Influence of Socioeconomic Status on Knowledge of Obesity and Diabetes among Adolescents in Chennai, South India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
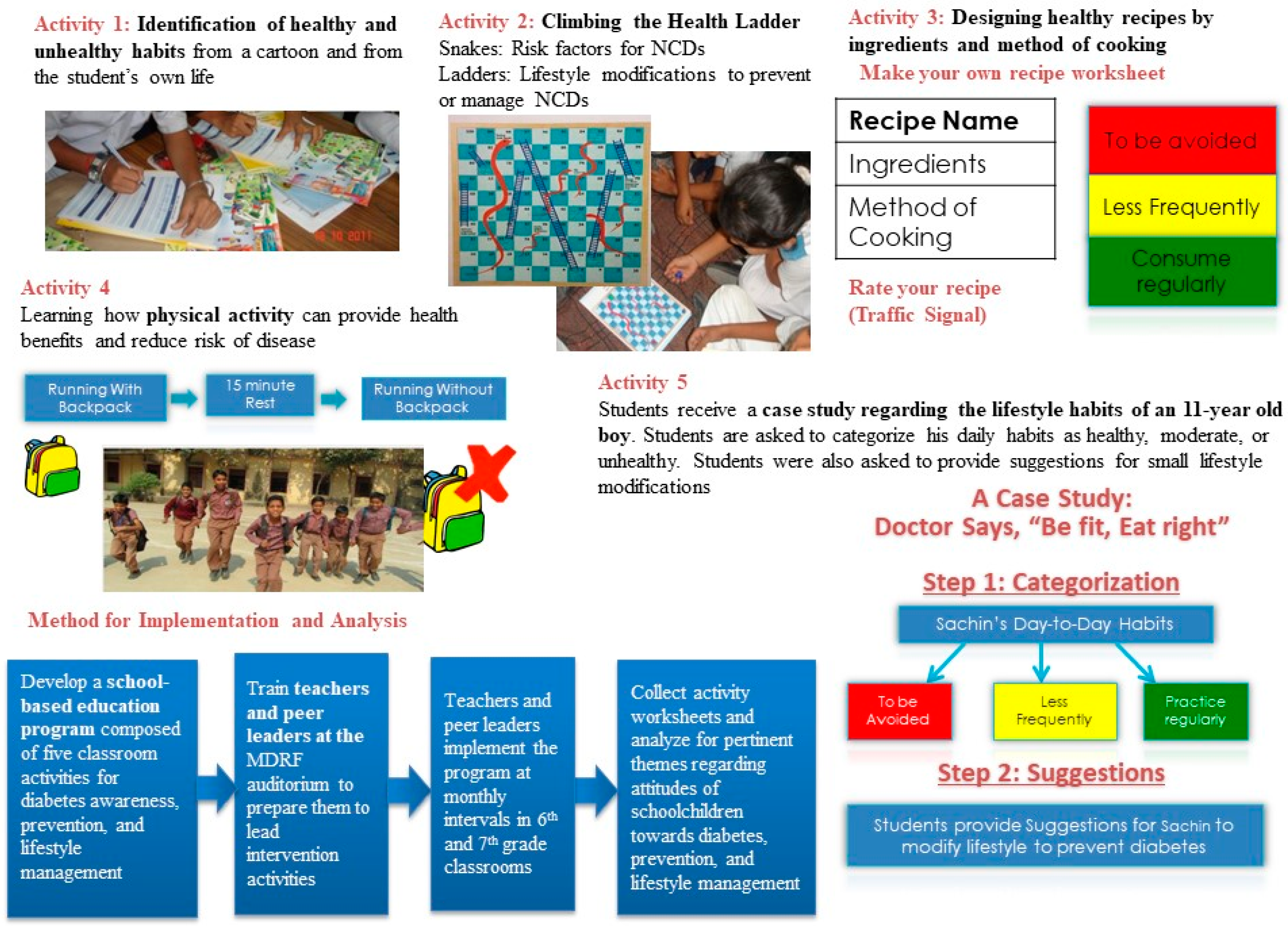
2.2. Structure
2.3. Anthropometric Measures
2.4. Data Analysis
3. Results
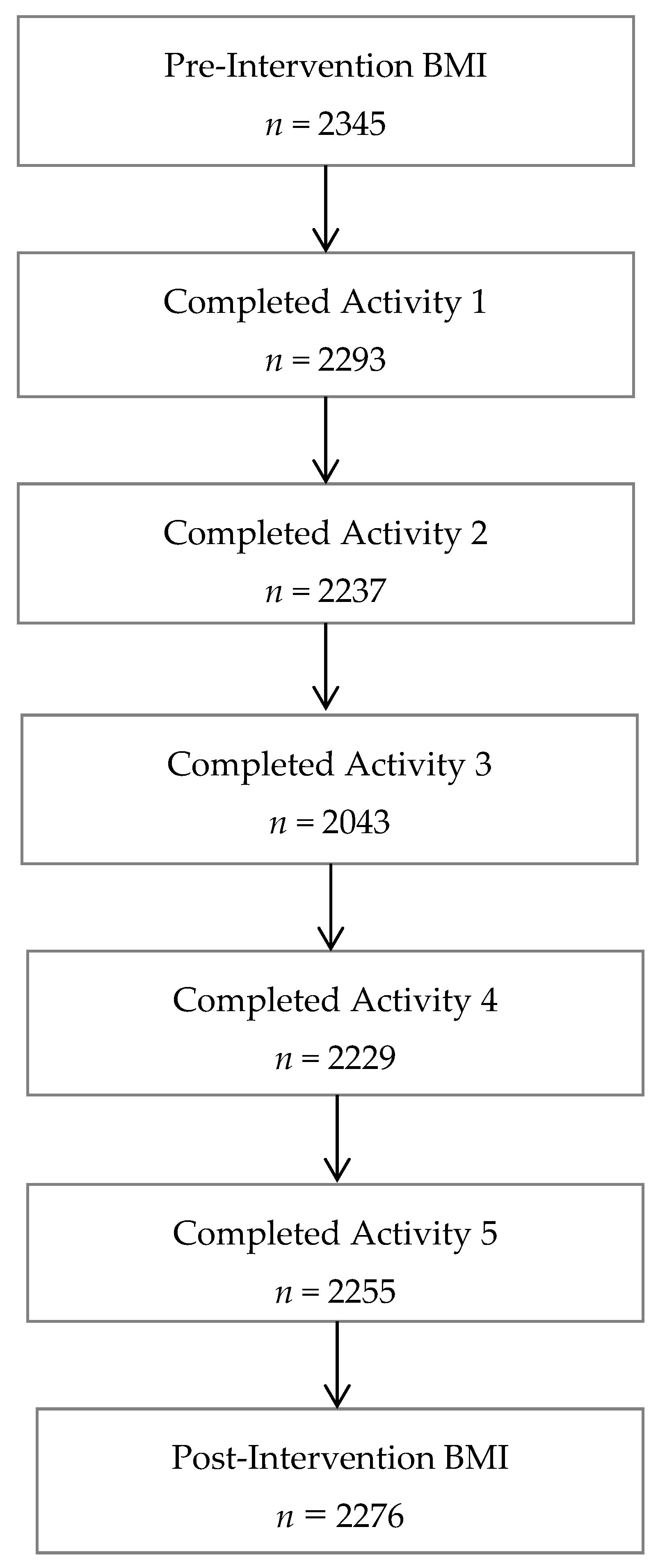
3.1. Participant Characteristics
