Assessment of the Baby Friendly Hospital Initiative Implementation in the Eastern Mediterranean Region
Abstract
:1. Background
2. Methods
2.1. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bagchi, K. Nutrition in the Eastern Mediterranean region of the World Health Organization. East. Mediterr. Health J. 2008, 14, S107–S113. [Google Scholar] [PubMed]
- Hwalla, N.; Al Dhaheri, A.S.; Radwan, H.; Alfawaz, H.A.; Fouda, M.A.; Al-Daghri, N.M.; Zaghloul, S.; Blumberg, J.B. The prevalence of micronutrient deficiencies and inadequacies in the Middle East and approaches to interventions. Nutrients 2017, 9, 229. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Regional Committee for the Eastern Mediterranean. Regional Strategy on Nutrition 2010–2019. EM/RC57/4. Available online: http://applications.emro.who.int/docs/EM_RC57_4_en.pdf (accessed on 6 October 2016).
- Shetty, P. Achieving the goal of halving global hunger by 2015. Proc. Nutr. Soc. 2006, 65, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Horta, B.L.; Loret de Mola, C.; Quevendo, L.; Pinheiro, R.T.; Gigante, D.P.; Gonçalves, H.; Barros, F.C. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: A prospective birth cohort study from Brazil. Lancet Glob. Health 2015, 3, e199–e205. [Google Scholar] [CrossRef]
- Victoria, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Kaseverc, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 457–490. [Google Scholar] [CrossRef]
- Patro-Gołąb, B.; Zalewski, B.M.; Kołodziej, M.; Kouwenhoven, S.; Poston, L.; Godfrey, K.M.; Koletzko, B.; Goudoever, J.; Szajewska, H. Nutritional interventions or exposures in infants and children aged up to three years and their effects on subsequent risk of overweight, obesity, and body fat: A systematic review of systematic reviews. Obes. Rev. 2016, 17, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O. Overweight and obesity in Eastern Mediterranean region: Prevalence and possible causes. J. Obes. 2011, 2011, 407237. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O.; Hassan, A.S.; Obeid, O. The paradox of nutrition-related diseases in the Arab countries: The need for action. Int. J. Environ. Res. Public Health 2011, 8, 3637–3671. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O.; Al-Hazzaa, H.M. Prevalence and risk factors associated with nutrition-related noncommunicable diseases in the Eastern Mediterranean region. Int. J. Gen. Med. 2012, 5, 199–217. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Singh, G.; Yakoob, M.Y.; Abdollahi, M.; Al-Hooti, S.; et al. The impact of dietary habits and metabolic risk factors on cardiovascular and diabetes mortality in countries of the Middle East and North Africa in 2010: A comparative risk assessment analysis. BMJ Open 2015, 5, e006385. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). National Implementation of the Baby Friendly Hospital Initiative, 2017; License CC BY-NC-SA 3.0 IGO; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Framework for Health Information Systems and Core Indicators for Monitoring Health Situation and Health System Performance. WHO-EMRO, 2015. Available online: http://applications.emro.who.int/dsaf/EMROPUB_2015_EN_1904.pdf?ua=1&ua=1 (accessed on 1 March 2016).
- Martin, L.; Moazzem Hossain, S.M.; Casanovas, C.; Guyon, A. Learning from Large Scale Community-Based Programmes to Improve Breastfeeding Practices; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Al-Nuaimi, N.; Katende, G.; Arulappan, J. Breastfeeding Trends and Determinants Implications and recommendations for Gulf Cooperation Council countries. Sultan Qaboos Univ. Med. J. 2017, 17, e155–e161. [Google Scholar] [CrossRef] [PubMed]
- United Nations International Children’s Emergency Fund (UNICEF). Nutrition: Current Status and Progress. Available online: Data.unicef.org/topic/nutrition/infant-and-young-child-feeding (accessed on 1 March 2017).
