Hardness, Cohesiveness, and Adhesiveness of Oral Moisturizers and Denture Adhesives: Selection Criteria for Denture Wearers
Abstract
:1. Introduction
2. Material and Methods
2.1. Tested Materials
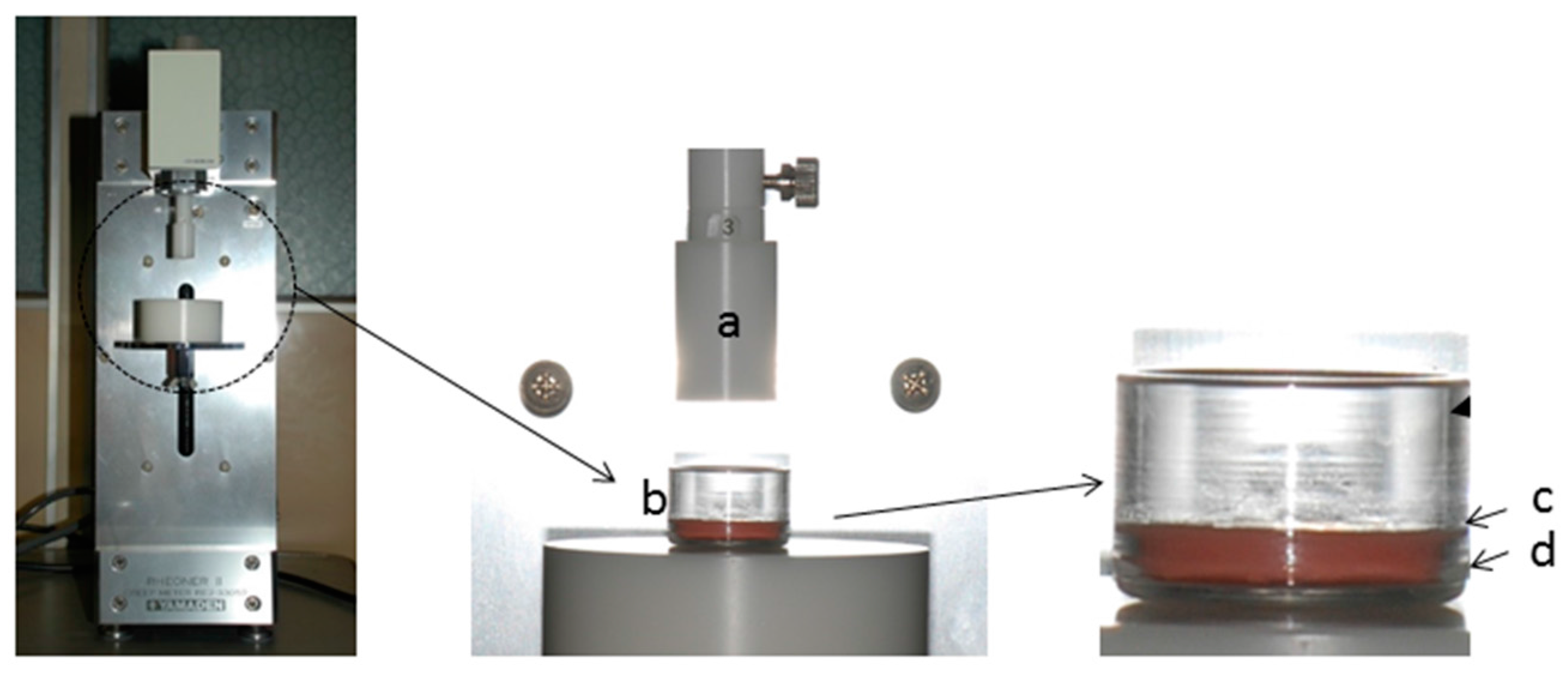
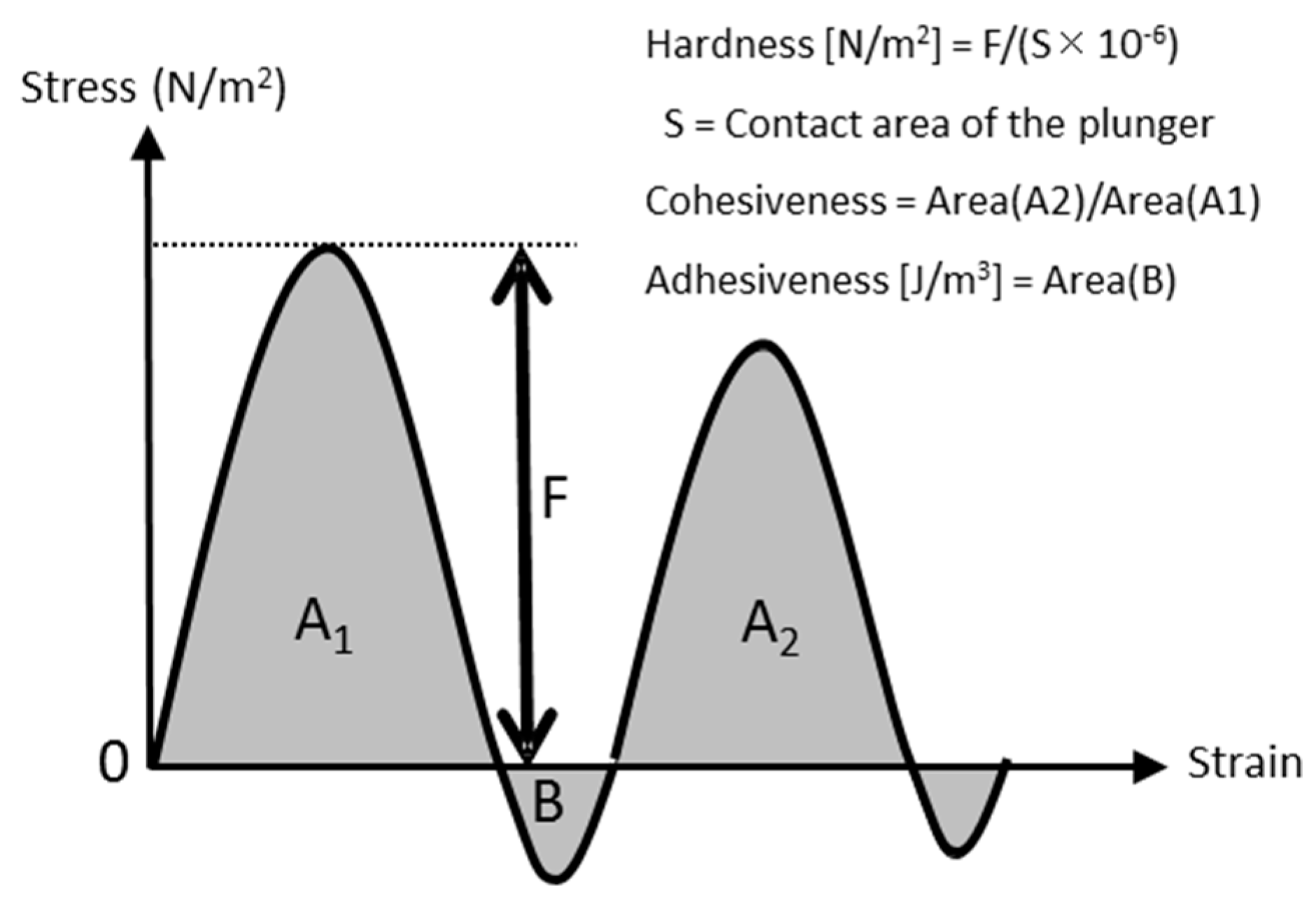
2.2. Measurements of Material Properties
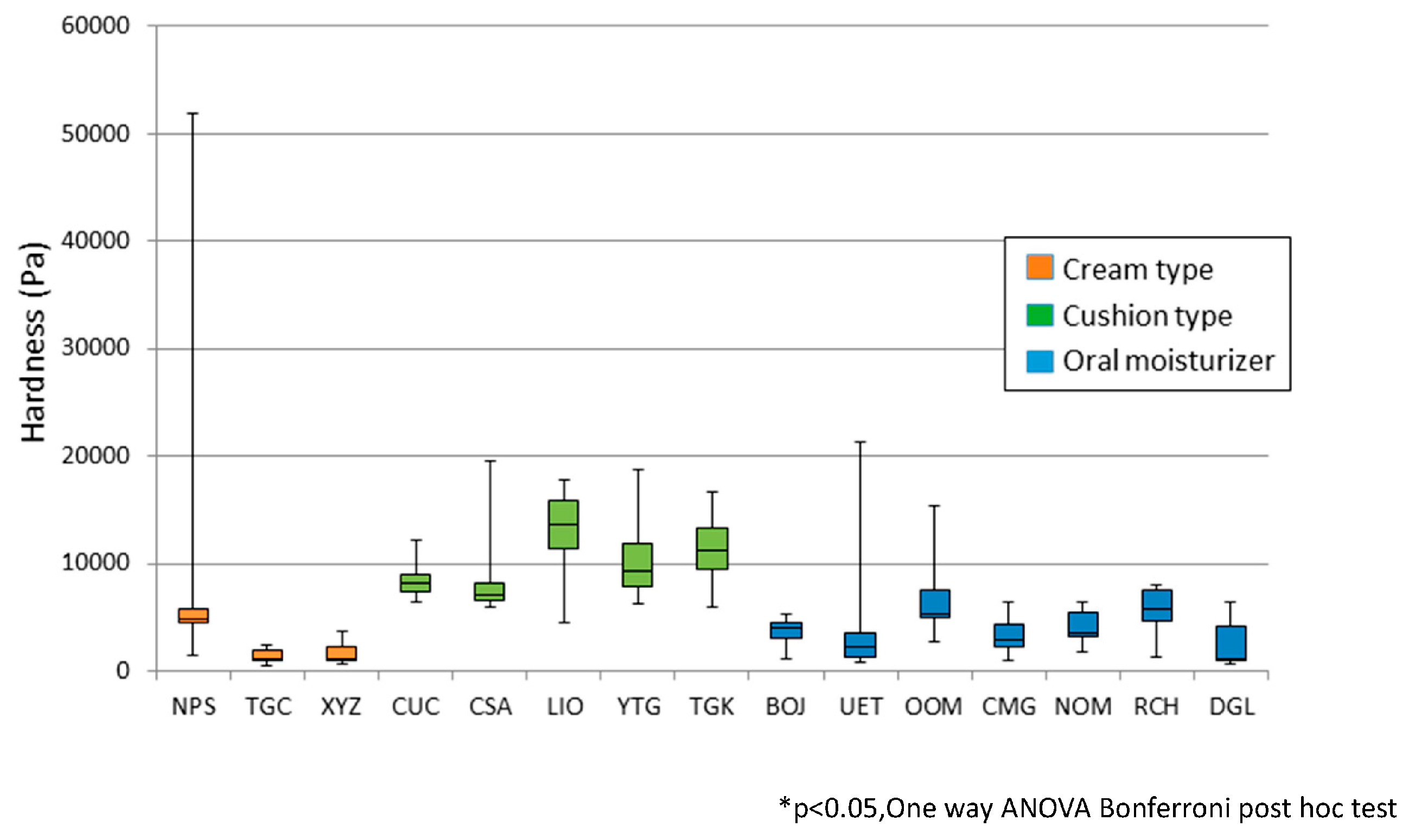
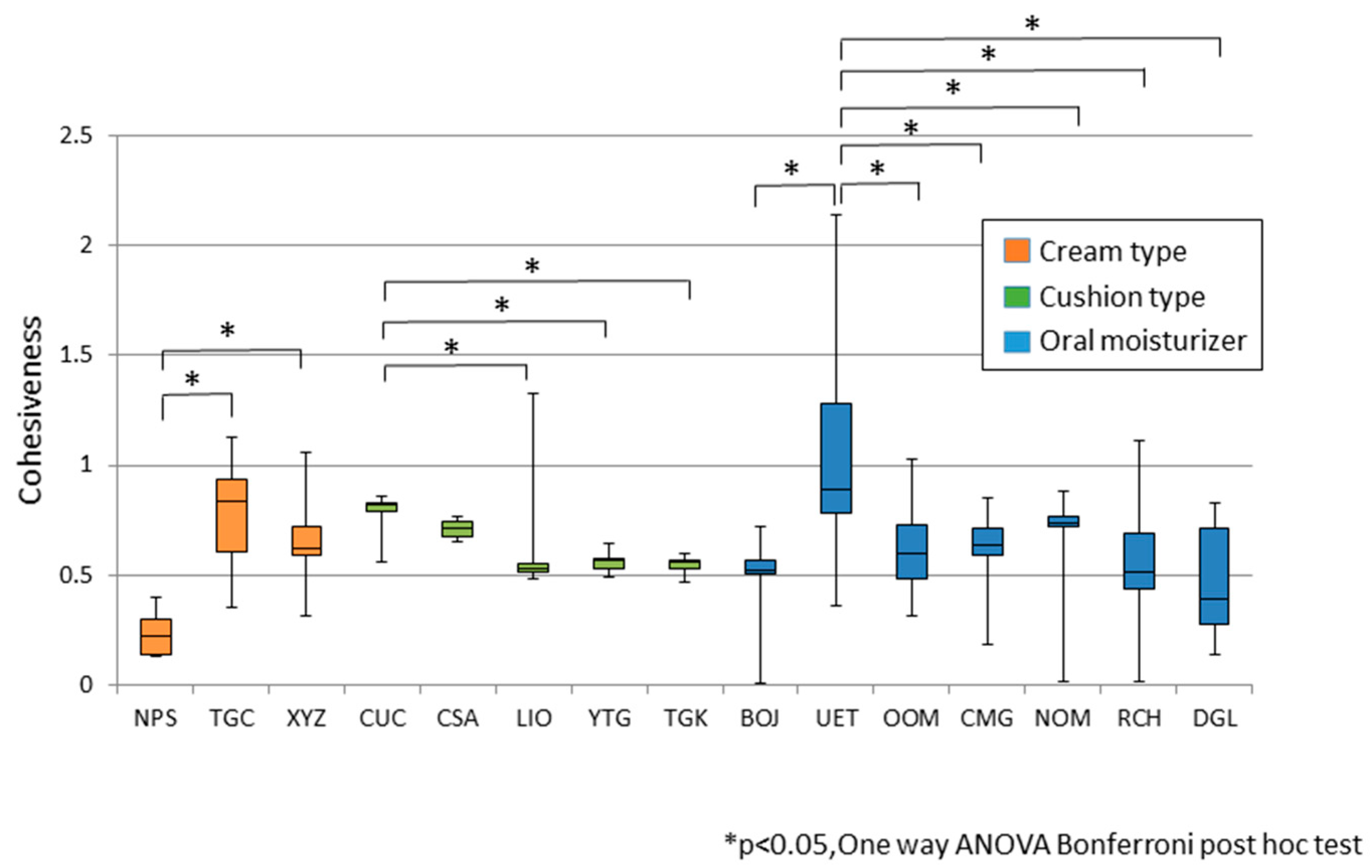
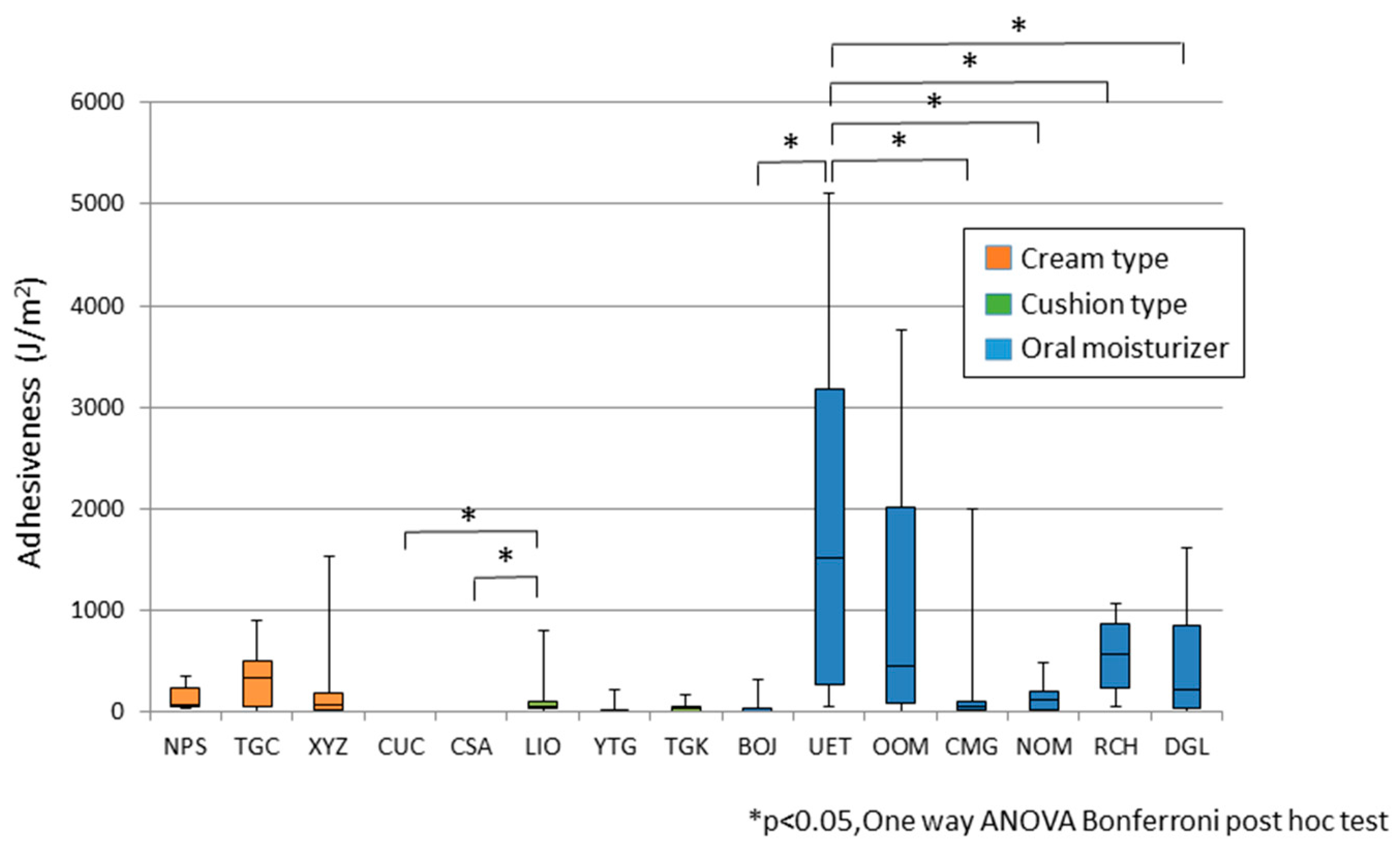
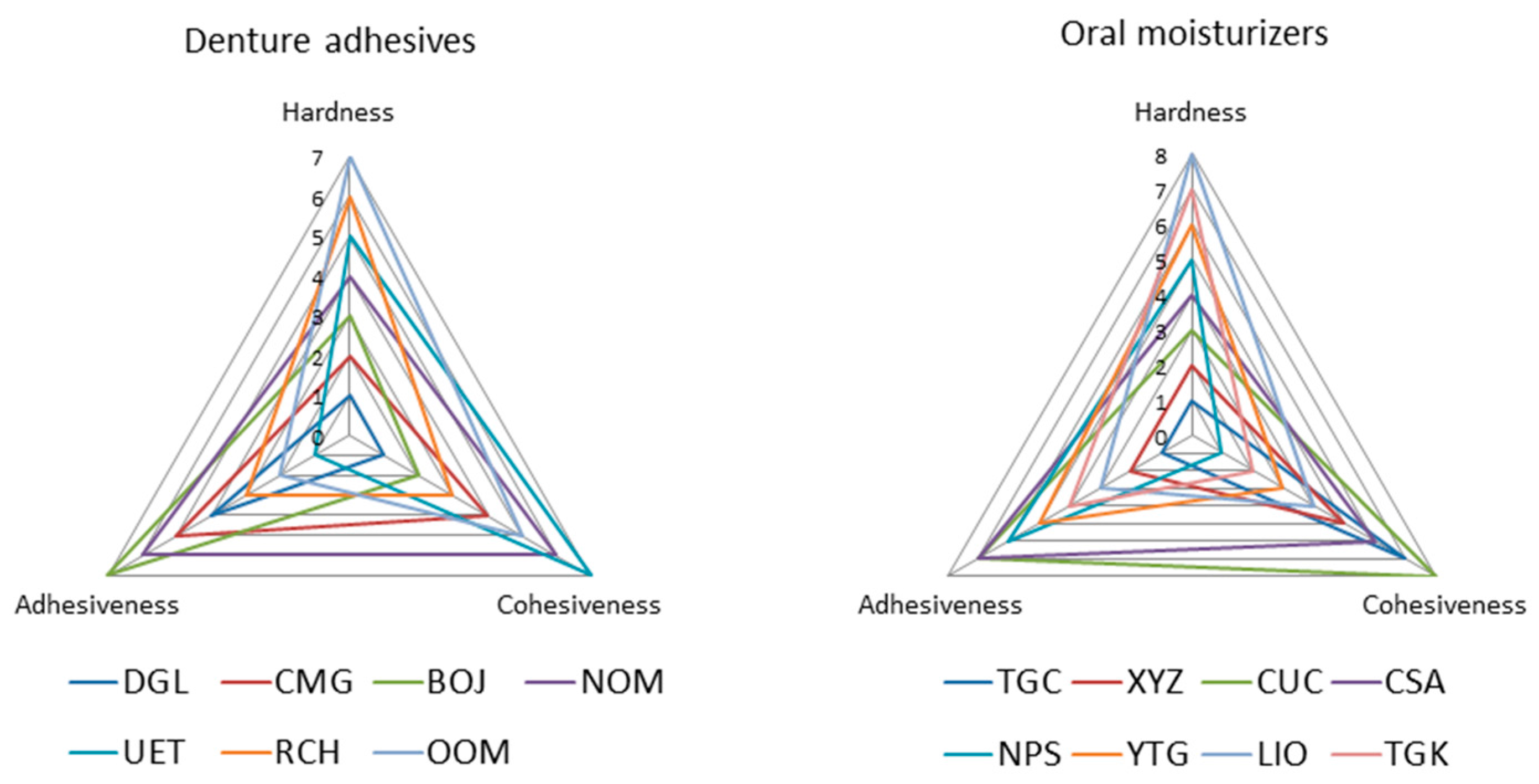
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Diaz-Arnold, A.M.; Marek, C.A. The impact of saliva on patient care: A literature review. J. Prosthet. Dent. 2002, 88, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Morii, K.; Kashiwagi, J.; Nokubi, T.; Ettinger, R.L. Impact of dry mouth on oral symptoms and function in removable denture wearers in Japan. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Amemiya, M.; Morii, K.; Matsuda, K.; Furuya-Yoshinaka, M.; Yoshinaka, M.; Nokubi, T. Association between oral stereognostic ability and masticatory performance in aged complete denture wearers. Int. J. Prosthodont. 2007, 20, 245–250. [Google Scholar] [PubMed]
- Tanasiewicz, M.; Hildebrandt, T.; Obersztyn, I. Xerostomia of Various Etiologies: A Review of the Literature. Adv. Clin. Exp. Med. 2016, 25, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Gil-Montoya, J.A.; Guardia-López, I.; González-Moles, M.A. Evaluation of the clinical efficacy of a mouthwash and oral gel containing the antimicrobial proteins lactoperoxidase, lysozyme and lactoferrin in elderly patients with dry mouth—A pilot study. Gerodontology 2008, 25, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Nishi, Y.; Fujishima, K.; Nishio, M.; Minemoto, Y.; Kanie, T.; Nishimura, M. Impact of Types of Moisturizer and Humidity on the Residual Weight and Viscosity of Liquid and Gel Oral Moisturizers. J. Prosthodont. 2015. [Google Scholar] [CrossRef] [PubMed]
- Papadiochou, S.; Emmanouil, I.; Papadiochos, I. Denture adhesives: A systematic review. J. Prosthet. Dent. 2015, 113, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.R.; Shajahan, P.A.; Mathew, J.; Koruthu, A.; Aravind, P.; Ahammed, M.F. Denture Adhesives in Prosthodontics: An Overview. J. Int. Oral Health 2015, 7 (Suppl. 1), 93–95. [Google Scholar] [PubMed]
- Felton, D.; Cooper, L.; Duqum, I.; Minsley, G.; Guckes, A.; Haug, S.; Meredith, P.; Solie, C.; Avery, D.; Deal Chandler, N.; et al. Evidence-based guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. J. Prosthodont. 2011, 20 (Suppl. 1), S1–S12. [Google Scholar] [CrossRef] [PubMed]