3.2. Pre- and Post- Intervention BMI
3.3. Activity Responses and Feedback from Peer Leaders and Teachers
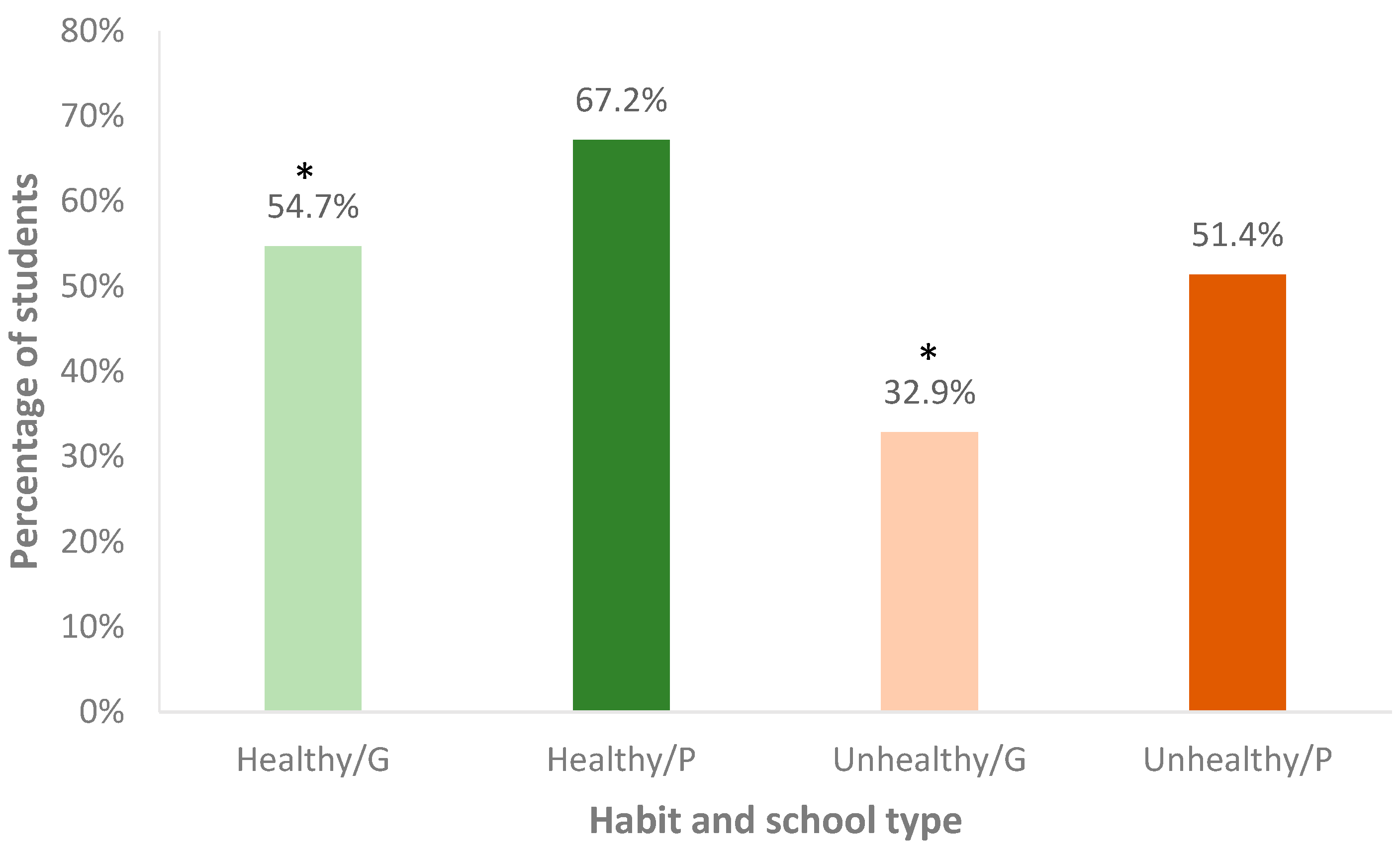
3.3.1. Activity 1: Way to Health
3.3.2. Activity 2: Climbing the Health Ladder
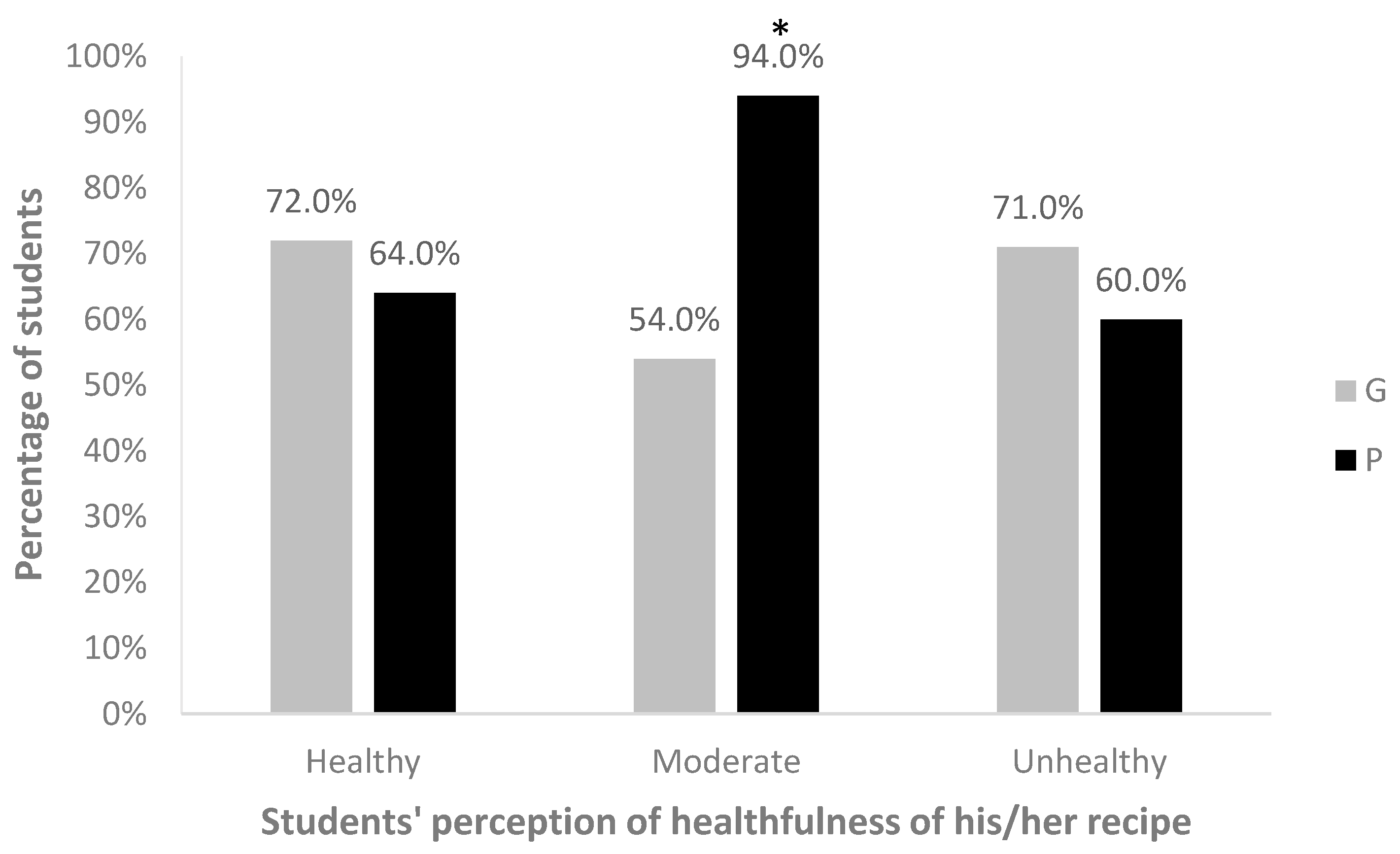
3.3.3. Activity 3: Pass It on-The Traffic Signal
3.3.4. Activity 4: Jump Forward and Race with Pace
3.3.5. Activity 5: Doctor Says “Be Fit, Eat Right”
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Key Messages
- A school-based co-curriculum program for educating adolescents about healthy lifestyle modifications to prevent diabetes and improve overall health status was well-received in a sample of government and private schools in Chennai, India.
- This study found divergences in comprehension of the diabetes education program between students from government (low socio-economic status (SES)) and private (high SES) schools.
- Intervention strategies must be adapted to the culture and socioeconomic status of students from different school settings.