- Al Juaid, D.A.; Binns, C.W.; Giglia, R.C. Breastfeeding in Saudi Arabia: A review. Int. Breastfeed. J. 2014, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Dashti, M.; Scott, J.A.; Edwards, C.A.; Al-Sughayer, M. Determinants of breastfeeding initiation among mothers in Kuwait. Int. Breastfeed. J. 2010, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Radwan, H. Influences and Determinants of Breastfeeding and Weaning Practices of Emirati Mothers. Ph.D. Thesis, Teesside University, Middleborough, UK, 2013. [Google Scholar]
- Ayed, A.A. Knowledge, attitude and practice regarding exclusive breastfeeding among mothers attending primary health care centers in Abha city. Int. J. Med. Sci. Public Health 2014, 3, 1355–1363. [Google Scholar] [CrossRef]
- Otolorin, E.; Gomez, P.; Currie, S.; Thapa, K.; Dao, B. Essential basic and emergency obstetric and newborn care: From education and training to service delivery and quality of care. Int. J. Gynecol. Obs. 2015, 130, S46–S53. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Abubakar, I.I.; Tillmann, T.; Banerjee, A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Lim, S.S.; Allen, K.; Bhutta, Z.A.; Dandona, L.; Forouzanfar, M.H.; Fullman, N.; Gething, P.W.; Goldberg, E.M.; Hay, S.I.; Holmberg, M.; et al. Measuring the health-related sustainable development goals in 188 countries: A baseline analysis from the global burden of disease study 2015. Lancet 2016, 388, 1813–1850. [Google Scholar] [CrossRef] [Green Version]
- Al Shehri, A.; Al Fattani, A.; Al Alwan, I. Obesity among Saudi children. Saudi J. Obes. 2013, 1, 3–9. [Google Scholar] [CrossRef]
- Ministry of Health and Population. Ministerial Decree 36/2014; Ministry of Health and Population: Cairo, Egypt, 2014.
- Bannor, R.; Asare, A.K.; Bawole, J.N. Effectiveness of social media for communicating health messages in Ghana. Health Educ. 2017, 117, 342–371. [Google Scholar] [CrossRef]
- Feldman-Winter, L.; Barone, L.; Milcarek, B.; Hunter, K.; Meek, J.; Morton, J.; Williams, T.; Naylor, A.; Lawrence, R.A. Residency Curriculum Improves Breastfeeding Care. Pediatrics 2010, 126, 289–297. [Google Scholar] [CrossRef] [PubMed]
- World Health Assembly Resolution, WHA69.9. Ending Inappropriate Promotion of Foods for Infants and Young Children; Agenda Item 12.1; WHO: Geneva, Switzerland, 28 May 2016. [Google Scholar]
- Food and Agriculture Organization. Joint FAO/WHO food standards programme codex committee on nutrition and foods special dietary uses. In Proceedings of the Thirty-Eighth Session; Food and Agriculture Organization: Hamburg, Germany, 2016. [Google Scholar]
- Nasreddine, L.; Hwalla, N.; Saliba, A.; Akl, C.; Naja, F. Prevalence and correlates of preschool overweight and obesity amidst the nutrition transition: Findings from a national cross-sectional study in Lebanon. Nutrients 2017, 9, 266. [Google Scholar] [CrossRef] [PubMed]
- Oot, L.; Sethuraman, K.; Ross, J.; Sommerfelt, A.E. The Effect of Suboptimal Breastfeeding on Preschool Overweight/Obesity: A Model in PROFILES for Country-Level Advocacy. Available online: http://pdf.usaid.gov/pdf_docs/PA00MNT3.pdf (accessed on 1 March 2017).
