Irritability is Common and is Related to Poorer Psychosocial Outcomes in Youth with Functional Abdominal Pain Disorders (FAPD)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Questionnaires
2.2.1.1. Background and Demographics
2.2.1.2. FGID Status
2.2.1.3. Irritability Measure
Affective Reactivity Index (ARI, Parent and Child Report)
2.2.1.4. Measures of Psychological, Family-Related and Pain-Related Functioning
Functional Disability Index (FDI, Parent and Child Report)
Pain Catastrophizing Scale (PCS, Child Report)
Child Depression Inventory (CDI-2, Child Report)
Screen for Child Anxiety-Related Disorders (SCARED, Parent and Child Report)
Depression Anxiety Stress Scales (DASS-21, Parent Report)
2.2.2. Statistical Analyses
3. Results
3.1. Participant Characteristics
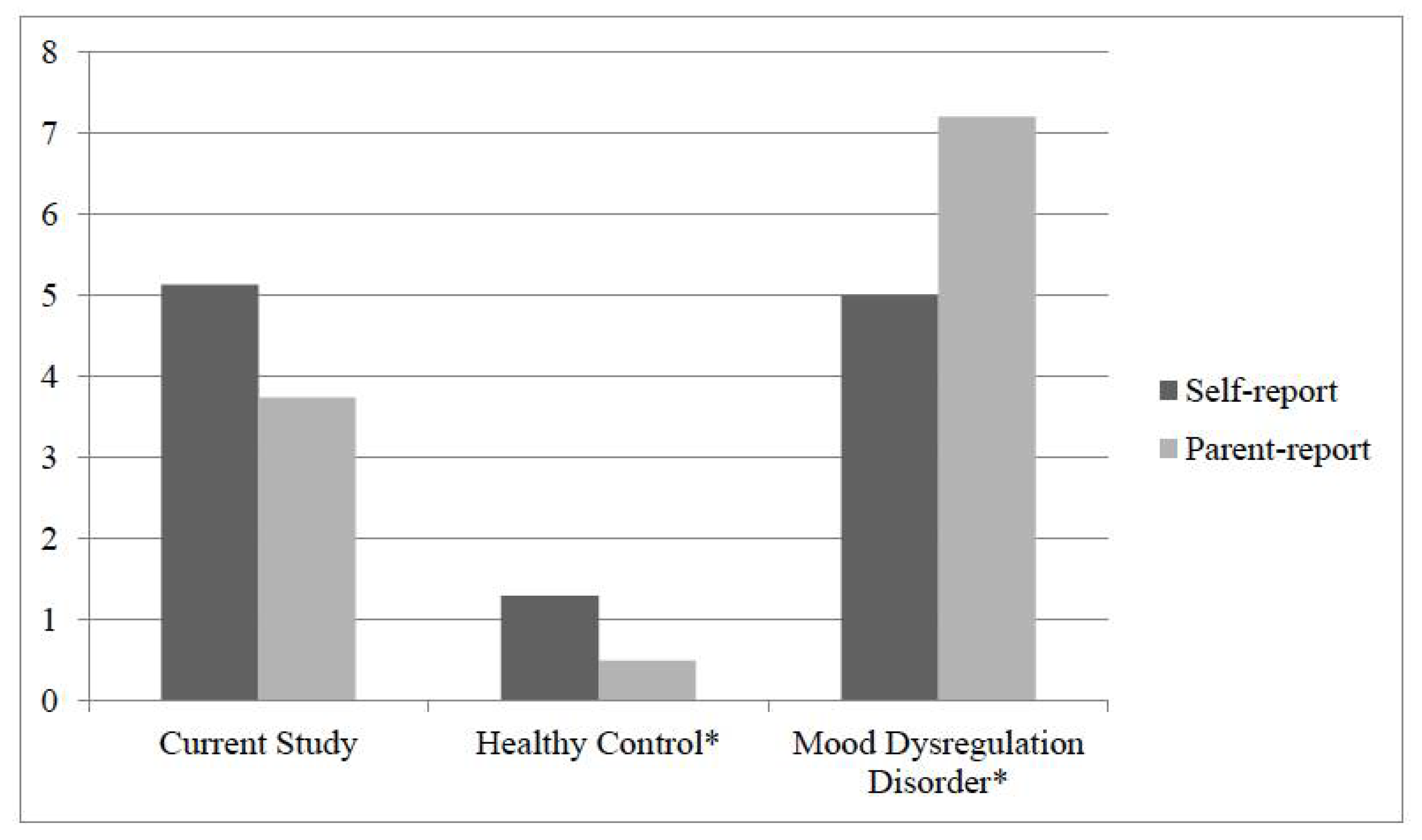
3.2. Rates of Irritability in Youth with FAPD vs. Validation Samples
3.3. Irritability in Relation to other Psychosocial and Pain-Related Outcomes
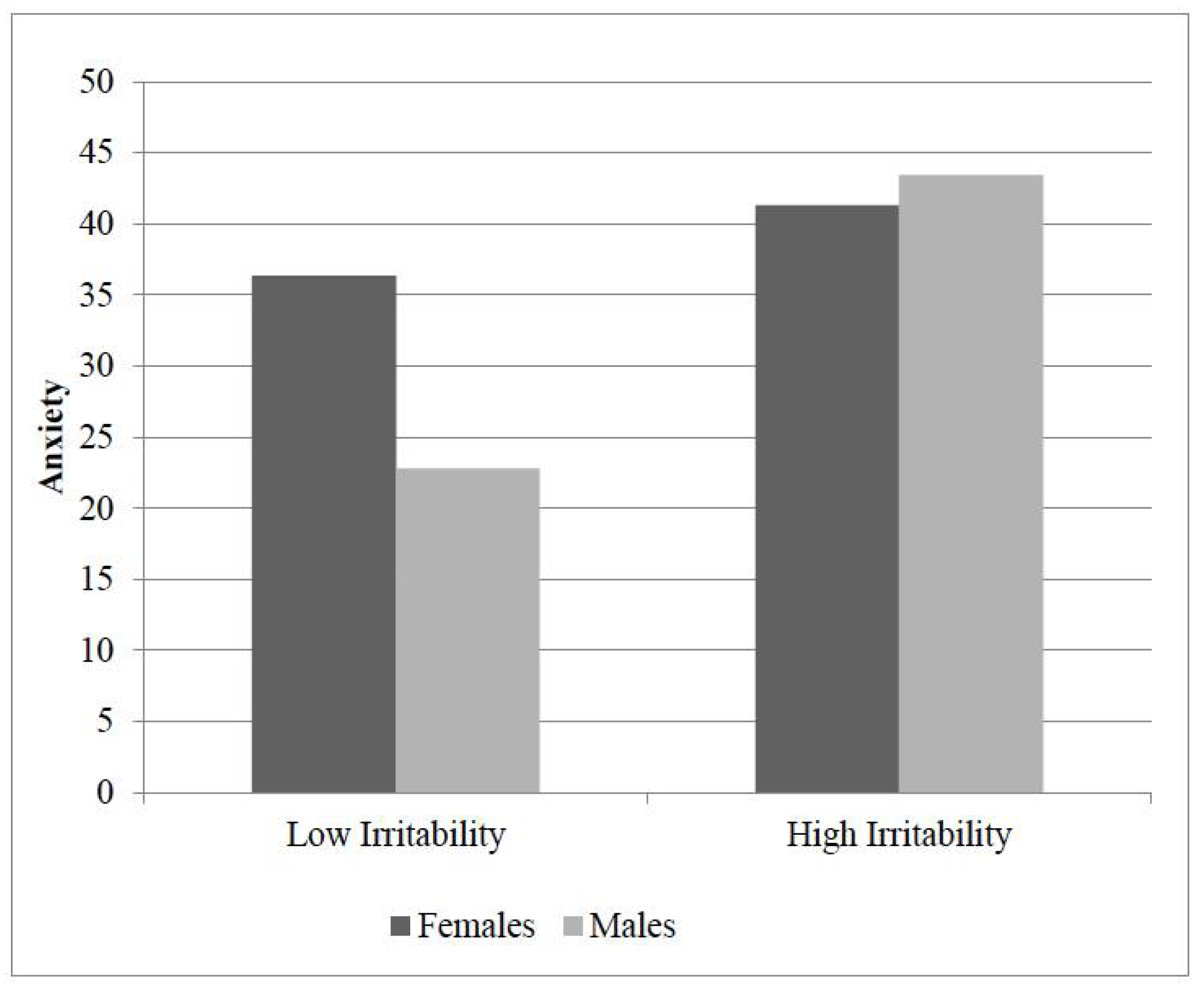
3.4. Irritability by Gender
3.5. Moderator Analyses
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Campo, J.V.; Bridge, J.; Ehmann, M.; Altman, S.; Lucas, A.; Birmaher, B.; Di Lorenzo, C.; Iyengar, S.; Brent, D.A. Recurrent abdominal pain, anxiety, and depression in primary care. JAMA Pediatr. 2004, 113, 817–824. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Lynch-Jordan, A.; Mezoff, A.G.; Farrell, M.K.; Cohen, M.B.; Kashikar-Zuck, S. Importance of addressing anxiety in youth with functional abdominal pain: Suggested guidelines for physicians. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Rasquin, A.; Di Lorenzo, C.; Forbes, D.; Guiraldes, E.; Hyams, J.S.; Staiano, A.; Walker, L.S. Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology 2006, 130, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Wu, J.; Ma, Y.L.; Tsang, A.; GUO, W.J.; Sung, J. Irritable bowel syndrome is strongly associated with generalized anxiety disorder: A community study. Aliment. Pharmacol. Therapeut. 2009, 30, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Fond, G.; Loundou, A.; Hamdani, N.; Boukouaci, W.; Dargel, A.; Oliveira, J.; Roger, M.; Tamouza, R.; Leboyer, M.; Boyer, L. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): A systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2014, 264, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Canavan, C.; West, J.; Card, T. The epidemiology of irritable bowel syndrome. Clin. Epidemiol. 2014, 6, 71. [Google Scholar] [PubMed]