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
Appendix A.1. Activity 1
Appendix A.2. Activity 2
Appendix A.3. Activity 3
Appendix A.4. Activity 4
Appendix A.5. Activity 5
Appendix B
| Pre-Intervention | Post-Intervention | p-Value * | |
|---|---|---|---|
| Overall | 144.0 ± 8.2 | 147.0 ± 8.5 | <0.0001 |
| Height | |||
| Boy | 143.1 ± 8.2 | 146.1 ± 8.7 | <0.0001 |
| Girl | 145.2 ± 8.1 | 148.1 ± 8.0 | <0.0001 |
| Weight | |||
| Boy | 36.3 ± 10.3 | 38.9 ± 10.9 | <0.0001 |
| Girl | 38.3 ± 10.3 | 41.3 ± 10.8 | <0.0001 |
References
- International Diabetes Federation. IDF Diabetes Atlas, 7th ed.; International Diabetes Federation: Brussels, Belgium, 2015; Available online: http://www.diabetesatlas.org (accessed on 26 December 2016).
- Pradeepa, R.; Anjana, R.M.; Joshi, S.R.; Bhansali, A.; Deepa, M.; Joshi, P.P.; Dhandania, V.K.; Madhu, S.V.; Rao, P.V.; Geetha, L.; et al. Prevalence of generalized & abdominal obesity in urban & rural India—The ICMR-INDIAB Study (Phase-I) [ICMR-INDIAB-3]. Indian J. Med. Res. 2015, 142, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.R.; Mohan, V.; Joshi, S.S.; Mechanick, J.I.; Marchetti, A. Transcultural Diabetes Nutrition Therapy Algorithm: The Asian Indian Application. Curr. Diabetes Rep. 2012, 12, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Anjana, R.M.; Pradeepa, R.; Deepa, M.; Datta, M.; Sudha, V.; Unnikrishnan, R.; Bhansali, A.; Joshi, S.R.; Joshi, P.P.; Yajnik, C.S.; et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdiaDIABetes (ICMR-INDIAB) study. Diabetologia 2011, 54, 3022–3027. [Google Scholar] [CrossRef] [PubMed]
- Ranjani, H.; Sonya, J.; Anjana, R.M.; Mohan, V. Prevalence of glucose intolerance among children and adolescents in urban South India (ORANGE-2). Diabetes Technol. Ther. 2013, 15, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Jagadesan, S.; Harish, R.; Miranda, P.; Unnikrishnan, R.; Anjana, R.M.; Mohan, V. Prevalence of overweight and obesity among school children and adolescents in Chennai. Indian Pediatr. 2014, 51, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Mohan, V.; Deepa, R.; Deepa, M.; Somannavar, S.; Datta, M. A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J. Assoc. Physicians India 2005, 53, 759–763. [Google Scholar] [PubMed]
- Norris, S.L.; Engelgau, M.M.; Narayan, K.M. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care 2001, 24, 561–587. [Google Scholar] [CrossRef] [PubMed]
- A Report From The Diabetes Summit for South-East Asia, Chennai, India, November 28th–30th, 2008. In Practical Diabetes International Supplement 2009; John Wiley & Sons: Hoboken, NJ, USA, 2008; Available online: https://www.worlddiabetesfoundation.org/sites/default/files/Report.Summit.India2008.pdf (accessed on 26 December 2016).