- World Health Organization; Regional office for the Eastern Mediterranean. Food marketing to children and adolescents in the Eastern Mediterranean region: Implications for public health. In Proceedings of the 54th Session Regional Committee for the Eastern Mediterranean, Cairo, Egypt, 20–23 October 2007; EM/RC54/Tech.Disc.2. Available online: http://www.emro.who.int/rc54/media/pdf/EMRC54TECHDISC02en.pdf (accessed on 30 July 2008).
| Group I: Advanced Nutrition Transition | Group II: Early Nutrition Transition | Group III: High Acute and Chronic Malnutrition | Group IV: Complex Emergency, Severe Child and Maternal Undernutrition | ||||
|---|---|---|---|---|---|---|---|
| Country | Designated Hospitals | Country | Designated Hospitals | Country | Designated Hospitals | Country | Designated Hospitals |
| Iran | 376 | Egypt | 13 | Djibouti | 4 | Afghanistan | 18 |
| Tunisia | 141 | Jordan | 3 | Iraq | 15 | Somalia | 0 |
| Kuwait | 1 | Lebanon | 21 | Pakistan | 42 | Syria | 21 |
| Bahrain | 6 | Morocco | 17 | Sudan | 25 | Yemen | 0 |
| Qatar | 0 | Palestine | 0 | Libya | 0 | ||
| UAE | 15 | ||||||
| Oman | 51 | ||||||
| Saudi Arabia | 60 | ||||||
| Total (832) | 650 | 57 | 86 | 39 | |||
| Percent | 78.12 | 6.85 | 10.34 | 4.69 | |||
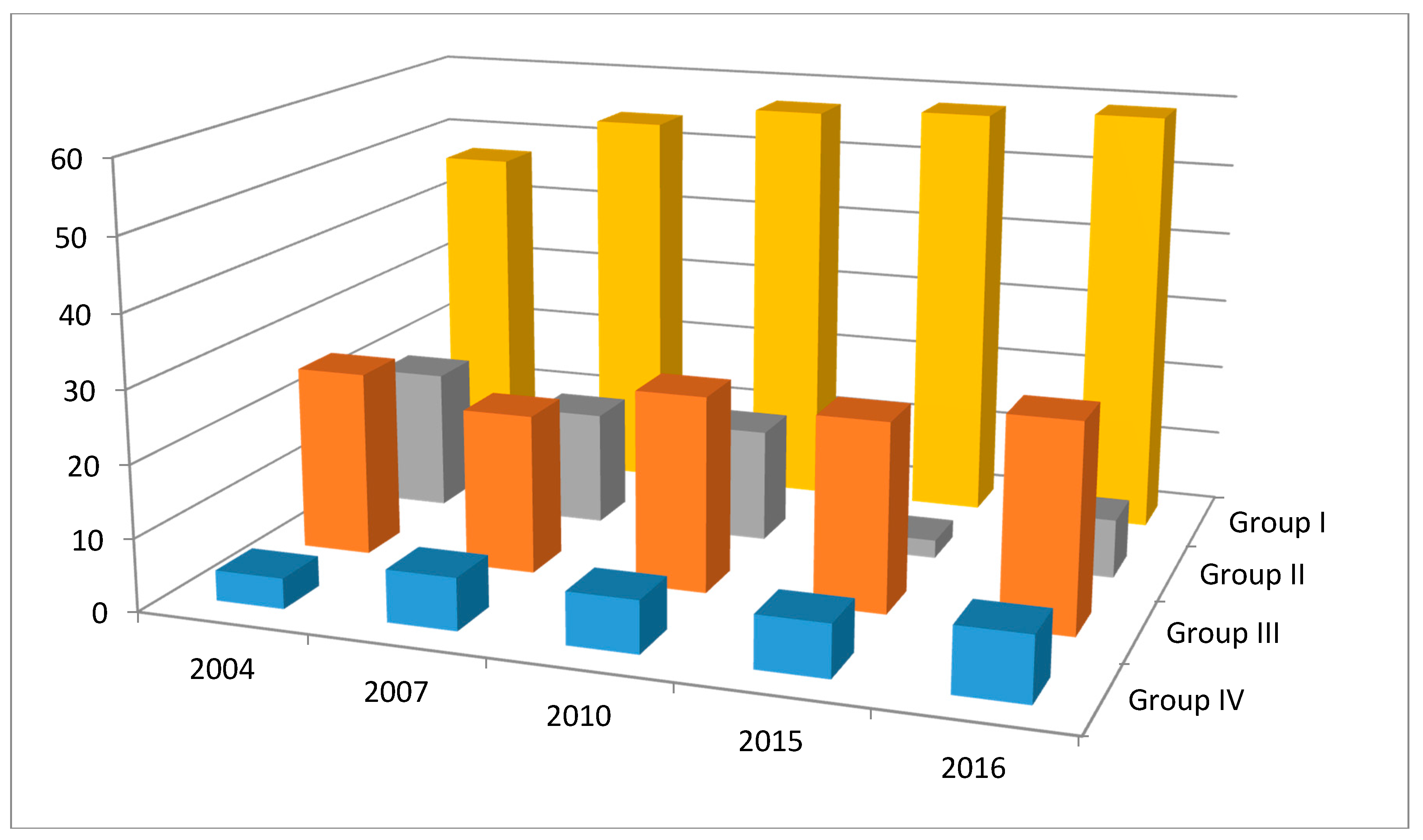
| Country by Group | 2004 (%) | 2007 (%) | 2010 (%) | 2015 (%) | 2016 (%) |
|---|---|---|---|---|---|
