Age and Gender Differences in Psychological Distress among African Americans and Whites: Findings from the 2016 National Health Interview Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measures
2.2.1. Psychological Distress
2.2.2. Distress Interference
2.3. Analytic Approach
3. Results
3.1. Psychological Distress among Men and Women
3.2. Effects of Psychological Distress on Psychological Distress Interference
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Neighbors, H.; Trierweiler, S.; Ford, B.; Muroff, J. Racial differences in DSM diagnosis using a semi-structured instrument: The importance of clinical judgment in the diagnosis of African Americans. J. Health Soc. Behav. 2003, 44, 237–256. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.-L.T.; Manderscheid, R.W.; Walters, E.E.; Zaslavsky, A.M. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Maske, U.E.; Busch, M.A.; Jacobi, F.; Beesdo-Baum, K.; Seiffert, I.; Wittchen, H.U.; Riedel-Heller, S.; Hapke, U. Current major depressive syndrome measured with the patient health questionnaire-9 (PHQ-9) and the composite international diagnostic interview (CIDI): Results from a cross-sectional population-based study of adults in Germany. BMC Psychiatry 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Snowden, L.R. Bias in mental health assessment and intervention: Theory and evidence. Am. J. Public Health 2003, 93, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Villatoro, A.P.; Morales, E.S.; Mays, V.M. Family culture in mental health help-seeking and utilization in a nationally representative sample of Latinos in the United States: The NLAAS. Am. J. Orthopsychiatry 2014, 84, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, K.L.; Peterson, T.L.; Beecher, B. An exploration of mental health literacy among older African Americans. Aging Ment. Health 2013, 17, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.; Cheney, A.; Olson, M.; Haynes, T.; Bryant, K.; Cottoms, N.; Reaves, C.; Curran, G. Rural African Americans’ perspectives on mental health: Comparing focus groups and deliberative democracy forums. J. Health Care Poor Underserved 2017, 28, 548–565. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Yu, Y.; Jackson, J.S.; Anderson, N.B. Racial differences in physical and mental health, socio-economic status, stress and discrimination. J. Health Psychol. 1997, 2, 335–351. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, K.D.; Taylor, R.J.; Watkins, D.C.; Chatters, L. Correlates of psychological distress and major depressive disorder among African American men. Res. Soc. Work Pract. 2011, 21, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Neighbors, H.W.; Njai, R.; Jackson, J.S. Race, ethnicity, John Henryism, and depressive symptoms: The national survey of American life adult reinterview. Res. Hum. Dev. 2007, 4, 71–87. [Google Scholar] [CrossRef]
- Sue, S.; Chu, J.Y. The mental health of ethnic minority groups: Challenges posed by the supplement to the Surgeon General’s report on mental health. Cult. Med. Psychiatry 2003, 27, 447–465. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.M.; Bates, L.M. Do racial patterns in psychological distress shed light on the African American-White depression paradox? A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 913–928. [Google Scholar] [CrossRef] [PubMed]
- Decker, F.H. Occupational and non-occupational factors in job satisfaction and psychological distress among nurses. Res. Nurs. Health 1997, 20, 453–464. [Google Scholar] [CrossRef]
- Burnette, D.; Mui, A.C. Psychological well-being of the old-old Hispanics. J. Clin. Geropsychol. 1997, 3, 227–244. [Google Scholar]
- Muntaner, C.; Ng, E.; Vanroelen, C.S.; Phelan, J.C.; Bierman, A. Social stratification, social closure, and social class as determinants of mental health disparities. In Handbook of the Sociology of Mental Health, 2nd ed.; Aneshensel, C.S., Phelan, J.C., Bierman, A., Eds.; Springer: Dordrecht, The Netherlands, 2013; pp. 205–227. ISBN 978-94-007-4276-5. [Google Scholar]
- Earl, T.; Williams, D.; Anglade, S. An update on the mental health of Black Americans: Puzzling dilemmas and needed research. J. Black Psychol. 2011, 37, 485–498. [Google Scholar] [CrossRef]
