Gravimetric Viral Diagnostics: QCM Based Biosensors for Early Detection of Viruses
Abstract
:1. Introduction
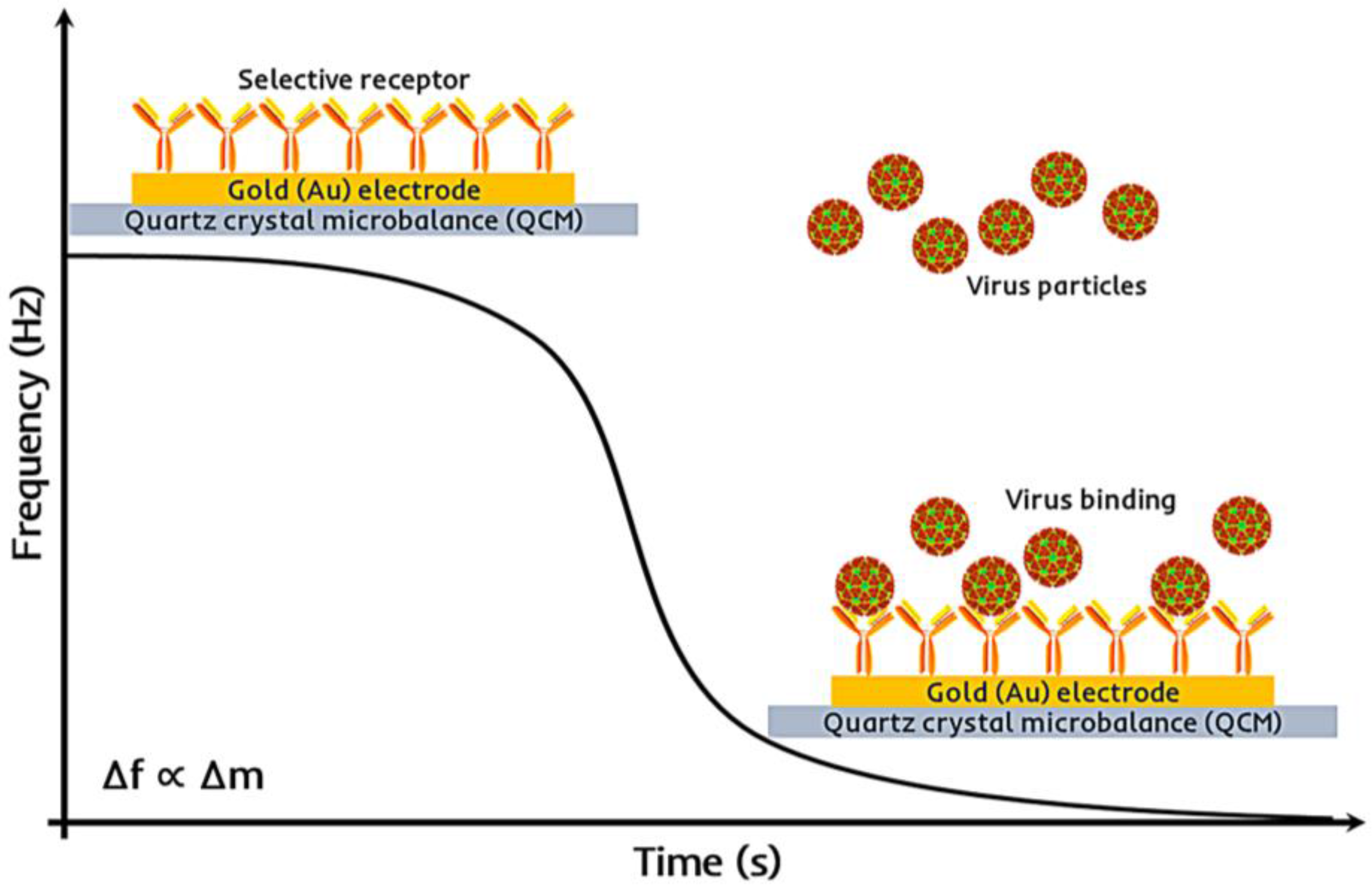
2. Quartz Crystal Microbalance: Transducer Design and Fabrication
3. Receptors for QCM Virus Sensors
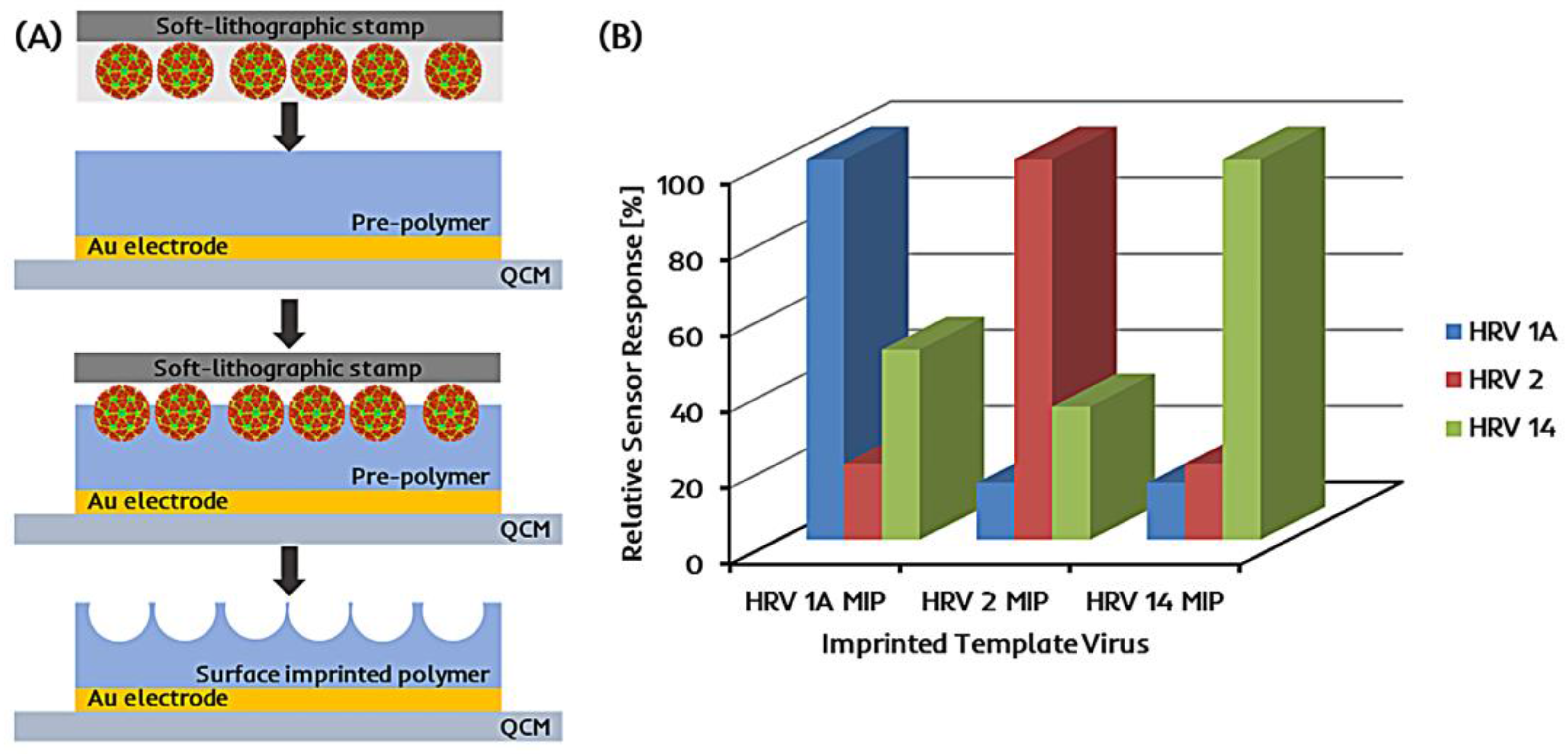
3.1. Synthetic Antibodies: Molecularly Imprinted Polymers for QCM Virus Sensors
3.1.1. Soft-Lithography
3.1.2. Epitope Imprinting
3.1.3. Plastic Antibody Replica
3.2. Natural Antibodies for QCM Virus Sensors
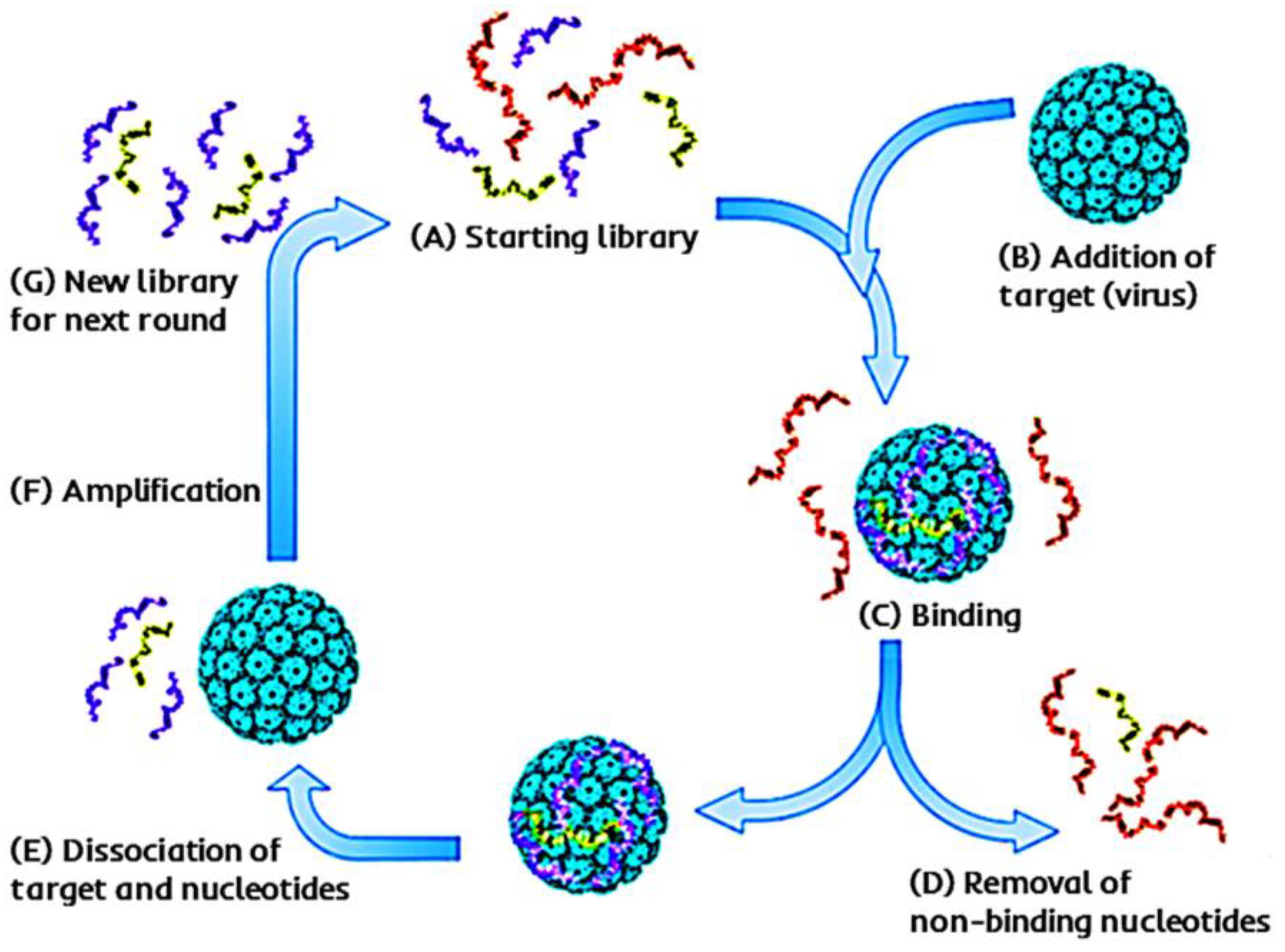
3.3. DNA and Aptamers for QCM Virus Sensors
3.3.1. DNA
3.3.2. Aptamers
4. Summary and Outlook
Acknowledgments
Author Contributions
Conflicts of Interest
References and note
- Wang, J. Electrochemical biosensors: Towards point-of-care cancer diagnostics. Biosens. Bioelectron. 2006, 21, 1887–1892. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Goryll, M.; Sin, L.Y.M.; Wong, P.K.; Chae, J. Microfluidic-based biosensors toward point-of-care detection of nucleic acids and proteins. Microfluid. Nanofluid. 2011, 10, 231–247. [Google Scholar] [CrossRef]
- Tokel, O.; Inci, F.; Demirci, U. Advances in Plasmonic Technologies for Point of Care Applications. Chem. Rev. 2014, 114, 5728–5752. [Google Scholar] [CrossRef] [PubMed]
- Wiedbrauk, D.L.; Farkas, D.H. Molecular Methods for Virus Detection; Academic Press, Inc.: San Diego, CA, USA, 1995. [Google Scholar]
- Mahony, J.B. Detection of Respiratory Viruses by Molecular Methods. Clin. Microbiol. Rev. 2008, 21, 716–747. [Google Scholar] [CrossRef] [PubMed]
- Jartti, T.; Söderlund-Venermo, M.; Hedman, K.; Ruuskanen, O.; Mäkelä, M.J. New molecular virus detection methods and their clinical value in lower respiratory tract infections in children. Paediatr. Respir. Rev. 2013, 14, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Boonham, N.; Kreuze, J.; Winter, S.; van der Vlugt, R.; Bergervoet, J.; Tomlinson, J.; Mumford, R. Methods in virus diagnostics: From ELISA to next generation sequencing. Virus Res. 2014, 186, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Ito, K.; Ishimori, Y. Microfabricated disposable DNA sensor for detection of hepatitis B virus DNA. Sens. Actuators B Chem. 1998, 46, 220–225. [Google Scholar] [CrossRef]
- Xu, C.; Feng, Y.; Chen, Y.; Gao, J.; Lu, Y. Rapid detection of measles virus using reverse transcription loop-mediated isothermal amplification coupled with a disposable lateral flow device. Diagn. Microbiol. Infect. Dis. 2016, 85, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Zhuo, M.; Zhang, X.; Xu, C.; Jiang, J.; Gao, F.; Wan, Q.; Li, Q.; Wang, T. Indium-tin-oxide thin film transistor biosensors for label-free detection of avian influenza virus H5N1. Anal. Chim. Acta 2013, 773, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-M.; Cen, Y.; Huang, L.-J.; Yu, R.-Q.; Chu, X. Upconversion fluorescence resonance energy transfer biosensor for sensitive detection of human immunodeficiency virus antibodies in human serum. Chem. Commun. 2014, 50, 4759–4762. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-H.; Lee, G.-Y.; Ko, H.; Chang, Y.W.; Kang, M.-J.; Pyun, J.-C. Development of SPR biosensor for the detection of human hepatitis B virus using plasma-treated parylene-N film. Biosens. Bioelectron. 2014, 56, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Altintas, Z.; Gittens, M.; Pocock, J.; Tothill, I.E. Biosensors for waterborne viruses: Detection and removal. Biochimie 2015, 115, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Diouani, M.F.; Helali, S.; Hafaid, I.; Hassen, W.M.; Snoussi, M.A.; Ghram, A.; Jaffrezic-Renault, N.; Abdelghani, A. Miniaturized biosensor for avian influenza virus detection. Mater. Sci. Eng. C 2008, 28, 580–583. [Google Scholar] [CrossRef]
- Bajwa, S.Z.; Mustafa, G.; Samardzic, R.; Wangchareansak, T.; Lieberzeit, P.A. Nanostructured materials with biomimetic recognition abilities for chemical sensing. Nanoscale Res. Lett. 2012, 7, 328. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Jiang, D.; Shao, J.; Sun, X. Magnetic molecularly imprinted polymer nanoparticles based electrochemical sensor for the measurement of Gram-negative bacterial quorum signaling molecules (N-acyl-homoserine-lactones). Biosens. Bioelectron. 2016, 75, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Dickert, F.L.; Hayden, O. Bioimprinting of Polymers and Sol-Gel Phases. Selective Detection of Yeasts with Imprinted Polymers. Anal. Chem. 2002, 74, 1302–1306. [Google Scholar] [CrossRef] [PubMed]
