Parent and Child Report of Pain and Fatigue in JIA: Does Disagreement between Parent and Child Predict Functional Outcomes?
Abstract
:1. Introduction
2. Methods
2.1. Electronic Diary Variables
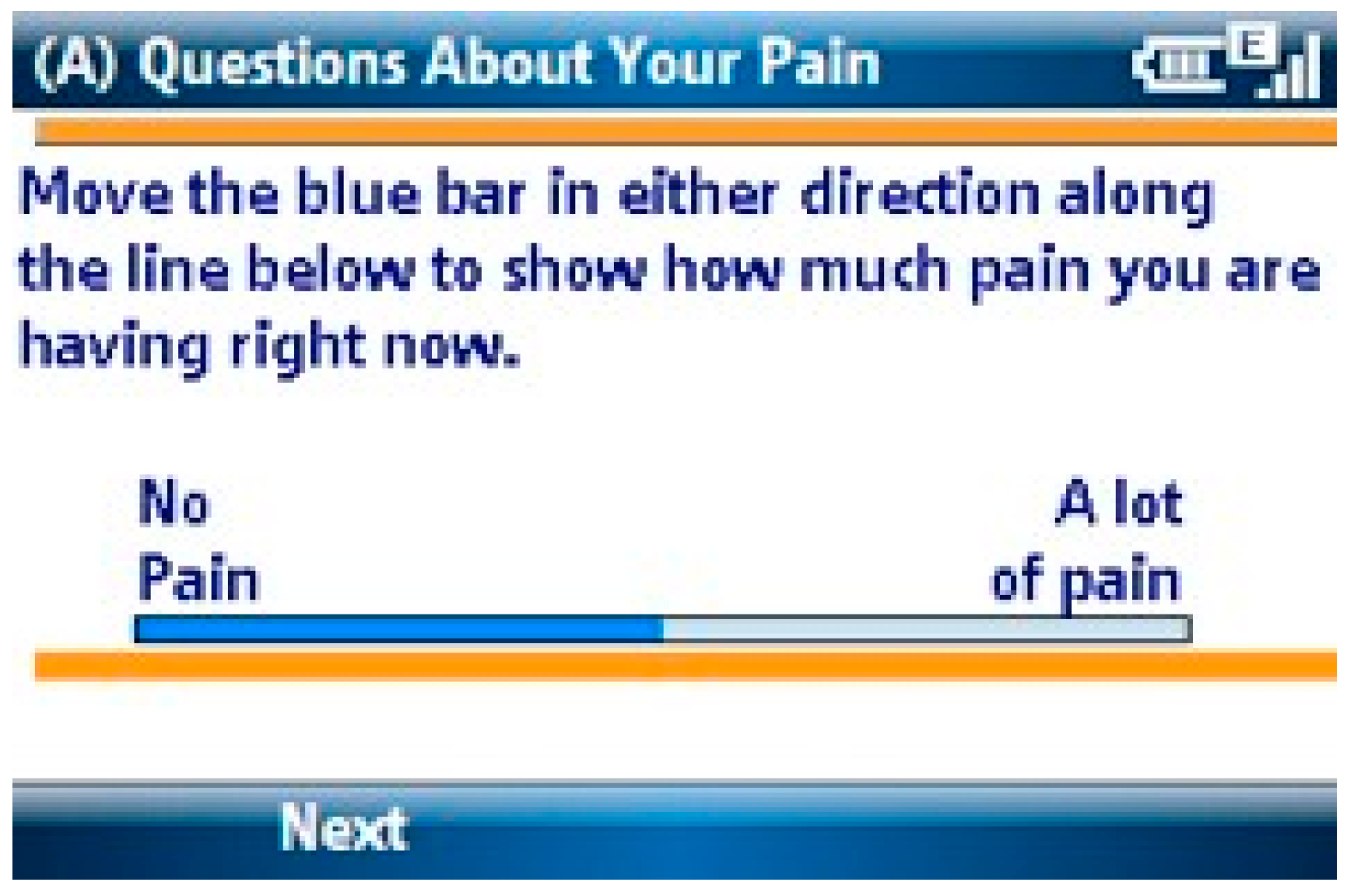
2.1.1. Pain Intensity
2.1.2. Fatigue Intensity
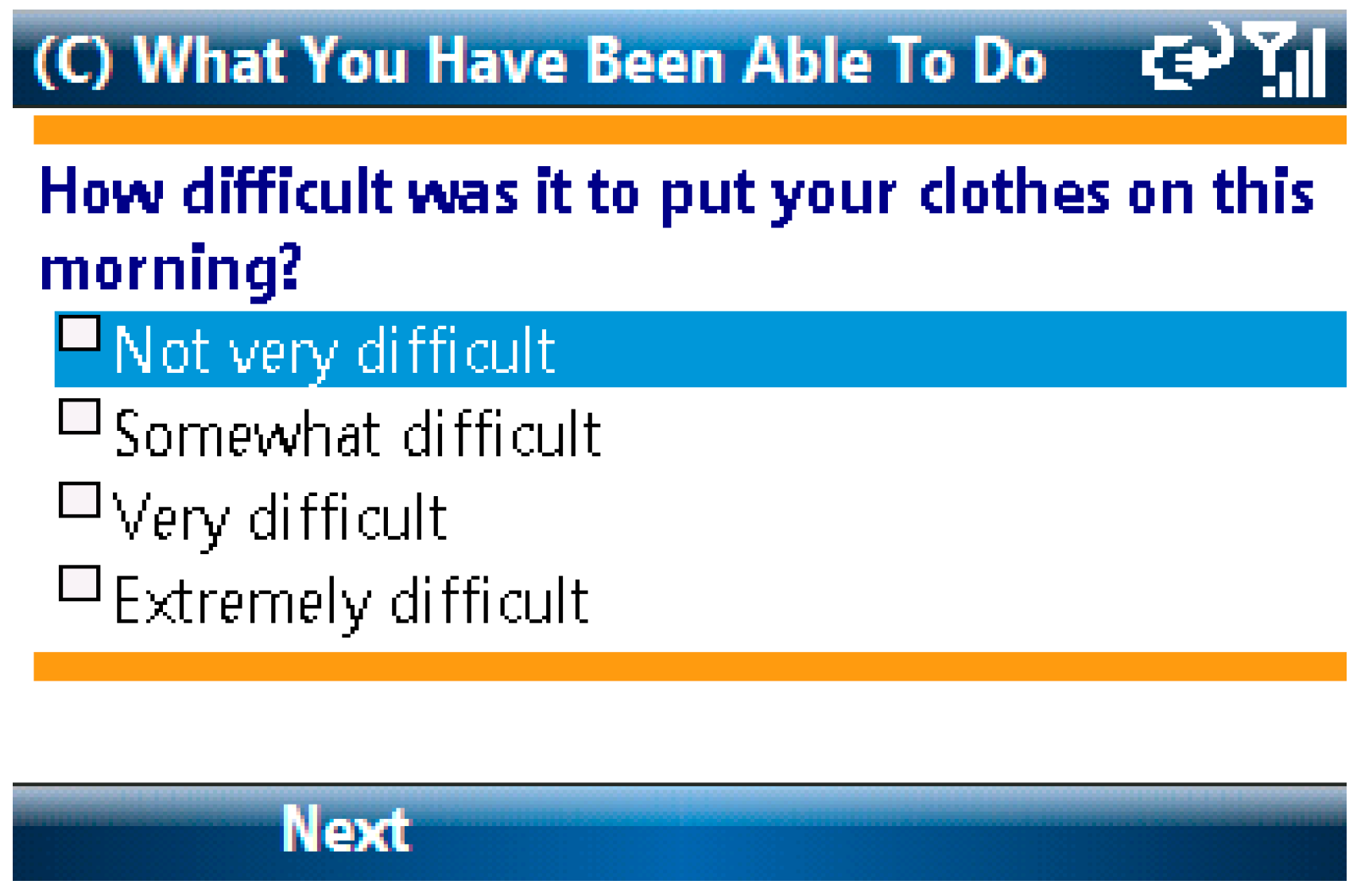
2.1.3. Activity Limitations
2.1.4. Negative Mood
2.2. Data Analysis Plan
3. Results
3.1. Descriptive Statistics
3.1.1. Demographics
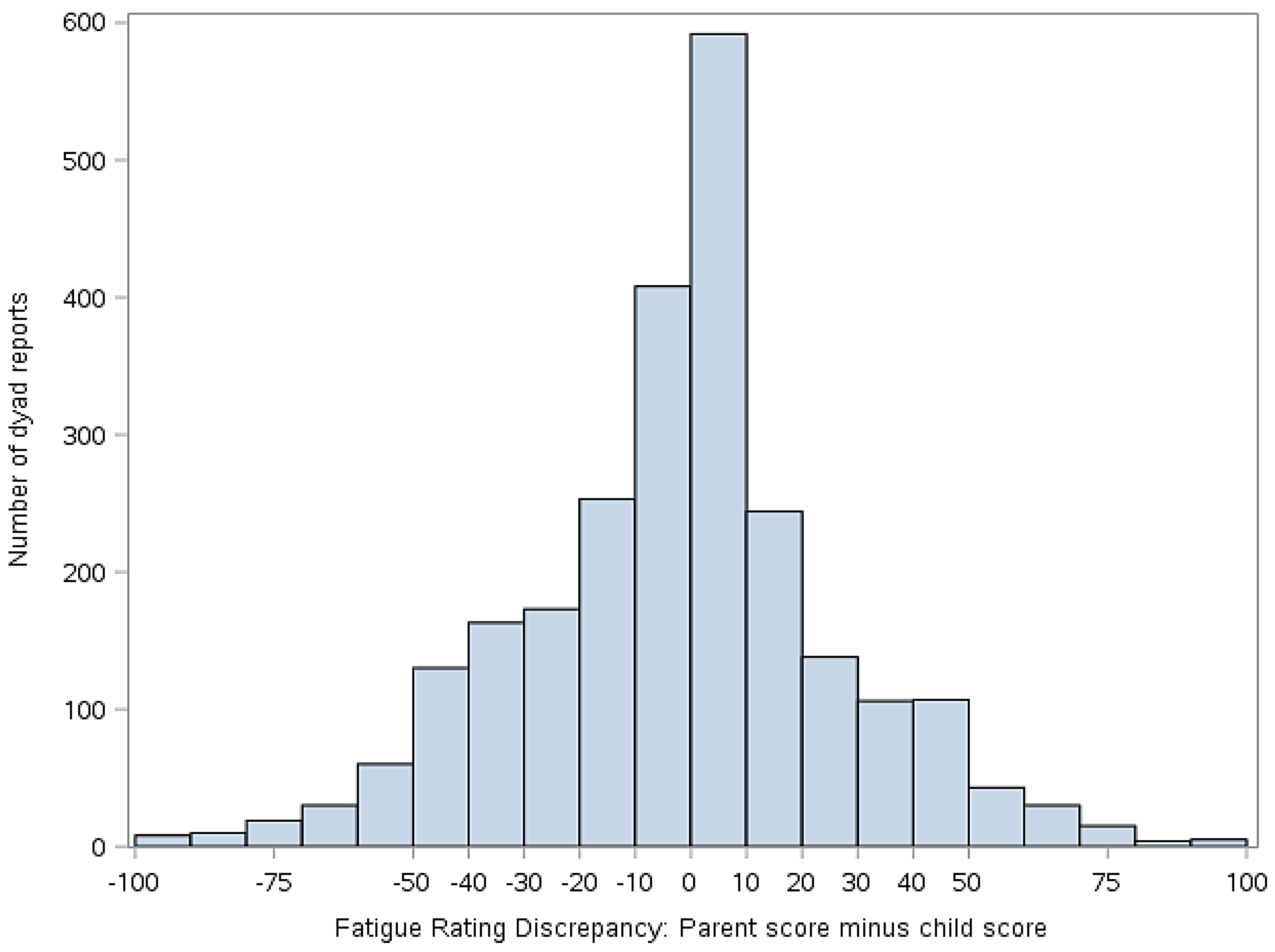
3.1.2. Discrepancies between Child and Parent Report of Pain and Fatigue
3.2. Hypothesis Testing
3.2.1. Parent-Child Discrepancies in Pain Intensity and Fatigue Reports as a Predictor of Mood
3.2.3. Parent-Child Discrepancy in Pain Intensity and Fatigue Reports as a Predictor of Activity Limitation
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Schanberg, L.E.; Sandstrom, M.J. Causes of pain in children with arthritis. Rheum. Dis. Clin. N. Am. 1999, 1, 31–53. [Google Scholar] [CrossRef]
- Gutierrez-Suarez, R.; Pistorio, A.; Cespedes, C.; Norambuena, X.; Flato, B.; Rumba, I.; Harjacek, M.; Nielsen, S.; Susic, G.; Mihaylova, D.; et al. For Pediatric Rheumatology International Trials Organisation (PRINTO). Health-related quality of life of patients with juvenile idiopathic arthritis coming from 3 different geographic areas. The PRINTO multinational quality of life cohort study. Rheumatology 2007, 46, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Chambers, C.T. