Measuring Activity Performance of Older Adults Using the activPAL: A Rapid Review
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Assessment of Methodological Quality
3. Results
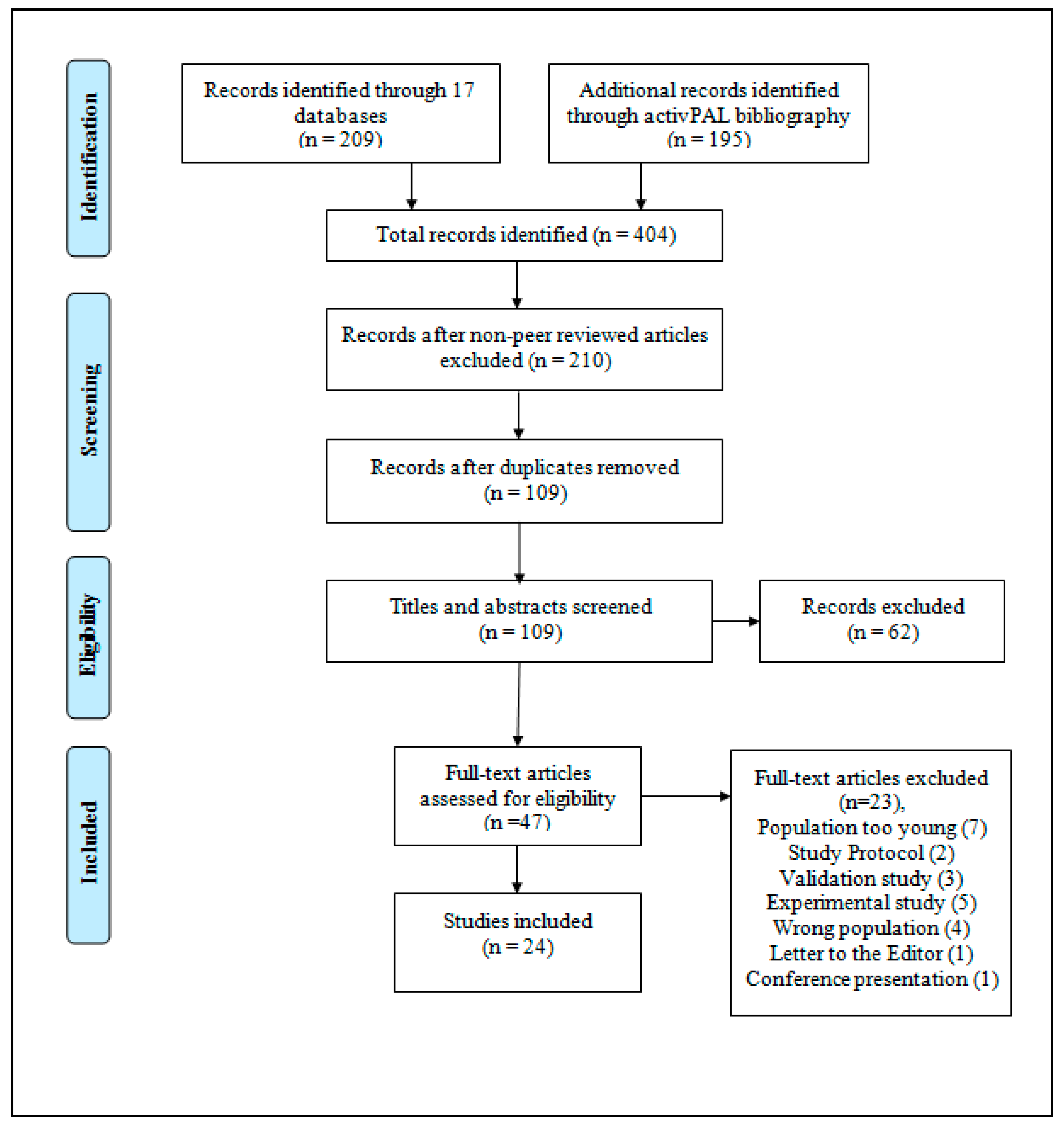
3.1. Study Selection
3.2. Study Characteristics
3.3. Participant Characteristics
3.4. Physical Activity Outcomes
3.5. Sedentary Behavior Outcomes
3.6. Limitations of the activPAL and Reporting Limitations
3.7. Quality Assessment
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Physical Activity and Older Adults. 2011. Available online: http://www.who.int/dietphysicalactivity/physical-activity-recommendations-65years.pdf?ua=1 (accessed on 30 August 2017).
