Magnet-Retained Two-Mini-Implant Overdenture: Clinical and Mechanical Consideration
Abstract
:1. Introduction
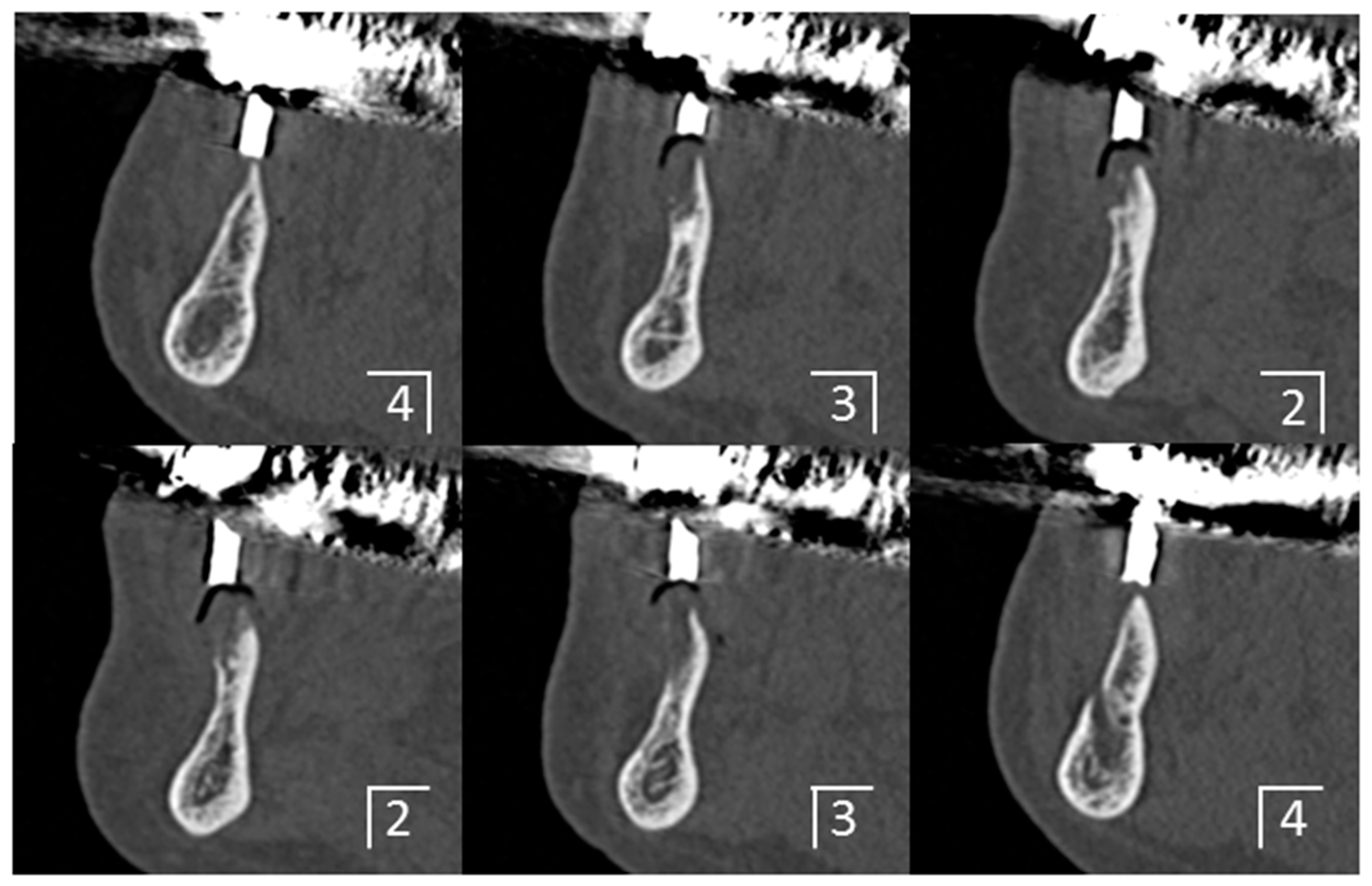
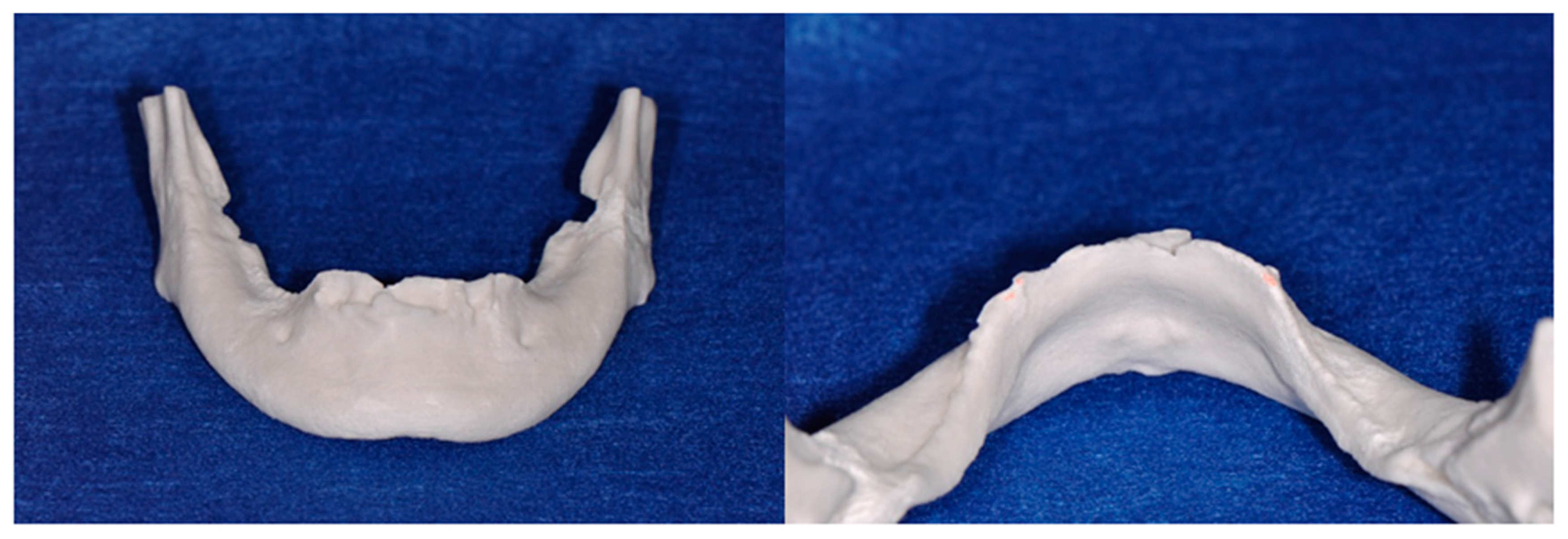