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain 2005, 119, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Sztajnbok, F.; Coronel-Martinez, D.L.; Diaz-Maldonado, A.; Novarini, C.; Pistorio, A.; Viola, S.; Ruperto, N.; Buoncompagni, A.; Martini, A.; Ravelli, A. Discordance between physician’s and parent’s global assessments in juvenile idiopathic arthritis. Rheumatology 2007, 46, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Munitis, P.I.; Bandeira, M.; Pistorio, A.; Magni-Manzoni, S.; Ruperto, N.; Schivo, A.; Martini, A.; Ravelli, A. Level of agreement between children, parents, and physicians in rating pain intensity in juvenile idiopathic arthritis. Arthritis Rheum. 2006, 55, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Zebracki, K.; Cox, S.; Newman, A.J.; Singer, N.G. Juvenile idiopathic arthritis: Parent-child discrepancy on reports of pain and disability. J. Rheumatol. 2004, 31, 1840–1846. [Google Scholar] [PubMed]
- Stone, A.A.; Shiffman, S. Ecological momentary assessment: Measuring real world processes in behavioral medicine. Ann. Behav. Med. 1994, 16, 199–202. [Google Scholar]
- Claar, R.L.; Guite, J.W.; Kaczynski, K.J.; Logan, D.E. Factor structure of the Adult Responses to Children’s Symptoms: Validation in children and adolescents with diverse chronic pain conditions. Clin. J. Pain 2010, 26, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Guite, J.W.; McCue, R.L.; Sherker, J.L.; Sherry, D.D.; Rose, J.B. Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: The mediating role of pain catastrophizing. Clin. J. Pain 2011, 27, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Claar, R.L.; Logan, D.L. Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J. Pediatr. Psychol. 2008, 33, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Bromberg, M.H.; Connelly, M.; Anthony, K.K.; Gil, K.M.; Schanberg, L.E. Prospective mediation models of sleep, pain, and daily function in children with arthritis using ecological momentary assessment. Clin. J. Pain 2016, 32, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.; Bromberg, M.H.; Anthony, K.K.; Gill, K.M.; Franks, L.; Schanberg, L.E. Emotion regulation predicts pain and functioning in children with juvenile idiopathic arthritis: An electronic diary study. J. Pediatr. Psychol. 2012, 37, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Bromberg, M.H.; Connelly, M.; Anthony, K.K.; Gil, K.M.; Schanberg, L.E. Self-reported pain and disease symptoms persist in juvenile idiopathic arthritis despite treatment advances: An electronic diary study. Arthritis Rheumatol. 2014, 66, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.; Anthony, K.K.; Sarniak, R.; Bromberg, M.H.; Gil, K.M.; Schanberg, L.E. Parent pain responses as predictors of daily activities and mood in children with juvenile idiopathic arthritis: The utility of electronic diaries. J. Pain Symptom Manag. 