Evaluation of the Omaha System Prototype Icons for Global Health Literacy
Abstract
:1. Introduction
1.1. Use of Symbols in the Digital World
1.2. Use of Symbols in Health Care
1.3. Interpretation of Visual Information to Transcend Communication Barriers
1.4. The Omaha System
2. Materials and Methods
2.1. Aim 1. Surveys
2.2. Aim 2. Focus Groups
3. Results
3.1. Aim 1. Surveys
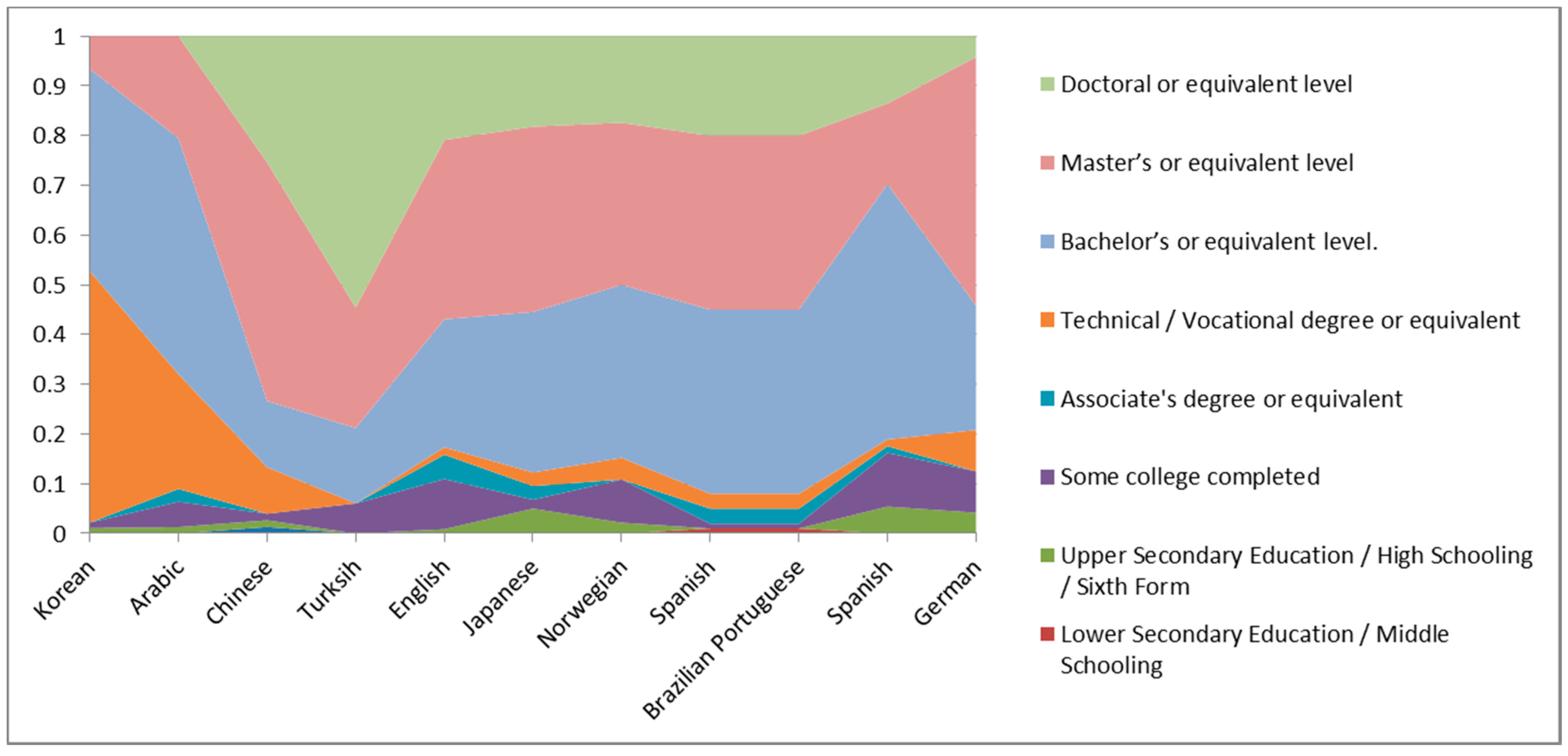
3.1.1. Level of Education of Respondents
