Breast Cancer: Exploring the Facts and Holistic Needs during and beyond Treatment
Abstract
:1. Epidemiology and Classification of Breast Cancer
2. Diagnosis and Treatment
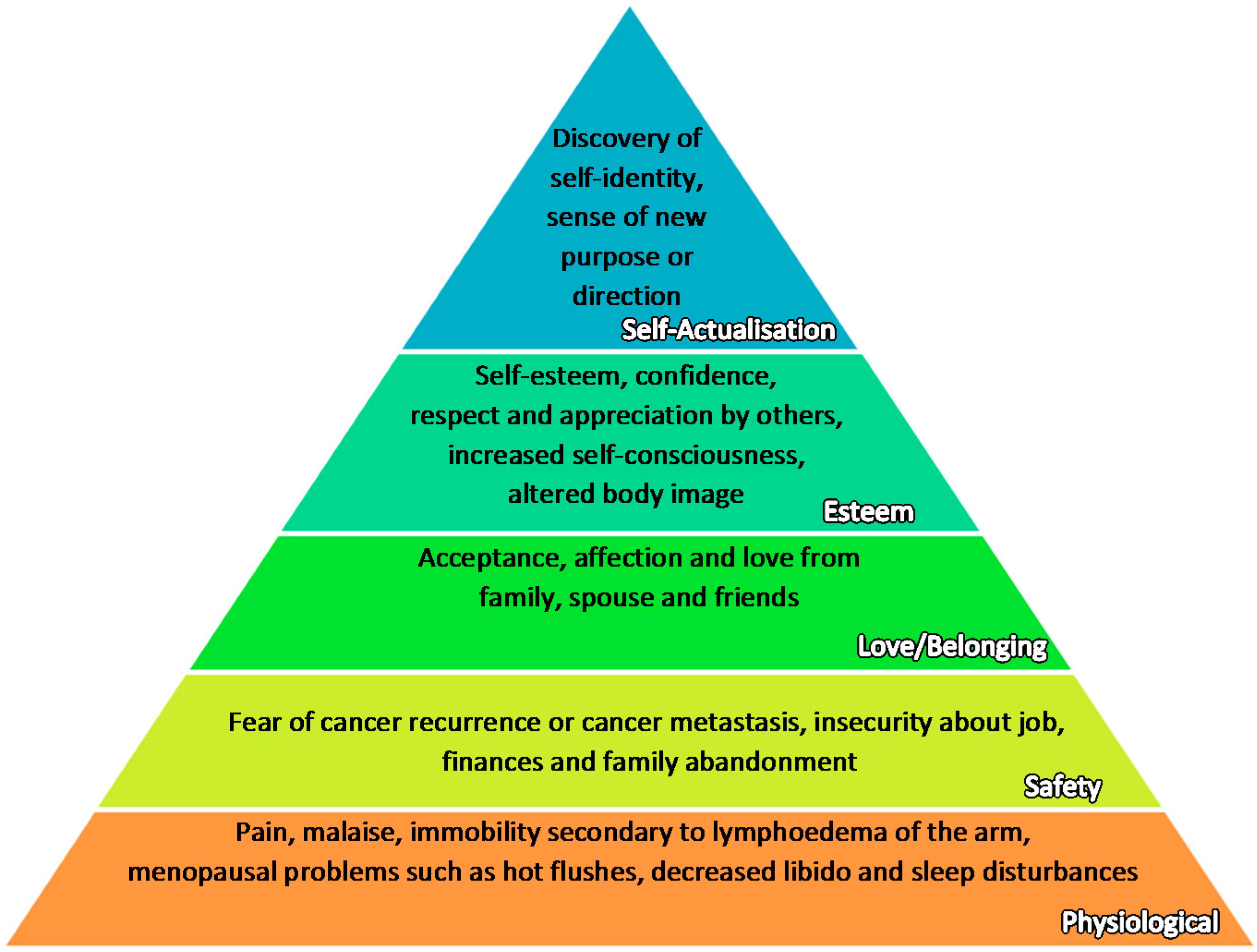
3. Holistic Needs
4. Holistic Needs at Time of Diagnosis
5. Holistic Needs during Treatment
5.1. Managing Physical Side Effects
5.1.1. Professional Advice from Cancer Care Team
5.1.2. Exercises
5.1.3. Complementary Medicine
5.2. Managing Psychological Stresses
5.2.1. Social Support
5.2.2. Spiritual Care
5.2.3. Recreation
6. Holistic Needs after Treatment
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global Cancer Incidence and Mortality Rates and Trends—An Update. Cancer J. Clin. 2016, 65, 87–108. [Google Scholar] [CrossRef]
- Population Reference Bureau. 2008 World Population Data Sheet. 2008, p. 7. Available online: http://www.prb.org/pdf08/08WPDS_Eng.pdf (accessed on 16 March 2017).