2010, 39, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.N.; Stevens, B.J.; Feldman, B.M.; Streiner, D.L.; McGrath, P.J.; Dupuis, A. Using an electronic pain diary to better understand pain in children and adolescents with arthritis. Pain Manag. 2011, 1, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.A.; Hicks, G.; Nino-Murcia, G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991, 36, 291–298. [Google Scholar] [CrossRef]
- Palermo, T.M.; Witherspoon, D.; Valenzuela, D.; Drotar, D.D. Development and validation of the Child Activity Limitations Interview: A measure of pain-related functional impairment in school-age children and adolescents. Pain 2004, 109, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Young, N.L.; Williams, J.I.; Yoshida, K.K.; Wright, J.G. Measurement properties of the activities scale for kids. J. Clin. Epidemiol. 2000, 53, 125–137. [Google Scholar] [CrossRef]
- Laurent, J.; Salvatore, J.; Catanzaro, T.E.; Joiner, K.D.; Rudolph, K.I.; Potter, S.L.; Osborne, L.; Gathright, T. A measure of positive and negative affect for children: Scale development and preliminary validation. Psychol. Assess. 1999, 11, 326–338. [Google Scholar] [CrossRef]
- Watson, W.; Lee, A.C.; Carey, G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J. Abnorm. Psychol. 1998, 97, 346–353. [Google Scholar] [CrossRef]
- Claar, R.L.; Simons, L.E.; Logan, D. Parental response to children’s pain: The moderating impact of children’s emotional distress on symptoms and disability. Pain 2008, 138, 172–179. [Google Scholar] [CrossRef] [PubMed]