- Muscatello, M.R.; Bruno, A.; Mento, C.; Pandolfo, G.; Zoccali, R.A. Personality traits and emotional patterns in irritable bowel syndrome. World J. Gastroenterol. 2016, 22, 6402. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, N.R.; Jagpal, A.; Peugh, J.; Farrell, M.K.; Cohen, M.B.; Mezoff, A.G.; Lynch-Jordan, A.; Kashikar-Zuck, S. Risk Categorization Predicts Disability in Pain-associated Functional Gastrointestinal Disorders after 6 Months. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Lader, M. Generalized anxiety disorder. In Encyclopedia of Psychopharmacology; Springer: Berlin/Heidelberg, Germany, 2015; pp. 699–702. [Google Scholar]
- Cunningham, N.R.; Lynch-Jordan, A.; Barnett, K.; Peugh, J.; Sil, S.; Goldschneider, K.; Kashikar-Zuck, S. Child pain catastrophizing mediates the relation between parent responses to pain and disability in youth with functional abdominal pain. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.; Zeman, J.; Walker, L.S. Recurrent abdominal pain in children: Psychiatric diagnoses and parental psychopathology. J. Am. Acad. Child Adolesc. Psychiatry 1990, 29, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Garber, J.; Greene, J.W. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J. Abnorm. Psychol. 1993, 102, 248. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Sherman, A.L.; Bruehl, S.; Garber, J.; Smith, C.A. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 2012, 153, 1798–1806. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics Subcommittee on Chronic Abdominal Pain. Chronic abdominal pain in children. Pediatrics 2005, 115, 812. [Google Scholar]
- Stringaris, A.; Goodman, R.; Ferdinando, S.; Razdan, V.; Muhrer, E.; Leibenluft, E.; Brotman, M.A. The Affective Reactivity Index: A concise irritability scale for clinical and research settings. J. Child Psychol. Psychiatry 2012, 53, 1109–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub.: Washington, DC, USA, 2013. [Google Scholar]
- Dennis, T.A. Interactions between emotion regulation strategies and affective style: Implications for trait anxiety versus depressed mood. Motiv. Emot. 2007, 31, 200–207. [Google Scholar] [CrossRef]
- Stoddard, J.; Stringaris, A.; Brotman, M.A.; Montville, D.; Pine, D.S.; Leibenluft, E. Irritability in child and adolescent anxiety disorders. Depress. Anxiety 2014, 31, 566–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, N.R.; Jagpal, A.; Tran, S.T.; Kashikar-Zuck, S.; Goldschneider, K.R.; Coghill, R.C.; Lynch-Jordan, A.M. Anxiety adversely impacts response to cognitive behavioral therapy in children with chronic pain. J. Pediatr. 2016, 171, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Zeman, J.L. Parental response to child illness behavior. J. Pediatr. Psychol. 1992, 17, 49–71. [Google Scholar] [CrossRef] [PubMed]
