Student Perceptions and Acceptance of Mobile Technology in an Undergraduate Nursing Program
Abstract
:1. Introduction
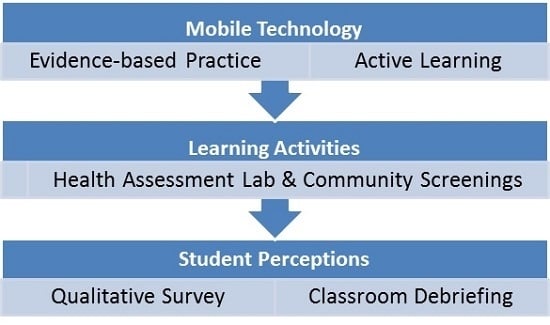
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Williams, M.G.; Dittmer, A. Textbooks on tap: Using electronic books housed in handheld devices in nursing clinical courses. Nurs. Educ. Perspect. 2009, 30, 220–225. [Google Scholar] [PubMed]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001; p. 164. Available online: http://iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx (accessed on 31 May 2017).
- Grabowsky, A. Smartphone use to answer clinical questions: A descriptive study of APNs. Med. Ref. Serv. Q. 2015, 34, 135–148. [Google Scholar] [CrossRef] [PubMed]
- Day-Black, C. Minorities in nursing education: Using smartphones. ABNF J 2015, 26, 85–89. [Google Scholar] [PubMed]
- Poushter, J. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies; Pew Research Center: Washington, DC, USA, 2016; Available online: http://www.pewglobal.org/files/2016/02/pew_research_center_global_technology_report_final_february_22_2016.pdf (accessed on 31 May 2017).
- McNally, G.; Frey, R.; Crossan, M. Nurse manager and student nurse perceptions of the use of personal smartphones or tablets and the adjunct applications, as an educational tool in clinical settings. Nurse Educ. Pract. 2017, 23, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Raman, J. Mobile technology in nursing education: Where do we go from here? A review of the literature. Nurse Educ. Today 2015, 35, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Doyle, G.J.; Garrett, B.; Currie, L.M. Integrating mobile devices into nursing curricula: Opportunities for implementation using Rogers’ Diffusion of Innovation model. Nurse Educ. Today 2014, 34, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Phillippi, J.C.; Wyatt, T.H. Smartphones in nursing education. Comput. Inform. Nurs. 2011, 29, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Wittmann-Price, R.A.; Kennedy, L.D.; Godwin, C. Use of personal phones by senior nursing students to access health care information during clinical education: Staff nurses’ and students’ perceptions. J. Nurs. Educ. 2012, 51, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Kroning, M. The importance of integrating active learning in education. Nurse Educ. Pract. 2014, 14, 447–448. [Google Scholar] [CrossRef] [PubMed]
- Swenty, C.L.; Titzer, J.L. A sense of urgency: Integrating technology and informatics in advance practice nursing education. J. Nurse Pract. 2014, 10, e57–e67. [Google Scholar] [CrossRef]
- Elliott, L.; DeCristofaro, C.; Carpenter, A. Blending technology in teaching advanced health assessment in a family nurse practitioner program: Using personal digital assistants in a simulation laboratory. J. Am. Acad. Nurse Pract. 2012, 24, 536–543. [Google Scholar] [CrossRef] [PubMed]
- George, T.P.; DeCristofaro, C. Use of smartphones with undergraduate nursing students. J. Nurs. Educ. 2016, 55, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Martyn, J.; Larkin, K.; Sander, T.; Yuginovich, T.; Jamieson-Proctor, R. Distance and devices—Potential barriers to use of wireless handheld devices. Nurse Educ. Today 2014, 34, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Friederichs, H.; Marschall, B.; Weissenstein, A. Practicing evidence based medicine at the bedside: A randomized controlled pilot study in undergraduate medical students assessing the practicality of tablets, smartphones, and computers in clinical life. BMC Med. Inform. Decis. Mak. 2014, 14, 113. [Google Scholar] [CrossRef] [PubMed]
- Gaglani, S.M.; Topol, E.J. iMedEd: The role of mobile health technologies in medical education. Acad. Med. 2014, 89, 1207–1209. [Google Scholar] [CrossRef] [PubMed]
- SplendApps. BMI Calculator. Available online: https://play.google.com/store/apps/details?id=com.splendapps.bmicalc (accessed on 31 May 2017).
- National Heart Lung and Blood Institute. NHLBI BMI Calculator. Available online: https://itunes.apple.com/us/app/nhlbi-bmi-calculator/id446441346?mt= (accessed on 31 May 2017).
- Agency for Healthcare Research and Quality. ePSS Electronic Preventive Services Selector. Available online: http://epss.ahrq.gov/PDA/index.jsp (accessed on 31 May 2017).
- Joslin Diabetes Center. Goals for Blood Glucose Control 2017. Available online: http://www.joslin.org/info/Goals-for-Blood-Glucose-Control.html (accessed on 31 May 2017).