- Weber, M.B.; Ranjani, H.; Meyers, G.C.; Mohan, V.; Narayan, K.M. A model of translational research for diabetes prevention in low and middle-income countries: The Diabetes Community Lifestyle Improvement Program (D-CLIP) trial. Prim. Care Diabetes 2012, 6, 3–9. [Google Scholar] [CrossRef] [PubMed]
- The Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999, 22, 623–634. [Google Scholar] [PubMed]
- Bantle, J.P.; Wylie-Rosett, J.; Albright, A.L.; Apovian, C.M.; Clark, N.G.; Franz, M.J.; Hoogwerf, B.J.; Lichtenstein, A.H.; Mayer-Davis, E.; Mooradian, A.D.; et al. Nutrition recommendations and interventions for diabetes—2006: A position statement of the American Diabetes Association. Diabetes Care 2006, 29, 2140–2157. [Google Scholar] [CrossRef] [PubMed]
- Ranjani, H.; Pradeepa, R.; Mehreen, T.S.; Anjana, R.M.; Anand, K.; Garg, R.; Mohan, V. Determinants, consequences and prevention of childhood overweight and obesity: An Indian context. Indian J. Endocrinol. Metab. 2014, 18 (Suppl. S1), S17–S25. [Google Scholar] [CrossRef] [PubMed]
- Balagopal, P.; Kamalamma, N.; Patel, T.G.; Misra, R. A community-based participatory diabetes prevention and management intervention in rural India using community health workers. Diabetes Educ. 2012, 38, 822–834. [Google Scholar] [CrossRef] [PubMed]
- Rosenbloom, A.L.; Young, R.S.; Joe, J.R.; Winter, W.E. Emerging epidemic of type 2 diabetes in youth. Diabetes Care 1999, 22, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Sonya, J.; Ranjani, H.; Pradeepa, R.; Mohan, V. Obesity Reduction and Awareness and Screening of Noncommunicable Diseases through Group Education in Children and Adolescents (ORANGE): Methodology Paper (ORANGE-1). J. Diabetes Sci. Technol. 2010, 4, 1256–1264. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, A.; Snehalata, C.; Yamuna, A.; Murugesan, N.; Narayan, K.M. Insulin resistance and clustering of cardiometabolic risk factor in urban teenagers in southern India. Diabetes Care 2007, 30, 1828–1833. [Google Scholar] [CrossRef] [PubMed]
- Treviño, R.P.; Yin, Z.; Hernandez, A.; Hale, D.E.; Garcia, O.A.; Mobley, C. Impact of the Bienestar School-Based Diabetes Mellitus Prevention Program on Fasting Capillary Glucose Levels: A Randomized Controlled Trial. Arch. Pediatr. Adolesc. Med. 2004, 158, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Bassi, S.; Gupta, V.K.; Chopra, I.; Ranjani, H.; Saligram, N.; Arora, M. Novel school-based health intervention program—A step toward early diabetes prevention. Int. J. Diabetes Dev. Ctries. 2015, 35, 460–468. [Google Scholar] [CrossRef]
- Narayan, K.M.; Fagot-Campagna, A.; Imperatore, G. Type 2 diabetes in children: A problem lurking for India? Indian Pediatr. 2001, 38, 701–704. [Google Scholar] [PubMed]