| Group I: Advanced nutrition transition | |||||
| Iran | 94 | 96 | 96 | 86 | 86 |
| Tunisia | 93 | 93 | 93 | - | 93 |
| Kuwait | 33 | 33 | 33 | 25 | 25 |
| Bahrain | 21 | 21 | 21 | - | 23 |
| Qatar | 0 | 50 | 50 | 50 | 50 |
| United Arab Emirates | 40 | 40 | 59 | 65 | 70 |
| Oman | 100 | 100 | 100 | 100 | 100 |
| Saudi Arabia | 1 | 2 | 7 | 24 | 24.1 |
| Range | 1–100 | 2–100 | 7–100 | 25–100 | 23–100 |
| Mean percent | 47.75 | 54.4 | 57.38 | 58.33 | 58.89 |
| SD | ±42.05 | ±37.50 | ±36.05 | ±31.32 | ±32.59 |
| Group II: Early nutrition transition | |||||
| Egypt | 3 | 3 | 3 | 0 | 5 |
| Jordan | 49 | 4 | 4 | 4 | 4 |
| Lebanon | 16 | 16 | 9 | 0 | 21 |
| Morocco | 17 | 38 | 38 | 5 | 5 |
| Palestine | 0 | 0 | 0 | 0 | 0 |
| Range | 0–49 | 0–38 | 0–38 | 0–5 | 0–21 |
| Mean | 17 | 12.2 | 10.8 | 1.8 | 7 |
| SD | ±19.43 | ±15.66 | ±15.55 | ±2.49 | ±8.09 |
| Group III: Chronic malnutrition | |||||
| Djibouti | 0 | 0 | 0 | 0 | 0 |
| Iraq | 55 | 49 | 59 | - | 21 |
| Sudan | 9 | 11 | 11 | 0 | 11 |
| Pakistan | 4 | 7 | 7 | 0 | 65 |
| Range | 0–55 | 7–49 | 7–59 | 0 | 11–65 |
| Mean | 17 | 16.75 | 19.25 | 0 | 24.25 |
| SD | +25.59 | +21.98 | +26.89 | 0 | +28.49 |
| Group IV: Complex emergency situations | |||||
| Afghanistan | 1 | 1 | 1 | 1 | 17.3 |
| Libya | 0 | 0 | 0 | 0 | 0 |
| Somalia | 0 | 0 | 0 | 0 | 2 |
| Syrian Arab Republic | 20 | 35 | 35 | 35 | 25 |
| Yemen | 0 | 0 | 0 | 0 | 0 |
| Range | 0–20 | 0–35 | 0–35 | 0–35 | 0–25 |