- Felton, D.; Cooper, L.; Duqum, I.; Minsley, G.; Guckes, A.; Haug, S.; Meredith, P.; Solie, C.; Avery, D.; Chandler, N.D.; et al. Evidence-based guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. J. Am. Dent. Assoc. 2011, 142 (Suppl. 1), 1S–20S. [Google Scholar] [CrossRef] [PubMed]
- Bourne, M.C. Food Texture and Viscosity: Concept and Measurement; Academic Press: London, UK, 2002. [Google Scholar]
- Bourne, M.C. Relation between texture and mastication. J. Texture Stud. 2004, 35, 125–143. [Google Scholar] [CrossRef]
- Goto, T.; Nakamich, A.; Watanabe, M.; Nagao, K.; Matsuyama, M.; Ichikawa, T. Influence of food volume per mouthful on chewing and bolus properties. Physiol. Behav. 2015, 141, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Wada, S.; Goto, T.; Fujimoto, K.; Watanabe, M.; Nagao, K.; Ichikawa, T. Changes in food bolus texture during. J. Texture Stud. 2016. [Google Scholar] [CrossRef]
- Ohguri, T.; Kawano, F.; Ichikawa, T.; Matsumoto, N. Influence of occlusal scheme on the pressure distribution under a complete denture. Int. J. Prosthodont. 1999, 12, 353–358. [Google Scholar] [PubMed]
- Emmer, T.J., Jr.; Emmer, T.J., Sr.; Vaidyanathan, J.; Vaidyanathan, T.K. Measurement of submucosal forces transmitted to dental implants. J. Oral Implantol. 1999, 25, 155–160. [Google Scholar] [CrossRef]
- Kano, H.; Kurogi, T.; Shimizu, T.; Nishimura, M.; Murata, H. Viscosity and adhesion strength of cream-type denture adhesives and mouth moisturizers. Dent. Mater. J. 2012, 31, 960–968. [Google Scholar] [CrossRef] [PubMed]
| Commercial Name | Products | Code | |
|---|---|---|---|
| Oral Moisturizers | Biotene Oralbalance jel® | GlaxoSmithKline (Tokyo, Japan) * | BOJ |
| Wet-aid | Kamemizu Chem. Ind (Osaka, Japan)* | UET | |
| OptreozTM oral Moisturizer | 3M Japan (Tokyo, Japan) * | OOM | |