- Owen, N.; Healy, G.; Matthews, C.; Dunstan, D. Too much sitting: The population-health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Grant, P.M.; Granat, M.H.; Thow, M.K.; Maclaren, W.M. Analyzing free-living physical activity of older adults in different environments using body-worn activity monitors. J. Aging Phys. Act. 2010, 18, 171–184. [Google Scholar] [CrossRef] [PubMed]
- De Bruin, E.D.; Hartmann, A.; Uebelhart, D.; Murer, K.; Zijilstra, W. Wearable systems for monitoring mobility-related activities in older people: A systematic review. Clin. Rehabil. 2008, 22, 878–895. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.; Sugiyama, T.; Healy, G.; Salmon, J.; Dunstan, D.; Owen, N. Validity and reliability of measures of television viewing time and other non-occupational sedentary behavior of adults: A review. Obes. Rev. 2008, 10, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Taraldsen, K.; Chastin, S.F.M.; Riphagen, I.I.; Vereijken, B.; Helbostad, J.L. Physical activity monitoring by use of accelerometer-based body-worn sensors in older adults: A systematic literature review of current knowledge and applications. Maturitas 2012, 71, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Godfrey, A.; Galna, B.; Mhiripiri, D.; Burn, D.; Rochester, L. Ambulatory activity in incident Parkinsons: More than meets the eye? J. Neurol. 2013, 260, 2964–2972. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farías, N.; Brown, W.J.; Olds, T.S.; Geeske Peeters, G.M. Validity of self-report methods for measuring sedentary behaviour in older adults. J. Sci. Med. Sport 2014, 18, 662–666. [Google Scholar] [CrossRef] [PubMed]
- Shephard, R.J. Limits to the measurement of habitual physical activity by questionnaires. Br. J. Sports Med. 2003, 37, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Sallas, J.F.; Saelens, B.E. Assessment of physical activity by self-report: Status, limitations, and future directions. Res. Q. Exerc. Sport 2000, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Hagströmer, M.; Pober, D.M.; Bowles, H.R. Best practices for using physical activity monitors in population-based research. Med. Sci. Sports Exerc. 2012, 44 (Suppl. 1), S68–S76. [Google Scholar] [CrossRef] [PubMed]
- Davies, G.; McGowan, A.; Dall, P.; Granat, M.; Paton, J. Validity, practical utility, and reliability of the activPAL in preschool children. Med. Sci. Sports Exerc. 2012, 44, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Aminian, S.; Hinckson, E. Examining the validity of the ActivPAL monitor in measuring posture and ambulatory movement in children. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwardson, C.; Winkler, E.; Bodicoat, D.; Yates, T.; Davies, M.; Dunstan, D.; Healy, G. Considerations when using the activPAL monitor in field-based research with adult populations. J. Sport Health Sci. 2017, 6, 162–178. [Google Scholar] [CrossRef]
- Grant, M.; Dall, P.; Mitchell, S.; Granat, M. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J. Aging Phys. Act. 2008, 16, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Taralsden, K.; Askim, T.; Sletvold, O.; Einarsen, E.K.; Bjåstad, K.G.; Indredavik, B.; Helbostad, J.L. Evaluation of a body-worn sensor system to measure physical activity in older people with impaired function. Phys. Ther. 2011, 91, 277–285. [Google Scholar]