- Jackson, J.S.; Knight, K.M.; Rafferty, J.A. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am. J. Public Health 2010, 100, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Sellers, S.L.; Bonham, V.; Neighbors, H.W.; Amell, J.W. Effects of racial discrimination and health behaviors on mental and physical health of middle-class African American men. Health Educ. Behav. 2009, 36, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R. The health of men: Structured inequalities and opportunities. Am. J. Public Health 2003, 93, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.N. Critical race theory speaks to the sociology of mental health: Mental health problems produced by racial stratification. J. Health Soc. Behav. 2003, 44, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.W.; Chatters, L.M.; Taylor, R.J.; Aranda, M.P.; Lincoln, K.D.; Thomas, C.S. Discrimination, serious psychological distress, and church-based emotional support among African American men across the life span. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017. [Google Scholar] [CrossRef] [PubMed]
- Somervell, P.D.; Leaf, P.J.; Weissman, M.M.; Blazer, D.G.; Bruce, M.L. The prevalence of major depression in Black and White adults in five United States communities. Am. J. Epidemiol. 1989, 130, 725–735. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Priest, N.; Anderson, N.B. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 2016, 4, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.J. More than Just Race: Being Black and Poor in the Inner City, 1st ed.; W.W. Norton & Company: New York, NY, USA, 2009; ISBN 978-039-333-763-1. [Google Scholar]
- Lincoln, K.D.; Taylor, R.J.; Chae, D.T.; Chatters, L.M. Demographic correlates of psychological well-being and distress among older African Americans and Caribbean African American adults. Best Pract. Ment. Health 2010, 6, 103–126. [Google Scholar] [PubMed]
- Watkins, D.C.; Hudson, D.L.; Caldwell, C.H.; Siefert, K.; Jackson, J.S. Discrimination, mastery, and depressive symptoms among African American men. Res. Soc. Work Pract. 2011, 21, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, A.V. Creating Mental Illness; University of Chicago Press: Chicago, IL, USA, 2002. [Google Scholar]
- Schwartz, S.; Meyer, I.H. Mental health disparities research: The impact of within and between group analyses on tests of social stress hypotheses. Soc. Sci. Med. 2010, 70, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.J. Health disparities and the stress hypothesis: A commentary on Schwartz and Meyer. Soc. Sci. Med. 2010, 70, 1119–1120. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Burgard, S.; Zivin, K. Long-term reciprocal associations between depressive symptoms and number of chronic medical conditions: Longitudinal support for Black-White health paradox. J. Racial Ethn. Health Disparities 2015, 2, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. The Black-White paradox in health: Flourishing in the face of social inequality and discrimination. J. Pers. 2009, 77, 1677–1706. [Google Scholar] [CrossRef] [PubMed]
- Mezuk, B.; Abdou, C.M.; Hudson, D.; Kershaw, K.N.; Rafferty, J.A.; Lee, H.; Jackson, J.S. “White Box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Soc. Ment. Health 2013, 3, 79–95. [Google Scholar] [CrossRef] [PubMed]
- Mouzon, D.M. Can family relationships explain the race paradox in mental health? J. Marriage Fam. 2013, 75, 470–485. [Google Scholar] [CrossRef]
- Parsons, V.L.; Moriarity, C.; Jonas, K.; Moore, T.F.; Davis, K.E.; Thompkins, L. Design and estimation for the National Health Interview Survey, 2006–2015. Available online: https://www.cdc.gov/nchs/data/series/sr_02/sr02_165.pdf (accessed on 15 November 2017).
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.T.; Walters, E.E.; Zaslavsky, A. Short screening scales to monitor population prevalances and trends in nonspecific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Sung, H.-Y.; Max, W.; Shi, Y.; Ong, M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int. J. Methods Psychiatr. Res. 2012, 21, 88–97. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. National Health Interview Survey, 2016. Public-Use Data File and Documentation. Available online: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm (accessed on 14 November 2017).