- Seidler, K.; Polreichová, M.; Lieberzeit, P.A.; Dickert, F.L. Biomimetic Yeast Cell Typing—Application of QCMs. Sensors 2009, 9, 8146–8157. [Google Scholar] [CrossRef] [PubMed]
- Seidler, K.; Lieberzeit, P.A.; Dickert, F.L. Application of yeast imprinting in biotechnology and process control. Analyst 2009, 134, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Idil, N.; Hedström, M.; Denizli, A.; Mattiasson, B. Whole cell based microcontact imprinted capacitive biosensor for the detection of Escherichia coli. Biosens. Bioelectron. 2017, 87, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Hayden, O.; Mann, K.-J.; Krassnig, S.; Dickert, F.L. Biomimetic ABO Blood-Group Typing. Angew. Chem. Int. Ed. 2006, 45, 2626–2629. [Google Scholar] [CrossRef] [PubMed]
- Mujahid, A.; Dickert, F.L. Blood Group Typing: From Classical Strategies to the Application of Synthetic Antibodies Generated by Molecular Imprinting. Sensors 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- Mujahid, A.; Aigner, S.; Dickert, F.L. Micro-structured interdigital capacitors with synthetic antibody receptors for ABO blood-group typing. Sens. Actuators B Chem. 2017, 242, 378–383. [Google Scholar] [CrossRef]
- Washburn, A.L.; Luchansky, M.S.; Bowman, A.L.; Bailey, R.C. Quantitative, Label-Free Detection of Five Protein Biomarkers Using Multiplexed Arrays of Silicon Photonic Microring Resonators. Anal. Chem. 2010, 82, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.; Gurbuz, Y.; Niazi, J.H. Biosensors for cardiac biomarkers detection: A review. Sens. Actuators B Chem. 2012, 171–172, 62–76. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.X.J.; Hoshino, K. Molecular Sensors and Nanodevices: Principles, Designs and Applications in Biomedical Engineering; Elsevier Science: Waltham, MA, USA, 2013. [Google Scholar]
- Heller, D.A.; Baik, S.; Eurell, T.E.; Strano, M.S. Single-Walled Carbon Nanotube Spectroscopy in Live Cells: Towards Long-Term Labels and Optical Sensors. Adv. Mater. 2005, 17, 2793–2799. [Google Scholar] [CrossRef]
- Lin, T.-Y.; Hu, C.-H.; Chou, T.-C. Determination of albumin concentration by MIP-QCM sensor. Biosens. Bioelectron. 2004, 20, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Li, G.; Ma, X.; Wang, Y.; Wu, G.; Cheng, Y. Polyaniline-TiO2 nano-composite-based trimethylamine QCM sensor and its thermal behavior studies. Sens. Actuators B Chem. 2008, 133, 374–380. [Google Scholar] [CrossRef]
- Mujahid, A.; Dickert, F.L. SAW and Functional Polymers. In Gas Sensing Fundamentals; Kohl, C.-D., Wagner, T., Eds.; Springer Series on Chemical Sensors and Biosensors; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Afzal, A.; Iqbal, N.; Mujahid, A.; Schirhagl, R. Advanced vapor recognition materials for selective and fast responsive surface acoustic wave sensors: A review. Anal. Chim. Acta 2013, 787, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Dickert, F.L.; Hayden, O.; Halikias, K.P. Synthetic receptors as sensor coatings for molecules and living cells. Analyst 2001, 126, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Mujahid, A.; Afzal, A.; Glanzing, G.; Leidl, A.; Lieberzeit, P.A.; Dickert, F.L. Imprinted sol-gel materials for monitoring degradation products in automotive oils by shear transverse wave. Anal. Chim. Acta 2010, 675, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Buttry, D.A.; Ward, M.D. Measurement of interfacial processes at electrode surfaces with the electrochemical quartz crystal microbalance. Chem. Rev. 1992, 92, 1355–1379. [Google Scholar] [CrossRef]
- Singh, A.K.; Singh, M. Molecularly imprinted Au-nanoparticle composite-functionalized EQCM sensor for l-serine. J. Electroanal. Chem. 2016, 780, 169–175. [Google Scholar] [CrossRef]
- Sauerbrey, G. Verwendung von Schwingquarzen zur Wägung dünner Schichten und zur Mikrowägung. Z. Phys. 1959, 155, 206–222. (In Deutsch) [Google Scholar] [CrossRef]