- Reid, N.; Eakin, E.; Henwood, T.; Keogh, J.W.; Senior, H.E.; Gardiner, P.A.; Winkler, E.; Healy, G.N. Objectively measured activity patterns among adults in residential aged care. Int. J. Environ. Res. Public Health 2013, 10, 6783–6798. [Google Scholar] [CrossRef] [PubMed]
- Kunkel, D.; Fitton, C.; Burnett, M.; Ashburn, A. Physical inactivity post-stroke: A 3-year longitudinal study. Disabil. Rehabil. 2015, 37, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Khangura, S.; Konnyu, K.; Cushman, R.; Grimshaw, J.; Moher, D. Evidence summaries: The evolution of a rapid review approach. Syst. Rev. 2012, 1, 10. [Google Scholar] [CrossRef] [PubMed]
- Cummings, G.; Estabrooks, C. The effects of hospital restructuring that included layoffs on individual nurses who remained employed: A systematic review of impact. Int. J. Sociol. Soc. Policy 2003, 21, 176–199. [Google Scholar] [CrossRef]
- Estabrooks, C.; Vivek, G.; Elaine, T.; Pinfold, P.; Sawka, C.; Williams, I. Decision aids, are they worth it? A systematic review. J. Health Serv. Res. Policy 2001, 6, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Godfrey, A.; Conway, R.; Leonard, M.; Meagher, D.; Ólaighin, G.M. Motion analysis in delirium: A discrete approach in determining physical activity for the purpose of delirium motoric subtyping. Med. Eng. Phys. 2010, 32, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Peiris, C.L.; Taylor, N.F.; Shields, N. Patients receiving inpatient rehabilitation for lower limb orthopaedic conditions do much less physical activity than recommended in guidelines for healthy older adults: An observational study. J. Physiother. 2013, 59, 39–44. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Olds, T.S.; Hillsdon, M.; Pulsford, R.; Hurst, T.L.; Eston, R.G.; Gomersall, S.R.; Johnston, K.; Langford, J. Assessing sedentary behavior with the GENEActiv: Introducing the sedentary sphere. Med. Sci. Sports Exerc. 2014, 46, 1235–1247. [Google Scholar] [CrossRef] [PubMed]
- Davenport, S.J.; Arnold, M.; Hua, C.; Schenck, A.; Batten, S.; Taylor, N.F. Physical activity levels during acute inpatient admission after hip fracture are very low. Physiother. Res. Int. 2015, 20, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Chastin, S.F.M.; McInnes, L.; Little, L.; Briggs, P.; Rochester, L. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing 2011, 40, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Klenk, J.; Büchele, G.; Rapp, K.; Franke, S.; Peter, R. ActiFE Study Group. Walking on sunshine: Effect of weather conditions on physical activity in older people. J. Epidemiol. Community Health 2012, 66, 474–476. [Google Scholar] [CrossRef] [PubMed]