- Lipani, T.A.; Walker, L.S. Children’s appraisal and coping with pain: Relation to maternal ratings of worry and restriction in family activities. J. Pediatr. Psychol. 2006, 31, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Parker, G.; Brotchie, H. Gender differences in depression. Int. Rev. Psychiatry 2010, 22, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Charbonneau, A.M.; Mezulis, A.H.; Hyde, J.S. Stress and emotional reactivity as explanations for gender differences in adolescents’ depressive symptoms. J. Youth Adolesc. 2009, 38, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Logan, D.E.; Claar, R.L.; Scharff, L. Social desirability response bias and self-report of psychological distress in pediatric chronic pain patients. Pain 2008, 136, 366–372. [Google Scholar] [CrossRef] [PubMed]
- McLean, C.P.; Anderson, E.R. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 2009, 29, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.R. Making sense of multiple informants in child and adolescent psychopathology: A guide for clinicians. J. Psychoeduc. Assess. 2007, 25, 139–149. [Google Scholar] [CrossRef]
- Berkout, O.V.; Young, J.N.; Gross, A.M. Mean girls and bad boys: Recent research on gender differences in conduct disorder. Aggress. Violent Behav. 2011, 16, 503–511. [Google Scholar] [CrossRef]
- Altemus, M.; Sarvaiya, N.; Epperson, C.N. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014, 35, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.A. Functional gastrointestinal disorders: History, pathophysiology, clinical features, and Rome IV. Gastroenterology 2016, 150, 1262–1279. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.A.; Dumitrascu, D.L. Rome III: New standard for functional gastrointestinal disorders. J. Gastrointest. Liver Dis. 2006, 15, 237. [Google Scholar]
- Claar, R.L.; Walker, L.S. Functional assessment of pediatric pain patients: Psychometric properties of the functional disability inventory. Pain 2006, 121, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Kashikar-Zuck, S.; Flowers, S.R.; Claar, R.L.; Guite, J.W.; Logan, D.E.; Lynch-Jordan, A.M.; Palermo, T.M.; Wilson, A.C. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain 2011, 152, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Bijttebier, P.; Eccleston, C.; Mascagni, T.; Mertens, G.; Goubert, L.; Verstraeten, K. The child version of the pain catastrophizing scale (PCS-C): A preliminary validation. Pain 2003, 104, 639–646. [Google Scholar] [CrossRef]
- Kovacs, M. The Children’s Depression, Inventory (CDI). Psychopharmacol. Bull. 1985, 21, 995–998. [Google Scholar] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders IV-TR; American Psychiatric Association: Washington, DC, USA, 2002. [Google Scholar]
