Immersive Virtual Reality for Pediatric Pain
Abstract
:1. Introduction
2. Review of Virtual Reality in Pediatrics
2.1. Acute and Procedural Pain
2.2. Chronic Pain
2.3. Other Applications
3. Qualities of Virtual Reality
3.1. Presence
3.2. Interactivity
3.3. Social Interactions in Virtual Reality
3.4. Customization
3.5. Embodiment
4. Practical Aspects of Virtual Reality: Hardware and Software
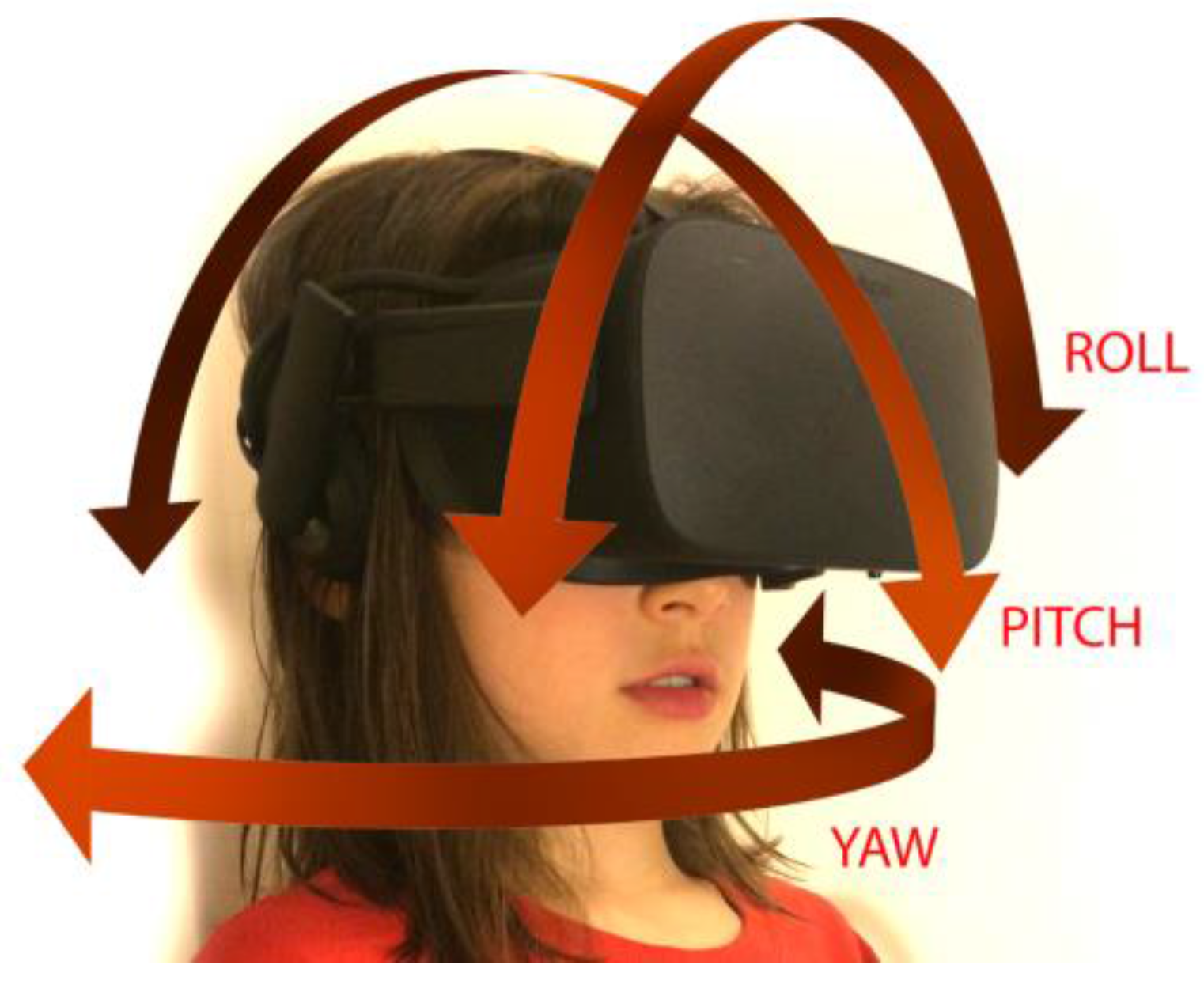
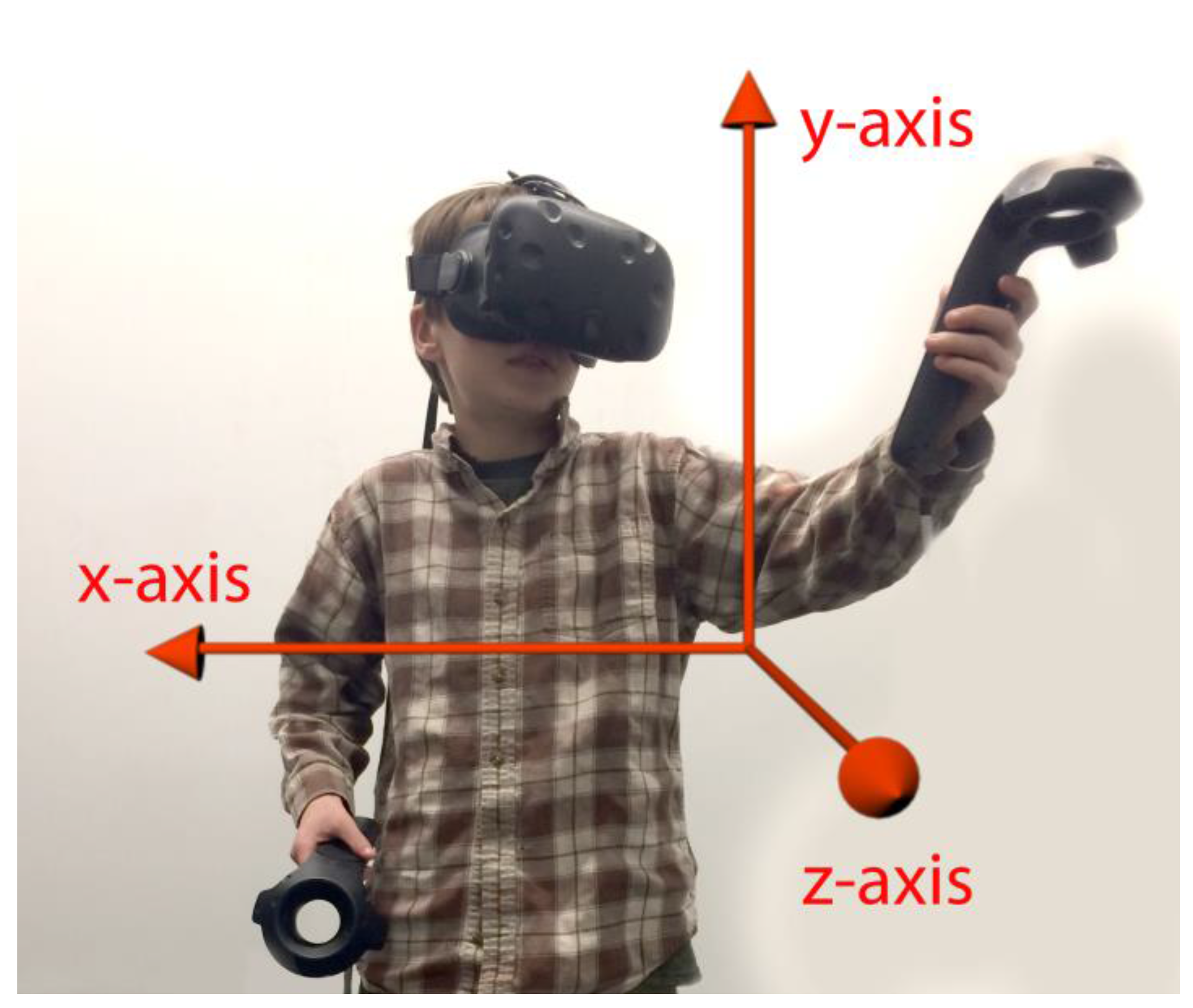
4.1. Tracking Movement
4.2. Hardware Issues to Consider for Children
4.3. Virtual Content
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Cummings, J.J.; Bailenson, J.N. How immersive is enough? A meta-analysis of the effect of immersive technology on user presence. Media Psychol. 2016, 19, 272–309. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Doctor, J.N.; Patterson, D.R.; Carrougher, G.J.; Furness, T.A., III. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 2000, 85, 305–309. [Google Scholar] [CrossRef]
- Human Photonics Laboratory. Available online: www.Vrpain.com (accessed on 7 March 2017).