- Klenk, J.; Denkinger, M.; Nikolaus, T.; Peter, R.; Rothenbacher, D.; Koenig, W. ActiFE Study Group. Association of objectively measured physical activity with established and novel cardiovascular biomarkers in elderly subjects: Every step counts. J. Epidemiol. Community Health 2012, 67, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, A.; Lord, S.; Galna, B.; Mathers, J.C.; Burn, D.J.; Rochester, L. The association between retirement and age on physical activity in older adults. Age Ageing 2014, 43, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Salbach, N.M.; Brooks, D.; Romano, J.; Woon, L.; Dolmage, T. Cardiorespiratory responses during the 6-minute walk and ramp cycle ergometer tests and their relationship to physical activity in stroke. Neurorehabil. Neural Repair 2014, 28, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Gennuso, K.P.; Thraen-Borowski, K.M.; Gangnon, R.E.; Colbert, L.H. Patterns of sedentary behavior and physical function in older adults. Aging Clin. Exp. Res. 2015, 28, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Klenk, J.; Kerse, N.; Rapp, K.; Nikolaus, T.; Becker, C.; Rothenbacher, D.; Peter, R.; Denkinger, M.D.; the ActiFE Study Group. Physical activity and different concepts of fall risk estimation in older people—Results of the ActiFE-Ulm study. PLoS ONE 2015, 10, e0129098. [Google Scholar] [CrossRef] [PubMed]
- Clarke-Moloney, M.; Godfrey, A.; O’Connor, V.; Meagher, H.; Burke, P.E.; Kavanagh, E.G.; Grace, P.A.; Lyons, G.M. Mobility in patients with venous leg ulceration. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Maddocks, M.; Byrne, A.; Johnson, C.D.; Wilson, R.H.; Fearon, K.C.H.; Wilcock, A. Physical activity level as an outcome measure for use in cancer cachexia trials: A feasibility study. Support Care Cancer 2010, 18, 1539–1544. [Google Scholar] [CrossRef] [PubMed]
- Clarke, C.L.; Holdsworth, R.J.; Ryan, C.G.; Granat, M.H. Free-living physical activity as a novel outcome measure in patients with intermittent claudication. Eur. J. Vasc. Endovasc. Surg. 2012, 45, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Maddocks, M.; Wilcock, A. Exploring physical activity level in patients with thoracic cancer: Implications for use as an outcome measure. Support Care Cancer 2012, 20, 1113–1116. [Google Scholar] [CrossRef] [PubMed]
- Mactier, K.; Lord, S.; Godfrey, A.; Burn, D.; Rochester, L. The relationship between real world ambulatory activity and falls in incident Parkinson’s disease: Influence of classification scheme. Parkinsonism Relat. Disord. 2014, 21, 236–242. [Google Scholar] [CrossRef] [PubMed]
- English, C.; Healy, G.N.; Coates, A.; Lewis, L.; Olds, T.; Bernhardt, J. Sitting and activity time in people with stroke. Phys. Ther. 2015, 96, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Duncan, F.; Lewis, S.J.; Greig, C.A.; Dennis, M.S.; Sharpe, M.; MacLullich, A.M.; Mead, G.E. Exploratory longitudinal cohort study of association of fatigue after stroke. Stroke 2015, 46, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Stansfield, B.; Clarke, C.; Dall, P.; Godwin, J.; Holdsworth, R.; Granat, M. True cadence and step accumulation are not equivalent: The effect of intermittent claudication on free-living cadence. Gait Posture 2015, 41, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2013, 11, 35–49. [Google Scholar] [CrossRef] [PubMed]
- Esliger, D.W.; Copeland, J.L.; Barnes, J.D.; Treambla, M.S. Standardizing and optimizing the use of accelerometer data for free-living physical activity monitoring. J. Phys. Act. Health 2005, 2, 366–383. [Google Scholar] [CrossRef]