- Population Reference Bureau. 2012 World Population Data Sheet. 2012, p. 6. Available online: http://www.prb.org/pdf12/2012-population-data-sheet_eng.pdf (accessed on 16 March 2017).
- National Registry of Diseases Office, Health Promotion Board. Singapore Cancer Registry Interim Annual Report Trends in Cancer Incidence in Singapore 2010–2014. 2015; p. 8. Available online: https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/cancer-trends-2010-2014_interim-annual-report_final-(public)_220615.pdf?sfvrsn=0 (accessed on 14 January 2017).
- Tao, Z.; Shi, A.; Lu, C.; Song, T.; Zhang, Z.; Zhao, J. BC: Epidemiology and etiology. Cell Biochem. Biophys. 2015, 72, 333–338. [Google Scholar] [CrossRef]
- World Health Organization. NCD Mortality and Morbidity. Available online: http://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed on 16 March 2017).
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010. 2010, p. 9. Available online: http://www.who.int/nmh/publications/ncd_report_full_en.pdf (accessed on 16 March 2017).
- Singletary, S.E. Rating the risk factors for BC. Ann. Surg. 2003, 237, 474–482. [Google Scholar] [CrossRef]
- McPherson, K.; Steel, C.; Dixon, J.M. BC—Epidemiology, risk factors, and genetics. BMJ 2003, 321, 624–628. [Google Scholar] [CrossRef]
- Verma, R.; Bowen, R.L.; Slater, S.E.; Mihaimeed, F.; Jones, J.L. Pathological and epidemiological factors associated with advanced stage at diagnosis of BC. Br. Med. Bull. 2012, 103, 129–145. [Google Scholar] [CrossRef]
- Wu, L.; Wang, F.; Xu, R.; Zhang, S.; Peng, X.; Feng, Y.; Wang, J.; Lu, C. Promoter methylation of BRCA1 in the prognosis of BC: A meta-analysis. BC Res. Treat. 2013, 142, 619–627. [Google Scholar] [CrossRef]
- Antoniou, A.; Pharoah, P.D.P.; Narod, S.; Risch, H.A.; Eyfjord, J.E.; Hopper, J.L.; Loman, N.; Olsson, H.; Johannsson, O.; Borg, Å.; et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: A combined analysis of 22 studies. Am. J. Hum. Genet. 2003, 72, 1117–1130. [Google Scholar] [CrossRef]
- Ford, D.; Easton, D.F.; Stratton, M.; Narod, S.; Goldgar, D.; Devilee, P.; Bishop, D.T.; Weber, B.; Lenoir, G.; Chang-Claude, J.; et al. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in BC families. Am. J. Hum. Genet. 1998, 62, 676–689. [Google Scholar] [CrossRef]
- Brenton, J.D.; Carey, L.A.; Ahmed, A.A.; Caldas, C. Molecular classification and molecular forecasting of BC: Ready for clinical application? J. Clin. Oncol. 2005, 23, 7350–7360. [Google Scholar] [CrossRef]
- Malhotra, G.K.; Zhao, X.; Band, H.; Band, V. Histological, molecular and functional subtypes of BCs. Cancer Boil. Ther. 2010, 10, 955–960. [Google Scholar] [CrossRef]
- Shah, R.; Rosso, K.; Nathanson, S.D. Pathogenesis, prevention, diagnosis and treatment of BC. World J. Clin. Oncol. 2014, 5, 283–298. [Google Scholar] [CrossRef]
- Liu, S.V.; Melstrom, L.; Yao, K.; Russell, C.A.; Sener, S.F. Neoadjuvant therapy for breast cancer. J. Surg. Oncol. 2010, 101, 283–291. [Google Scholar] [CrossRef]
- Yeo, B.; Turner, N.C.; Jones, A. An update on the medical management of breast cancer. BMJ 2014, 348, g3608. [Google Scholar] [CrossRef]
- Zalenski, R.J.; Raspa, R. Maslow’s Hierarchy of Needs: A Framework for Achieving Human Potential in Hospice. J. Palliat. Med. 2006, 9, 1120–1127. [Google Scholar] [CrossRef]
- Adler, N.E.; Page, A.E.K. Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting; Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. In The Psychosocial Needs of Cancer Patients, 1st ed.; National Academies Press: Washington, DC, USA, 2008; Available online: https://www.ncbi.nlm.nih.gov/books/NBK4011/ (accessed on 14 November 2016).