- Schmitt, Y.S.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R.; Jensen, M.P.; Soltani, M.; Carrougher, G.J.; Nakamura, D.; Sharar, S.R. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns 2011, 37, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Jeffs, D.; Dorman, D.; Brown, S.; Files, A.; Graves, T.; Kirk, E.; Meredith-Neve, S.; Sanders, J.; White, B.; Swearingen, C.J. Effect of virtual reality on adolescent pain during burn wound care. J. Burn Care Res. 2014, 35, 395–408. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.J.; Kimble, R.M.; Rodger, S.; Ware, R.S.; Cuttle, L. Play and heal: Randomized controlled trial of Ditto™ intervention efficacy on improving re-epithelialization in pediatric burns. Burns 2014, 40, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.; Rodger, S.; Bucolo, S.; Greer, R.; Kimble, R.M. Multi-modal distraction. Using technology to combat pain in young children with burn injuries. Burns 2010, 36, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Pardesi, O.; Fuzaylov, G. Pain management in pediatric burn patients: Review of recent literature and future directions. J. Burn Care Res. 2017. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Meyer, W.J., III; Ramirez, M.; Roberts, L.; Seibel, E.J.; Atzori, B.; Sharar, S.R.; Patterson, D.R. Feasibility of articulated arm mounted Oculus Rift Virtual Reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.I.; Kim, S.H.; Kant, A.J.; Joseph, M.H.; Rizzo, A.S. Effectiveness of virtual reality for pediatric pain distraction during IV placement. CyberPsychol. Behav. 2006, 9, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.L.; Baker, C.M. Pain in children: comparison of assessment scales. Pediatr. Nurs. 1988, 14, 9–17. [Google Scholar] [PubMed]
- Nilsson, S.; Finnström, B.; Kokinsky, E.; Enskär, K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur. J. Oncol. Nurs. 2009, 13, 102–109. [Google Scholar] [CrossRef] [PubMed]
- He, H.G.; Zhu, L.; Chan, S.W.C.; Liam, J.L.W.; Li, H.C.W.; Ko, S.S.; Klainin-Yobas, P.; Wang, W. Therapeutic play intervention on children’s perioperative anxiety, negative emotional manifestation and postoperative pain: A randomized controlled trial. J. Adv. Nurs. 2015, 71, 1032–1043. [Google Scholar] [CrossRef] [PubMed]
- Shahrbanian, S.; Ma, X.; Aghaei, N.; Korner-Bitensky, N.; Moshiri, K.; Simmonds, M.J. Use of virtual reality (immersive vs. non immersive) for pain management in children and adults: A systematic review of evidence from randomized controlled trials. Eur. J. Exp. Biol. 2012, 2, 1408–1422. [Google Scholar]
- Ramachandran, V.S.; Rogers-Ramachandran, D. Synaesthesia in phantom limbs induced with mirrors. Proc. Biol. Sci. 1996, 263, 377–386. [Google Scholar] [CrossRef] [PubMed]
- McCabe, C.; Haigh, R.; Ring, E.; Halligan, P.; Wall, P.; Blake, D. A controlled pilot study of the utility of mirror visual feedback in the treatment of complex regional pain syndrome (type 1). Rheumatology 2003, 42, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Fukumori, S.; Matsusaki, T.; Maruo, T.; Ishikawa, S.; Nishie, H.; Takata, K.; Mizuhara, H.; Mizobuchi, S.; Nakatsuka, H. Nonimmersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: An open-label pilot study. Pain Med. 2010, 11, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Harvie, D.S.; Broecker, M.; Smith, R.T.; Meulders, A.; Madden, V.J.; Moseley, G.L. Bogus visual feedback alters onset of movement-evoked pain in people with neck pain. Psychol. Sci. 2015, 26, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.B.; Sesto, M.E.; Ponto, K.; Leonard, J.; Mason, A.; Vanderheiden, G.; Williams, J.; Radwin, R.G. Use of virtual reality feedback for patients with chronic neck pain and kinesiophobia. IEEE Trans. Neural Syst. Rehabil. Eng. 2016. [Google Scholar] [CrossRef] [PubMed]