| Mean | 4.2 | 7.2 | 7.2 | 7.2 | 8.86 |
| SD | ±8.84 | ±15.55 | ±15.54 | ±15.5 | ±11.57 |
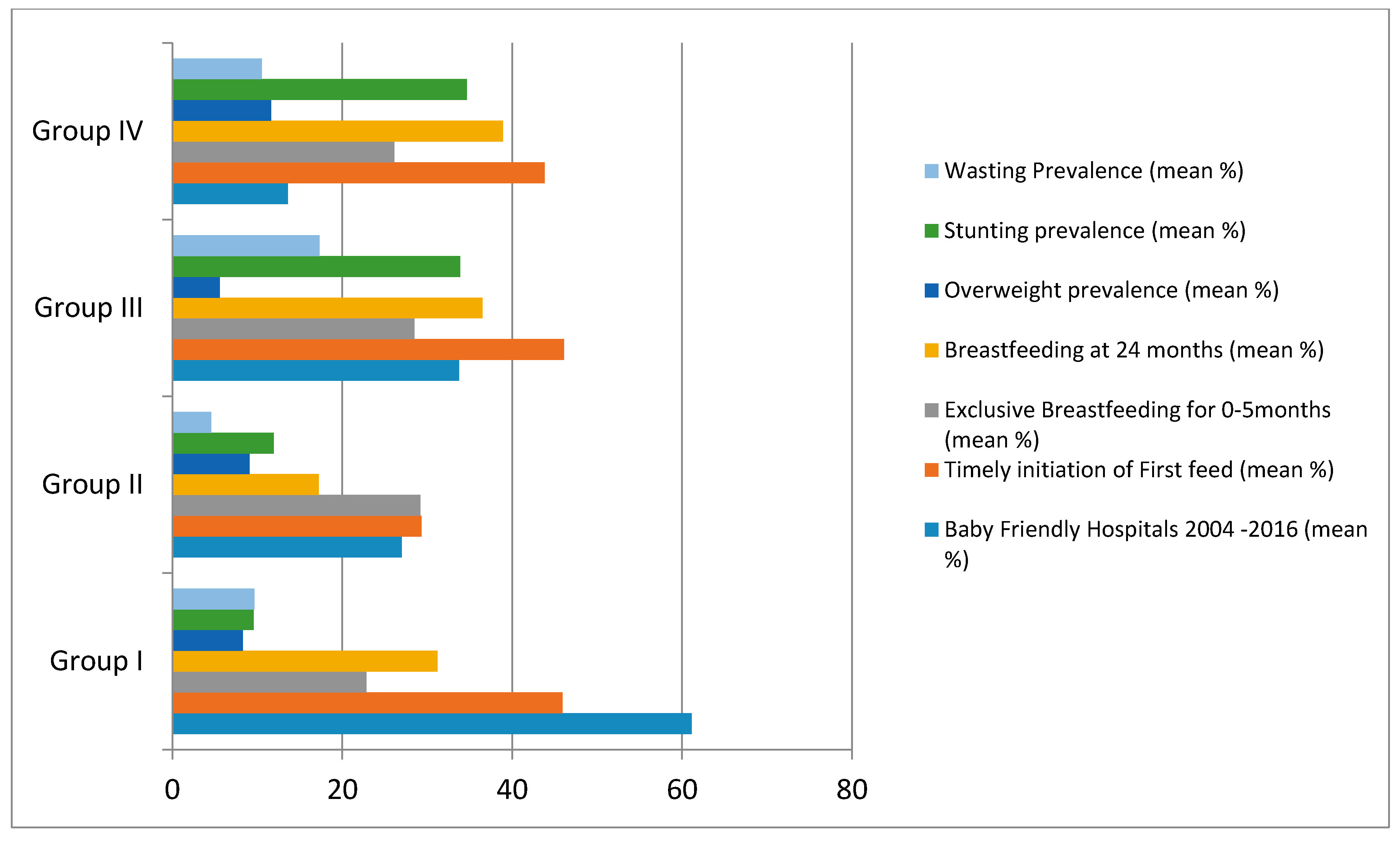
| Country by Group | Baby Friendly Hospitals 2004–2016 (%) | Timely Initiation of First Feed (%) | Exclusive Breastfeeding for 6 Months (%) | Continued Breastfeeding for 24 Months (%) | Overweight Prevalence (%) | Stunting Prevalence (%) | Wasting Prevalence (%) | |
|---|---|---|---|---|---|---|---|---|
| Group I (8) | ||||||||
| Range | 23–100 | 1–71.1 | 8.5–53.1 | 9–51 | 1.9–15 | 4.9–10.1 | 2.1–10.1 | |
| Mean | 1378.33 | 21.37 | 19.87 | 25.33 | 8.29 | 9.55 | 9.65 | |
| SD | ±32.88 | ±33.42 | ±15.90 | ±14.90 | ±4.57 | ±3.28 | ±3.98 | |
| Group II (5) | ||||||||
| Range | 0–49 | 0–41.3 | 22.7–39.7 | 10.6–25 | 5.7–15.5 | 7.3–22.3 | 1.2–9.5 | |
| Mean | 27 | 29.3 | 29.2 | 17.225 | 9.075 | 11.92 | 4.54 | |
| SD | ±20.08 | ±9.39 | ±7.33 | ±6.34 | ±5.03 | ±6.637 | ±3.426 | |
| Group III (4) | ||||||||
| Range | 0–65 | 18–68.7 | 1.3–55.4 | 18.4–56.1 | 3.1–10.1 | 22.6–45 | 7.433 | |
| Mean | 22 | 28 | 20.48 | 21.931 | 4.569 | 33.875 | 17.3 | |
| SD | ±29.59 | ±21.51 | ±23.29 | ±18.74 | ±3.93 | ±9.78 | ±11.32 | |
| Group IV (5) | ||||||||
| Range | 0–35 | 0–53.6 | 5.3–43.3 | 24.9–58.6 | 4–20.15 | 21.0–42.1 | 6.5–16.3 | |
| Mean | 13.6 | 43.8 | 26.1 | 38.9 | 11.6 | 34.66 | 10.54 | |
| SD | ±19.66 | ±14.07 | ±21.25 | ±11.27 | ±6.88 | ±12.10 | ±4.1476 | |