- Clarke, T.C.; Ward, B.W.; Norris, T.; Schiller, J.S. Early release of selected estimates based on data from the National Health Interview Survey, January–September 2016: Lack of health insurance coverage and type of coverage. Center for Disease Control and Prevention. 2017. Available online: https//www.cdc.gov/nchs/data/nhis/earlyreleaseZearlyrelease201702_01.pdf (accessed on 13 October 2017).
- Ryff, C.D.; Keyes, C.L.M.; Hughes, D.L. Psychological well-being in MIDUS: Profiles of ethnic/racial diversity and life-course uniformity. In How Healthy Are We? A National Study of Well-being at Midlife; Brim, O.G., Ryff, C.D., Kessler, R.C., Eds.; University of Chicago Press: Chicago, IL, USA, 2004; pp. 398–422. ISBN 9780226074771. [Google Scholar]
- Assari, S.; Lankarani, M.M. Association between stressful life events and depression; intersection of race and gender. J. Racial Ethn. Health Disparities 2016, 3, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M. Depressive symptoms are associated with more hopelessness among white than black older adults. Front. Public Health 2016, 4, 82. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M. Reciprocal associations between depressive symptoms and mastery among older adults; Black-White difference. Front. Public Health 2017, 8, 279. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.C. Depression over the adult life course for African American men: Toward a framework for research and practice. Am. J. Mens Health 2012, 6, 194–210. [Google Scholar] [CrossRef] [PubMed]
- Wester, S.R.; Vogel, D.L.; Wei, M.; McLain, R. African-American men, gender role conflict, and psychological distress: The role of racial identity. J. Couns. Dev. 2006, 84, 419–429. [Google Scholar] [CrossRef]
- Watkins, D.C.; Wharton, T.; Mitchell, J.A.; Matusko, N.; Kales, H. Perceptions and receptivity of non-spousal family support: A mixed methods study of psychological distress among older, church-going African American men. J. Mix Methods Res. 2017, 1, 487–509. [Google Scholar] [CrossRef] [PubMed]
- Brady, S.S.; Winston, W.; Gockley, S.E. Stress-related externalizing behavior among African American youth: How could policy and practice transform risk into resilience? J. Soc. Issues 2014, 70, 315–341. [Google Scholar] [CrossRef]