- Won, A.S.; Tataru, C.A.; Cojocaru, C.M.; Krane, E.J.; Bailenson, J.N.; Niswonger, S.; Golianu, B. Two virtual reality pilot studies for the treatment of pediatric CRPS. Pain Med. 2015, 16, 1644–1647. [Google Scholar] [CrossRef] [PubMed]
- Lebel, A.; Becerra, L.; Wallin, D.; Moulton, E.; Morris, S.; Pendse, G.; Jasciewicz, J.; Stein, M.; Aiello-Lammens, M.; Grant, E. fMRI reveals distinct CNS processing during symptomatic and recovered complex regional pain syndrome in children. Brain 2008, 131, 1854–1879. [Google Scholar] [CrossRef] [PubMed]
- Becerra, L.; Sava, S.; Simons, L.E.; Drosos, A.M.; Sethna, N.; Berde, C.; Lebel, A.A.; Borsook, D. Intrinsic brain networks normalize with treatment in pediatric complex regional pain syndrome. NeuroImage Clin. 2014, 6, 347–369. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.; Pielech, M.; Erpelding, N.; Linnman, C.; Moulton, E.; Sava, S.; Lebel, A.; Serrano, P.; Sethna, N.; Berde, C. The responsive amygdala: Treatment-induced alterations in functional connectivity in pediatric complex regional pain syndrome. Pain 2014, 155, 1727–1742. [Google Scholar] [CrossRef] [PubMed]
- Makin, T.R.; Scholz, J.; Henderson Slater, D.; Johansen-Berg, H.; Tracey, I. Reassessing cortical reorganization in the primary sensorimotor cortex following arm amputation. Brain 2015, 138, 2140–2146. [Google Scholar] [CrossRef] [PubMed]
- Walz, A.D.; Usichenko, T.; Moseley, G.L.; Lotze, M. Graded motor imagery and the impact on pain processing in a case of CRPS. Clin. J. Pain 2013, 29, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Reid, D. Virtual reality in pediatric neurorehabilitation: Attention deficit hyperactivity disorder, autism and cerebral palsy. Neuroepidemiology 2011, 36, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Weiss, P.L.; Tirosh, E.; Fehlings, D. Role of virtual reality for cerebral palsy management. J. Child Neurol. 2014, 29, 1119–1124. [Google Scholar] [CrossRef] [PubMed]
- Biffi, E.; Beretta, E.; Cesareo, A.; Maghini, C.; Turconi, A.C.; Reni, G.; Strazzer, S. An immersive virtual reality platform to enhance walking ability of children with acquired brain injuries. Methods Inf. Med. 2017, 56, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Meyns, P.; Pans, L.; Plasmans, K.; Heyrman, L.; Desloovere, K.; Molenaers, G. The Effect of additional virtual reality training on balance in children with cerebral palsy after lower limb surgery: A feasibility study. Games Health J. 2017, 6, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Trost, Z.; Zielke, M.; Guck, A.; Nowlin, L.; Zakhidov, D.; France, C.R.; Keefe, F. The promise and challenge of virtual gaming technologies for chronic pain: The case of graded exposure for low back pain. Pain Manag. 2015, 5, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Collado-Mateo, D.; Dominguez-Muñoz, F.J.; Adsuar, J.C.; Merellano-Navarro, E.; Gusi, N. Exergames for women with fibromyalgia: A randomised controlled trial to evaluate the effects on mobility skills, balance and fear of falling. PeerJ 2017, 5, e3211. [Google Scholar] [CrossRef] [PubMed]
