Psychotherapy Training on Psychological Mindedness in a Japanese Nurse Population: Effects and Personality Correlates
Abstract
:1. Introduction
2. Methods
2.1. Participants and Procedures
2.2. Measurements
2.2.1. Psychological Mindedness
2.2.2. Personality Traits
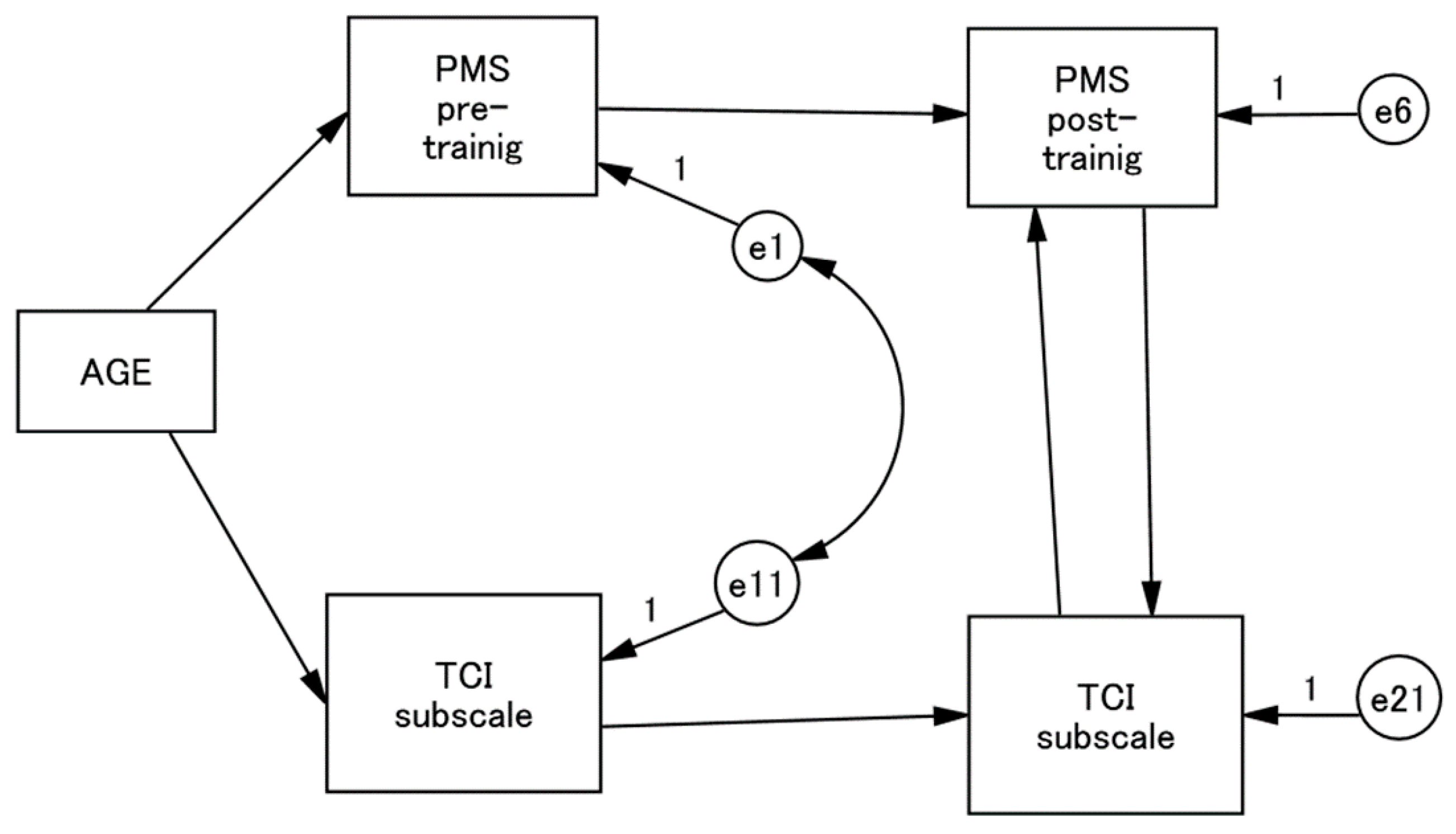
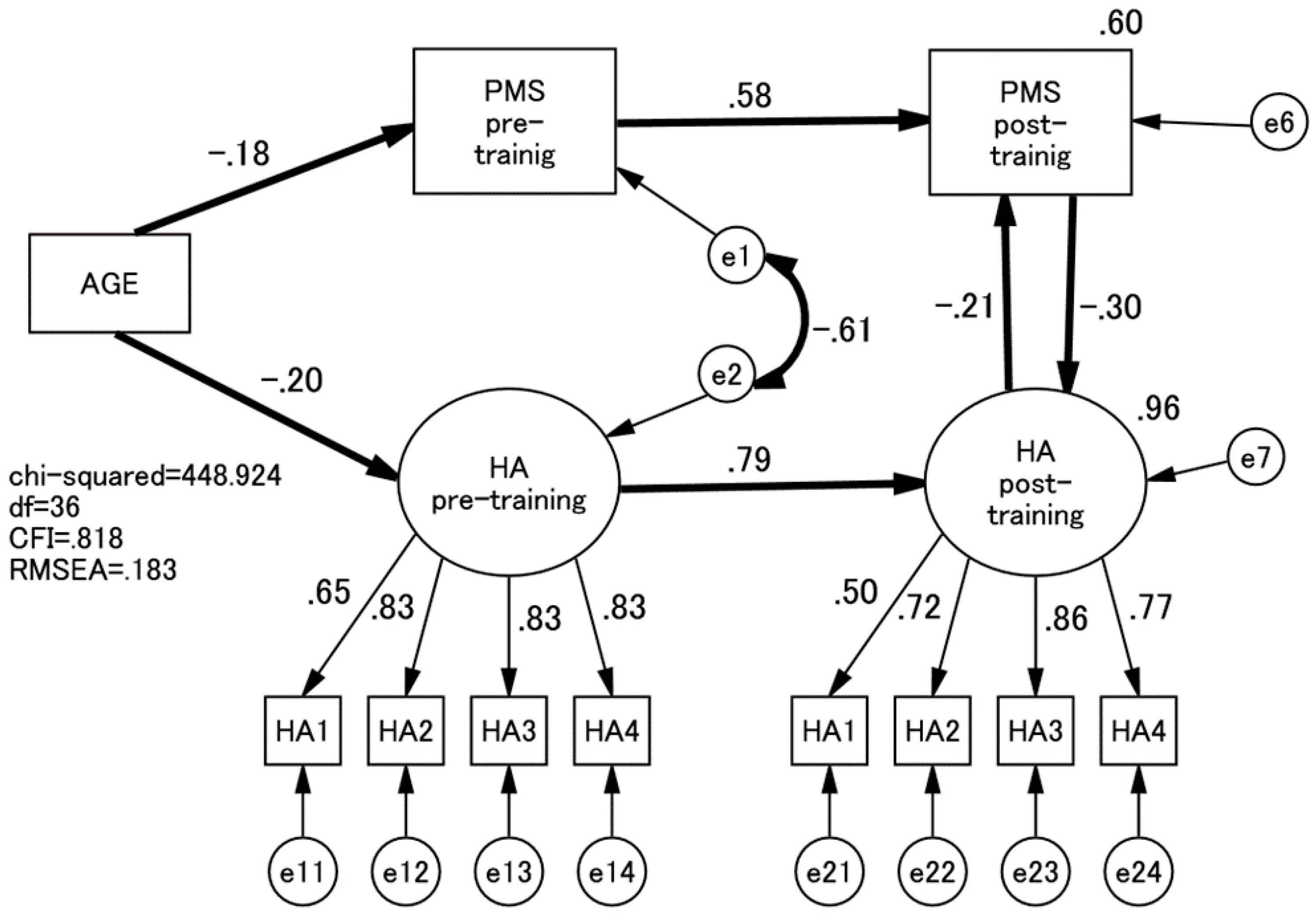
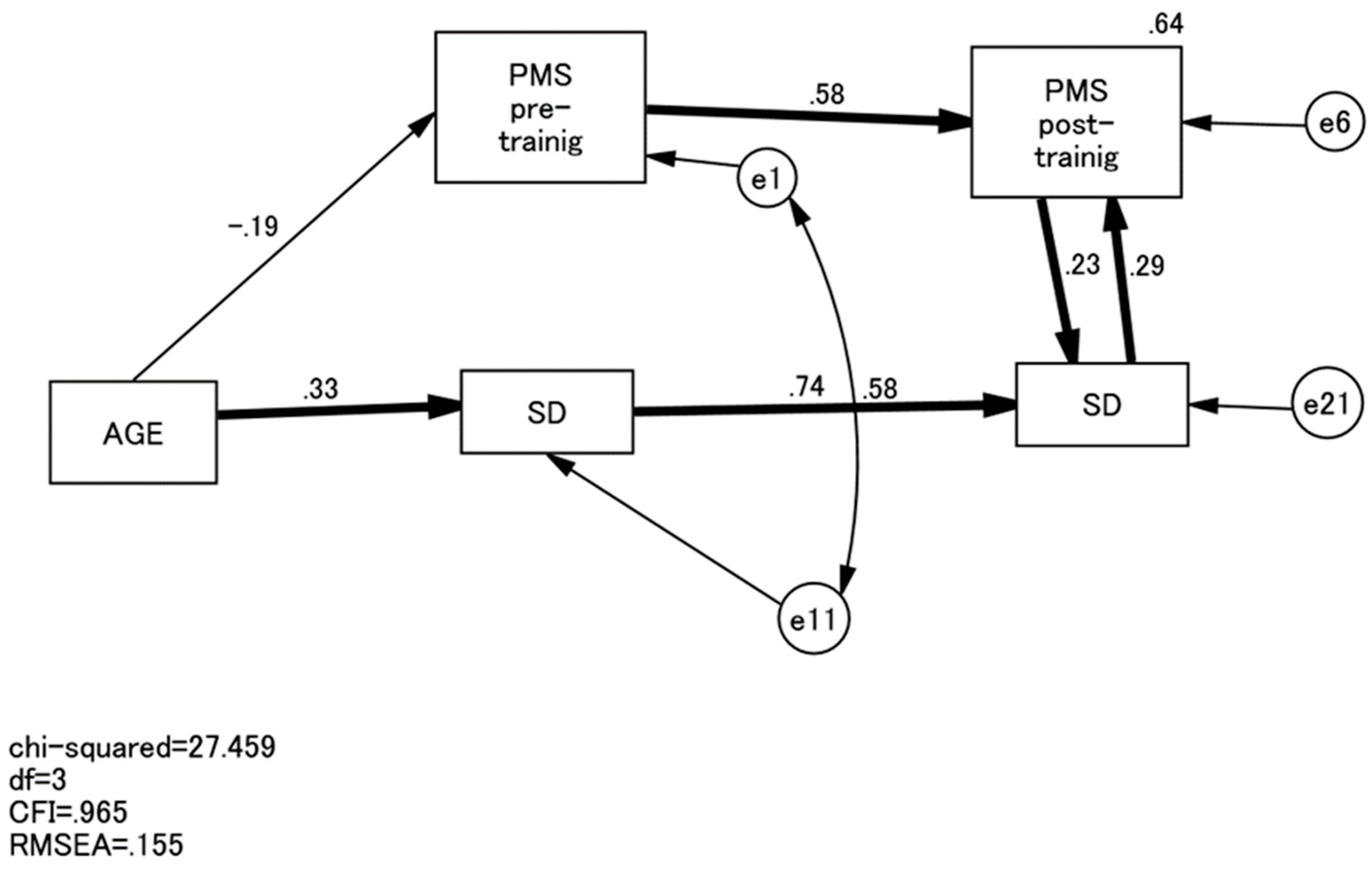
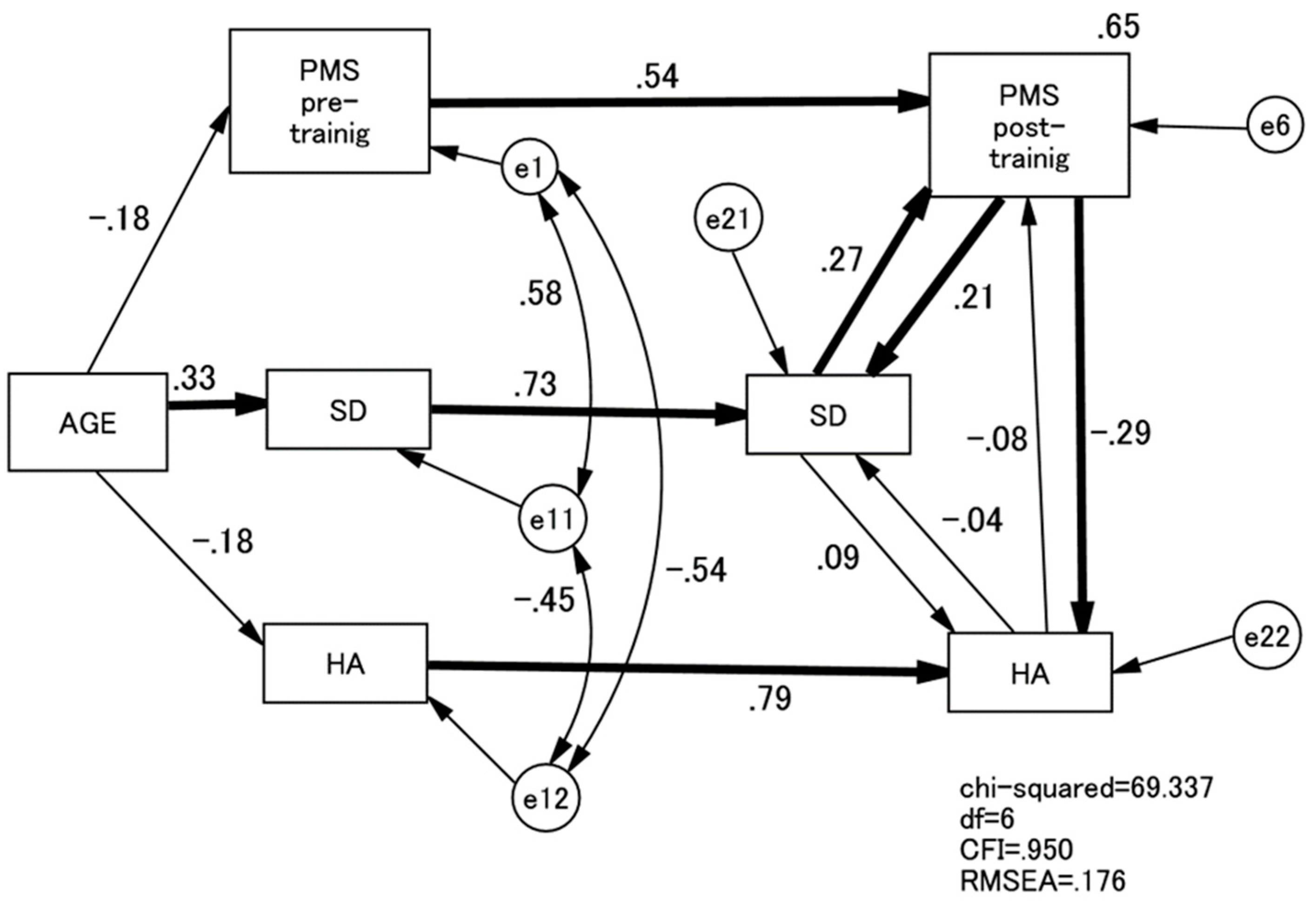
2.3. Data Analyses
2.4. Ethical Consideration
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Stuart, S.; O’Hara, M.W.; Gorman, L.L. The prevention and psychotherapeutic treatment of postpartum depression. Arch. Womens Ment. Health 2003, 6 (Suppl. 2), S57–S69. [Google Scholar] [CrossRef] [PubMed]
- Conte, H.R.; Ratto, R.; Karasu, T.B. The psychological mindedness scale: Factor structure and relationship to outcome of psychotherapy. J. Psychother. Pract. Res. 1996, 5, 250–259. [Google Scholar] [PubMed]
- Appelbaum, S.A. Psychological-mindedness: Word, concept and essence. Int. J. Psychoanal. 1973, 54, 35–46. [Google Scholar] [PubMed]
- Beitel, M.; Ferrer, E.; Cecero, J.J. Psychological mindedness and awareness of self and others. J. Clin. Psychol. 2005, 61, 739–750. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.R.; Farber, B.A.; Schonbar, R.A. The relationship of psychological-mindedness to adult perceptions of early parental rejection. J. Clin. Psychol. 1998, 54, 1079–1084. [Google Scholar] [CrossRef]
