal and suppression of negative emotion. Biolog. Psychiatry 2008, 63, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Mennin, D.S.; Holaway, R.M.; Fresco, D.M.; Moore, M.T.; Heimberg, R.G. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behav. Ther. 2007, 38, 284–302. [Google Scholar] [CrossRef] [PubMed]
- DeSteno, D.; Gross, J.J.; Kubzansky, L. Affective science and health: The importance of emotion and emotion regulation. Health Psychol. 2013, 32, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Giese-Davis, J.; Conrad, A.; Nouriani, B.; Spiegel, D. Exploring emotion-regulation and autonomic physiology in metastatic breast cancer patients: Repression, suppression, and restraint of hostility. Personal. Individ. Differ. 2008, 44, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.E.; Stanton, A.L. Coping resources, coping processes, and mental health. Annu. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Strosahl, K.; Wilson, K.G. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; Guilford Press: New York, NY, USA, 1999; p. 304. [Google Scholar]
- Campbell-Sills, L.; Barlow, D.H.; Brown, T.A.; Hofmann, S.G. Effects of suppression and acceptance on emotional responses of individuals with anxiety and mood disorders. Behav. Res. Ther. 2006, 44, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Bruehl, S.; Burns, J.W.; Chung, O.Y.; Quartana, P. Anger management style and emotional reactivity to noxious stimuli among chronic pain patients and healthy controls: The role of endogenous opioids. Health Psychol. 2008, 27, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, M.A.; Stanton, A.L.; Bower, J.E.; Thomas, K.S.; Litwin, M.S.; Breen, E.C.; Irwin, M.R. Inflammatory biomarkers and emotional approach coping in men with prostate cancer. Brain Behav. Immun. 2013, 32, 173–179. [Google Scholar] [CrossRef] [PubMed]
- McKenna, M.C.; Zevon, M.A.; Corn, B.; Rounds, J. Psychosocial factors and the development of breast cancer: A meta-analysis. Health Psychol. 1999, 18, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, D.; Kato, P.M. Psychosocial influences on cancer incidence and progression. Harv. Rev. Psychiatry 1996, 4, 10–26. [Google Scholar] [CrossRef] [PubMed]
- Tamagawa, R.; Giese-Davis, J.; Speca, M.; Doll, R.; Stephen, J.; Carlson, L.E. Trait mindfulness, repression, suppression, and self-reported mood and stress symptoms among women with breast cancer. J. Clin. Psychol. 2013, 69, 264–277. [Google Scholar] [CrossRef] [PubMed]
- Van Middendorp, H.; Lumley, M.A.; Jacobs, J.W.G.; van Doornen, L.J.P.; Bijlsma, J.W.J.; Geenen, R. Emotions and emotional approach and avoidance strategies in fibromyalgia. J. Psychosom. Res. 2008, 64, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Stanton, A.L.; Danoff-Burg, S.; Cameron, C.L.; Bishop, M.; Collins, C.A.; Kirk, S.B.; Sworowski, L.A.; Twillman, R. Emotionally expressive coping predicts psychological and physical adjustmen to breast cancer. J. Consult. Clin. Psychol. 2000, 68, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Stanton, A.L.; Danoff-Burg, S.; Sworowski, L.A.; Collins, C.A.; Branstetter, A.D.; Rodriguez-Hanley, A.; Kirk, S.B.; Austenfeld, J.L. Randomized, Controlled Trial of Written Emotional Expression and Benefit Finding in Breast Cancer Patients. J. Clin. Oncol. 2002, 20, 4160–4168. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A. The future of emotion regulation research capturing context. Perspect. Psychol. Sci. 2013, 8, 155–172. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.A.; Green, P.A.; Barrett, L.F. Affective Science Perspectives on Cancer Control Strategically Crafting a Mutually Beneficial Research Agenda. Perspect. Psychol. Sci. 2015, 10, 328–345. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhu, X.; Yang, Y.; He, J.; Yi, J.; Wang, Y.; Zhang, J. Cognitive emotion regulation: Characteristics and effect on quality of life in women with breast cancer. Health Qual. Life Outcomes 2015. [Google Scholar] [CrossRef] [PubMed]