| Correlations with nutritional indices | ||||||||
| Children under five | Timely first suckle for all country groups | Exclusive breastfeeding for all country groups | Continued breastfeeding for 12 months & 24 months for all country groups | |||||
| First hour of life | p-value | (0–5 mo) | p-value | At 12 mo | At 24 mo | p-value | ||
| Stunting | r = 0.09 | p > 0.05 | r = 0.05 | p > 0.05 | r = 0.69 * | r = 0.908 ** | p < 0.001 p < 0.01 p > 0.05 | |
| Wasting | r = 0.22 | p > 0.05 | r = 0.13 | p > 0.05 | r = 0.67 * | r = 0.87 ** | ||
| Overweight | r = 0.51 * | p < 0.05 | r = 0.11 | p > 0.05 | r = 0.05 | r = 0.36 | ||
| Obesity | r = 0.51 * | p < 0.05 | r = 0.22 | p > 0.05 | r = 0.475 * | r = 0.33 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Jawaldeh, A.; Abul-Fadl, A. Assessment of the Baby Friendly Hospital Initiative Implementation in the Eastern Mediterranean Region. Children 2018, 5, 41. https://doi.org/10.3390/children5030041
Al-Jawaldeh A, Abul-Fadl A. Assessment of the Baby Friendly Hospital Initiative Implementation in the Eastern Mediterranean Region. Children. 2018; 5(3):41. https://doi.org/10.3390/children5030041
Chicago/Turabian StyleAl-Jawaldeh, Ayoub, and Azza Abul-Fadl. 2018. "Assessment of the Baby Friendly Hospital Initiative Implementation in the Eastern Mediterranean Region" Children 5, no. 3: 41. https://doi.org/10.3390/children5030041




