Health and Self-Regulation among School-Age Children Experiencing Family Homelessness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Procedure
2.3. Measures
2.3.1. Predictor: Risk and Adversity
2.3.2. Predictor: Self-Regulation
2.3.3. Predictor: Intellectual Function
2.3.4. Outcome: Health
2.4. Statistical Analysis
3. Results
3.1. Demographics
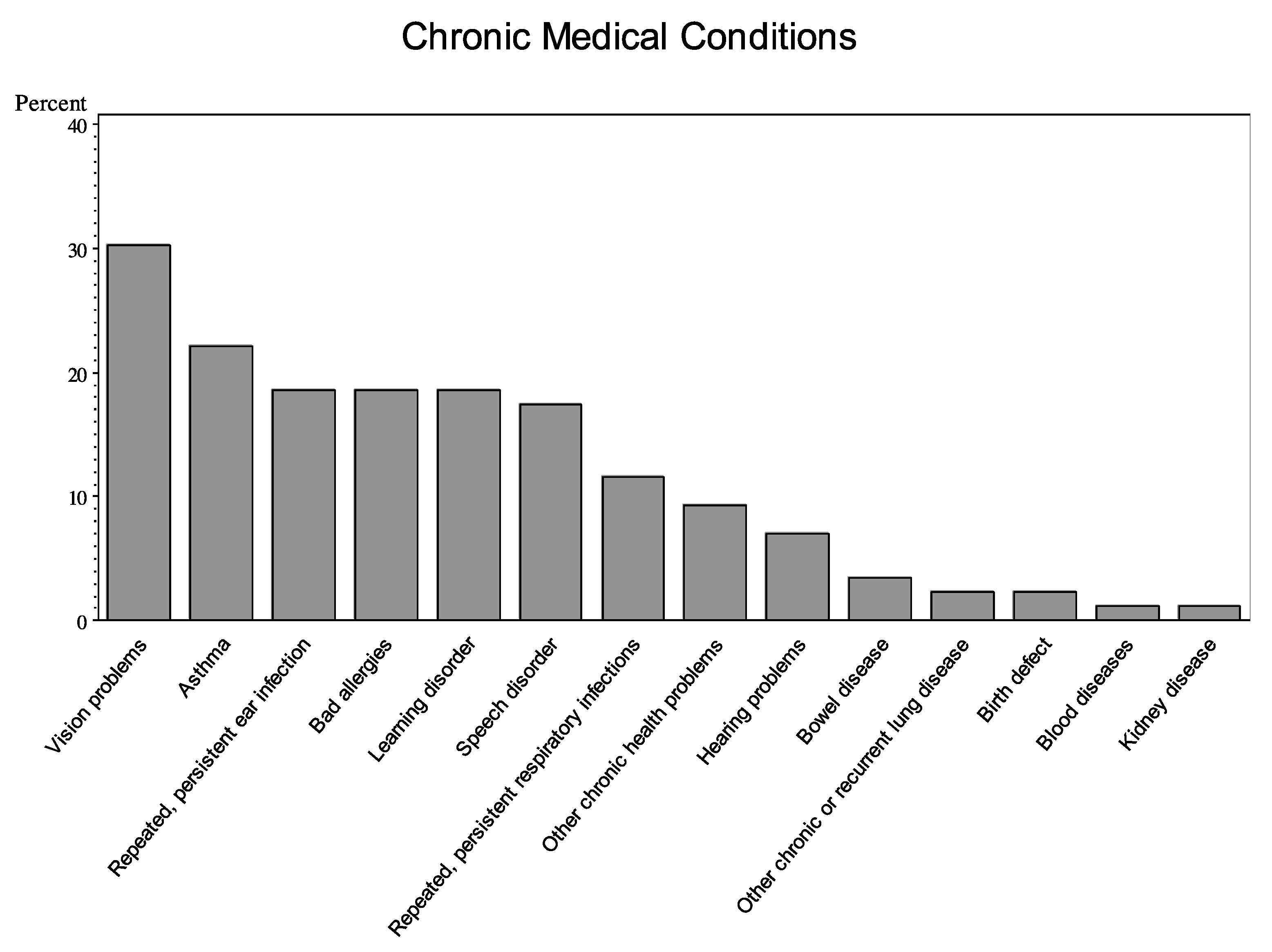
3.2. Health Conditions
3.3. Associations Between Child Characteristics and Health
3.4. Self-Regulation and Health
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Khadduri, J.; Culhane, D. Annual Homeless Assessment Report (AHAR); US Department of Housing and Urban Development: Washington, DC, USA, 2014.