- El-Najjar, A.R.; Negm, M.G.; El-Sayed, W.M. The relationship between depression, disease activity and physical function in juvenile idiopathic arthritis patients in Zagazig University Hospitals—Egypt. Egypt. Rheumatol. 2014, 36, 145–150. [Google Scholar] [CrossRef]
- Normura, Y.; Wickramaratne, P.J.; Warner, V.; Weissman, M. Family discord, parental depression and psychopathology in offspring: Ten-year follow-up. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Östlie, I.L.; Aasland, A.; Johansson, I.; Flatö, B.; Möller, A. A longitudinal follow-up study of physical and psychosocial health in young adults with chronic childhood arthritis. Clin. Exp. Rheumatol. 2009, 27, 1039–1046. [Google Scholar] [PubMed]
- Schanberg, L.E.; Anthony, K.K.; Gil, K.M.; Maurin, E.C. Daily Pain and Symptoms in Children with Polyarticular Arthritis. Arthritis Rheum. 2003, 48, 1390–1397. [Google Scholar] [CrossRef] [PubMed]
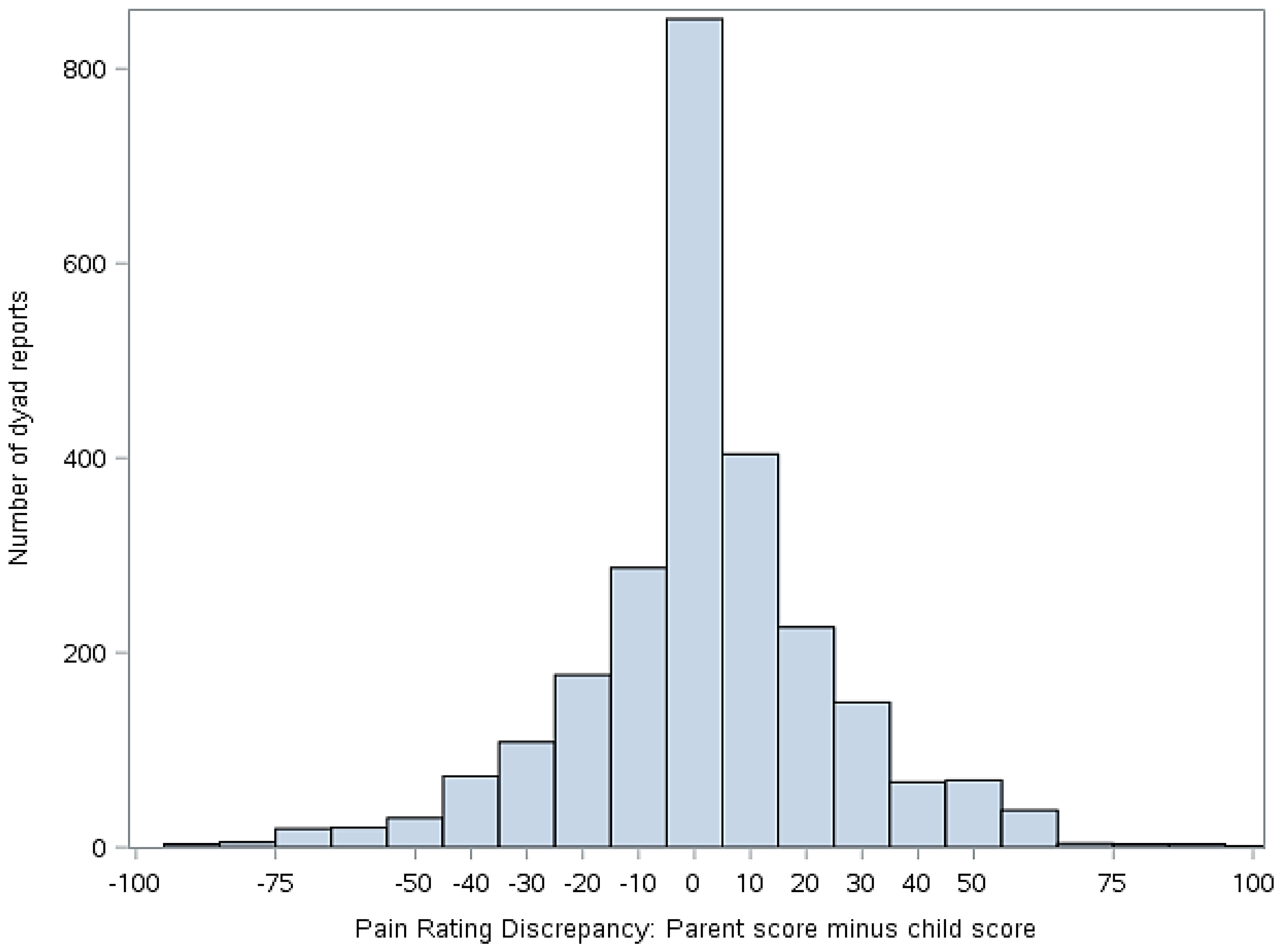
| Discrepancy Group (Parent Score-Child Score) | Dyad Reports n (%) (N 1 = 2537) |
|---|---|
| High Discrepancy (−100 to −51, child rated higher) | 177 (7.0%) |
| Moderate Discrepancy (−50 to −11, child rated higher) | 467 (18.4%) |
| Low Discrepancy (−10 to 9, parent and child rated similarly) 2 | 1172 (46.2%) |
| Moderate Discrepancy (10 to 49, parent rated higher) | 640 (25.2%) |
| High Discrepancy (50 to 100, parent rated higher) | 81 (3.2%) |
| Discrepancy Group (Parent Score-Child Score) | Dyad Reports n (%) (N 1 = 2411) |
|---|---|
| High Discrepancy (−100 to −51, child rated higher) 2 | 0 |