- Beitel, M.; Cecero, J.J. Predicting psychological mindedness from personality style and attachment security. J. Clin. Psychol. 2003, 59, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Beitel, M.; Ferrer, E.; Cecero, J.J. Psychological mindedness and cognitive style. J. Clin. Psychol. 2004, 60, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Farber, B.A. The genesis, development, and implications of psychological mindedness in psychotherapists. Psychotherapy 1985, 22, 170–177. [Google Scholar] [CrossRef]
- Farber, B.A. Psychological mindedness: Can there be too much of a good things? Psychotherapy 1989, 26, 210–217. [Google Scholar] [CrossRef]
- Hall, J.A. Psychological-mindedness: A conceptual model. Am. J. Psychother. 1992, 46, 131–140. [Google Scholar] [PubMed]
- Costa, P.T.; McCrae, R.R. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI); Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 1992. [Google Scholar]
- Zlotnick, C.; Johnson, S.L.; Miller, I.W.; Pearlstein, T.; Howard, M. Postpartum depression in women receiving public assistance: Pilot study of an interpersonal-therapy-oriented group intervention. Am. J. Psychiatry 2001, 158, 638–640. [Google Scholar] [CrossRef] [PubMed]
- Murray, L.; Cooper, P.J. Postpartum depression and child development. Psychol. Med. 1997, 27, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Condon, J.T.; Boyce, P.; Corkindale, C.J. The First-Time Fathers Study: A prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust. N. Z. J. Psychiatry 2004, 38, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Markowitz, J.C.; Klerman, G. Comprehensive Guide to Interpersonal Psychotherapy; Basic Books: New York, NY, USA, 2000. [Google Scholar]
- Takegata, M.; Ohashi, Y.; Haruna, M.; Kitamura, T. Theoretical framework for interpersonal psychotherapy in the prevention of postpartum depression: A commentary. Int. J. Nurs. Health Sci. 2014, 1, 37–40. [Google Scholar]
- Zlotnick, C.; Miller, I.W.; Pearlstein, T.; Howard, M.; Sweeney, P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am. J. Psychiatry 2006, 163, 1443–1445. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Dowswell, T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst. Rev. 2013, Cd001134. [Google Scholar] [CrossRef]