- Cutuli, J.J.; Herbers, J.E. Promoting resilience for children who experience family homelessness: Opportunities to encourage developmental competence. Cityscape 2014, 16, 113–139. [Google Scholar]
- Briggs, M. AAP Policy Statement: Providing care for children and adolescents facing homelessness and housing insecurity. Pediatrics 2013, 16, 1206–1210. [Google Scholar]
- Masten, A.S.; Miliotis, D.; Graham-Bermann, S.A.; Ramirez, M.; Neemann, J. Children in homeless families: Risks to mental health and development. J. Consult. Clin. Psychol. 1993, 61, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, Y.; Shinn, M.; Weitzman, B.C. Academic achievement among formerly homeless adolescents and their continuously housed peers. J. School Psychol. 2004, 42, 179–199. [Google Scholar] [CrossRef]
- Evans, G.W.; Kim, P. Childhood Poverty, Chronic Stress, Self-Regulation, and Coping. Child Dev. Perspect. 2013, 7, 43–48. [Google Scholar] [CrossRef]
- Blair, C.; Raver, C.C. Child development in the context of adversity: Experiential canalization of brain and behavior. Am. Psychol. 2012, 67, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Zelazo, P.D.; Carlson, S.M. Hot and cool executive function in childhood and adolescence: Development and plasticity. Child Dev. Perspect. 2012, 6, 354–360. [Google Scholar] [CrossRef]
- Diamond, A.; Lee, K. Interventions shown to aid executive function development in children 4 to 12 years old. Science 2011, 333, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.; Garner, A.; Health, C. Leveraging the biology of adversity to address the roots of disparities in health and development. Pediatrics 2012, 129. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Obradovic, J. Competence and resilience in development. Ann. N. Y. Acad. Sci. 2006, 1094, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Lengua, L.J.; Moran, L.; Zalewski, L.; Ruberry, E.; Kiff, C.; Thompson, S. Relations of growth in effortful control to family income, cumulative risk, and adjustment in preschool-age children. J. Abnorm. Child Psychol. 2015, 43, 705–720. [Google Scholar] [CrossRef] [PubMed]
- Buckner, J.C.; Mezzacappa, E.; Beardslee, W.R. Characteristics of resilient youths living in poverty: The role of self-regulatory processes. Dev. Psychopathol. 2003, 15, 139–162. [Google Scholar] [CrossRef] [PubMed]
- Buckner, J.C.; Mezzacappa, E.; Beardslee, W.R. Self-regulation and its relations to adaptive functioning in low income youths. Am. J. Orthopsychiatr. 2009, 79, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Obradović, J. Effortful control and adaptive functioning of homeless children: Variable focused and person-focused analyses. J. Appl. Dev. Psychol. 2010, 31, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Herbers, J.E.; Cutuli, J.J.; Monn, A.R.; Narayan, A.J.; Masten, A.S. Trauma, adversity, and parent-child relationships among young children experiencing homelessness. J. Abnorm. Child Psychol. 2014, 42, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, T.E.; Arseneault, L.; Belsky, D.; Dickson, N.; Hancox, R.J.; Harrington, H.L.; Houts, R.; Poulton, R.; Roberts, B.W.; Ross, S.; et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc. Natl. Acad. Sci. USA 2011, 108, 2693–2698. [Google Scholar] [CrossRef]
- Weinreb, L.; Goldberg, R.; Bassuk, E.; Perloff, J. Determinants of health and service use patterns in homeless and low-income housed children. Pediatrics 1998, 102, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Cutuli, J.J.; Herbers, J.E.; Lafavor, T.L.; Ahumada, S.M.; Masten, A.S.; Oberg, C.N. Asthma and adaptive functioning among homeless kindergarten-aged children in emergency Housing. J. Health Care Poor Underserv. 2014, 25, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Edidin, J.P.; Ganim, Z.; Hunter, S.J.; Karnik, N.S. The mental and physical health of homeless youth: A literature review. Child Psychiatr. Hum. Dev. 2012, 43, 354–375. [Google Scholar] [CrossRef] [PubMed]