- Classen, C.; Koopman, C.; Angell, K.; Spiegel, D. Coping styles associated with psychological adjustment to advanced breast cancer. Health Psychol. 1996, 15, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Iwamitsu, Y.; Shimoda, K.; Abe, H.; Tani, T.; Okawa, M.; Buck, R. Anxiety, emotional suppression, and psychological distress before and after breast cancer diagnosis. Psychosomatics 2005, 46, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Iwamitsu, Y.; Shimoda, K.; Abe, H.; Tani, T.; Okawa, M.; Buck, R. The relation between negative emotional suppression and emotional distress in breast cancer diagnosis and treatment. Health Commun. 2005, 18, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, M.A.; Goldstein, B.A. Not all negative emotions are equal: The role of emotional expression in online support groups for women with breast cancer. Psycho-Oncol. 2006, 15, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Low, C.A.; Stanton, A.L.; Danoff-Burg, S. Expressive disclosure and benefit finding among breast cancer patients: Mechanisms for positive health effects. Health Psychol. 2006, 25, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Schroevers, M.; Kraaij, V.; Garnefski, N. How do cancer patients manage unattainable personal goals and regulate their emotions. Br. J. Health Psychol. 2008, 13, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yi, J.; He, J.; Chen, G.; Li, L.; Yang, Y.; Zhu, X. Cognitive emotion regulation strategies as predictors of depressive symptoms in women newly diagnosed with breast cancer. Psycho-Oncol. 2014, 23, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Leroy, T.; Christophe, V.; Antoine, P.; Nandrino, J.L. Difficulties in emotion regulation and emotional distress in cancer patients. Psychol. Health 2012. [Google Scholar] [CrossRef] [Green Version]
- Peh, C.X.; Kua, E.H.; Mahendran, R. Hope, emotion regulation, and psychosocial well-being in patients newly diagnosed with cancer. Support. Care Cancer 2016, 24, 1955–1962. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S.E.; Berenbaum, H. Are Specific Emotion Regulation Strategies Differentially Associated with Posttraumatic Growth Versus Stress? J. Aggress. Maltreat. Trauma 2015, 24, 794–808. [Google Scholar] [CrossRef]
- Alvarez, I.; Leal, I. Cognitive emotion regulation predicting posttraumatic stress and posttraumatic growth in breast cancer survivors. Psychol. Health 2010. [Google Scholar] [CrossRef]
- Smyth, J.M.; Arigo, D. Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Curr. Opin. Psychiatry 2009, 22, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Austenfeld, J.L.; Stanton, A.L. Coping through emotional approach: A new look at emotion, coping, and health-related outcomes. J. Personal. 2004, 72, 1335–1364. [Google Scholar] [CrossRef] [PubMed]
- Reed, R.G.; Weihs, K.L.; Sbarra, D.A.; Breen, E.C.; Irwin, M.R.; Butler, E.A. Emotional acceptance, inflammation, and sickness symptoms across the first two years following breast cancer diagnosis. Brain Behav. Immun. 2016, 56, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.P.; Fiscella, K.; Kawachi, I.; Duberstein, P.; Muennig, P. Emotion suppression and mortality risk over a 12-year follow-up. J. Psychosom. Res. 2013, 75, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Andersen, B.L.; Shapiro, C.L.; Farrar, W.B.; Crespin, T. Sharla Wells-DiGregorio Psychological responses to cancer recurrence: A controlled prospective study. Cancer 2005, 104, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.C.; Thornton, L.M.; Shapiro, C.L.; Andersen, B.L. Surviving recurrence: Psychological and quality of life recovery. Cancer 2008, 112, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Stanton, A.L.; Low, C.A. Dispositional and stressor-related emotion regulation in the context of a chronic, life-limiting stressor. J. Personal. 2012, 80, 287–311. [Google Scholar] [CrossRef] [PubMed]