- Senkowski, D.; Heinz, A. Chronic pain and distorted body image: Implications for multisensory feedback interventions. Neurosci. Biobehav. Rev. 2016, 69, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Kaczynski, K.J. The Fear Avoidance model of chronic pain: Examination for pediatric application. J. Pain 2012, 13, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Pekyavas, N.O.; Ergun, N. Comparison of virtual reality exergaming and home exercise programs in patients with subacromial impingement syndrome and scapular dyskinesis: Short term effect. Acta Orthop. Traumatol. Turc. 2017, in press. [Google Scholar] [CrossRef] [PubMed]
- Odell, S.; Logan, D.E. Pediatric pain management: The multidisciplinary approach. J. Pain Res. 2013, 6, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Shiri, S.; Feintuch, U.; Weiss, N.; Pustilnik, A.; Geffen, T.; Kay, B.; Meiner, Z.; Berger, I. A virtual reality system combined with biofeedback for treating pediatric chronic headache—A pilot study. Pain Med. 2013, 14, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Soltani, M.; Teeley, A.M.; Wiechman, S.A.; JENSEN, M.P.; SHARAR, S.R.; Patterson, D.R. Virtual reality hypnosis for pain control in a patient with gluteal hidradenitis: A case report. Contemp. Hypn. Integr. Ther. 2011, 28, 142–147. [Google Scholar]
- Lombard, M.; Ditton, T. At the heart of it all: The concept of presence. J. Comput. Med. Commun. 1997, 3. [Google Scholar] [CrossRef]
- Wiederhold, B.K.; Jang, D.; Kaneda, M.; Cabral, I.; Lurie, Y.; May, T.; Kim, I.; Wiederhold, M.D.; Kim, S. An investigation into physiological responses in virtual environments: an objective measurement of presence. In Towards Cyberpsychology: Mind, Cognitions and Society in the Internet Age; Riva, G., Galimberti, C., Eds.; IOS Press: Amsterdam, 2001; pp. 176–182. [Google Scholar]
- Sanchez-Vives, M.V.; Slater, M. From presence to consciousness through virtual reality. Nat. Rev. Neurosci. 2005, 6, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Dahlquist, L.M.; Weiss, K.E.; Clendaniel, L.D.; Law, E.F.; Ackerman, C.S.; McKenna, K.D. Effects of videogame distraction using a virtual reality type head-mounted display helmet on cold pressor pain in children. J. Pediatr. Psychol. 2009, 34, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Law, E.F.; Dahlquist, L.M.; Sil, S.; Weiss, K.E.; Herbert, L.J.; Wohlheiter, K.; Horn, S.B. Videogame distraction using virtual reality technology for children experiencing cold pressor pain: The role of cognitive processing. J. Pediatr. Psychol. 2011, 36, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Sharar, S.R.; Carrougher, G.J.; Nakamura, D.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Arch. Phys. Med. Rehabil. 2007, 88, S43–S49. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, T.; Speck, D.; Wettstein, D.; Masnari, O.; Beeli, G.; Jäncke, L. Feeling present in arousing virtual reality worlds: Prefrontal brain regions differentially orchestrate presence experience in adults and children. Front. Hum. Neurosci. 2008, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Flavell, J.H.; Flavell, E.R.; Green, F.L.; Korfmacher, J.E. Do young children think of television images as pictures or real objects? J. Broadcast. Electron. Media 1990, 34, 399–419. [Google Scholar] [CrossRef]