- Höök, F.; Kasemo, B.; Nylander, T.; Fant, C.; Sott, K.; Elwing, H. Variations in Coupled Water, Viscoelastic Properties, and Film Thickness of a Mefp-1 Protein Film during Adsorption and Cross-Linking: A Quartz Crystal Microbalance with Dissipation Monitoring, Ellipsometry, and Surface Plasmon Resonance Study. Anal. Chem. 2001, 73, 5796–5804. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, K.K.; Gordon, J.G. Frequency of a quartz microbalance in contact with liquid. Anal. Chem. 1985, 57, 1770–1771. [Google Scholar] [CrossRef]
- Sohna Sohna, J.E.; Cooper, M.A. Does the Sauerbrey equation hold true for binding of peptides and globular proteins to a QCM? A systematic study of mass dependence of peptide and protein binding with a piezoelectric sensor. Sens. Bio-Sens. Res. 2016, 11, 71–77. [Google Scholar] [CrossRef]
- Uttenthaler, E.; Schräml, M.; Mandel, J.; Drost, S. Ultrasensitive quartz crystal microbalance sensors for detection of M13-Phages in liquids. Biosens. Bioelectron. 2001, 16, 735–743. [Google Scholar] [CrossRef]
- Zeng, H.; Jiang, Y.; Xie, G.; Yu, J. Polymer coated QCM sensor with modified electrode for the detection of DDVP. Sens. Actuators B Chem. 2007, 122, 1–6. [Google Scholar] [CrossRef]
- Korposh, S.; Selyanchyn, R.; Lee, S.-W. Nano-assembled thin film gas sensors. IV. Mass-sensitive monitoring of humidity using quartz crystal microbalance (QCM) electrodes. Sens. Actuators B Chem. 2010, 147, 599–606. [Google Scholar] [CrossRef]
- Latif, U.; Mujahid, A.; Afzal, A.; Sikorski, R.; Lieberzeit, P.A.; Dickert, F.L. Dual and tetraelectrode QCMs using imprinted polymers as receptors for ions and neutral analytes. Anal. Bioanal. Chem. 2011, 400, 2507–2515. [Google Scholar] [CrossRef]
- Rodahl, M.; Höök, F.; Fredriksson, C.; Keller, C.A.; Krozer, A.; Brzezinski, P.; Voinova, M.; Kasemo, B. Simultaneous frequency and dissipation factor QCM measurements of biomolecular adsorption and cell adhesion. Faraday Discuss. 1997, 107, 229–246. [Google Scholar] [CrossRef]
- Marx, K.A. Quartz Crystal Microbalance: A Useful Tool for Studying Thin Polymer Films and Complex Biomolecular Systems at the Solution-Surface Interface. Biomacromolecules 2003, 4, 1099–1120. [Google Scholar] [CrossRef] [PubMed]
- Arnau, A. A Review of Interface Electronic Systems for AT-cut Quartz Crystal Microbalance Applications in Liquids. Sensors 2008, 8, 370–411. [Google Scholar] [CrossRef] [PubMed]
- Tuantranont, A.; Wisitsora-at, A.; Sritongkham, P.; Jaruwongrungsee, K. A review of monolithic multichannel quartz crystal microbalance: A review. Anal. Chim. Acta 2011, 687, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Haupt, K.; Linares, A.V.; Bompart, M.; Bui, B.T.S. Molecularly imprinted polymers. In Molecular Imprinting; Springer: Berlin, Germany, 2011; pp. 1–28. [Google Scholar]
- Li, S.; Ge, Y.; Piletsky, S.A.; Turner, A.P.F. A Zipper-Like On/Off-Switchable Molecularly Imprinted Polymer. Adv. Funct. Mater. 2011, 21, 3344–3349. [Google Scholar] [CrossRef]
- Haupt, K.; Mosbach, K. Molecularly imprinted polymers and their use in biomimetic sensors. Chem. Rev. 2000, 100, 2495–2504. [Google Scholar] [CrossRef] [PubMed]
- Bolisay, L.D.; Culver, J.N.; Kofinas, P. Optimization of Virus Imprinting Methods To Improve Selectivity and Reduce Nonspecific Binding. Biomacromolecules 2007, 8, 3893–3899. [Google Scholar] [CrossRef] [PubMed]
- Schirhagl, R. Bioapplications for molecularly imprinted polymers. Anal. Chem. 2014, 86, 250–261. [Google Scholar] [CrossRef] [PubMed]
- Mosbach, K. Molecular imprinting. Trends Biochem. Sci. 1994, 19, 9–14. [Google Scholar] [CrossRef]
- Sellergren, B. Important considerations in the design of receptor sites using noncovalent imprinting. Am. Chem. Soc. 1998, 703, 49–81. [Google Scholar]
- Wulff, G.; Biffis, A. Molecular imprinting with covalent or stoichiometric non-covalent interactions. Tech. Instrum. Anal. Chem. 2001, 23, 71–111. [Google Scholar]
- Sellergren, B. The non-covalent approach to molecular imprinting. Tech. Instrum. Anal. Chem. 2001, 23, 113–184. [Google Scholar]
- Dickert, F.L.; Hayden, O. Non-covalent molecularly imprinted sensors for vapours, polyaromatic hydrocarbons and complex mixtures. Tech. Instrum. Anal. Chem. 2001, 23, 503–525. [Google Scholar]