| Moderate Discrepancy (−50 to −11, child rated higher) | 719 (29.8%) |
| Low Discrepancy (−10 to 9, parent and child rated similarly) 3 | 1000 (41.5%) |
| Moderate Discrepancy (10 to 49, parent rated higher) | 595 (24.7%) |
| High Discrepancy (50 to 100, parent rated higher) | 97 (4.0%) |
| Predictor variable: Discrepancy Group 1 (Parent Score-Child Score, Pain) | Estimate | Standard Error | p-Value |
|---|---|---|---|
| High Discrepancy (−100 to −51, child rated higher) | 0.074 | 0.030 | 0.014 |
| Moderate Discrepancy (−50 to −11, child rated higher) | 0.001 | 0.020 | 0.964 |
| Moderate Discrepancy (10 to 49, parent rated higher) | 0.017 | 0.019 | 0.373 |
| High Discrepancy (50 to 100, parent rated higher) | 0.011 | 0.045 | 0.813 |
| Predictor Variable: Discrepancy Group 1 (Parent Score-Child Score, Fatigue) | Estimate | Standard Error | p-Value |
|---|---|---|---|
| High Discrepancy (−100 to −51, child rated higher) 2 | - | - | - |
| Moderate Discrepancy (−50 to −11, child rated higher) | 0.056 | 0.017 | 0.002 |
| Moderate Discrepancy (10 to 49, parent rated higher) | 0.016 | 0.019 | 0.397 |
| High Discrepancy (50 to 100, parent rated higher) | 0.113 | 0.038 | 0.003 |
| Predictor Variable: Discrepancy Group 1 (Parent Score-Child Score, Pain) | Estimate | Standard Error | p-Value |
|---|---|---|---|
| High Discrepancy (−100 to −51, child rated higher) | 1.097 | 0.538 | 0.043 |
| Moderate Discrepancy (−50 to −11, child rated higher) | 0.277 | 0.368 | 0.452 |