- Berti, L.C.; Zylbert, S.; Rolnitzky, L. Comparison of health status of children using a school-based health center for comprehensive care. J. Pediatr. Health Care 2001, 15, 244–250. [Google Scholar] [CrossRef]
- McQuaid, E.L.; Kopel, S.J.; Nassau, J.H. Behavioral adjustment in children with asthma: A meta-analysis. J. Dev. Behav. Pediatr. 2001, 22, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Cutuli, J.J.; Wiik, K.L.; Herbers, J.E.; Gunnar, M.R.; Masten, A.S. Cortisol function among early school-aged homeless children. Psychoneuroendocrinology 2010, 35, 833–845. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Sesma, A., Jr. Risk and resilience among children homeless in Minneapolis. CURA Report. 1999, 47, 1–6. [Google Scholar]
- Masten, A.; Neemann, J.; Andenas, S. Life events and adjustment in adolescents: The significance of event independence, desirability and chronicity. J. Res. Adolesc. 1994, 4, 71–97. [Google Scholar] [CrossRef]
- Gioia, G.A. Behavior Rating Inventory of Executive Function: Professional Manual; Psychological Assessment Resources, Inc.: Lutz, FL, USA, 2000. [Google Scholar]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms and Profiles; University of Vermont, Research Center for Children, Youth, and Families: Burlington, VT, USA, 2001. [Google Scholar]
- Conners, C.K.; Sitarenos, G.; Parker, J.D.; Epstein, J.N. The revised Conners’ Parent Rating Scale (CPRS-R): Factor structure, reliability, and criterion validity. J. Abnorm. Child Psychol. 1998, 26, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Delis, D.C.; Kaplan, E.; Kramer, J.H. Delis-Kaplan Executive Function System (D-KEFS); The Psychological Corporation: San Antonio, TX, USA, 2001. [Google Scholar]
- Mueller, S.T. The PEBL Manual, Version 0.11; Lulu Press: Raleigh, NC, USA, 2010; ISBN 978-055-765-817-6. [Google Scholar]
- Wechsler, D. Wechsler Abbreviated Scale of Intelligence; The Psychological Corporation; Harcourt Brace & Company: New York, NY, USA, 1999. [Google Scholar]
- Armstrong, J.M.; Goldstein, L.H.; The MacArthur Working Group on Outcome Assessment. Manual for the MacArthur Health and Behavior Questionnaire (HBQ 1.0); University of Pittsburgh: Pittsburgh, PA, USA, 2003. [Google Scholar]
- Berry, C.A.; Quinn, K.; Wolf, R.; Mosnaim, G.; Shalowitz, M. Validation of the Spanish and English versions of the asthma portion of the Brief Pediatric Asthma Screen Plus among Hispanics. Ann. Allergy Asthma Immunol. 2005, 95, 53–60. [Google Scholar] [CrossRef]
- Lyons, D.M.; Parker, K.J.; Katz, M.; Schatzberg, A.F. Developmental cascades linking stress inoculation, arousal regulation, and resilience. Front. Behav. Neurosci. 2009, 3. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.P.; Boyce, W.T.; McEwen, B.S. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA 2009, 301, 2252–2259. [Google Scholar] [CrossRef] [PubMed]
- Best, J.R.; Miller, P.H.; Jones, L.L. Executive functions after age 5: Changes and correlates. Dev. Rev. 2009, 29, 180–200. [Google Scholar] [CrossRef] [PubMed]
- Samuels, J.; Shinn, M.; Buckner, J.C. Homeless Children: Update on Research, Policy, Programs, and Opportunities; Report prepared for the Office of the Assistant Secretary for Planning and Evaluation; U.S. Department of Health and Human Services: Washington, DC, USA, 2010.