- Schirhagl, R.; Latif, U.; Podlipna, D.; Blumenstock, H.; Dickert, F.L. Natural and Biomimetic Materials for the Detection of Insulin. Anal. Chem. 2012, 84, 3908–3913. [Google Scholar] [CrossRef] [PubMed]
- Whitcombe, M.J.; Chianella, I.; Larcombe, L.; Piletsky, S.A.; Noble, J.; Porter, R.; Horgan, A. The rational development of molecularly imprinted polymer-based sensors for protein detection. Chem. Soc. Rev. 2011, 40, 1547–1571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickert, F.L.; Hayden, O. Molecular imprinting in chemical sensing. TrAC Trends Anal. Chem. 1999, 18, 192–199. [Google Scholar] [CrossRef]
- Mujahid, A.; Lieberzeit, P.A.; Dickert, F.L. Chemical sensors based on molecularly imprinted sol-gel materials. Materials 2010, 3, 2196–2217. [Google Scholar] [CrossRef]
- Mujahid, A.; Iqbal, N.; Latif, U. Molecularly Imprinted Polymers (MIPs): Virus Sensing Applications. In Encyclopedia of Biomedical Polymers and Polymeric Biomaterials; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Perez, N.; Alexander, C.; Vulfson, E.N. Surface imprinting of microorganisms. Tech. Instrum. Anal. Chem. 2001, 23, 295–304. [Google Scholar]
- Hayden, O.; Lieberzeit, P.A.; Blaas, D.; Dickert, F.L. Artificial Antibodies for Bioanalyte Detection—Sensing Viruses and Proteins. Adv. Funct. Mater. 2006, 16, 1269–1278. [Google Scholar] [CrossRef]
- Lieberzeit, P.A.; Gazda-Miarecka, S.; Halikias, K.; Schirk, C.; Kauling, J.; Dickert, F.L. Imprinting as a versatile platform for sensitive materials—Nanopatterning of the polymer bulk and surfaces. Sens. Actuators B Chem. 2005, 111–112, 259–263. [Google Scholar] [CrossRef]
- Jenik, M.; Schirhagl, R.; Schirk, C.; Hayden, O.; Lieberzeit, P.; Blaas, D.; Paul, G.; Dickert, F.L. Sensing Picornaviruses Using Molecular Imprinting Techniques on a Quartz Crystal Microbalance. Anal. Chem. 2009, 81, 5320–5326. [Google Scholar] [CrossRef] [PubMed]
- Wangchareansak, T.; Thitithanyanont, A.; Chuakheaw, D.; Paul Gleeson, M.; Lieberzeit, P.; Sangma, C. A novel approach to identify molecular binding to the influenza virus H5N1: Screening using molecularly imprinted polymers (MIPs). MedChemComm 2014, 5, 617–621. [Google Scholar] [CrossRef]
- Tai, D.-F.; Lin, C.-Y.; Wu, T.-Z.; Chen, L.-K. Recognition of dengue virus protein using epitope-mediated molecularly imprinted film. Anal. Chem. 2005, 77, 5140–5143. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.-H.; Zhang, Y.; Tang, S.-F.; Fang, Z.-B.; Yang, H.-H.; Chen, X.; Chen, G.-N. Sensing HIV related protein using epitope imprinted hydrophilic polymer coated quartz crystal microbalance. Biosens. Bioelectron. 2012, 31, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Schirhagl, R.; Lieberzeit, P.A.; Dickert, F.L. Chemosensors for Viruses Based on Artificial Immunoglobulin Copies. Adv. Mater. 2010, 22, 2078–2081. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Whitesides, G.M. Soft lithography. Annu. Rev. Mater. Sci. 1998, 28, 153–184. [Google Scholar] [CrossRef]
- Mujahid, A.; Iqbal, N.; Afzal, A. Bioimprinting strategies: From soft lithography to biomimetic sensors and beyond. Biotechnol. Adv. 2013, 31, 1435–1447. [Google Scholar] [CrossRef] [PubMed]
- Kane, R.S.; Takayama, S.; Ostuni, E.; Ingber, D.E.; Whitesides, G.M. Patterning proteins and cells using soft lithography. Biomaterials 1999, 20, 2363–2376. [Google Scholar] [CrossRef]
- Kryscio, D.R.; Peppas, N.A. Critical review and perspective of macromolecularly imprinted polymers. Acta Biomater. 2012, 8, 461–473. [Google Scholar] [CrossRef] [PubMed]
- Qin, D.; Xia, Y.; Whitesides, G.M. Soft lithography for micro-and nanoscale patterning. Nat. Protoc. 2010, 5, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Dickert, F.L.; Hayden, O.; Lieberzeit, P.; Haderspoeck, C.; Bindeus, R.; Palfinger, C.; Wirl, B. Nano- and micro-structuring of sensor materials—From molecule to cell detection. Synth. Met. 2003, 138, 65–69. [Google Scholar] [CrossRef]
- Hayden, O.; Bindeus, R.; Haderspöck, C.; Mann, K.-J.; Wirl, B.; Dickert, F.L. Mass-sensitive detection of cells, viruses and enzymes with artificial receptors. Sens. Actuators B Chem. 2003, 91, 316–319. [Google Scholar] [CrossRef]
- Wangchareansak, T.; Thitithanyanont, A.; Chuakheaw, D.; Gleeson, M.P.; Lieberzeit, P.A.; Sangma, C. Influenza A virus molecularly imprinted polymers and their application in virus sub-type classification. J. Mater. Chem. B 2013, 1, 2190–2197. [Google Scholar] [CrossRef]