3.1.2. Involvement in Professional Health Care
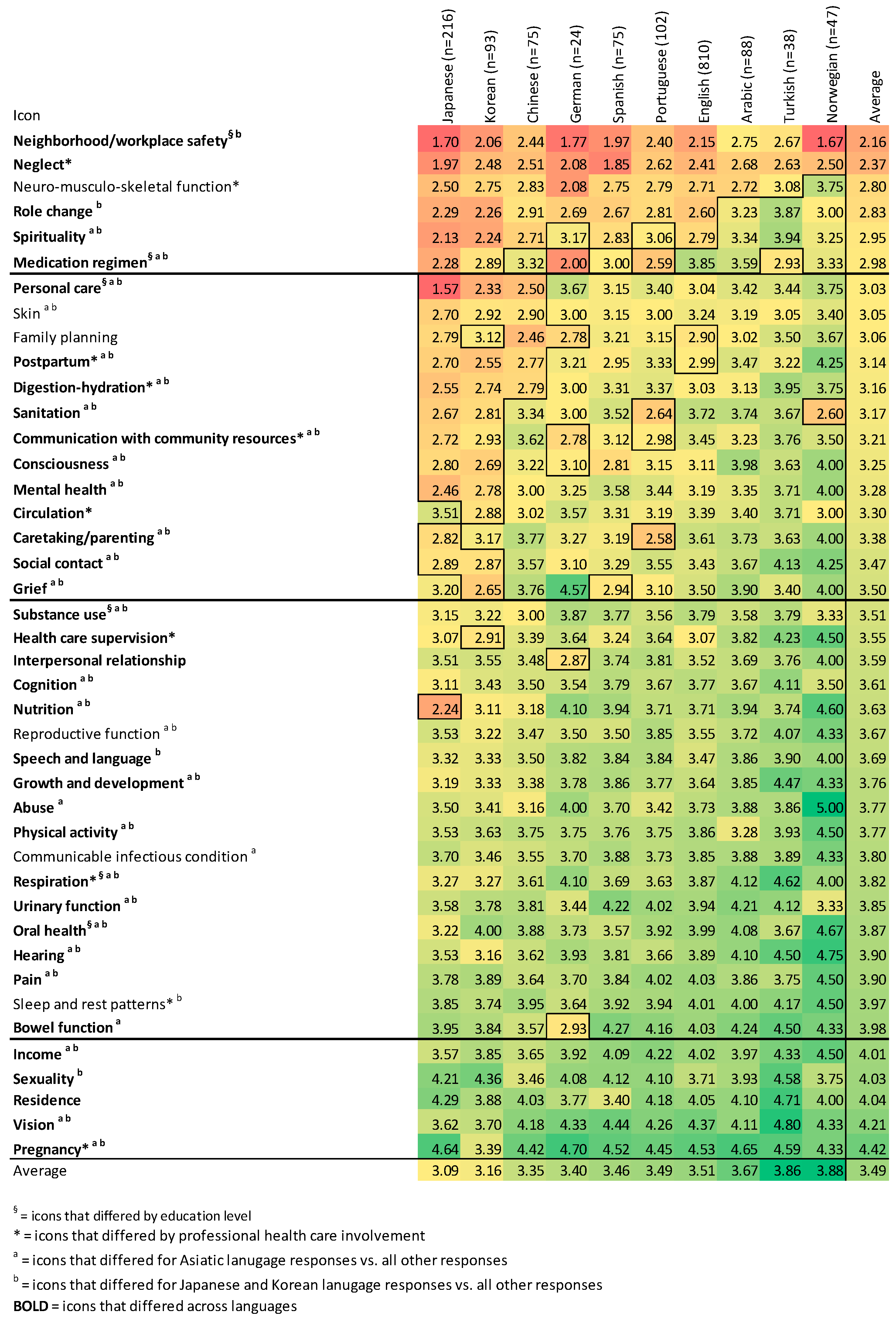
3.1.3. Overall Ratings
3.1.4. Ratings by Language
3.1.5. Patterns in Heat Map of Survey Results by Language and Overall
3.1.6. Comments Provided by Respondents
- Low literacy people may not be able to recognize the organs for bowel/the icon representing the Bowel function is too static, should be more dynamic to hint at the actual movement/organ for bowel may only be recognized by health care professionals.