- Lau, R.R.; Quadrel, M.J.; Hartman, K.A. Development and change of young adults’ preventive health beliefs and behavior: Influence from parents and peers. J. Health Soc. Behav. 1990, 31, 240–259. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Boyce, W.F.; Simpson, K.; Pickett, W. Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am. J. Clin. Nutr. 2006, 83, 139–145. [Google Scholar] [PubMed]
- Lawton, J.; Ahmad, N.; Hanna, L.; Douglas, M.; Hallowell, N. “I can’t do any serious exercise”: Barriers to physical activity amongst people of Pakistani and Indian origin with type 2 diabetes. Health Educ. Res. 2006, 21, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Sharma, D.; Larson, R.W. School stress in India: Effects on time and daily emotions. Int. J. Behav. Dev. 2002, 26, 500–508. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Lemkau, J.P. Cultural issues in the primary care of south Asians. J. Immigr. Health 2000, 2, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Horton, S.; Kim, S.; Mahal, A.; Shuigao, J. Trends in diet, nutritional status, and diet-related noncommunicable diseases in China and India: The economic costs of the nutrition transition. Nutr. Rev. 2001, 59, 379–390. [Google Scholar] [CrossRef] [PubMed]
| Variables | No. of Participants (%) (n = 2276) | School Type | ||
|---|---|---|---|---|
| Private No. (%) (n = 1784) | Government No. (%) (n = 492) | p-Value | ||
| Age in years * (mean age = 11.1) | ||||
| 10 | 561 (24.7) | 452 (25.3) | 109 (22.2) | 0.0003 |
| 11 | 1016 (44.6) | 820 (46.0) | 196 (39.8) | |
| 12 | 601 (26.4) | 447 (25.1) | 154 (31.3) | |
| 13 | 98 (4.3) | 65 (3.6) | 33 (6.7) | |
| Gender * | ||||
| Boy | 1294 (56.9) | 944 (52.9) | 350 (71.1) | <0.0001 |
| Girl | 982 (43.2) | 840 (47.1) | 142 (28.9) | |
| Intervention Compliance * | ||||
| Compliant | 2181 (95.8) | 1748 (98.0) | 433 (88.0) | <0.0001 |
| Non-compliant | 95 (4.2) | 36 (2.0) | 59 (12.0) | |
| Anthropometric measures † (mean ± SD) | ||||
| Height (cm) | 147.0 ± 8.5 | 148.5 ± 8.0 | 141.3 ± 7.5 | <0.0001 |
| Weight (kg) | 39.9 ± 10.9 | 41.7 ± 10.7 | 33.5 ± 9.1 | |
| Pre-Intervention BMI | Post-Intervention BMI | p-Value * | |||
|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | ||
| Overall | 2276 | 17.7 ± 3.7 | 2276 | 18.3 ± 3.8 | <0.0001 |
| School | |||||
| Government | 492 | 15.9 ± 3.1 | 492 | 16.6 ± 3.4 | <0.0001 |
| Private | 1784 | 18.2 ± 3.7 | 1784 | 18.7 ± 3.8 | <0.0001 |
| Gender | |||||
| Boy | 1294 | 17.4 ± 3.6 | 1294 | 18.0 ± 3.8 | <0.0001 |
| Girl | 982 | 18.0 ± 3.7 | 982 | 18.6 ± 3.8 | <0.0001 |
| Theme | Common Outcomes | Rationale |
|---|---|---|