- Ge, Y.; Turner, A.P.F. Too large to fit? Recent developments in macromolecular imprinting. Trends Biotechnol. 2008, 26, 218–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rachkov, A.; Minoura, N. Towards molecularly imprinted polymers selective to peptides and proteins. The epitope approach. Biochim. Biophys. Acta BBA Protein Struct. Mol. Enzymol. 2001, 1544, 255–266. [Google Scholar] [CrossRef]
- Nishino, H.; Huang, C.-S.; Shea, K.J. Selective protein capture by epitope imprinting. Angew. Chem. Int. Ed. 2006, 45, 2392–2396. [Google Scholar] [CrossRef] [PubMed]
- Hansen, D.E. Recent developments in the molecular imprinting of proteins. Biomaterials 2007, 28, 4178–4191. [Google Scholar] [CrossRef] [PubMed]
- Tai, D.-F.; Lin, C.-Y.; Wu, T.-Z.; Huang, J.-H.; Shu, P.-Y. Artificial Receptors in Serologic Tests for the Early Diagnosis of Dengue Virus Infection. Clin. Chem. 2006, 52, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Piletsky, S.A.; Turner, N.W.; Laitenberger, P. Molecularly imprinted polymers in clinical diagnostics—Future potential and existing problems. Med. Eng. Phys. 2006, 28, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhao, M.; Yang, Y. Molecular Imprinting Technique for Biomimetic Sensing and Diagnostics. In Biomedical Nanomaterials; Zhao, Y., Shen, Y., Eds.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2016. [Google Scholar]
- Schirhagl, R.; Podlipna, D.; Lieberzeit, P.A.; Dickert, F.L. Comparing biomimetic and biological receptors for insulin sensing. Chem. Commun. 2010, 46, 3128. [Google Scholar] [CrossRef] [PubMed]
- Ochsenbein, A.F.; Zinkernagel, R.M. Natural antibodies and complement link innate and acquired immunity. Immunol. Today 2000, 21, 624–630. [Google Scholar] [CrossRef]
- Cheng, X.; Chen, G.; Rodriguez, W.R. Micro- and nanotechnology for viral detection. Anal. Bioanal. Chem. 2009, 393, 487–501. [Google Scholar] [CrossRef] [PubMed]
- Caygill, R.L.; Blair, G.E.; Millner, P.A. A review on viral biosensors to detect human pathogens. Anal. Chim. Acta 2010, 681, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Uttenthaler, E.; Kößlinger, C.; Drost, S. Quartz crystal biosensor for detection of the African Swine Fever disease. Anal. Chim. Acta 1998, 362, 91–100. [Google Scholar] [CrossRef]
- Uttenthaler, E.; Kößlinger, C.; Drost, S. Characterization of immobilization methods for African swine fever virus protein and antibodies with a piezoelectric immunosensor1. Biosens. Bioelectron. 1998, 13, 1279–1286. [Google Scholar] [CrossRef]
- Makaraviciute, A.; Ruzgas, T.; Ramanavicius, A.; Ramanaviciene, A. A QCM-D Study of Reduced Antibody Fragments Immobilized on Planar Gold and Gold Nanoparticle Modified Sensor Surfaces. Key Eng. Mater. 2014, 605, 340–343. [Google Scholar] [CrossRef]
- Li, D.; Wang, J.; Wang, R.; Li, Y.; Abi-Ghanem, D.; Berghman, L.; Hargis, B.; Lu, H. A nanobeads amplified QCM immunosensor for the detection of avian influenza virus H5N1. Biosens. Bioelectron. 2011, 26, 4146–4154. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Xu, J.; Ji, H.-F.; Li, G.; Chen, H. Quartz crystal microbalance based biosensor for rapid and sensitive detection of maize chlorotic mottle virus. Anal. Methods 2014, 6, 4530–4536. [Google Scholar] [CrossRef]
- Kim, Y.K.; Lim, S.-I.; Cho, Y.-Y.; Choi, S.; Song, J.-Y.; An, D.-J. Detection of H3N2 canine influenza virus using a Quartz Crystal Microbalance. J. Virol. Methods 2014, 208, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-Q.; Shen, H.-X.; Cheng, Q.; Liu, L.-C. Sensitive electrogravimetric immunoassay of hepatitis B surface antigen through hyperbranched polymer bridge linked to multiple secondary antibodies. Chem. Pap. 2016, 70, 1031–1038. [Google Scholar] [CrossRef]
- HAU is a unit, which is commonly used to quantify avian influenza virus (AIV) sub-types. It is based on the hemagglutination assay (HA). It relies on the fact that hemagglutinin, a surface protein of AIV, agglutinates the red blood cells. HAU indicates at which dilution of virus solution, the agglutination takes place after incubating for one hour with 1% erythrocyte solution.