- Birmaher, B.; Khetarpal, S.; Brent, D.; Cully, M.; Balach, L.; Kaufman, J.; Neer, S.M. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Jastrowski Mano, K.E.; Evans, J.R.; Tran, S.T.; Anderson Khan, K.; Weisman, S.J.; Hainsworth, K.R. The psychometric properties of the Screen for Child Anxiety Related Emotional Disorders in pediatric chronic pain. J. Pediatr. Psychol. 2012, 37, 999–1011. [Google Scholar] [CrossRef] [PubMed]
- Dorn, L.D.; Campo, J.C.; Thato, S.; Dahl, R.E.; Lewin, D.; Chandra, R.; Di Lorenzo, C. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, N.R.; Cohen, M.B.; Farrell, M.K.; Mezoff, A.G.; Lynch-Jordan, A.; Kashikar-Zuck, S. Concordant parent-child reports of anxiety predict impairment in youth with functional abdominal pain. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176. [Google Scholar] [CrossRef]
- George, D.; Mallery, P. IBM SPSS Statistics 23 Step by Step: A Simple Guide and Reference; Routledge: Abingdon, UK, 2016. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, T.R.; Birmaher, B.; Axelson, D.; Goldstein, B.I.; Gill, M.K.; Esposito-Smythers, C.; Ryan, N.D.; Strober, M.A.; Hunt, J.; Keller, M. Psychosocial functioning among bipolar youth. J. Affect. Disord. 2009, 114, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Hua, L.L.; Wilens, T.; Martelon, M.; Wong, P.; Wozniak, J.; Biederman, J. Psychosocial functioning, familiality, and psychiatric comorbidity in bipolar youth with and without psychotic features. J. Clin. Psychiatry 2011, 72, 397–405. [Google Scholar] [CrossRef] [PubMed]
- De Los Reyes, A.; Augenstein, T.M.; Wang, M.; Thomas, S.A.; Drabick, D.A.; Burgers, D.E.; Rabinowitz, J. The Validity of the Multi-Informant Approach to Assessing Child and Adolescent Mental Health; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Lynch-Jordan, A.M.; Kashikar-Zuck, S.; Goldschneider, K.R. Parent perceptions of adolescent pain expression: The adolescent pain behavior questionnaire. Pain 2010, 151, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Safdar, S.; Friedlmeier, W.; Matsumoto, D.; Yoo, S.H.; Kwantes, C.T.; Kakai, H.; Shigemasu, E. Variations of emotional display rules within and across cultures: A comparison between Canada, USA, and Japan. Can. J. Behav. Sci. 2009, 41, 1. [Google Scholar] [CrossRef]
- Martin, A.L.; McGrath, P.A.; Brown, S.C.; Katz, J. Anxiety sensitivity, fear of pain and pain-related disability in children and adolescents with chronic pain. Pain Res. Manag. 2007, 12, 267–272. [Google Scholar] [CrossRef] [PubMed]