- Centers for Disease Control and Prevention. Measuring Blood Pressure 2014. Available online: http://www.cdc.gov/bloodpressure/measure.htm (accessed on 31 May 2017).
- Centers for Disease Control and Prevention. About adult BMI 2015. Available online: http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/ (accessed on 31 May 2017).
- National Heart Lung and Blood Institute. How is High Cholesterol Diagnosed? 2016. Available online: http://www.nhlbi.nih.gov/health/health-topics/topics/hbc/diagnosis (accessed on 31 May 2017).
- Agency for Healthcare Research & Quality. Men: Stay Healthy at Any Age. 2012. Available online: https://archive.ahrq.gov/patients-consumers/patient-involvement/healthy-men/index.html (accessed on 31 May 2017).
- Agency for Healthcare Research & Quality. Women: Stay Healthy at Any Age. 2014. Available online: https://archive.ahrq.gov/patients-consumers/prevention/lifestyle/healthy-women.html (accessed on 31 May 2017).
- Levine, D.M.; Lipsitz, S.R.; Linder, J.A. Trends in seniors’ use of digital health technology in the United States, 2011–2014. JAMA 2016, 316, 538–540. [Google Scholar] [CrossRef] [PubMed]
| What skills have you developed from participating in the community screening activity? |
| What were your best and worst experiences in the community screening activity? |
| Was there anything that affected your performance at the community screening activity? |
| What are your thoughts on the use of smartphone apps in nursing practice? |
| Will you continue to use smartphone apps in your nursing education and nursing practice? |
| What types of responses from patients did you receive when you used apps to provide them with patient education? |
| Gender | |
| Female | 84.5% (n = 60) |
| Male | 15.5% (n = 11) |
| Race | |
| Caucasian | 81.7% (n = 58) |
| Black/African/American | 16.9% (n = 12) |
| Other Race | 1% (n = 1) |
| Age | |
| 18–25 years of age | 88.7% (n = 63) |
| 26–35 years of age | 8.5% (n =6) |
| 36–45 years of age | 1.4% (n = 1) |
| 46–55 years of age | 1.4% (n = 1) |
| Theme 1: Communication and patient interaction | Students felt that this learning activity benefited them by improving their comfort level when taking patient histories and providing patient education. One student said there was a “better interaction with patients and techniques” and another stated “I developed better social skills in a real-life setting”. Communication skills were also felt to be enhanced. Student comments included: “how to communicate information to multiple patients, ask the right questions, become comfortable during the appointment, interact naturally”. |
| Theme 2: Cultural competence | Of importance to future nursing interactions with the area’s patient population, a student commented, “I learned how to communicate with people of different races and cultural backgrounds” and another stated, “how to deal with all kinds of people and how to have different approaches towards people”. An interesting comment was, “the patients aren’t scary”. |
| Theme 3: Patient education skills | Students were required to provide individualized patient education based on the ePSS app results. Comments included: “how to talk to patients about their results from blood glucose and cholesterol results” and “I was familiar with diabetes management and prevention; however this screening has enhanced my ability in skills in dealing with this disease”. |
| Theme 4: Knowledge base and application | Students felt they were able to translate didactic knowledge to real-world application. Comments include: “understanding how to implement what we learned in class”, “practice what we learned in lab”, “applying what we learned in class to real situations”, and “patient interaction and knowledge of the material”. |
| Theme 5: Nursing role | Students indicated that the screenings assisted them in embracing the nursing role. Comments included “it got me over my first patient anxiety”, “I feel more comfortable talking and having a patient/nurse interaction”, and “Confidence, talking to real patients, practice asking personal questions”. |
| Theme 6: Perception of smartphone apps | Overall, over 90% of students plan to continue using smartphone apps in their nursing practice. Students reported finding the apps “helpful”, “useful”, “I think they are convenient, it is nice to have all the information you need at your fingertips”, “I think they are very helpful and a great advancement in nursing”, “very quick and easy to use as a resource”, and “they are very useful and meaningful, being that my peers and I are dependent on technology and smartphones”. |
| Theme 7: Patient acceptance | Students reported positive feedback and acceptance of the apps from patients. One nursing student stated that patients “were impressed that I was able to obtain information that quickly and accurately”, and “patients seemed comfortable with apps”. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
George, T.P.; DeCristofaro, C.; Murphy, P.F.; Sims, A. Student Perceptions and Acceptance of Mobile Technology in an Undergraduate Nursing Program. Healthcare 2017, 5, 35. https://doi.org/10.3390/healthcare5030035
George TP, DeCristofaro C, Murphy PF, Sims A. Student Perceptions and Acceptance of Mobile Technology in an Undergraduate Nursing Program. Healthcare. 2017; 5(3):35. https://doi.org/10.3390/healthcare5030035
Chicago/Turabian StyleGeorge, Tracy P., Claire DeCristofaro, Pamela F. Murphy, and Archie Sims. 2017. "Student Perceptions and Acceptance of Mobile Technology in an Undergraduate Nursing Program" Healthcare 5, no. 3: 35. https://doi.org/10.3390/healthcare5030035