| Moderate Discrepancy (10 to 49, parent rated higher) | −0.037 | 0.354 | 0.916 |
| High Discrepancy (50 to 100, parent rated higher) | −1.471 | 0.820 | 0.075 |
| Predictor Variable: Discrepancy Group 1 (Parent Score-Child Score, Fatigue) | Estimate | Standard Error | p-Value |
|---|---|---|---|
| High Discrepancy (−100 to −51, child rated higher) 2 | - | - | - |
| Moderate Discrepancy (−50 to −11, child rated higher) | −0.796 | 0.328 | 0.016 |
| Moderate Discrepancy (10 to 49, parent rated higher) | −0.230 | 0.350 | 0.512 |
| High Discrepancy (50 to 100, parent rated higher) | −1.179 | 0.704 | 0.096 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaultney, A.C.; Bromberg, M.H.; Connelly, M.; Spears, T.; Schanberg, L.E. Parent and Child Report of Pain and Fatigue in JIA: Does Disagreement between Parent and Child Predict Functional Outcomes? Children 2017, 4, 11. https://doi.org/10.3390/children4020011
Gaultney AC, Bromberg MH, Connelly M, Spears T, Schanberg LE. Parent and Child Report of Pain and Fatigue in JIA: Does Disagreement between Parent and Child Predict Functional Outcomes? Children. 2017; 4(2):11. https://doi.org/10.3390/children4020011
Chicago/Turabian StyleGaultney, Amy C., Maggie H. Bromberg, Mark Connelly, Tracy Spears, and Laura E. Schanberg. 2017. "Parent and Child Report of Pain and Fatigue in JIA: Does Disagreement between Parent and Child Predict Functional Outcomes?" Children 4, no. 2: 11. https://doi.org/10.3390/children4020011