- Schmid-Büchi, S.; Halfens, R.J.; Dassen, T.; Van Den Borne, B. A review of psychosocial needs of breast-cancer patients and their relatives. J. Clin. Nurs. 2008, 17, 2895–2909. [Google Scholar] [CrossRef]
- Ho, G.H.; Tan, B.L. Implementing Breast Cancer Survivorship Programme. In Proceedings of the 3rd Regional Oncology Nursing Conference, Singapore, 18 January 2013; Available online: https://www.nccs.com.sg/documents/ronc/conference_slides/Con_17Jan_Breast_Care_Survivorship_Programme_NCCS.pdf (accessed on 18 December 2016).
- The NCCS Definition of a “Cancer Survivor”. Available online: https://www.canceradvocacy.org/news/defining-cancer-survivorship/ (accessed on 14 November 2016).
- Fields, D. Slaying the Cancer Giant with the Word of God: An Autobiography of a Cancer Survivor, 1st ed.; WestBow Press: Bloomington, IN, USA, 2012; p. 119. [Google Scholar]
- Benson, J.; Gui, G.; Tuttle, T. Early Breast Cancer: From Screening to Multidisciplinary Management, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2012; p. 326. [Google Scholar]
- Cancer Action Team. Holistic Common Assessment of Supportive and Palliative Care Needs for Adults with Cancer: Assessment Guidance. Available online: http://www.birminghamcancer.nhs.uk/uploads/document_file/document/4d9452b9358e9858ab0029b2/finalprintedreportguidancerevisedholisticcommonassessmentfinal_1_.pdf (accessed on 28 December 2016).
- Levit, L.A.; Balogh, E.P.; Nass, S.J.; Ganz, P.A. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis, 1st ed.; National Academies Press: Washington, DC, USA, 2013; pp. 7–8. Available online: https://www.nap.edu/read/18359/chapter/1 (accessed on 29 December 2016).
- Redman, S.; Turner, J.; Davis, C. Improving supportive care for women with breast cancer in Australia: The challenge of modifying health systems. Psycho-Oncology 2003, 12, 521–531. [Google Scholar] [CrossRef]
- Taylor, C.; Shewbridge, A.; Harris, J.; Green, J.S. Benefits of multidisciplinary teamwork in the management of breast cancer. Breast Cancer Targets Ther. 2013, 5, 79–85. [Google Scholar] [CrossRef]
- Breast Cancer Specialists & Doctors, Swedish Medical Center Seattle and Issaquah. Available online: http://www.swedish.org/services/cancer-institute/cancer-types/breast-cancer/our-providers (accessed on 1 April 2017).
- The Cancer Institute Hospital of JFCR. Available online: http://www.jfcr.or.jp/hospital-en/department/breast/ (accessed on 1 April 2017).
- Singapore General Hospital. Breast Care. 2016. Available online: https://www.sgh.com.sg/clinical-departments-centers/nursing/nursing-specialities/pages/breast-care.aspx (accessed on 28 December 2016).