- DeSousa, D.A.; Stringaris, A.; Leibenluft, E.; Koller, S.H.; Manfro, G.G.; Salum, G.A. Cross-cultural adaptation and preliminary psychometric properties of the Affective Reactivity Index in Brazilian Youth: Implications for DSM-5 measured irritability. Trends Psychiatry Psychother. 2013, 35, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Ribas, P.; Brotman, M.A.; Valdivieso, I.; Leibenluft, E.; Stringaris, A. The status of irritability in psychiatry: A conceptual and quantitative review. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 556–570. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Barlow, D.H. Incorporating Emotion Regulation into Conceptualizations and Treatments of Anxiety and Mood Disorders; American Psychological Association: Washington, DC, USA, 2007. [Google Scholar]
- Lenze, S.N.; Pautsch, J.; Luby, J. Parent-child interaction therapy emotion development: A novel treatment for depression in preschool children. Depress. Anxiety 2011, 28, 153–159. [Google Scholar] [CrossRef] [PubMed]
| Child Characteristics | n (%) |
|---|---|
| Age, mean (SD) | 11.5 (1.7) |
| Male | 26 (37.7) |
| Race | |
| White | 62 (89.9) |
| African American | 1 (1.4) |
| Asian | 1 (1.4) |
| Native Hawaiian/Other Pacific Islander | 0 (0) |
| American Indian | 1 (1.4) |
| Biracial | 4 (5.8) |
| mean (SD) | |
| Pain Intensity | 3.4 (1.9) |
| FDI | 18.3 (8.4) |
| CDI | 14.8 (9.2) |
| PCS | 26.9 (11.7) |
| SCARED | 36.1 (15.9) |
| ARI | 5.1 (4.2) |
| Parent/Caregiver Characteristics | n (%) |
| Male | 8 (11.6) |
| Mother Education Level | |
| High School | 13 (18.8) |
| Some College/Technical School | 21 (30.4) |
| College Degree | 23 (33.3) |
| Graduate Degree | 12 (17.4) |
| Father Education Level | |
| Less than High School | 5 (7.2) |
| High School | 22 (31.9) |
| Some College/Technical School | 19 (27.5) |
| College Degree | 17 (24.6) |
| Graduate Degree | 6 (8.7) |
| mean (SD) | |
| FDI, parent report | 14.4 (11.4) |
| SCARED, parent report | 31.2 (14.4) |
| ARI, parent report | 3.7 (4.0) |
| DASS Stress | 6.5 (4.4) |
| DASS Anxiety | 3.2 (4.1) |
| DASS Depression | 3.2 (3.9) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ARI Self-report | 1 | ||||||||||
| 2. ARI Parent-report | 0.484 ** | 1 | |||||||||
| 3. SCARED Self-report | 0.391 ** | 0.127 * | 1 | ||||||||
| 4. SCARED Parent-report | 0.263 | 0.351 | 0.553 ** | 1 | |||||||
| 5. FDI Self-report | 0.197 | 0.251 | 0.164 | 0.138 | 1 | ||||||
| 6. FDI Parent-report | 0.088 | 0.177 | 0.107 | 0.349 ** | 0.476 ** | 1 | |||||
| 7. CDI | 0.582 ** | 0.342 * | 0.554 ** | 0.242 | 0.295 * | 0.091 | 1 | ||||
| 8. PCS | 0.307 * | 0.098 | 0.404 ** | 0.175 | 0.276 * | 0.190 | 0.512 ** | 1 | |||
| 9. DASS Stress | 0.123 | 0.513 ** | 0.119 | 0.375 | 0.218 | 0.231 | 0.044 | 0.024 | 1 | ||
| 10. DASS Anxiety | 0.128 | 0.364 ** | 0.145 | 0.398 ** | 0.203 | 0.312 * | 0.045 | −0.011 | 0.647 ** | 1 | |