- Chu, X.; Zhao, Z.-L.; Shen, G.-L.; Yu, R.-Q. Quartz crystal microbalance immunoassay with dendritic amplification using colloidal gold immunocomplex. Sens. Actuators B Chem. 2006, 114, 696–704. [Google Scholar] [CrossRef]
- Yu, J.-S.; Liao, H.-X.; Gerdon, A.E.; Huffman, B.; Scearce, R.M.; McAdams, M.; Alam, S.M.; Popernack, P.M.; Sullivan, N.J.; Wright, D.; et al. Detection of Ebola virus envelope using monoclonal and polyclonal antibodies in ELISA, surface plasmon resonance and a quartz crystal microbalance immunosensor. J. Virol. Methods 2006, 137, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Lim, S.-I.; Choi, S.; Cho, I.-S.; Park, E.-H.; An, D.-J. A novel assay for detecting canine parvovirus using a quartz crystal microbalance biosensor. J. Virol. Methods 2015, 219, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Karpovich, D.S.; Blanchard, G.J. Direct Measurement of the Adsorption Kinetics of Alkanethiolate Self-Assembled Monolayers on a Microcrystalline Gold Surface. Langmuir 1994, 10, 3315–3322. [Google Scholar] [CrossRef]
- Tominaga, M.; Ohira, A.; Yamaguchi, Y.; Kunitake, M. Electrochemical, AFM and QCM studies on ferritin immobilized onto a self-assembled monolayer-modified gold electrode. J. Electroanal. Chem. 2004, 566, 323–329. [Google Scholar] [CrossRef]
- Lee, T.M.-H.; Li, L.-L.; Hsing, I.-M. Enhanced Electrochemical Detection of DNA Hybridization Based on Electrode-Surface Modification. Langmuir 2003, 19, 4338–4343. [Google Scholar] [CrossRef]
- Su, X.; Wu, Y.-J.; Robelek, R.; Knoll, W. Surface Plasmon Resonance Spectroscopy and Quartz Crystal Microbalance Study of Streptavidin Film Structure Effects on Biotinylated DNA Assembly and Target DNA Hybridization. Langmuir 2005, 21, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Giamblanco, N.; Conoci, S.; Russo, D.; Marletta, G. Single-step label-free hepatitis B virus detection by a piezoelectric biosensor. RSC Adv. 2015, 5, 38152–38158. [Google Scholar] [CrossRef]
- Yao, C.; Xiang, Y.; Deng, K.; Xia, H.; Fu, W. Sensitive and specific HBV genomic DNA detection using RCA-based QCM biosensor. Sens. Actuators B Chem. 2013, 181, 382–387. [Google Scholar] [CrossRef]
- Zhou, X.; Liu, L.; Hu, M.; Wang, L.; Hu, J. Detection of hepatitis B virus by piezoelectric biosensor. J. Pharm. Biomed. Anal. 2002, 27, 341–345. [Google Scholar] [CrossRef]
- Kleo, K.; Kapp, A.; Ascher, L.; Lisdat, F. Detection of vaccinia virus DNA by quartz crystal microbalance. Anal. Biochem. 2011, 418, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-R.; Jeong, H.-D.; Hong, S. QCM DNA biosensor for the diagnosis of a fish pathogenic virus VHSV. Talanta 2010, 82, 899–903. [Google Scholar] [CrossRef] [PubMed]
- Dell’Atti, D.; Zavaglia, M.; Tombelli, S.; Bertacca, G.; Cavazzana, A.O.; Bevilacqua, G.; Minunni, M.; Mascini, M. Development of combined DNA-based piezoelectric biosensors for the simultaneous detection and genotyping of high risk Human Papilloma Virus strains. Clin. Chim. Acta 2007, 383, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Eun, A.J.-C.; Huang, L.; Chew, F.-T.; Fong-Yau Li, S.; Wong, S.-M. Detection of two orchid viruses using quartz crystal microbalance-based DNA biosensors. Phytopathology 2002, 92, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Wang, L.; Callaway, Z.T.; Lu, H.; Huang, T.J.; Li, Y. A nanowell-based QCM aptasensor for rapid and sensitive detection of avian influenza virus. Sens. Actuators B Chem. 2017, 240, 934–940. [Google Scholar] [CrossRef]
- Brockman, L.; Wang, R.; Lum, J.; Li, Y. QCM Aptasensor for Rapid and Specific Detection of Avian Influenza Virus. Open J. Appl. Biosens. 2013, 2, 97–103. [Google Scholar] [CrossRef]
- Xu, L.; Wang, R.; Kelso, L.C.; Ying, Y.; Li, Y. A target-responsive and size-dependent hydrogel aptasensor embedded with QD fluorescent reporters for rapid detection of avian influenza virus H5N1. Sens. Actuators B Chem. 2016, 234, 98–108. [Google Scholar] [CrossRef]
- Wang, R.; Li, Y. Hydrogel based QCM aptasensor for detection of avian influenzavirus. Biosens. Bioelectron. 2013, 42, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Minunni, M.; Tombelli, S.; Gullotto, A.; Luzi, E.; Mascini, M. Development of biosensors with aptamers as bio-recognition element: The case of HIV-1 Tat protein. Biosens. Bioelectron. 2004, 20, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Skládal, P.; Riccardi, C.; dos, S.; Yamanaka, H.; da Costa, P.I. Piezoelectric biosensors for real-time monitoring of hybridization and detection of hepatitis C virus. J. Virol. Methods 2004, 117, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-H.; Chuang, Y.-C.; Lu, Y.-C.; Lin, H.-C.; Yang, Y.-L.; Lin, C.-S. A method of layer-by-layer gold nanoparticle hybridization in a quartz crystal microbalance DNA sensing system used to detect dengue virus. Nanotechnology 2009, 20, 215501. [Google Scholar] [CrossRef] [PubMed]
- Peterson, A.W.; Heaton, R.J.; Georgiadis, R.M. The effect of surface probe density on DNA hybridization. Nucleic Acids Res. 2001, 29, 5163–5168. [Google Scholar] [CrossRef] [PubMed]
- Boozer, C.; Ladd, J.; Chen, S.; Yu, Q.; Homola, J.; Jiang, S. DNA Directed Protein Immobilization on Mixed ssDNA/Oligo(ethylene glycol) Self-Assembled Monolayers for Sensitive Biosensors. Anal. Chem. 2004, 76, 6967–6972. [Google Scholar] [CrossRef] [PubMed]
- Wandtke, T.; Woźniak, J.; Kopiński, P. Aptamers in Diagnostics and Treatment of Viral Infections. Viruses 2015, 7, 751–780. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-C.; Chang, H.-T. Aptamer-based fluorescence sensor for rapid detection of potassium ions in urine. Chem. Commun. 2008, 12, 1461–1463. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, B.; Qi, Y.; Jin, Y. Label-free aptamer-based colorimetric detection of mercury ions in aqueous media using unmodified gold nanoparticles as colorimetric probe. Anal. Bioanal. Chem. 2009, 393, 2051–2057. [Google Scholar] [CrossRef] [PubMed]