- Richert, R.A.; Robb, M.B.; Smith, E.I. Media as social partners: The social nature of young children’s learning from screen media. Child Dev. 2011, 82, 82–95. [Google Scholar] [CrossRef] [PubMed]
- Dahlquist, L.M.; McKenna, K.D.; Jones, K.K.; Dillinger, L.; Weiss, K.E.; Ackerman, C.S. Active and passive distraction using a head-mounted display helmet: Effects on cold pressor pain in children. Health Psychol. 2007, 26, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Bryanton, C.; Bosse, J.; Brien, M.; Mclean, J.; McCormick, A.; Sveistrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Olson, C.K. Children’s motivations for video game play in the context of normal development. Rev. Gener. Psychol. 2010, 14, 180. [Google Scholar] [CrossRef]
- Blakemore, S.-J.; Mills, K.L. Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 2014, 65, 187–207. [Google Scholar] [CrossRef] [PubMed]
- Claxton, L.J.; Ponto, K.C. Understanding the properties of interactive televised characters. J. Appl. Dev. Psychol. 2013, 34, 57–62. [Google Scholar] [CrossRef]
- Forgeron, P.A.; King, S.; Stinson, J.N.; McGrath, P.J.; MacDonald, A.J.; Chambers, C.T. Social functioning and peer relationships in children and adolescents with chronic pain: A systematic review. Pain Res. Manag. 2010, 15, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Beals, L.; Bers, M.U. A developmental lens for designing virtual worlds for children and youth. Int. J. Learn. Media 2009, 51–65. [Google Scholar] [CrossRef]
- Ni, L.T.; Fehlings, D.; Biddiss, E. Design and evaluation of virtual reality-based therapy games with dual focus on therapeutic relevance and user experience for children with cerebral palsy. Games Health J. 2014, 3, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.M.; Workman, M. Effects of virtual reality on symptom distress in children receiving chemotherapy. CyberPsychol. Behav. 1999, 2, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Li, H.C.W.; Lopez, V.; Lee, T.L.I. Effects of preoperative therapeutic play on outcomes of school-age children undergoing day surgery. Res. Nurs. Health 2007, 30, 320–332. [Google Scholar]
- Fox, J.; Bailenson, J.N.; Tricase, L. The embodiment of sexualized virtual selves: The Proteus effect and experiences of self-objectification via avatars. Comput. Hum. Behav. 2013, 29, 930–938. [Google Scholar] [CrossRef]
- Yee, N.; Bailenson, J. The Proteus effect: The effect of transformed self-representation on behavior. Hum. Commun. Res. 2007, 33, 271–290. [Google Scholar] [CrossRef]
- Jäncke, L.; Cheetham, M.; Baumgartner, T. Virtual reality and the role of the prefrontal cortex in adults and children. Front. Neurosci. 2009, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J.O.; Bailenson, J.N.; Obradović, J.; Aguiar, N.R. The influence of Immersive virtual reality on children’s inhibitory control and social behavior. Presented at the International Communication’s 67th Annual Conference, San Diego, CA, USA, 25–29 May 2017. [Google Scholar]
- Rasmussen, N.B. Top 10 Most Viewed 360° Videos of 2016. Time, 26 July 2016. [Google Scholar]
| Key Word Search | Number of Articles Obtained | Number of Articles Deemed Relevant and Utilized in Review |
|---|---|---|
| Virtual Reality and Pediatric Procedures | 94 | 13 |
| Virtual Reality and Pediatric Anxiety | 14 | 7 |
| Virtual Reality and Procedural Anxiety | 13 | 8 |
| Virtual Reality and Pediatric Procedural Anxiety | 5 | 5 |