- Boyce, W.T.; Ellis, B.J. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Dev. Psychopathol. 2005, 17, 271–301. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Roisman, G.I.; Long, J.D.; Burt, K.B.; Obradovic, J.; Riley, J.R.; Tellegen, A. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Dev. Psychol. 2005, 41, 733–746. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; McEwen, B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012, 106, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Hostinar, C.E.; Gunnar, M.R. The developmental effects of early life stress: An overview of current theoretical frameworks. Curr. Dir. Psychol Sci. 2013, 22, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Franke, H.A. Toxic Stress: Effects, Prevention and Treatment. Children 2014, 1, 390–402. [Google Scholar] [CrossRef] [PubMed]
- Taliaferro, L.A.; Borowsky, I.W. Beyond prevention: Promoting healthy youth development in primary care. Am. J. Public Health 2012, 102, S317–S321. [Google Scholar] [CrossRef] [PubMed]
- Hagan, J.F.; Shaw, J.S.; Duncan, P.M. (Eds.) Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 3rd ed.; American Academy of Pediatrics (AAP): Elk Grove Village, IL, USA, 2008. [Google Scholar]
- Ortiz, R.; Sibinga, E. The role of mindfulness in reducing the adverse effects of childhood stress and trauma. Children 2017, 4. [Google Scholar] [CrossRef] [PubMed]
| n (%) | Range | Mean (SD) | |
|---|---|---|---|
| Covariates | |||
| Male | 46 (53) | ||
| Race | |||
| African American | 55 (64) | ||
| Other | 27 (33) | ||
| Age | 9.1–11.9 | 10.5 (0.81) | |
| Predictors | |||
| Adversity: Cumulative Risk Index | 0–8 | 4.0 (1.8) | |
| Intellectual function: WASI Matrix Reasoning IQ (T-score) | 24–66 | 46.1 (10.6) | |
| Self-Regulation: Emotional Control Composite (Z-score) | −1.02–2.0 | 0.0 (0.73) | |
| Self-Regulation: Shifting/Inhibitory Control Task (scaled score) | 1–17 | 9.5 (3.1) | |
| Self-Regulation: Planning/Self-Monitoring Task (raw score) | 1–13 | 7.5 (2.5) | |
| Self-Regulation: BRIEF total (T-score) | 35.2–84 | 50.7 (11.4) | |
| Self-Regulation: BRIEF Behavioral Regulation Index (T-score) | 36–92 | 52.0 (14,5) | |
| Self-Regulation BRIEF Metacognition Index (T-score) | 31–89 | 50.5 (13.2) | |
| Health Outcomes | |||
| Physical Health Problems Index | 0.16–0.95 | 0.51 (0.23) | |
| Chronic Medical Conditions | 0–7 | 1.63 (1.69) | |
| Global Physical Health | 0–2.6 | 0.64 (0.62) | |
| Child-reported Respiratory Symptom Score | 0–5 | 2.0 (1.5) |
| Risk Factors | n (%) |
|---|---|
| Single parent household | 71 (83) |
| Presence of four or more children living in the home | 43 (50) |
| The child experienced the divorce of his or her parents | 42 (49) |
| The parent’s perceived level of stress was extremely stressful | 42 (49) |
| Parent under 18 years of age when first child was born | 36 (42) |
| The child saw violence happening to other people | 33 (38) |
| Parent education less than a high school degree | 30 (35) |
| The child saw a parent injured by another person | 26 (30) |
| The child was placed in foster care | 12 (14) |
| The child was the victim of physical or sexual abuse | 7 (8) |
| One of the child’s parents died | 5 (6) |
| Physical Health Problems Index (Parent-Reported) β (SE) | Child-Reported Respiratory Symptoms β (SE) | |
|---|---|---|
| Adversity/Cumulative Risk Index | 0.03 (0.02) * | 0.3 (0.1) ** |
| Intellectual Functioning | ||
| WASI Matrix Reasoning IQ (T-score) | −0.002 (0.002) | −0.02 (0.02) |
| Self-Regulation | ||
| Emotional Control Composite (Z-score) ^ | 0.1 (0.3) *** | 0.6 (0.2) * |
| Task Shifting and Inhibitory Control Task Score (scaled score) | −0.02 (0.008) * | −0.1 (0.05) * |
| Planning and Self-Monitoring Task Score (raw score) | −0.02 (0.01) | −0.1 (0.08) |
| BRIEF Total (T-score) ^ | 0.006 (0.002) ** | 0.03 (0.01) * |
| BRIEF Behavioral Regulation Index (T-score) ^ | 0.005 (0.001) ** | 0.03 (0.01) * |
| BRIEF Metacognition Index (T-score) ^ | 0.005 (0.002) * | 0.02 (0.01) |
| Health | ||
| Child-reported Respiratory Symptom Score | 0.05 (0.02) ** | --- |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barnes, A.J.; Lafavor, T.L.; Cutuli, J.J.; Zhang, L.; Oberg, C.N.; Masten, A.S. Health and Self-Regulation among School-Age Children Experiencing Family Homelessness. Children 2017, 4, 70. https://doi.org/10.3390/children4080070
Barnes AJ, Lafavor TL, Cutuli JJ, Zhang L, Oberg CN, Masten AS. Health and Self-Regulation among School-Age Children Experiencing Family Homelessness. Children. 2017; 4(8):70. https://doi.org/10.3390/children4080070
Chicago/Turabian StyleBarnes, Andrew J., Theresa L. Lafavor, J. J. Cutuli, Lei Zhang, Charles N. Oberg, and Ann S. Masten. 2017. "Health and Self-Regulation among School-Age Children Experiencing Family Homelessness" Children 4, no. 8: 70. https://doi.org/10.3390/children4080070