- Jo, M.; Ahn, J.-Y.; Lee, J.; Lee, S.; Hong, S.W.; Yoo, J.-W.; Kang, J.; Dua, P.; Lee, D.; Hong, S.; et al. Development of Single-Stranded DNA Aptamers for Specific Bisphenol A Detection. Oligonucleotides 2011, 21, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Lubin, A.A.; Heeger, A.J.; Plaxco, K.W. Label-Free Electronic Detection of Thrombin in Blood Serum by Using an Aptamer-Based Sensor. Angew. Chem. 2005, 117, 5592–5595. [Google Scholar] [CrossRef]
- Shangguan, D.; Li, Y.; Tang, Z.; Cao, Z.C.; Chen, H.W.; Mallikaratchy, P.; Sefah, K.; Yang, C.J.; Tan, W. Aptamers evolved from live cells as effective molecular probes for cancer study. Proc. Natl. Acad. Sci. USA 2006, 103, 11838–11843. [Google Scholar] [CrossRef] [PubMed]
- Wiraja, C.; Yeo, D.; Lio, D.; Labanieh, L.; Lu, M.; Zhao, W.; Xu, C. Aptamer technology for tracking cells’ status & function. Mol. Cell. Ther. 2014, 2, 33. [Google Scholar] [PubMed]
- Fletcher, S.J.; Phillips, L.W.; Milligan, A.S.; Rodda, S.J. Toward specific detection of Dengue virus serotypes using a novel modular biosensor. Biosens. Bioelectron. 2010, 26, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Pavski, V.; Le, X.C. Detection of Human Immunodeficiency Virus Type 1 Reverse Transcriptase Using Aptamers as Probes in Affinity Capillary Electrophoresis. Anal. Chem. 2001, 73, 6070–6076. [Google Scholar] [CrossRef] [PubMed]
- Rahim Ruslinda, A.; Tanabe, K.; Ibori, S.; Wang, X.; Kawarada, H. Effects of diamond-FET-based RNA aptamer sensing for detection of real sample of HIV-1 Tat protein. Biosens. Bioelectron. 2013, 40, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Suh, S.-K.; Song, S.; Oh, H.-B.; Hwang, S.-H.; Hah, S.S. Aptamer-based competitive binding assay for one-step quantitation of hepatitis B surface antigen. Analyst 2014, 139, 4310–4314. [Google Scholar] [CrossRef] [PubMed]
- Binning, J.M.; Wang, T.; Luthra, P.; Shabman, R.S.; Borek, D.M.; Liu, G.; Xu, W.; Leung, D.W.; Basler, C.F.; Amarasinghe, G.K. Development of RNA aptamers targeting Ebola virus VP35. Biochemistry (Mosc.) 2013, 52, 8406–8419. [Google Scholar] [CrossRef] [PubMed]
- Shum, K.T.; Tanner, J.A. Differential Inhibitory Activities and Stabilisation of DNA Aptamers against the SARS Coronavirus Helicase. ChemBioChem 2008, 9, 3037–3045. [Google Scholar] [CrossRef] [PubMed]
- Jang, K.J.; Lee, N.-R.; Yeo, W.-S.; Jeong, Y.-J.; Kim, D.-E. Isolation of inhibitory RNA aptamers against severe acute respiratory syndrome (SARS) coronavirus NTPase/Helicase. Biochem. Biophys. Res. Commun. 2008, 366, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Escudero-Abarca, B.I.; Suh, S.H.; Moore, M.D.; Dwivedi, H.P.; Jaykus, L.-A. Selection, Characterization and Application of Nucleic Acid Aptamers for the Capture and Detection of Human Norovirus Strains. PLoS ONE 2014, 9, e106805. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.-R.; Hu, G.-Q.; Xue, X.-H.; Li, L.; Zheng, X.-X.; Gao, Y.-W.; Yang, S.-T.; Xia, X.-Z. Selection of an aptamer against rabies virus: A new class of molecules with antiviral activity. Virus Res. 2014, 184, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Nitsche, A.; Kurth, A.; Dunkhorst, A.; Pänke, O.; Sielaff, H.; Junge, W.; Muth, D.; Scheller, F.; Stöcklein, W.; Dahmen, C.; et al. One-step selection of Vaccinia virus-binding DNA aptamers by MonoLEX. BMC Biotechnol. 2007, 7, 48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yu, Z.; Jiang, F.; Fu, P.; Shen, J.; Wu, W.; Li, J. Two DNA Aptamers against Avian Influenza H9N2 Virus Prevent Viral Infection in Cells. PLoS ONE 2015, 10, e0123060. [Google Scholar] [CrossRef] [PubMed]
- Wongphatcharachai, M.; Wang, P.; Enomoto, S.; Webby, R.J.; Gramer, M.R.; Amonsin, A.; Sreevatsan, S. Neutralizing DNA Aptamers against Swine Influenza H3N2 Viruses. J. Clin. Microbiol. 2013, 51, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Shiratori, I.; Akitomi, J.; Boltz, D.A.; Horii, K.; Furuichi, M.; Waga, I. Selection of DNA aptamers that bind to influenza A viruses with high affinity and broad subtype specificity. Biochem. Biophys. Res. Commun. 2014, 443, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Ellington, A.D.; Szostak, J.W. In vitro selection of RNA molecules that bind specific ligands. Nature 1990, 346, 818–822. [Google Scholar] [CrossRef] [PubMed]
- Tuerk, C.; Gold, L. Systematic evolution of ligands by exponential enrichment: RNA ligands to bacteriophage T4 DNA polymerase. Science 1990, 249, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Iliuk, A.B.; Hu, L.; Tao, W.A. Aptamer in Bioanalytical Applications. Anal. Chem. 2011, 83, 4440–4452. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.J.; Lee, J.-W.; Ellington, A.D. Applications of Aptamers as Sensors. Annu. Rev. Anal. Chem. 2009, 2, 241–264. [Google Scholar] [CrossRef] [PubMed]
- Van den Kieboom, C.H.; van der Beek, S.L.; Mészáros, T.; Gyurcsányi, R.E.; Ferwerda, G.; de Jonge, M.I. Aptasensors for viral diagnostics. TrAC Trends Anal. Chem. 2015, 74, 58–67. [Google Scholar] [CrossRef] [Green Version]
- Leija-Montoya, A.G.; Benítez-Hess, M.L.; Alvarez-Salas, L.M. Application of Nucleic Acid Aptamers to Viral Detection and Inhibition. In Nucleic Acids—From Basic Aspects to Laboratory Tools, Edited by Marcelo L. Larramendy and Sonia Soloneski; InTech: Rijeka, Croatia, 2016; pp. 93–119. [Google Scholar]
- Kumar, P.K.R. Monitoring Intact Viruses Using Aptamers. Biosensors 2016, 6, 40. [Google Scholar] [CrossRef] [PubMed]
- Tombelli, S.; Mascini, M.; Braccini, L.; Anichini, M.; Turner, A.P. Coupling of a DNA piezoelectric biosensor and polymerase chain reaction to detect apolipoprotein E polymorphisms. Biosens. Bioelectron. 2000, 15, 363–370. [Google Scholar] [CrossRef]