| Virtual Reality and Pediatric Chronic Pain | 4 | 4 |
| Virtual Reality and Pediatric Acute Pain | 5 | 5 |
| Virtual Reality and Pain | 312 | 31 |
| Virtual Reality and Acute pain | 35 | 16 |
| Virtual Reality and Chronic Pain | 63 | 27 |
| Benefits |
|
| Side Effects |
|
| Product Name | Pricing for Headset at Time of Publication | Product Information | Description | Appropriate Ages | Limitations | Tracking |
|---|---|---|---|---|---|---|
| Head and Hand Tracking | ||||||
| HTC Vive | $799 | https://www.vive.com/us/ | HMD & hand trackers, whole-room VR | (minimum 7+) | Requires “VR ready” personal computer (PC) | Positional and rotational |
| Oculus Rift &Touch Controllers | $599.98 | https://www.oculus.com/rift/ | HMD & hand trackers, can be set up on a desktop | 13+ | Requires “VR ready” PC | Positional and rotational |
| PlayStation VR | $499 | https://www.playstation.com/en-us/explore/playstation-vr/ | Video game console HMD and hand trackers | 12+ | Requires Sony PS4, compatible only with PlayStation games | Positional and rotational |
| Head Tracking | ||||||
| Google Cardboard | $5 and up | https://vr.google.com/cardboard/ | Phone-based | Unspecified; with adult supervision (single use <5–10 min) | No hand tracking, limited interactivity; requires VR-compatible phone | Rotational |
| Google Daydream | $79 | https://vr.google.com/daydream/ | Phone-based; lightweight; includes controller | 13+ | Currently limited software library; requires VR-compatible phone | Rotational with one controller |
| Gear VR | $129.99 | https://www.oculus.com/gear-vr/ | Phone-based, adjustable headset with hand controller | 13+ | Limited features compared to PC-based VR; requires VR-compatible phone | Rotational |
| Game Title | Hardware Compatibility | Where to Find It | Potential Applications | Qualities |
|---|---|---|---|---|
| Google Earth VR | -HTC Vive -Oculus Rift | https://vr.google.com/earth/ | -Anxiety -Distraction therapy -Procedural pain | -Hands-free -Cinematic -Engaging |
| Minecraft | -HTC Vive -Oculus Rift -Samsung -GearVR -Cardboard | 1. Install PC version of Minecraft 2. Install Vivecraft (http://www.vivecraft.org/) for VR compatibility | -Anxiety -Distraction therapy | -Controller required -Well-known by kids -Engaging |
| Guided Meditation VR | -HTC Vive -Oculus Rift -Samsung -GearVR | https://guidedmeditationvr.com/download/ | -Anxiety -Distraction therapy -Procedural pain | -Hands Free -Calming |
| The Lab | -HTC Vive -Oculus Rift | http://store.steampowered.com/app/450390/The_Lab/ | -Anxiety -Distraction therapy | -Exploration -Specific movements (archery + slingshot) -Scenic |
| The Blu | -HTC Vive -Oculus Rift | http://store.steampowered.com/app/451520/theBlu/ | -Anxiety -Distraction therapy | -Hands-free -Cinematic -Exploration |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Won, A.S.; Bailey, J.; Bailenson, J.; Tataru, C.; Yoon, I.A.; Golianu, B. Immersive Virtual Reality for Pediatric Pain. Children 2017, 4, 52. https://doi.org/10.3390/children4070052
Won AS, Bailey J, Bailenson J, Tataru C, Yoon IA, Golianu B. Immersive Virtual Reality for Pediatric Pain. Children. 2017; 4(7):52. https://doi.org/10.3390/children4070052
Chicago/Turabian StyleWon, Andrea Stevenson, Jakki Bailey, Jeremy Bailenson, Christine Tataru, Isabel A. Yoon, and Brenda Golianu. 2017. "Immersive Virtual Reality for Pediatric Pain" Children 4, no. 7: 52. https://doi.org/10.3390/children4070052