- Kitamura, T.; Okamura, S.; Takeda, S.; Fujita, J.; Uesato, C.; Sugiyama, T.; Kusaka, H.; Sato, S.; Fukushima, K.; Oba, T.; et al. Preventive Effects of Midwife-Led Psychological Intevention on the Severity of Depression after Childbirth; Japanese Ministry of Health and Labour: Tokyo, Japan, 2006; pp. 2–10. [Google Scholar]
- Conte, H.R.; Plutchik, R.; Jung, B.B.; Picard, S.; Karasu, T.B.; Lotterman, A. Psychological mindedness as a predictor of psychotherapy outcome: A preliminary report. Compr. Psychiatry 1990, 31, 426–431. [Google Scholar] [CrossRef]
- Cloninger, C.R.; Przybeck, T.R.; Svrakic, D.M.; Wetzel, R.D. The Temperament and Character Inventory (TCI): A Guide to its Development and Use; Centre for Psychobiology of Personality, Washington University: St. Louis, MO, USA, 1994. [Google Scholar]
- Kijima, N.; Saito, R.; Takeuchi, M.; Yoshino, A.; Ono, Y.; Kato, M.; Kitamura, T. Kloninger no kishitsu to seikaku no 7 jigen moderu oyobi nihongo-ban Temperament and Character Inventory (TCI) [Cloninger’s seven-factor model of temperament and character and the Japanese version of Temperament and Character Inventory (TCI)]. Arch. Psychiatry Diagn. Clin. Eval. 1996, 7, 379–399. [Google Scholar]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar]
- Cloninger, C.R.; Svrakic, D.M.; Przybeck, T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 975–990. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.T.; McCrae, R.R. Trait Psychology Comes of Age. Nebr. Symp. Motiv. 1991, 39, 169–204. [Google Scholar] [PubMed]