- Consciousness and Mental health could be easily confused.
- For Neglect, have someone alone far away from a group of people/perhaps a closed door with another person outside with their back turned to indicate the seated figure is left alone/maybe have someone turning head away from another.
- Sexuality: This was a tough one to associate an image with. But should know more about sexuality rather than just being male or female. This is really about sexual behavior/activity/identification/intimacy.
- Most of the icons do not appeal to me.
- The mental health icon represents the image of a head, but for Japanese, they tend to associate the heart or chest with where the mind or spirit exists.
- Consciousness might exist in the brain.
- The symbol of oral health as dental floss looks American.
- These points of view are necessary if you use the icons globally.
- The human image is old-fashioned. It might be due to straight line instead of curvy line. And the human image is relatively large in icons of human group. And icons have both women and men but it might not be necessary. If so, then keep both of them equally.
- Overall, the icons are complicated and too much. It would be better to reduce the images in the icon and to show more intuitive images. I cannot get Digestion-hydration, Sanitation, and Post-partum but I like the way of Medication regimen and Growth & development.
- How about expressing breathing, actual action for respiratory icon?
- What does Rx mean? The Korean word for grief seems inappropriate (Figure 3).
- When you asked about vision, do you mean sight or look to the future?
- For example the symbol for blood circulation, I wanted to guess ‘heart’. If it had arrows to show blood in motion then maybe I would guess circulation.
- The sleeping person only invoked the word or idea of sleep but not the phrase ‘styles of sleep’.
- Pregnant woman should be shown sideways to show pregnancy bump.
- Dental hygiene should show a tooth brush.
- Nutrition should show a variety of fruit and vegetables
- Infectious diseases should show sneezing person more clearly.
- The message is not very clear with the Reproductive function. I see the image as a gynecological problem which is not always the same as reproductive function.
- For Hearing—the ear should be the only icon for hearing, it would be better understood if changed to sound waves.
- I do not understand why in some icons the red indicates a function and in others red indicates a problem.
- I believe that the Pain icon should express pain throughout the body and with a frown gesture
- Postpartum, too similar to the icon of pregnancy. Perhaps the female figure should have the arms holding the baby.
- Safety in the workplace/neighborhood: For me that icon represents neither the workplace nor the neighborhood.
- I think the eye icon does not have to refer to Vision, it could refer to the eye, so you should clarify.
- The icon of Cognition may be representative, but is more like calculation. You are on the right track but it can be improved
3.2. Aim 2. Focus Groups
- Challenging to depict abstract and/or complex concepts. Participants emphasized the challenges of depicting abstract concepts of Consciousness: “I think consciousness and higher thinking is so abstract it can be hard to portray the icon” and depicting complexity: Communication with community resources: “I think it fits well with the communication part but not the community resources part. I just see people in a circle talking.” An abstract icon displayed with a hint or a definition was more easily identified. For example, a participant explained “I think it definitely fits. It just took a little while, like the first time seeing it to get there. But now that I know it then, it like correlates once you know it”.
- Level of detail should be sufficient but not excessive. Participants tended to examine details of icons, missing the main message that the icon was intended to convey. For example, participants over-analyzed minute details as in this exchange regarding the Social contact icon.
- P1: Umm… I’m not sure why its red. Those look like coffee cups to me. Unless they are like cups of water? Maybe like that person’s a little higher so maybe that the lower person is the patient.
- P2: Yeah I would agree. So there are two cups of coffee on the table, two people maybe. We can’t see if they are holding hands or not… maybe something about interpersonal…
- P1: Maybe like patient care? Maybe? Yeah.
- P2: I do not see that because there’s nothing really… but I do see that one is higher so maybe… but when its smaller I’m not sure if you would be able to tell… Let’s see because this is a really good point… well this cup is also closer so maybe that another point or just how they are positioned.
