Trends in Food and Beverage Portion Sizes in Australian Children; a Time-Series Analysis Comparing 2007 and 2011–2012 National Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
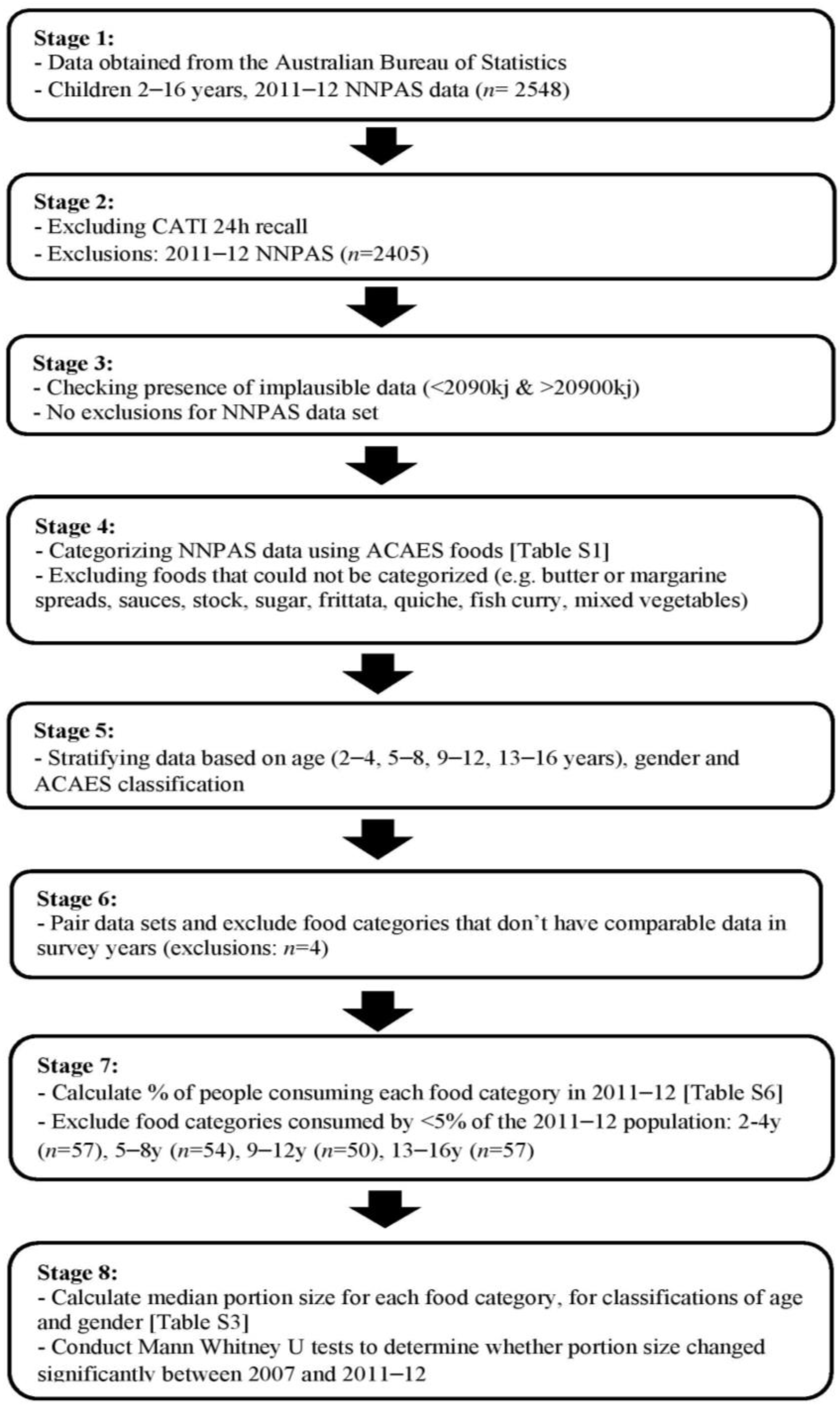
2.3. Data Handling
2.4. Data Analysis
3. Results
3.1. Portion Size Outcomes
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Australian Bureau of Statistics. Australian Health Survey: Updated Results, 2011–2012. 2014. Available online: http://www.abs.gov.au/ausstats/[email protected]/Lookup/4364.0.55.003Chapter12011-2012 (accessed on 5 March 2015).