- Ward, D.; Evenson, K.; Vaughn, A.; Rodgers, A.; Troiano, R. Accelerometer use in physical activity: Best practices and research recommendations. Med. Sci. Sports Exerc. 2005, 37 (Suppl. 11), S582–S588. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Slaughter, S.; Jones, C.; Wagg, A. Measuring activity performance of continuing care residents using the ActivPAL: An exploratory study. J. Frailty Aging 2016, 5, 158–161. [Google Scholar] [PubMed]
| Author | Country | Study Design | Population and Setting | n | Mean Age, Years (Standard Deviation) | Time Worn (h) | Activity Outcome Measured Daily Average (SD) |
|---|---|---|---|---|---|---|---|
| Clarke-Moloney et al., 2007 [34] | UK | Cross-sectional | Patients with leg ulcers and healthy age-matched controls | 50 (24 M, 26 F) | 70.5 (median) (IQR–NR) | 24 h × 7 days | LU median (range) % time upright = 30.8 (8.4–30.6) C median (range) % time upright = 27.7 (17.7–42.6) LU median (range) % time spent sitting/lying = 69.2 (49.4–91.6) C median (range) % time spent sitting/lying = 72.3 (57.4–82.3) LU median (range) step count = 6685 (2074–17,999) C median (range) step count = 8750 (4917–16,043) |
| Godfrey et al., 2010 [23] | UK | Cross-sectional | Palliative care patients | 40 (23 M, 17 F) | 68.4 (11.9) | 24 h × 1 day | Hours sitting/lying = 22.6 (2.12) Hours standing = 0.8 (1.27) Hours stepping = 0.21 (0.47) |
| Grant et al., 2010 [3] | UK | Cross-sectional | Older adults from two hospitals | 70 (25 M, 45 F) | City: 81.8 (6.7) Rural: 79.4 (4.7) Hospital: 74.7 (7.9) Healthy: 73.7 (5.5) | 24 h × 8 days | City ward hours upright = 1.17 (0.84) Rural ward hours upright = 1.34 (0.69) Day hospital hours upright = 3.89 (1.88) Community hospital hours upright = 6.01 (1.87) |
| Maddocks et al., 2010 [35] | UK | Cross-sectional | Individuals with lung or upper gastrointestinal cancer from an oncology clinic | 60 (40 M, 20 F) | 68.0 (9.0) | 24 h × 7 days | Waking hours sitting/lying = 10.8 (2.5) Hours standing = 3.4 (1.6) Hours stepping = 1.0 (0.7) Step count = 4244 (2939) |
| Lord et al., 2011 [27] | UK | Cross-sectional | Community-dwelling older adults | 56 (26 M, 30 F) | 78.9 (4.9) | 24 h × 7 days | Hours upright = 4.18 (1.73) Waking hours sitting/lying = 12.46 (1.94) Step count = 6343 (2807) |
| Clarke et al., 2012 [36] | UK | Cross-sectional | Individuals with IC from an outpatient clinic and healthy age-matched controls | 60 (36 M, 24 F) | IC: 67.2 (9.7) C: 66.8 (10.5) | 24 h × 7 days | C group step count = 8864 (3110) IC group step count = 6524 (2710) |
| Klenk et al., 2012 [28] | Germany | Cross-sectional | Community-dwelling older adults | 1324 (747 M, 577 F) | 74.6 (NR) | 24 h × 7 days | Men hours stepping = 1.74 (0.85) Women hours stepping = 1.72 (0.80) |
| Klenk et al., 2012 [29] | Germany | Cross-sectional | Community-dwelling older adults | 1253 (710 M, 543 F) | 75.6 (6.5) | 24 h × 7 days | Men hours stepping = 1.75 (0.69) Women hours stepping = 1.72 (0.66) |
| Maddocks et al., 2012 [37] | UK | Cross-sectional | Individuals with thoracic cancer from an outpatient clinic | 84 (54 M, 30 F) | 66.0 (9.0) | 24 h × 7 days | Total hours sitting/lying = 19.7 (2.1) Hours upright = 4.3 (2.0) Step count = 4246 (2983) |