- Terry, D.J.; Rawle, R.; Callan, V.J. The effects of social support on adjustment to stress: The mediating role of coping. Pers Relation 1995, 2, 97–124. [Google Scholar] [CrossRef]
| Variables | Cronbach | Mean (SD) | t | ||
|---|---|---|---|---|---|
| Pre-Training | Post-Training | Pre-Training | Post-Training | ||
| PMS | 0.84 | 0.93 | 83.1 (10.1) | 87.4 (14.1) | 6.4 *** |
| HA | 0.90 | 0.87 | 30.9 (8.4) | 29.0 (7.3) | 7.4 *** |
| NS | 0.76 | 0.65 | 26.9 (5.6) | 27.2 (4.5) | 1.4 |
| RD | 0.75 | 0.69 | 31.2 (3.4) | 31.1 (4.6) | 0.5 |
| P | 0.46 | 0.39 | 15.9 (2.6) | 16.7 (2.5) | 5.1 *** |
| SD | 0.85 | 0.79 | 43.9 (7.6) | 45.4 (7.2) | 5.4 *** |
| CO | 0.82 | 0.89 | 50.9 (6.9) | 51.3 (7.9) | 1.2 |
| ST | 0.85 | 0.89 | 20.1 (6.2) | 20.8 (7.0) | 2.3 * |
| Varibles | PMS | HA | NS | RD | P | SD | CO | ST |
|---|---|---|---|---|---|---|---|---|
| PMS | - | |||||||
| HA | −0.49 ** −60 ** | - | ||||||
| NS | 0.08 0.14 | −0.384 * −0.453 ** | - | |||||
| RD | 0.40 * 0.69 * | 0.051 0.308 | −0.015 −0.223 | - | ||||
| P | 0.36 * 0.28 | −0.312 * −0.132 | −0.081 −0.378 * | 0.204 0.389 * | - | |||
| SD | 0.39 * 0.67 ** | −0.455 ** −0.507 ** | −0.187 0.062 | 0.024 0.442 ** | 0.165 0.125 | - | ||