| ConCool Mouth Gel | Weltec (Osaka, Japan) * | CMG | |
| New Oral Moisturizer Ai Gel | Hishika Dental (Mie, Japan) | NOM | |
| Rifre-care® H | EN Otsuka Pharmaceutical (Iwate, Japan) * | RCH | |
| Denture Gel | Kamemizu Chemical Ind (Osaka, Japan) * | DGL | |
| Denture Adhesives | Cream-type | ||
| New Poligrip® Sa | GlaxoSmithKline (Tokyo, Japan) * | NPS | |
| Tough grip® cream | Kobayashi Pharmaceutical (Osaka, Japan) * | TGC | |
| Correct® XYL Cream | Shionogi Healthcare (Osaka, Japan) * | XYZ | |
| Cushion-type | |||
| Cushion Correct® | Shionogi Healthcare (Osaka, Japan) * | CUC | |
| Correct® Soft A | Shionogi Healthcare (Osaka, Japan) | CSA | |
| Liodent | Lion (Tokyo, Japan) * | LIO | |
| Yawaraka Tafugurippu® | Kobayashi Pharmaceutical (Osaka, Japan) * | YTG | |
| Tafugurippu® Kusshon | Kobayashi Pharmaceutical (Osaka,Japan) * | TGK |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujimoto, K.; Minami, N.; Goto, T.; Ishida, Y.; Watanabe, M.; Nagao, K.; Ichikawa, T. Hardness, Cohesiveness, and Adhesiveness of Oral Moisturizers and Denture Adhesives: Selection Criteria for Denture Wearers. Dent. J. 2016, 4, 34. https://doi.org/10.3390/dj4040034
Fujimoto K, Minami N, Goto T, Ishida Y, Watanabe M, Nagao K, Ichikawa T. Hardness, Cohesiveness, and Adhesiveness of Oral Moisturizers and Denture Adhesives: Selection Criteria for Denture Wearers. Dentistry Journal. 2016; 4(4):34. https://doi.org/10.3390/dj4040034
Chicago/Turabian StyleFujimoto, Keiko, Norikazu Minami, Takaharu Goto, Yuichi Ishida, Megumi Watanabe, Kan Nagao, and Tetsuo Ichikawa. 2016. "Hardness, Cohesiveness, and Adhesiveness of Oral Moisturizers and Denture Adhesives: Selection Criteria for Denture Wearers" Dentistry Journal 4, no. 4: 34. https://doi.org/10.3390/dj4040034