- P2: ... Hold on, Hold on. So interpersonal stuff. Two individuals having a conversation about stuff. This one is a little lower well but the same height, that might not be necessary… And then uhh. I have no idea.
- P3: Their hands at first threw me off—are they holding hands? Could one of them, I think the coffee and the table bring them together and the hands under the table… what are they doing back there? That was my only thought about their body language, it’s definitely intimate. I assume they’re holding hands behind the table.
- P4: But if I were to imagine this without arms, it looks more confrontational.
- P3: What if they had that same body language, but one hand over the other. Maybe the ambiguity is good so it doesn’t look too romantic. It also looks a little romantic.
- Literal interpretation is common. Icons were interpreted literally, as in the case of a prototype for Mental health that was intended to show that thoughts needed healing, but instead participants interpreted the image as head trauma. Similarly, a participant commented regarding Caretaking/parenting: “I think it’s still difficult to show caretaking. The first thing you go to is family and not the aspects within the family”.
- Balance between simplicity and specificity. Participants said “I think simple is the way to go, it should not be very explicit because they have to learn [the icons/definitions], correct?” and more specific details tended to decrease the overall appreciation of the image, even while participants recognized the need for them in describing the icons.
- Balance between representing the definition of the concept fully vs. the essence of the definition. For example, the definition of the Medication regimen concept is “use or application of over-the-counter and prescribed/recommended medications and infusions to meet guidelines for therapeutic action, safety, and schedule” [17], p. 373. “I drew a lady who’s like throwing pills into her mouth… I have a pillbox with pills in front of it and I thought the lady taking them would kind of complete the circle so those are the three elements that I thought should be there: actually someone taking them, having them, and having them on your schedule to kind of map out some of the strategies you would use. But that’s probably a big icon”. Participants agreed that representing this concept with one oral medication (capsule) image would convey the essence of the concept sufficiently. This was common across the definitions. When provided with the definition, participants seemed to simplify the definition (synthesize in their heads) to a few key words.
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Environmental Domain |  |  |  |  | ||
| Income | Sanitation | Residence | Neighborhood/workplace safety | |||
| Psychosocial Domain |  |  |  |  |  |  |
| Communication with community resources | Social contact | Role change | Interpersonal relationship | Spirituality | Grief | |
 |  |  |  |  |  | |
| Mental health | Sexuality | Caretaking/parenting | Neglect | Abuse | Growth and development | |
| Physiological Domain |  |  |  |  |  |  |
| Hearing | Vision | Speech and language | Oral health | Cognition | Pain | |
 |  |  |  |  |  | |
| Consciousness | Skin | Nero-musculo-skeletal function | Respiration | Circulation | Digestion-hydration | |
 |  |  |  |  |  | |
| Bowel function | Urinary function | Reproductive function | Pregnancy | Postpartum | Communicable/infectious condition | |
| Health-related Behaviors Domain |  |  |  |  | ||
| Nutrition | Sleep and rest patterns | Physical activity | Personal care | |||
 |  |  |  | |||
| Substance use | Family planning | Health care supervision | Medication regimen |
References
- American Institute of Graphic Arts (AIGA). Symbol Signs. Available online: http://www.aiga.org/symbol-signs/ (accessed on 4 April 2017).
- Society for Experimental Graphic Design (SEGD). Healthcare Symbols. Available online: https://segd.org/healthcare-symbols (accessed on 4 April 2017).
- Wolpin, S.E.; Nguyen, J.K.; Parks, J.J.; Lam, A.Y.; Morisky, D.E.; Fernando, L.; Chu, A.; Berry, D.L. Redesigning pictographs for patients with low health literacy and establishing preliminary steps for delivery via smart phones. Pharm. Pract. 2016, 14, 686. [Google Scholar] [CrossRef] [PubMed]
- VCM: An Iconic Language for the Visualization of Concepts in Medicine. Available online: http://vcm.univ-paris13.fr/content/clinical-guidelines (accessed on 21 May 2017).