- Northouse, L.L.; Mood, D.; Kershaw, T.; Schafenacker, A.; Mellon, S.; Walker, J.; Galvin, E.; Decker, V. Quality of life of women with recurrent breast cancer and their family members. J. Clin. Oncol. 2002, 20, 4050–4064. [Google Scholar] [CrossRef] [PubMed]
- Andersen, B.L.; Farrar, W.B.; Golden-Kreutz, D.M.; Glaser, R.; Emery, C.F.; Crespin, T.R.; Shapiro, C.L.; Carson, W.E., 3rd. Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. J. Clin. Oncol. 2004, 22, 3570–3580. [Google Scholar] [CrossRef] [PubMed]
- Shacham, S. A shortened version of the Profile of Mood States. J. Personal. Assess. 1983, 47, 305–306. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. Sociol. Methods Res. 1992, 21, 230–258. [Google Scholar] [CrossRef]
- Cliff, N. Some cautions concerning the application of causal modeling methods. Multivar. Behav. Res. 1983, 18, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Britton, P.C. The relation of coping strategies to alcohol consumption and alcohol-related consequences in a college sample. Addict. Res. Theory 2004, 12, 103–114. [Google Scholar] [CrossRef]
- Hong, R.Y. Worry and rumination: Differential associations with anxious and depressive symptoms and coping behavior. Behav. Res. Ther. 2007, 45, 277–290. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Aldao, A. Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personal. Individ. Differ. 2011, 51, 704–708. [Google Scholar] [CrossRef]
- Schmidt, S.; Tinti, C.; Levine, L.J.; Testa, S. Appraisals, emotions and emotion regulation: An integrative approach. Motiv. Emot. 2010, 34, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Markey, M.A.; Vander Wal, J.S. The role of emotional intelligence and negative affect in bulimic symptomatology. Compr. Psychiatry 2007, 48, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Lazarus, R.S. An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 1980, 21, 219–239. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, P.; Hurley, S.; Torres, M.; Jackson, J.; Boyd, P.; Chen, V.W. Use of coping strategies and breast cancer survival: Results from The Black/White Cancer Survival Study. Am. J. Epidemiol. 2000, 152, 940–949. [Google Scholar] [CrossRef] [PubMed]

| Measure | α | Baseline | Baseline Correlations | 4 Months | 12 Months | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Engagement | Disengagement | SF-36 MCS | Mean (SD) | Range | Mean (SD) | Range | ||
| POMS | ||||||||||
| Tension | 0.89 | 6.83 (4.81) | 0–23 | −0.11 | −0.41 * | −0.57 * | ||||
| Depression | 0.93 | 6.21 (6.07) | 0–27 | −0.00 | −0.48 * | −0.64 * | ||||
| Anger | 0.92 | 4.59 (4.54) | 0–28 | −0.07 | −0.39 * | −0.42 * | ||||
| Confusion | 0.84 | 4.43 (3.47) | 0–19 | −0.09 | −0.36 * | −0.57 * | ||||
| CES-D | 0.92 | 13.56 (9.60) | 0–45 | −0.09 | −0.38 * | −0.68 * | ||||
| Engagement | 0.86 | 1 | −0.10 * | −0.08 * | 3.02 (1.25) | 0.25–5.75 | ||||
| Disengagement | 0.71 | 1 | −0.17 * | 0.36 (0.60) | 0–2.67 | |||||
| SF-36 MCS | 0.88 | 1 | 50.32 (9.85) | 24.04–63.08 | ||||||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conley, C.C.; Bishop, B.T.; Andersen, B.L. Emotions and Emotion Regulation in Breast Cancer Survivorship. Healthcare 2016, 4, 56. https://doi.org/10.3390/healthcare4030056
Conley CC, Bishop BT, Andersen BL. Emotions and Emotion Regulation in Breast Cancer Survivorship. Healthcare. 2016; 4(3):56. https://doi.org/10.3390/healthcare4030056
Chicago/Turabian StyleConley, Claire C., Brenden T. Bishop, and Barbara L. Andersen. 2016. "Emotions and Emotion Regulation in Breast Cancer Survivorship" Healthcare 4, no. 3: 56. https://doi.org/10.3390/healthcare4030056