- Watkins, D.C.; Green, B.L.; Rivers, B.M.; Rowell, K.L. Depression and Black men: Implications for future research. J. Mens Health. Gend. 2006, 3, 227–235. [Google Scholar] [CrossRef]
- Watkins, D.C.; Walker, R.L.; Griffith, D.M. A meta-study of black male mental health and well-being. J. Black Psychol. 2010, 36, 303–330. [Google Scholar] [CrossRef]
- Woodard, A.T.; Taylor, R.J.; Chatters, L.M. Use of professional and informal support by Black men with mental disorders. Res. Soc. Work Pract. 2011, 21, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Moazen-Zadeh, E.; Assari, S. Depressive symptoms predict major depressive disorder after 15 years among Whites but not Blacks. Front. Public Health 2016, 13. [Google Scholar] [CrossRef] [PubMed]
| Age and Race Group | Men | Women | ||
|---|---|---|---|---|
| M | SD | M | SD | |
| Young White | 2.44 | 3.42 | 3.36 | 4.14 |
| Middle-Aged White | 2.55 | 3.97 | 3.10 | 4.19 |
| Older White | 2.02 | 3.52 | 2.66 | 3.95 |
| Young African American | 2.12 | 3.40 | 2.84 | 3.96 |
| Middle-Aged African American | 2.16 | 3.59 | 3.05 | 4.45 |
| Older African American | 2.23 | 3.87 | 2.35 | 3.76 |
| Total | 2.31 | 3.69 | 2.95 | 4.10 |
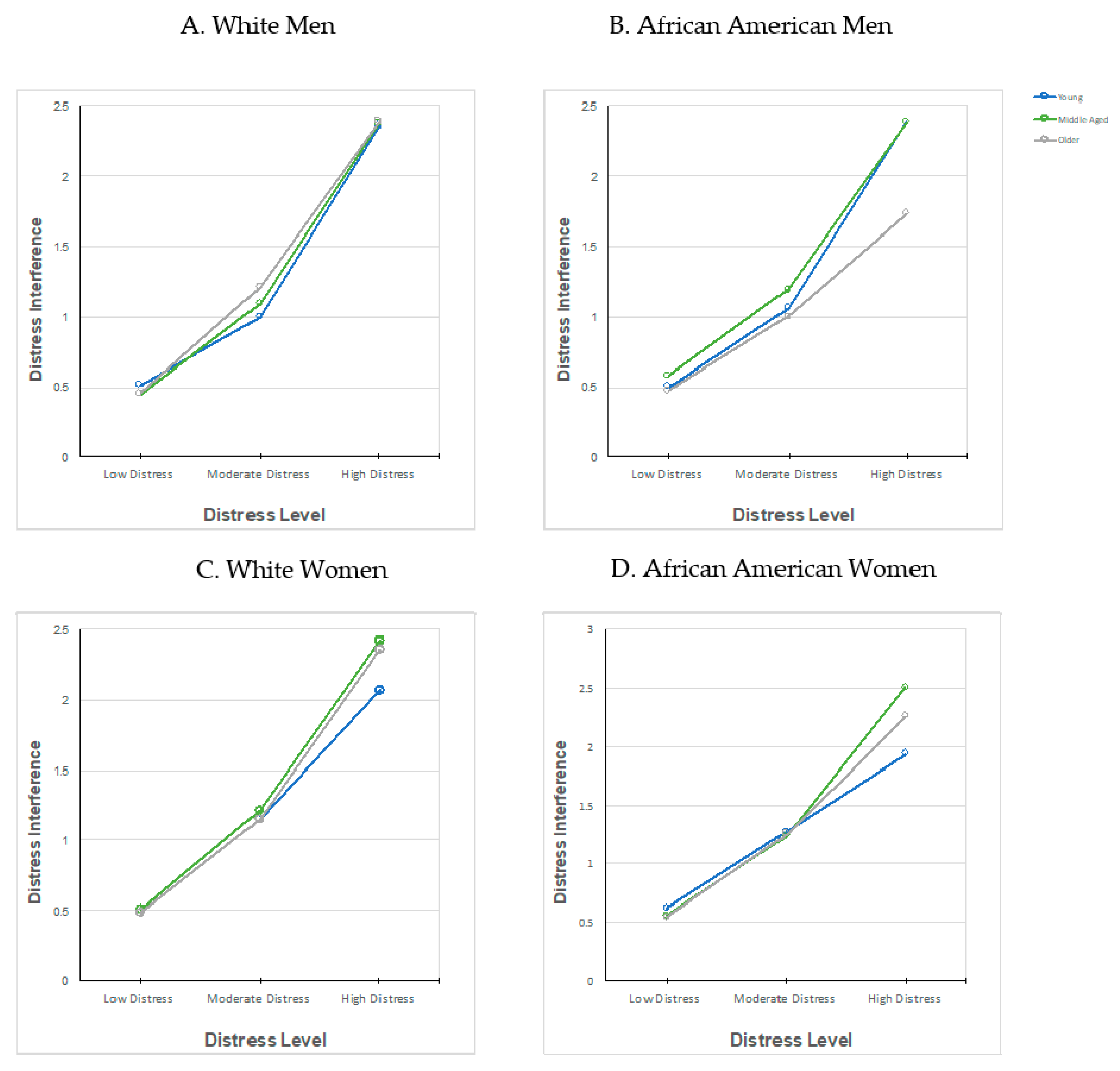
| Distress Level | Age Group | Race | Men | Women | ||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Low Distress | Young 18 to 30 | White | 0.51 | 0.73 | 0.49 | 0.65 |
| African American | 0.50 | 0.72 | 0.62 | 0.84 | ||
| Middle-Aged 31 to 54 | White | 0.45 | 0.74 | 0.51 | 0.73 | |
| African American | 0.58 | 0.78 | 0.56 | 0.82 | ||
| Older 55+ | White | 0.45 | 0.72 | 0.48 | 0.74 | |
| African American | 0.48 | 0.77 | 0.54 | 0.73 | ||
| Moderate Distress | Young 18 to 30 | White | 1.00 | 0.90 | 1.15 | 0.89 |
| African American | 1.06 | 0.97 | 1.27 | 1.01 | ||
| Middle-Aged 31 to 54 | White | 1.09 | 0.92 | 1.21 | 0.91 | |
| African American | 1.19 | 0.85 | 1.23 | 0.94 | ||
| Older 55+ | White | 1.21 | 0.92 | 1.14 | 0.92 | |
| African American | 1.00 | 0.93 | 1.25 | 0.90 | ||
| High Distress | Young 18 to 30 | White | 2.36 | 0.82 | 2.07 | 0.91 |
| African American | 2.39 | 0.74 | 1.93 | 0.95 | ||