- Lamy, J.B.; Duclos, C.; Bar-Hen, A.; Ouvrard, P.; Venot, A. An iconic language for the graphical representation of medical concepts. BMC Med. Inform. Decis. Mak. 2008, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Lamy, J.B.; Soualmia, L.F.; Kerdelhué, G.; Venot, A.; Duclos, C. Validating the semantics of a medical iconic language using ontological reasoning. J. Biomed. Inform. 2013, 46, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Choi, J. Development and pilot test of pictograph-enhanced breast health-care instructions for community-residing immigrant women. Int. J. Nurs. Pract. 2012, 18, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Griffon, N.; Kerdelhué, G.; Hamek, S.; Hassler, S.; Boog, C.; Lamy, J.B.; Duclos, C.; Venot, A.; Darmoni, S. Design and usability study of an iconic user interface to ease information retrieval of medical guidelines. J. Am. Med. Inform. Assoc. 2014, 21, e270–e277. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Nakamura, C.; Zeng-Treitler, Q. Assessment of pictographs developed through a participatory design process using an online survey tool. J. Med. Internet Res. 2009, 11, e5. [Google Scholar] [CrossRef] [PubMed]
- Kripalani, S.; Robertson, R.; Love-Ghaffari, M.H.; Henderson, L.E.; Praska, J.; Strawder, A.; Katz, M.G.; Jacobson, T.A. Development of an illustrated medication schedule as a low-literacy patient education tool. Patient Educ. Couns. 2007, 66, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Lalloo, C.; Stinson, J.N.; Hochman, J.R.; Adachi, J.D.; Henry, J.L. Adapting the Iconic Pain Assessment Tool Version 2 (IPAT2) for adults and adolescents with arthritis pain through usability testing and refinement of pain quality icons. Clin. J. Pain 2013, 29, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Glassman, P. Health Literacy. Accessed from the National Network of Libraries of Medicine. Available online: http://nnlm.gov/outreach/consumer/hlthlit.html (accessed on 4 April 2017).
- Lee, T.W.; Lee, S.H.; Kim, H.H.; Kang, S.J. Effective intervention strategies to improve health outcomes for cardiovascular disease patients with low health literacy skills: A systematic review. Asian Nurs. Res. 2013, 6, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Brown, T. Change by Design: How Design Thinking Transforms Organizations and Inspires Innovation; HarperCollins: New York, NY, USA, 2009. [Google Scholar]
- Papanek, V. Design for the Real World: Human Ecology and Social Change, 2nd ed.; Van Nostrand Reinhold Company: New York, NY, USA, 1984. [Google Scholar]
- Reed, D.J.; Monk, A. Design for Inclusion. In Designing Accessible Technology; Clarkson, J., Langdon, P., Eds.; Springer: London, UK, 2006; pp. 53–63. [Google Scholar]
- Martin, K.S. The Omaha System: A Key to Practice, Documentation, and Information Management, reprinted 2nd ed.; Health Connections Press: Omaha, NE, USA, 2005. [Google Scholar]
- Monsen, K.A.; Martinson, B.; Lawrence, E.C.; Maki, T.A.; Stromme, A.E.; Weirich, E.G.; Martin, K.S. Toward population health literacy, wellbeing, consumer engagement, and informational exchange: Developing Omaha System icons for digital platforms. Int. J. Healthc. 2015, 2, 71–81. [Google Scholar] [CrossRef]
- Knight, E.; Gunawardena, C.N.; Aydin, C.H. Cultural interpretations of the visual meaning of icons and images used in North American web design. Educ. Media Int. 2009, 46, 17–35. [Google Scholar] [CrossRef]
- McMaster, S.R. Crowdsourcing Global Culture: Visual Representation in the Age of Information. Ph.D. Thesis, Concordia University, Montreal, QC, Canada, 1 September 2016. [Google Scholar]
- Drewal, H.J. Visual and Sensorial Aspects. In Ifá Divination, Knowledge, Power, and Performance; Olupona, J., Abiodun, R.A., Eds.; Indiana University Press: Bloomington, IN, USA, 2016; pp. 325–339. [Google Scholar]
- Blake Huer, M. Examining perceptions of graphic symbols across cultures: Preliminary study of the impact of culture/ethnicity. Augment. Altern. Commun. 2000, 16, 180–185. [Google Scholar] [CrossRef]
- Monsen, K.A.; Holland, D.E.; Fung-Houger, P.W.; Vanderboom, C.E. Seeing the whole person: Feasibility of using the Omaha System to describe strengths of older adults with chronic illness. Res. Theory Nurs. Pract. 2014, 28, 299–315. [Google Scholar] [CrossRef] [PubMed]
- Monsen, K.A.; Peters, J.; Schlesner, S.; Vanderboom, C.E.; Holland, D.E. The gap in Big Data: Getting to wellbeing, strengths, and a whole person perspective. Glob. Adv. Health Med. 2015, 4, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Omaha System Guidelines. Available online: http://omahasystemguidelines.org/ (accessed on 4 April 2017).