| Lord et al., 2013 [7] | UK | Cross-sectional | Patients with newly diagnosed PD from secondary care services and healthy controls | 186 (112 M, 74 F) | PD: 67.3 (9.9) C: 69.2 (7.7) | 24 h × 7 days | C group % total time stepping = 6.9 (2.3) PD group % total time stepping = 5.1 (2) C group step count = 7816 (5452) PD group step count = 5452 (2501) |
| Peiris et al., 2013 [24] | Australia | Cross-sectional | Adult inpatients with lower limb orthopaedic condition | 54 (34 M, 40 F) | 74.0 (11.0) | 24 h × 3 days | Median (IQR) step count = 398 (140–993) Median (IQR) hours stepping = 0.13 (0.05–0.27) Hours upright = 0.97 (0.62) Hours sitting/lying = 23.0 (0.7) |
| Reid et al., 2013 [17] | Australia | Cross-sectional | Residential aged care residents | 31 (11 M, 20 F) | 84.2 (NR) | 24 h × 7 days | Waking hours sitting/lying = 12.4 (IQR = 1.7) Hours standing = 1.9 (IQR = 1.3) Hours stepping = 0.36 (IQR = 0.40) Step count = 1055 (IQR = 1110) |
| Rowlands et al., 2014 [25] | Australia | Cross-sectional | Individuals with COPD in a hospital | 10 (4 M, 6 F) | 75.9 (9.7) | 24 h × 1–2 days | Total hours sitting/lying = 22.15 (1.33) Total hours standing = 1.84 (1.34) |
| Aguilar-Farías et al., 2014 [8] | Australia | Cross-sectional | Community-dwelling older adults | 41 (14 M, 27 F) | 74.5 (7.6) | 24 h × 7 days | Waking hours sitting/lying = 9.60 (1.66) Waking weekday hours sitting/lying = 9.55 (1.64) Waking weekend hours sitting/lying = 9.68 (1.96) |
| Godfrey et al., 2014 [30] | UK | Cross-sectional | Community-dwelling older adults | 98 (50 M, 48 F) | 69.1 (7.6) | 24 h × 7 days | Employed % time sitting/lying = 78.00 (6.17) Employed % time stepping = 6.24 (2.18) Retired % time sitting/lying = 74.73 (5.77) Retired % time stepping = 1.76 (0.15) |
| Mactier et al., 2014 [38] | UK | Cross-sectional | Individuals newly diagnosed with PD | 111 (77 M, 34 F) | 68.7 (median) (IQR—60.9–75.0) | 24 h × 7 days | No falls median (IQR) % time stepping = 5.1 (3.9–6.5) Single fall median (IQR) % time stepping = 4.9 (3.4–5.7) Recurrent falls median (IQR) % time stepping = 5.1 (3.9–6.2) |
| Salbach et al., 2014 [31] | Canada | Cross-sectional | Community-dwelling PS | 16 (14 M, 2 F) | 71.1 (9.7) | Waking hours × 5 days | Hours upright = 3.15 (2.27) |
| Davenport et al., 2015 [26] | Australia | Cross-sectional | Older adults post-surgical from hip fractures | 20 (2 M, 18 F) | 79.1 (9.3) | 24 h × 7 days | % of day sitting/lying = 98.9 (1.0) % of day standing = 1.1(1.0) % of day stepping = 0.05(0.09) Step Count = 35.7 (80.4) |
| Duncan et al., 2015 [40] | UK | Prospective cohort | Individuals with acute stroke admitted to hospital or an outpatient clinic | 84 (56 M, 28 F) | 72.3 (median) (IQR—65.2–80.5) | 24 h × 7 days | Median (IQR) step count in thousands at 1 month = 2.841 (1.419–5.723) Median (IQR) step count in thousands at 6 months = 4.047 (2.056–5.822) Median (IQR) step count in thousands at 12 months = 4.314 (1.657–6.890) |
| English et al., 2015 [39] | Australia | Cross-sectional | Individual post-stroke and healthy controls | 63 (41 M, 22 F) | 68.4 (10.0) | 24 h × 7 days | PS hours sitting = 10.9 (2.0) C hours sitting = 8.2 (2.0) PS hours standing = 2.6 (1.5) C hours standing = 5.2 (1.7) PS hours stepping = 1.1 (0.8) C hours stepping = 2.2(0.8) PS step count = 2411 (1835) C step count = 5314 (2100) |