- Institute of Medicine (US); National Research Council (US) National Cancer Policy Board; Hewitt, M.; Herdman, R.; Holland, J. (Eds.) Meeting Psychosocial Needs of Women with Breast Cancer; The Effectiveness of Psychosocial Interventions for Women with Breast Cancer; National Academies Press: Washington, DC, USA, 2004; pp. 95–105. [Google Scholar]
- Institute of Medicine. Implementing Cancer Survivorship Care Planning; The National Academies Press: Washington, DC, USA, 2007; Available online: https://www.nap.edu/read/11739/chapter/1 (accessed on 29 December 2016).
- NUS News. Cancer Survivorship Programme Shows Promise. 2016. Available online: https://news.nus.edu.sg/highlights/10465-cancer-survivorship-programme-shows-promise (accessed on 27 December 2016).
- Singhealth. Cancer Survivorship Programme Proves Beneficial for Patients. 2016. Available online: https://www.singhealth.com.sg/TomorrowsMed/Article/Pages/Cancersurvivorshipprogrammeprovesbeneficialforpatients.aspx (accessed on 14 November 2016).
- Kübler-Ross, E. On Death and Dying; Macmillan: New York, NY, USA, 1969. [Google Scholar]
- Charmaz, K. Experiencing chronic illness. In Handbook of Social Studies in Health and Medicine; Albrecht, G.L., Fitzpatrick, R., Scrimshaw, S.C., Eds.; Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Stanton, A.L.; Collins, C.A.; Sworowski, L.A. Adjustment to chronic illness: Theory and research. In Handbook of Health Psychology; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2001. [Google Scholar]
- Kirkpatrick, C. Nurses’ Guide to Cancer Care, 1st ed.; Rowman & Littlefield: Totowa, NJ, USA, 1986; p. 136. [Google Scholar]
- Cancer Research UK. Coping with Cancer. 2016. Available online: http://www.cancerresearchuk.org/about-cancer/coping-with-cancer/coping-emotionally/cancer-and-your-emotions/ (accessed on 28 December 2016).
- Bertero, C.M.; Wilmoth, M.C. Breast cancer diagnosis in its treatment affecting the self: A meta-synthesis. Cancer Nurs. 2007, 30, 194–202. [Google Scholar] [CrossRef]
- Lam, W.W.T.; Fielding, R. The evolving experience of illness for Chinese women with breast cancer: A qualitative study. Psycho-Oncology 2003, 12, 127–140. [Google Scholar] [CrossRef]
- Lund-Nielsen, B.; Muller, K.; Adamsen, L. Malignant wounds in women with breast cancer: Feminine and sexual perspectives. J. Cancer Nur. 2005, 14, 56–64. [Google Scholar] [CrossRef]
- Segrin, C.; Badger, T.A.; Meek, P.; Lopez, A.M.; Bonham, E.; Sieger, A. Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. J. Soc. Pers. Relatsh. 2005, 22, 673–689. [Google Scholar] [CrossRef]
- Emanuel, L.; Ferris, F.D.; von Gunten, C.F.; Von Roenn, J.H. Cancer Survivorship: Role of Healthcare Providers. Medscape, 2010. Available online: http://www.medscape.com/viewarticle/728448_8 (accessed on 27 December 2016).
- Miller, R. Implementing a survivorship care plan for patients with breast cancer. Clin. J. Oncol. Nurs. 2008, 12, 479–487. Available online: go.galegroup.com.libproxy1.nus.edu.sg/ps/i.do?p=AONE&sw=w&u=nuslib&v=2.1&it=r&id=GALE%7CA179978701&sid=summon&asid=6cfdb704ffbf8e31f80d76f2493e9317 (accessed on 27 December 2016).
- Day, S.; Bevers, T.; Palos, G.; Rodriguez, M. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. Breast Dis. A Year Book Q. 2016, 27, 327–329. [Google Scholar] [CrossRef]
- Yong, F. Breast Cancer, 1st ed.; National Cancer Centre Singapore: Singapore, 2016; pp. 15–16. Available online: https://www.nccs.com.sg/Publications/CancerInformationBooklets/CancerType/Documents/NCCS_BreastCancer_Eng.pdf (accessed on 14 November 2016).