| 11. DASS Depression | −0.068 | 0.329 * | 0.064 | 0.363 | 0.148 | 0.339 ** | −0.027 | −0.002 | 0.597 ** | 0.702 ** | 1 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ARI Self-report | 1 | 0.567 ** | 0.252 | 0.242 | 0.197 | 0.169 | 0.574 ** | 0.249 | 0.093 | 0.195 | −0.047 |
| 2. ARI Parent-report | 0.411 | 1 | 0.144 | 0.227 | 0.125 | 0.152 | 0.524 ** | 0.029 | 0.282 | 0.233 | 0.094 |
| 3. SCARED Self-report | 0.593 ** | 0.212 | 1 | 0.430 * | 0.283 | 0.173 | 0.575 ** | 0.450 * | 0.093 | 0.131 | 0.005 |
| 4. SCARED Parent-report | 0.297 | 0.533 * | 0.691 ** | 1 | 0.096 | 0.322 | 0.317 | 0.209 | 0.204 | 0.291 | 0.144 |
| 5. FDI Self-report | 0.198 | 0.283 | 0.124 | 0.189 | 1 | 0.423 * | 0.342 | 0.252 | 0.001 | 0.253 | 0.144 |
| 6. FDI Parent-report | −0.066 | 0.194 | 0.063 | 0.403 | 0.559 * | 1 | 0.170 | 0.285 | 0.041 | 0.298 | 0.250 |
| 7. CDI | 0.627 ** | 0.269 | 0.519 * | 0.159 | 0.305 | 0.008 | 1 | 0.434 * | 0.078 | 0.189 | 0.028 |
| 8. PCS | 0.482 * | 0.403 | 0.315 | 0.130 | 0.465 | 0.085 | 0.613 ** | 1 | −0.010 | 0.041 | 0.054 |
| 9. DASS Stress | 0.139 | 0.587 * | 0.254 | 0.596 ** | 0.271 | 0.431 | 0.096 | 0.292 | 1 | 0.393 | 0.476 * |
| 10. DASS Anxiety | 0.048 | 0.405 | 0.218 | 0.529 * | 0.121 | 0.340 | −0.031 | 0.048 | 0.773 ** | 1 | 0.522 ** |
| 11. DASS Depression | −0.110 | 0.517 * | 0.152 | 0.611 ** | 0.122 | 0.466 | −0.058 | 0.004 | 0.705 ** | 0.849 ** | 1 |
| Model 1 | b | SE | β | t | p |
| Gender ^ | −5.690 | 3.637 | −0.174 | −1.565 | 0.122 |
| Irritability * | 1.502 | 0.420 | 0.398 | 3.578 | 0.001 |
| R2 = 0.183, F (2, 66) = 7.415, p = 0.001 | |||||
| Model 2 | |||||
| Gender ^ | −15.581 | 5.636 | −0.477 | −2.765 | 0.007 |
| Irritability * | 0.793 | 0.515 | 0.210 | 1.541 | 0.128 |
| Irritability *-by-Gender | 1.896 | 0.842 | 0.437 | 2.251 | 0.028 |
| ΔR2 = 0.059, ΔF (3, 65) = 5.069, p < 0.001 | |||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nelson, S.; Moorman, E.; Farrell, M.; Cunningham, N. Irritability is Common and is Related to Poorer Psychosocial Outcomes in Youth with Functional Abdominal Pain Disorders (FAPD). Children 2018, 5, 52. https://doi.org/10.3390/children5040052
Nelson S, Moorman E, Farrell M, Cunningham N. Irritability is Common and is Related to Poorer Psychosocial Outcomes in Youth with Functional Abdominal Pain Disorders (FAPD). Children. 2018; 5(4):52. https://doi.org/10.3390/children5040052
Chicago/Turabian StyleNelson, Sarah, Erin Moorman, Michael Farrell, and Natoshia Cunningham. 2018. "Irritability is Common and is Related to Poorer Psychosocial Outcomes in Youth with Functional Abdominal Pain Disorders (FAPD)" Children 5, no. 4: 52. https://doi.org/10.3390/children5040052