| Gennuso et al., 2015 [32] | USA | Cross-sectional | Community-dwelling older adults | 44 (16 M, 28 F) | 70.0 (8.0) | Waking hours × 3 days | Median (25–75%) M hours sitting = 9.6 (8.7–11.1) Median (25–75%) F hours sitting = 9.3 (7.9–10.3) |
| Klenk et al., 2015 [33] | Germany | Prospective cohort | Community-dwelling older adults | 1214 (693 M, 521 F) | 75.6 (6.5) | 24 h × 7 days | Hours stepping = 1.73 (0.67) |
| Kunkel et al., 2015 [18] | UK | Prospective cohort | Individuals post-stroke in a hospital | 76 (39 M, 35 F) | 76.0 (11.0) | 6–7 h × 1 day | PS % waking time sitting/lying = 94 PS % waking time standing = 4 PS % waking time stepping = 2 |
| Stansfield et al., 2015 [41] | UK | Cross-sectional | Individuals with IC from an outpatient service and healthy controls | 60 (36 M, 24 F) | IC: 67.2 (9.7) C: 66.8 (10.5) | 24 h × 7 days | C group hours stepping = 5.00 (1.17) C group step count = 8692 (2945) IC group hours stepping = 5.02 (1.67) IC group step count = 6531 (2712) |
| Study Reference | Design (/2) | Sample (/4) | Measurement (/6) | Statistical Analysis (/2) | Overall Rating (/14) |
|---|---|---|---|---|---|
| Clarke-Moloney et al., 2007 [34] | 1 | 1 | 0 | 1 | 3 (LOW) |
| Godfrey et al., 2010 [23] | 1 | 1 | 1 | 0 | 3 (LOW) |
| Grant et al., 2010 [3] | 1 | 1 | 3 | 1 | 6 (MEDIUM) |
| Maddocks et al., 2010 [35] | 1 | 3 | 3 | 0 | 7 (MEDIUM) |
| Lord et al., 2011 [27] | 1 | 1 | 4 | 1 | 7 (MEDIUM) |
| Clarke et al., 2012 [36] | 1 | 1 | 3 | 0 | 5 (MEDIUM) |
| Klenk et al., 2012 [28] | 2 | 2 | 3 | 1 | 8 (MEDIUM) |
| Klenk et al., 2012 [29] | 2 | 2 | 1 | 0 | 5 (MEDIUM) |
| Maddocks et al., 2012 [37] | 1 | 2 | 1 | 0 | 4 (LOW) |
| Lord et al., 2013 [7] | 1 | 1 | 2 | 1 | 5 (MEDIUM) |
| Peiris et al., 2013 [24] | 2 | 1 | 3 | 0 | 6 (MEDIUM) |
| Reid et al., 2013 [17] | 2 | 2 | 3 | 0 | 7 (MEDIUM) |
| Rowlands et al., 2014 [25] | 1 | 1 | 3 | 0 | 5 (MEDIUM) |
| Aguilar-Farías et al., 2014 [8] | 1 | 1 | 3 | 2 | 7 (MEDIUM) |
| Godfrey et al., 2014 [30] | 1 | 1 | 3 | 0 | 5 (MEDIUM) |
| Mactier et al., 2014 [38] | 2 | 1 | 1 | 0 | 4 (LOW) |
| Salbach et al., 2014 [31] | 1 | 0 | 1 | 2 | 4 (LOW) |
| Davenport et al., 2015 [26] | 2 | 2 | 3 | 0 | 7 (MEDIUM) |
| Duncan et al., 2015 [40] | 1 | 2 | 3 | 2 | 8 (MEDIUM) |
| English et al., 2015 [39] | 1 | 1 | 2 | 1 | 5 (MEDIUM) |
| Gennuso et al., 2015 [32] | 1 | 1 | 1 | 0 | 3 (LOW) |
| Klenk et al., 2015 [33] | 2 | 2 | 3 | 0 | 7 (MEDIUM) |
| Kunkel et al., 2015 [18] | 1 | 1 | 3 | 1 | 6 (MEDIUM) |
| Stansfield et al., 2015 [41] | 1 | 0 | 3 | 0 | 4 (LOW) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, C.S.; Slaughter, S.E.; Jones, C.A.; Ickert, C.; Wagg, A.S. Measuring Activity Performance of Older Adults Using the activPAL: A Rapid Review. Healthcare 2017, 5, 94. https://doi.org/10.3390/healthcare5040094
Chan CS, Slaughter SE, Jones CA, Ickert C, Wagg AS. Measuring Activity Performance of Older Adults Using the activPAL: A Rapid Review. Healthcare. 2017; 5(4):94. https://doi.org/10.3390/healthcare5040094
Chicago/Turabian StyleChan, Charice S., Susan E. Slaughter, C. Allyson Jones, Carla Ickert, and Adrian S. Wagg. 2017. "Measuring Activity Performance of Older Adults Using the activPAL: A Rapid Review" Healthcare 5, no. 4: 94. https://doi.org/10.3390/healthcare5040094