- Smith, K.B.; Pukall, C.F. An evidence based review of yoga as a complementary intervention for patients with cancer. Psycho-Oncology 2009, 18, 465–475. [Google Scholar] [CrossRef]
- Pinto, B.; Maruyama, N. Exercise in the rehabilitation of breast cancer survivors. Psycho-Oncology 1999, 8, 191–206. [Google Scholar] [CrossRef]
- Chow, W.H.; Chang, P.; Shen, H.M.; Verkooijen, H.M.; Lee, S.C.; Wong, A. Complementary and alternative medicine among Singapore cancer patients. Ann. Acad. Med. Singap. 2010, 39, 129–135. [Google Scholar]
- Li, X.; Yang, G.; Li, X.; Zhang, Y.; Yang, J.; Chang, J.; Sun, X.; Zhou, X.; Guo, Y.; Xu, Y. Traditional Chinese Medicine in Cancer Care: A Review of Controlled Clinical Studies Published in Chinese. PLoS ONE 2013, 8, e60338. [Google Scholar] [CrossRef]
- National Cancer Institute. Annual Costs of Cancer Care|Cancer Prevalence and Cost of Care Projections. 2016. Available online: https://costprojections.cancer.gov/annual.costs.html (accessed on 14 November 2016).
- Trusson, D.; Pilnick, A. The Role of Hair Loss in Cancer Identity: Perceptions of Chemotherapy-Induced Alopecia Among Women Treated for Early-Stage Breast Cancer or Ductal Carcinoma in Situ. Cancer Nurs. 2017, 40, E9–E16. [Google Scholar] [CrossRef]
- Watson, M.; Denton, S.; Baum, M.; Greer, S. Counselling breast cancer patients: A specialist nurse service. Couns. Psychol. Q. 2007, 1, 25–34. [Google Scholar] [CrossRef]
- Ell, K.; Nishimoto, R.; Mediansky, L.; Mantell, J.; Hamovitch, M. Social relations, social support and survival among patients with cancer. J. Psychosom. Res. 1992, 36, 531–541. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- American Society of Clinical Oncology. Tips for Caregiving. 2016. Available online: http://www.cancer.net/coping-with-cancer/caring-loved-one/tips-caregiving (accessed on 27 December 2016).
- Weaver, A.; Flannelly, K. The Role of Religion/Spirituality for Cancer Patients and Their Caregivers. South. Med. J. 2004, 97, 1210–1214. [Google Scholar] [CrossRef]
- Friedli, K.; King, M. Psychological support for patients having breast cancer surgery. BMJ 1996, 313, 360–361. [Google Scholar] [CrossRef]
- Puig, A.; Lee, S.; Goodwin, L.; Sherrard, P. The efficacy of creative arts therapies to enhance emotional expression, spirituality, and psychological well-being of newly diagnosed Stage I and Stage II breast cancer patients: A preliminary study. Arts Psychother. 2006, 33, 218–228. [Google Scholar] [CrossRef]
- Paice, J.; Nainis, N.; Ratner, J.; Wirth, J.; Lai, J. Relieving symptoms in cancer: Innovative use of expressive art therapy. J. Pain 2005, 6, S59. [Google Scholar] [CrossRef]
- Ewertz, M.; Anders, B.J. Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncol. 2011, 50, 187–193. [Google Scholar] [CrossRef]
- Jackisch, C.; Untch, M.; Blohmer, J.U.; Nitz, U.; Harbeck, N. Evolution of the 21-gene Assay Oncotype DX® from an Experimental Assay to an Instrument Assisting in Risk Prediction and Optimisation of Treatment Decision-making in Early Breast Cancer. Eur. Oncol. 2009, 6, 36–42. [Google Scholar]
- Tian, S.; Roepman, P.; van’t Veer, L.J.; Bernards, R.; De Snoo, F.; Glas, A.M. Biological functions of the genes in the mammaprint breast cancer profile reflect the hallmarks of cancer. Biomark. Insights 2009, 5, 129–138. [Google Scholar]
- Apostolou, P.; Fostira, F. Hereditary breast cancer: the era of new susceptibility genes. BioMed Res. Int. 2013, 2013, 747318. [Google Scholar] [CrossRef]
- Walsh, T.; Casadei, S.; Coats, K.H.; Swisher, E.; Stray, S.M.; Higgins, J.; Foretova, L. Spectrum of mutations in BRCA1, BRCA2, CHEK2, and TP53 in families at high risk of breast cancer. JAMA 2006, 295, 1379–1388. [Google Scholar] [CrossRef]