- Tombelli, S.; Minunni, M.; Luzi, E.; Mascini, M. Aptamer-based biosensors for the detection of HIV-1 Tat protein. Bioelectrochemistry 2005, 67, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Zhang, L.; Liang, Z.; Zhang, Y. Protein-imprinted materials: Rational design, application and challenges. Anal. Bioanal. Chem. 2012, 403, 2173–2183. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.E.; Puleo, D.A. Protein binding to peptide-imprinted porous silica scaffolds. Chem. Eng. J. 2008, 137, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, A.D.; Hamuro, Y. Synthetic Antibody Mimics-Multiple Peptide Loops Attached to a Molecular Scaffold. US 5770380 A, 23 June 1998. [Google Scholar]
- Wu, A.M.; Senter, P.D. Arming antibodies: Prospects and challenges for immunoconjugates. Nat. Biotechnol. 2005, 23, 1137–1146. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Soontornworajit, B.; Wang, Y. A Temperature-Responsive Antibody-Like Nanostructure. Biomacromolecules 2010, 11, 2087–2093. [Google Scholar] [CrossRef] [PubMed]
- Eulberg, D.; Klussmann, S. Spiegelmers: Biostable Aptamers. ChemBioChem 2003, 4, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Pagratis, N.C.; Bell, C.; Chang, Y.-F.; Jennings, S.; Fitzwater, T.; Jellinek, D.; Dang, C. Potent 2′-amino-, and 2′-fluoro-2′- deoxyribonucleotide RNA inhibitors of keratinocyte growth factor. Nat. Biotechnol. 1997, 15, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Kusser, W. Chemically modified nucleic acid aptamers for in vitro selections: Evolving evolution. Rev. Mol. Biotechnol. 2000, 74, 27–38. [Google Scholar] [CrossRef]
- Schirhagl, R.; Ren, K.; Zare, R.N. Surface-imprinted polymers in microfluidic devices. Sci. Chin. Chem. 2012, 55, 469–483. [Google Scholar] [CrossRef]
- Potyrailo, R.A.; Conrad, R.C.; Ellington, A.D.; Hieftje, G.M. Adapting Selected Nucleic Acid Ligands (Aptamers) to Biosensors. Anal. Chem. 1998, 70, 3419–3425. [Google Scholar] [CrossRef] [PubMed]





| Receptor | Template/Target | Polymer | Detection Limit | Reference |
|---|---|---|---|---|
| Soft-lithographically (surface) imprinted MIP | TMV | Polyurethane | 8 ng/mL | [64] |
| PPOV | Polyurethane | 5 × 105 virus particles/mL | [65] | |
| HRV 1A, HRV 2, HRV 14 | Polyurethane | 100 µg/mL | [66] | |
| H5N1, H5N3, H1N1, H1N3, H6N1 | Poly(acrylamide-co-methacrylic acid-co-methylmethacrylate-co-N-vinylpyrrolidone) with N,N-(1,2-dihydroxyethylene)bisacrylamide | 105 particles/mL | [67] | |
| Epitope imprinted MIP | Dengue virus NS1 protein | Poly(acrylic acid-co-acrylamide) with ethyleneglycol dimethylacrylate | 1 µg/L | [68] |
| HIV-1 GP41 | Polydopamine | 2 ng/mL | [69] | |
| Plastic antibody replica | HRV 14 | Poly(vinylpyrrolidone-co-methacrylic acid) with N,N′-(1,2-dihydroxyethylene)bisacrylamide | 2.5 × 1012 virus particles/mL | [70] |
| Receptor | Target | Fabrication/Immobilization Method | Detection Limit | Reference |
|---|---|---|---|---|
| Anti-H5 NAb | AIV H5N1 | Anti-H5 attached to nanobeads immobilized on 16-mercaptohexadecanoic acid monolayer | 0.128 HAU | [93] |
| Anti-MCMV NAb | MCMV | 3-mercaptopropanoic acid and 11-mercaptoundecanoic acid (10:1 ratio) crosslinked with anti-MCMV | 250 ng/mL | [94] |
| Monoclonal anti-CIV NP antibody | CIV H3N2 | ProLinker™ B immobilized anti-CIV monoclonal antibody | 14 nM | [95] |
| Secondary antibodies | HepBV | Secondary antibodies linked through carboxylated hyper-branched polymer | 2 ng/mL | [96] |
| Receptor | Target | Fabrication/Immobilization Method | Detection Limit | Reference |
|---|---|---|---|---|
| Immobilized DNA probe | HepBV | Thiolated-ssDNA probe | 1 f.mol/cm2 | [105] |
| Thiolated-DNA probe | 104 copies/mL | [106] | ||
| DNA immobilized via poly(ethyleneamine)-glutaraldehyde method | 0.01 µg/mL | [107] | ||
| Vaccinia virus | Biotinylated-DNA immobilized via NeutrAvidin protein | 1 nM | [108] | |
| VHSV | Biotinylated-DNA immobilized via avidin | 0.0016 µM | [109] | |
| HPV | Biotinylated-oligonucleotides immobilized via streptavidin | 30 nM | [110] | |
| CymMV and ORSV | Mercaptohexyl modified ssDNA-CymMV coat proteins and ssDNA-ORSV coat proteins | 0.05 ng/µL | [111] | |
| Immobilized aptamer | AIV H5N1 | Thiolated aptamer | 2 HAU | [112] |
| Streptavidin-biotin complexation plus particle label for amplification | 1 HAU | [113] | ||
| Aptamer embedded in hydrogel | 0.4 HAU | [114] | ||
| Aptamer embedded in hydrogel | 0.0128 HAU | [115] | ||
| HIV-1 Tat protein | Thiol monolayer and streptavidin-biotin complexation | 0.25 ppm | [116] |
| Technique | Detection Principle | Time | Cost | Remarks |
|---|---|---|---|---|
| Viral plaque assay | Measuring virus infective particles | Lengthy | Inexpensive | Conventional, Simple, Poor reproducibility |
| Hemagglutination assay | Virus protein assay | Lengthy | Inexpensive | Conventional, Simple, Poor reproducibility |
| Immunofluorescence assay | Virus protein assay | Moderately fast | Expensive | Modern, Sensitive, Poor reproducibility |
| ELISA | Virus Protein Binding with Enzymes | Rapid | Inexpensive | Modern, Highly Sensitive, Good reproducibility |
| PCR | Nucleic Acid Amplification | Rapid | Inexpensive | Modern, Highly Sensitive, Excellent reproducibility |
| Virus Flow Cytometry | Biophysical method of counting virus particles | Rapid | Expensive | Modern, Highly Sensitive, Excellent reproducibility |
| QCM gravimetric Sensor | Selective binding of virus particles or proteins | Fast | Inexpensive | Simple and reversible, Good reproducibility, Highly sensitive and selective |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afzal, A.; Mujahid, A.; Schirhagl, R.; Bajwa, S.Z.; Latif, U.; Feroz, S. Gravimetric Viral Diagnostics: QCM Based Biosensors for Early Detection of Viruses. Chemosensors 2017, 5, 7. https://doi.org/10.3390/chemosensors5010007
Afzal A, Mujahid A, Schirhagl R, Bajwa SZ, Latif U, Feroz S. Gravimetric Viral Diagnostics: QCM Based Biosensors for Early Detection of Viruses. Chemosensors. 2017; 5(1):7. https://doi.org/10.3390/chemosensors5010007
Chicago/Turabian StyleAfzal, Adeel, Adnan Mujahid, Romana Schirhagl, Sadia Zafar Bajwa, Usman Latif, and Saima Feroz. 2017. "Gravimetric Viral Diagnostics: QCM Based Biosensors for Early Detection of Viruses" Chemosensors 5, no. 1: 7. https://doi.org/10.3390/chemosensors5010007