| Middle-Aged 31 to 54 | White | 2.38 | 0.93 | 2.42 | 0.80 | |
| African American | 2.39 | 0.95 | 2.51 | 0.78 | ||
| Older 55+ | White | 2.39 | 0.84 | 2.36 | 0.84 | |
| African American | 1.73 | 1.05 | 2.25 | 1.02 | ||
| Men a | |||||
| Source | SS | df | MS | F | Eta Squared |
| Distress | 3,377,509.36 | 2 | 1,688,754.68 | 2,404,053.363 | 0.131 |
| Age | 29,066.81 | 2 | 14,533.407 | 20,689.26 | 0.001 |
| Race | 6814.66 | 1 | 6814.664 | 9701.12 | 0 |
| Distress × Age | 33,990.51 | 4 | 8497.627 | 12,096.93 | 0.002 |
| Distress × Race | 16,515.2 | 2 | 8257.599 | 11,755.24 | 0.001 |
| Age × Race | 54,799.86 | 2 | 27,399.93 | 39,005.6 | 0.002 |
| Distress × Age × Race | 26,929.89 | 4 | 6732.47 | 9584.12 | 0.001 |
| Error | 22,431,184.1 | 31,932,266 | 0.702 | ||
| Total | 60,876,378 | 31,932,284 | |||
| Women b | |||||
| Source | SS | df | MS | F | Eta Squared |
| Distress | 5,193,282.70 | 2 | 2,596,641.35 | 3,713,174.01 | 0.151 |
| Age | 54,433.97 | 2 | 27,216.99 | 38,920.05 | 0.002 |
| Race | 4233.26 | 1 | 4233.26 | 6053.52 | 0 |
| Distress × Age | 82,754.61 | 4 | 20,688.65 | 29,584.59 | 0.003 |
| Distress × Race | 8380.95 | 2 | 4190.47 | 5992.34 | 0 |
| Age × Race | 527.57 | 2 | 263.79 | 377.21 | 0 |
| Distress × Age × Race | 11,335.06 | 4 | 2833.76 | 4052.26 | 0 |
| Error | 29,271,196.26 | 41,857,550 | 0.7 | ||
| Total | 88,253,325 | 41,857,568 | |||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watkins, D.C.; Johnson, N.C. Age and Gender Differences in Psychological Distress among African Americans and Whites: Findings from the 2016 National Health Interview Survey. Healthcare 2018, 6, 6. https://doi.org/10.3390/healthcare6010006
Watkins DC, Johnson NC. Age and Gender Differences in Psychological Distress among African Americans and Whites: Findings from the 2016 National Health Interview Survey. Healthcare. 2018; 6(1):6. https://doi.org/10.3390/healthcare6010006
Chicago/Turabian StyleWatkins, Daphne C., and Natasha C. Johnson. 2018. "Age and Gender Differences in Psychological Distress among African Americans and Whites: Findings from the 2016 National Health Interview Survey" Healthcare 6, no. 1: 6. https://doi.org/10.3390/healthcare6010006