- Stadler, Z.K.; Schrader, K.A.; Vijai, J.; Robson, M.E.; Offit, K. Cancer genomics and inherited risk. J. Clin. Oncol. 2014, 32, 687–698. [Google Scholar] [CrossRef]
- Rizzolo, P.; Silvestri, V.; Tommasi, S.; Pinto, R.; Danza, K.; Falchetti, M.; Gulino, M.; Frati, P.; Ottini, L. Male breast cancer: Genetics, epigenetics, and ethical aspects. Ann. Oncol. 2013, 24, viii75–viii82. [Google Scholar] [CrossRef]
- Hutson, S. Attitudes and Psychological Impact of Genetic Testing, Genetic Counseling, and Breast Cancer Risk Assessment Among Women at Increased Risk. Oncol. Nurs. Forum 2003, 30, 241–246. [Google Scholar] [CrossRef]
- Breast Cancer Foundation. BEEP. 2016. Available online: http://www.bcf.org.sg/support/programmes/beep (accessed on 14 November 2016).
- Breast Cancer Network Japan. Available online: http://www.akebono-net.org/contents/e_index.html (accessed on 27 December 2016).
- Breast Cancer Care. Available online: https://www.breastcancercare.org.uk/ (accessed on 27 December 2016).
| Stages | Description |
|---|---|
| Denial | The first reaction to a malignant diagnosis is to deny the reality [37]. It is a temporary defense mechanism protecting one against the shock of a debilitating event [41]. |
| Anger | As an individual is eventually forced to face the truth, she starts to question why this is happening to her, and who is to blame [37]. She experiences intense pain and helplessness that manifest as anger directed to those around them [41]. During this stage, people around them may develop emotional resentments which could worsen their relationship. It is thus important for family and friends to empathize with the individual’s grieving phases. |
| Bargaining | The individual focuses on what she or others could have done differently to prevent the cancer from occurring. She imagines how much better life could have been without cancer. She may also make a pact with God in the hope that life could go back to the times before the diagnosis [37]. While such thoughts may help the individual to accept the diagnosis, it could lead to an intense sense of guilt. |
| Depression | After accepting cancer as inevitable, the individual feels a sense of emptiness and profound sadness [37]. She may see no meaning in doing anything. While many people seek to avoid settling into this state, it is important to recognize depression as a natural response to a great loss. One has to let herself face her emotions upfront and feel her grief fully before she can recover completely. This stage should not be rushed and different individuals may spend varying amounts of time in this stage [41]. |
| Acceptance | Acceptance may follow depression, as the individual decides that she is ready to accept what has happened [37]. She may not be completely alright with it, but she is willing to make adjustments and learn to live with it. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, Z.X.; Ong, M.S.; Jegadeesan, T.; Deng, S.; Yap, C.T. Breast Cancer: Exploring the Facts and Holistic Needs during and beyond Treatment. Healthcare 2017, 5, 26. https://doi.org/10.3390/healthcare5020026
Ng ZX, Ong MS, Jegadeesan T, Deng S, Yap CT. Breast Cancer: Exploring the Facts and Holistic Needs during and beyond Treatment. Healthcare. 2017; 5(2):26. https://doi.org/10.3390/healthcare5020026
Chicago/Turabian StyleNg, Zhi Xuan, Mei Shan Ong, Tamilarasi Jegadeesan, Shuo Deng, and Celestial T. Yap. 2017. "Breast Cancer: Exploring the Facts and Holistic Needs during and beyond Treatment" Healthcare 5, no. 2: 26. https://doi.org/10.3390/healthcare5020026