| CO | 0.73 ** 0.89 ** | −0.394 ** −0.549 ** | −0.179 −0.029 | 0.524 ** 0.715 ** | 0.525 ** 0.377 * | 0.532 ** 0.730 * | - | |
| ST | 0.26 0.45 ** | −0.468 ** −0.419 ** | 0.057 0.033 | 0.237 0.365 * | 0.558 ** 0.624 ** | 0.131 0.088 | 0.436 ** 0.396 * | - |
| age | −0.204 ** 0.062 | −0.179 ** −0.096 | −0.199 ** 0.062 | −0.080 −0.088 | −0.013 −0.164 ** | 0.359 *** 0.223 *** | 0.078 0.082 | 0.053 −0.085 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, T.; Takeda, S.; Yamagishi, Y.; Kubo, R.; Kitamura, T. Psychotherapy Training on Psychological Mindedness in a Japanese Nurse Population: Effects and Personality Correlates. Healthcare 2017, 5, 43. https://doi.org/10.3390/healthcare5030043
Saito T, Takeda S, Yamagishi Y, Kubo R, Kitamura T. Psychotherapy Training on Psychological Mindedness in a Japanese Nurse Population: Effects and Personality Correlates. Healthcare. 2017; 5(3):43. https://doi.org/10.3390/healthcare5030043
Chicago/Turabian StyleSaito, Tomomi, Satoru Takeda, Yukiko Yamagishi, Reiko Kubo, and Toshinori Kitamura. 2017. "Psychotherapy Training on Psychological Mindedness in a Japanese Nurse Population: Effects and Personality Correlates" Healthcare 5, no. 3: 43. https://doi.org/10.3390/healthcare5030043