- Qualtrics. Research Made Simple. Available online: https://www.qualtrics.com/research-core/ (accessed on 4 April 2017).
- Parker, A.; Tritter, J. Focus Group Method and Methodology: Current Practice and Recent Debate. Int. J. Res. Method Educ. 2006, 29, 23–27. [Google Scholar] [CrossRef]
- Gehlenborg, N.; Wong, B. Points of view: Heat maps. Nat. Methods 2012, 9, 213. [Google Scholar] [CrossRef] [PubMed]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; SAGE Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- University of Minnesota Center for Nursing Informatics. Omaha System Partnership. Available online: http://omahasystempartnership.org (accessed on 21 May 2017).

| Domains: Environmental | Psychosocial | Physiological | Health-Related Behaviors |
|---|---|---|---|
| Income | Communication with community resources | Hearing | Nutrition |
| Sanitation | Social contact | Vision | Sleep and rest patterns |
| Residence | Role change | Speech and language | Physical activity |
| Neighborhood/workplace safety | Interpersonal relationship | Oral health | Personal care |
| Spirituality | Cognition | Substance use | |
| Grief | Pain | Family planning | |
| Mental health | Consciousness | Health care supervision | |
| Sexuality | Skin | Medication regimen | |
| Caretaking/parenting | Neuro-musculo-skeletal function | ||
| Neglect | Respiration | ||
| Abuse | Circulation | ||
| Growth and development | Digestion-hydration | ||
| Bowel function | |||
| Urinary function | |||
| Reproductive function | |||
| Pregnancy | |||
| Postpartum | |||
| Communicable/infectious condition |
| All Languages (ANOVA) | Japanese and Korean vs. All Others (Independent Samples t-Test) | Chinese, Japanese, and Korean vs. All Others (Independent Samples t-Test) | |||
|---|---|---|---|---|---|
| Comparison of Mean Ratings | Lower | Higher | Lower | Higher | |
| Significant differences (p < 0.05) | 36 | 31 | 1 | 30 | 0 |
| No differences | 6 | 8 | 2 | 10 | 2 |
| Total | 42 | 39 | 3 | 40 | 2 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monsen, K.A.; Kang, Y.J.; Maki, T.A.; Stromme, A.E.; Weirich, E.G.; Lawrence, E.C.; Schneider, R.N.; Martinson, B.E. Evaluation of the Omaha System Prototype Icons for Global Health Literacy. Informatics 2017, 4, 13. https://doi.org/10.3390/informatics4020013
Monsen KA, Kang YJ, Maki TA, Stromme AE, Weirich EG, Lawrence EC, Schneider RN, Martinson BE. Evaluation of the Omaha System Prototype Icons for Global Health Literacy. Informatics. 2017; 4(2):13. https://doi.org/10.3390/informatics4020013
Chicago/Turabian StyleMonsen, Karen A., Yu Jin Kang, Taylor A. Maki, Annika E. Stromme, Elizabeth G. Weirich, Emily C. Lawrence, Ryan N. Schneider, and Barbara E. Martinson. 2017. "Evaluation of the Omaha System Prototype Icons for Global Health Literacy" Informatics 4, no. 2: 13. https://doi.org/10.3390/informatics4020013