- Perez-Escamilla, R.; Obbagy, J.E.; Altman, J.M.; Essery, E.V.; McGrane, M.M.; Wong, Y.P.; Spahn, J.M.; Williams, C.L. Dietary energy density and body weight in adults and children: A systematic review. J. Acad. Nutr. Diet. 2012, 112, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [PubMed]
- Young, L.R.; Nestle, M. The contribution of expanding portion sizes to the US obesity epidemic. Am. J. Public Health 2002, 92, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Ledikwe, J.H.; Ello-Martin, J.A.; Rolls, B.J. Portion sizes and the obesity epidemic. J. Nutr. 2005, 135, 905–909. [Google Scholar] [PubMed]
- World Health Organisation. Childhood Overweight and Obesity. 2012. Available online: http://www.who.int/elena/bbc/portion_childhood_obesity/en/ (accessed on 5 February 2015).
- Rolls, B.J. What is the role of portion control in weight management? Int. J. Obes. 2014, 38, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Savage, J.; Fisher, J.O. Right sizing prevention. Food portion size effects on children’s eating and weight. Appetite 2014, 88, 11–16. [Google Scholar] [CrossRef] [PubMed]
- McConahy, K.L.; Smiciklas-Wright, H.; Birch, L.L.; Mitchell, D.C.; Picciano, M.F. Food portions are positively related to energy intake and body weight in early childhood. J. Pediatr. 2002, 140, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Piernas, C.; Popkin, B.M. Food portion patterns and trends among, U.S. children and the relationship to total eating occasion size, 1977–2006. J. Nutr. 2011, 141, 1159–1164. [Google Scholar] [CrossRef] [PubMed]
- Chandon, P.W.B. Is food marketing making us fat? A multi-disciplinary review. Found. Trends Mark. 2011, 5, 1–86. [Google Scholar] [CrossRef]
- Zlatevska, N.D.C.; Holden, S.S. Sizing up the effect of portion size on consumption: A meta-analytic review. J. Mark. 2014, 78, 140–154. [Google Scholar] [CrossRef]
- Steenhuis, I.; Vermeer, W. Portion size: Review and framework for interventions. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 58. [Google Scholar] [CrossRef] [PubMed]
- Small, L.; Lane, H.; Vaughan, L.; Melnyk, B.; McBurnett, D. A systematic review of the evidence: The effects of portion size manipulation with children and portion education/training interventions on dietary intake with adults. Worldviews Evid. Based Nurs. 2013, 10, 69–81. [Google Scholar] [CrossRef] [PubMed]
- McConahy, K.L.; Smiciklas-Wright, H.; Mitchell, D.C.; Picciano, M.F. Portion size of common foods predicts energy intake among preschool-aged children. J. Am. Diet. Assoc. 2004, 104, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Kerr, M.A.; Rennie, K.L.; McCaffrey, T.A.; Wallace, J.M.W.; Hannon-Fletcher, M.P.; Livingstone, M.B.E. Snacking patterns among adolescents: A comparison of type, frequency and portion size between Britain in 1997 and Northern Ireland in 2005. Br. J. Nutr. 2009, 101, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.J.; Popkin, B.M. Patterns and trends in food portion sizes, 1977–1998. J. Am. Med. Assoc. 2003, 289, 450–453. [Google Scholar] [CrossRef]
- Nielsen, S.J.; Popkin, B.M. Changes in beverage intake between 1977 and 2001. Am. J. Prev. Med. 2004, 27, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, W.M.S.I.; Poelman, M.P. Small, medium, large or supersize? The development and evaluation of interventions targeted at portion size. Int. J. Obes. 2014, 38, S13–S18. [Google Scholar] [CrossRef] [PubMed]
- Collins, K.; Watson, J.; Collins, C. Food and beverage portion sizes in Australian children: A secondary analysis of 1995 and 2007 national data. BMC Public Health 2014, 14, 517. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Australian National Children’s Nutrition and Physical Activity Survey, Canberra (Aust): BASIC CURF [CD-ROM] version 2007. 2007.
- Australian Bureau of Statistics. Australian Health Survey: Users’ Guide, 2011–13. 2015. Available online: http://www.abs.gov.au/ausstats/[email protected]/mf/4363.0.55.001 (accessed on 5 March 2015).
- Department of Health and Ageing. Australian National Childrens Nutrition and Physical Activity Survey—User’s Guide; Commonwealth Government of Australia: Canberra, Australia, 2007. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/phd-nutrition-childrens-survey-userguide (accessed on 5 March 2015).