| Difficulty in distinguishing between a non-communicable and infectious disease among government school students | Misinterpretation of unsanitary, irresponsible, or irrespective habits as lifestyle behaviors causing diabetes. | Government school students often come from low-income families, who may struggle to think past their immediate needs (such as clean water and hygiene), and better comprehend the message of the intervention program. |
| Misinterpretation of a costly activity or meal as a healthy habit among private school students | Private school students often suggest eating at restaurants and riding cars as healthy lifestyle modifications to prevent diabetes. They may mistakenly associate wealth with a healthy lifestyle, and perceive certain unhealthy behaviors to be healthy. | Private school students come from higher income families, who can afford high-calorie restaurant food, television sets, video games, and other pleasures correlated with unhealthy eating and physical inactivity [22]. |
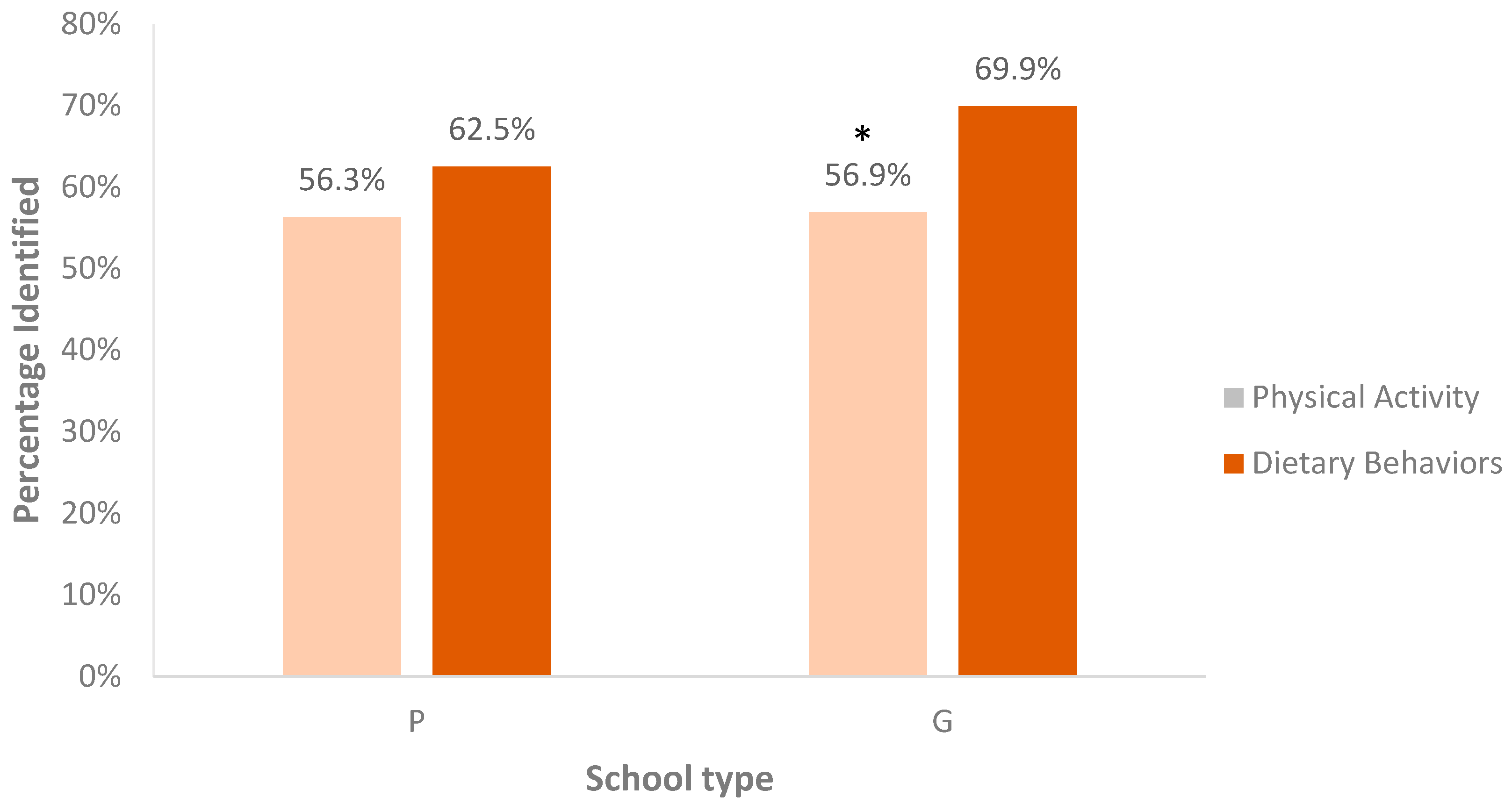
| Lack of awareness of physical activity and increased emphasis on dietary behaviors among both private and government school students | When asked to identify unhealthy lifestyle behaviors related to diabetes, more students correctly listed improper eating habits rather than physical inactivity or sedentary behaviors. Also, many students listed studying as a healthy lifestyle behavior to help prevent diabetes, even though it is a sedentary behavior. | It appears that children are unaware of how the built environment influences both their energy intake and energy expenditure. Certain barriers to exercise include inadequate places to exercise, or a desire to avoid pollution outdoors [23]. Familial pressure to succeed in school may also cause children to disregard studying as a sedentary behavior [24,25]. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panuganti, P.; Mehreen, T.S.; Anjana, R.M.; Mohan, V.; Mayer-Davis, E.; Ranjani, H. Influence of Socioeconomic Status on Knowledge of Obesity and Diabetes among Adolescents in Chennai, South India. Children 2017, 4, 61. https://doi.org/10.3390/children4080061
Panuganti P, Mehreen TS, Anjana RM, Mohan V, Mayer-Davis E, Ranjani H. Influence of Socioeconomic Status on Knowledge of Obesity and Diabetes among Adolescents in Chennai, South India. Children. 2017; 4(8):61. https://doi.org/10.3390/children4080061
Chicago/Turabian StylePanuganti, Pranati, T.S. Mehreen, Ranjit Mohan Anjana, Viswanathan Mohan, E. Mayer-Davis, and Harish Ranjani. 2017. "Influence of Socioeconomic Status on Knowledge of Obesity and Diabetes among Adolescents in Chennai, South India" Children 4, no. 8: 61. https://doi.org/10.3390/children4080061