- Bliss, R. Researchers produce innovation in dietary recall. Agric. Res. 2004, 52, 10–12. [Google Scholar]
- Watson, J.F.; Collins, C.E.; Sibbritt, D.W.; Dibley, M.J.; Garg, M.L. Reproducibility and comparative validity of a food frequency questionnaire for Australian children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2011, 6, 62. [Google Scholar] [CrossRef] [PubMed]
- Kellett, E.S.A.; Schmerlaib, Y. The Australian Guide to Healthy Eating; Australian Government Department of Health and Ageing: Canberra, Australia, 1998. [Google Scholar]
- Mikkilä, V.R.L.; Raitakari, O.T.; Pietinen, P.; Viikari, J. Consistent dietary patterns identified from childhood to adulthood: The cardiovascular risk in Young Finns Study. Br. J. Nutr. 2005, 93, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Carr, P.R.; Walter, V.; Brenner, H.; Hoffmeister, M. Meat subtypes and their association with colorectal cancer: Systematic review and meta-analysis. Int. J. Cancer 2016, 138, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B.; Doll, R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int. J. Cancer 1975, 15, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Carroll, K.K.B.L. Dietary fat and mammary carcinogenesis. Nutr. Cancer 1985, 6, 254–259. [Google Scholar] [CrossRef]
- Rose, D.P.; Boyar, A.P.; Wynder, E.L. International comparisons of mortality rates for cancer of the breast, ovary, prostate, and colon, and per capita food consumption. Cancer 1986, 58, 2363–2371. [Google Scholar] [CrossRef]
- Young, L.R.; Nestle, M. Reducing portion sizes to prevent obesity: A call to action. Am. J. Prev. Med. 2012, 43, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Baur, L.A. Child and adolescent obesity in the 21st century: An Australian perspective. Asia Pac. J. Clin. Nutr. 2002, 11, S524–S528. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines 2013. Available online: https://www.nhmrc.gov.au/guidelines-publications/n55 (accessed on 22 March 2015).
- Moreno, L.A.; Rodríguez, G. Dietary risk factors for development of childhood obesity. Curr. Opin. Clin. Nutr. Metab. Care 2007, 10, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Rangan, A.; Meertens, B.; Wu, J.H.Y. Changes in typical portion sizes of commonly consumed discretionary foods among Australian adults from 1995 to 2011–2012. Nutrients 2017, 9, 577. [Google Scholar] [CrossRef] [PubMed]
- Benton, D. Portion size: What we know and what we need to know. Crit. Rev. Food Sci. Nutr. 2013, 55, 988–1004. [Google Scholar] [CrossRef] [PubMed]
- Watson, W.L.; Kury, A.; Wellard, L.; Hughes, C.; Dunford, E.; Chapman, K. Variations in serving sizes of Australian snack foods and confectionery. Appetite 2015, 96, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Ello-Martin, J.A.; Ledikwe, J.H.; Rolls, B.J. The influence of food portion size and energy density on energy intake: Implications for weight management. Am. J. Clin. Nutr. 2005, 82, 236S–241S. [Google Scholar] [PubMed]
- Haby, M.M.; Markwick, A.; Peeters, A.; Shaw, J.; Vos, T. Future predictions of body mass index and overweight prevalence in Australia, 2005–2025. Health Promot. Int. 2012, 27, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Willet, W. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Rangan, A.M.; Kwan, J.S.L.; Louie, J.C.Y.; Flood, V.M.; Gill, T.P. Changes in core food intake among Australian children between 1995 and 2007. Eur. J. Clin. Nutr. 2011, 65, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Australasian Child & Adolescent Obesity Research Network. Available online: http://www.acaorn.org.au/streams/nutrition/assessment-methods/24hr-recall.php (accessed on 8 March 2015).
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van der Bend, D.; Bucher, T.; Schumacher, T.L.; Collins, K.; De Vlieger, N.; Rollo, M.; Burrows, T.L.; Watson, J.F.; Collins, C.E. Trends in Food and Beverage Portion Sizes in Australian Children; a Time-Series Analysis Comparing 2007 and 2011–2012 National Data. Children 2017, 4, 69. https://doi.org/10.3390/children4080069
Van der Bend D, Bucher T, Schumacher TL, Collins K, De Vlieger N, Rollo M, Burrows TL, Watson JF, Collins CE. Trends in Food and Beverage Portion Sizes in Australian Children; a Time-Series Analysis Comparing 2007 and 2011–2012 National Data. Children. 2017; 4(8):69. https://doi.org/10.3390/children4080069
Chicago/Turabian StyleVan der Bend, Daphne, Tamara Bucher, Tracy L. Schumacher, Kate Collins, Nienke De Vlieger, Megan Rollo, Tracy L. Burrows, Jane F. Watson, and Clare E. Collins. 2017. "Trends in Food and Beverage Portion Sizes in Australian Children; a Time-Series Analysis Comparing 2007 and 2011–2012 National Data" Children 4, no. 8: 69. https://doi.org/10.3390/children4080069