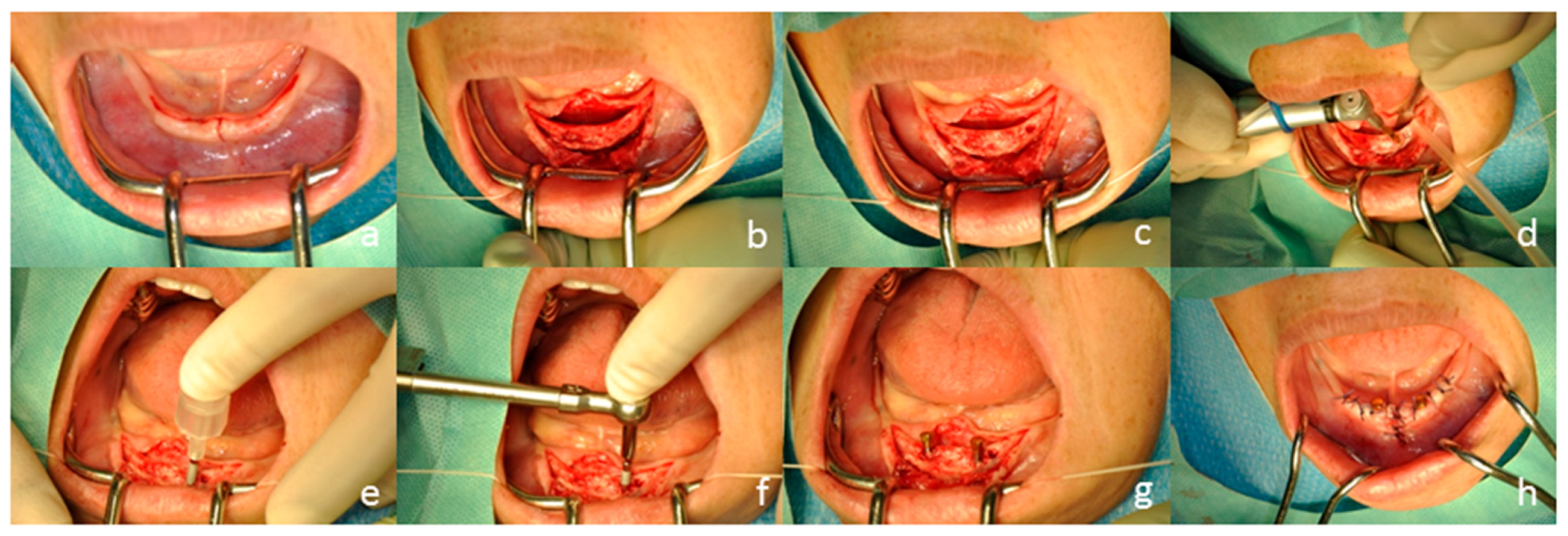
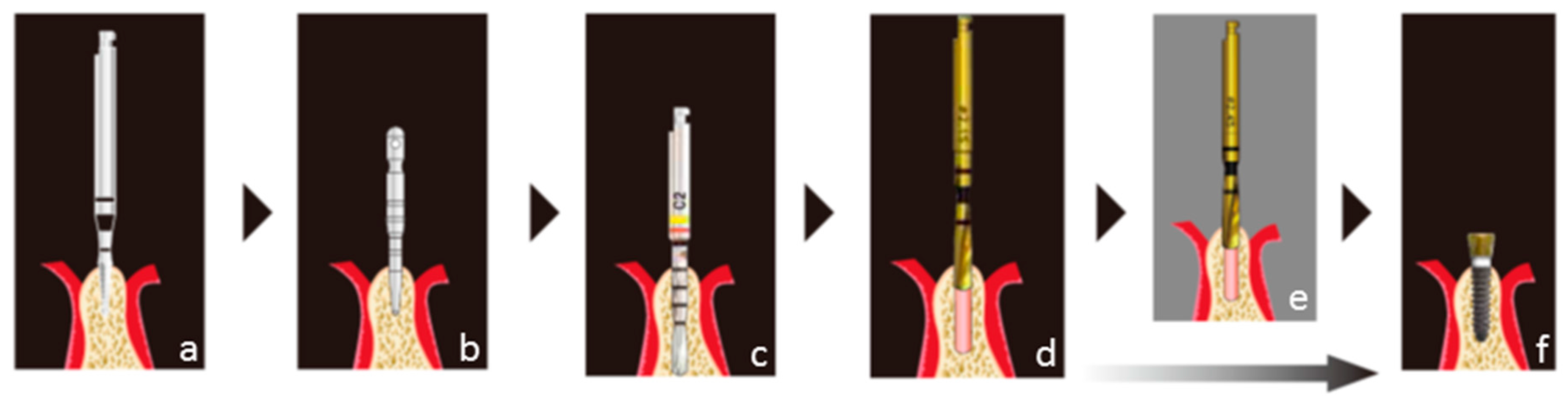
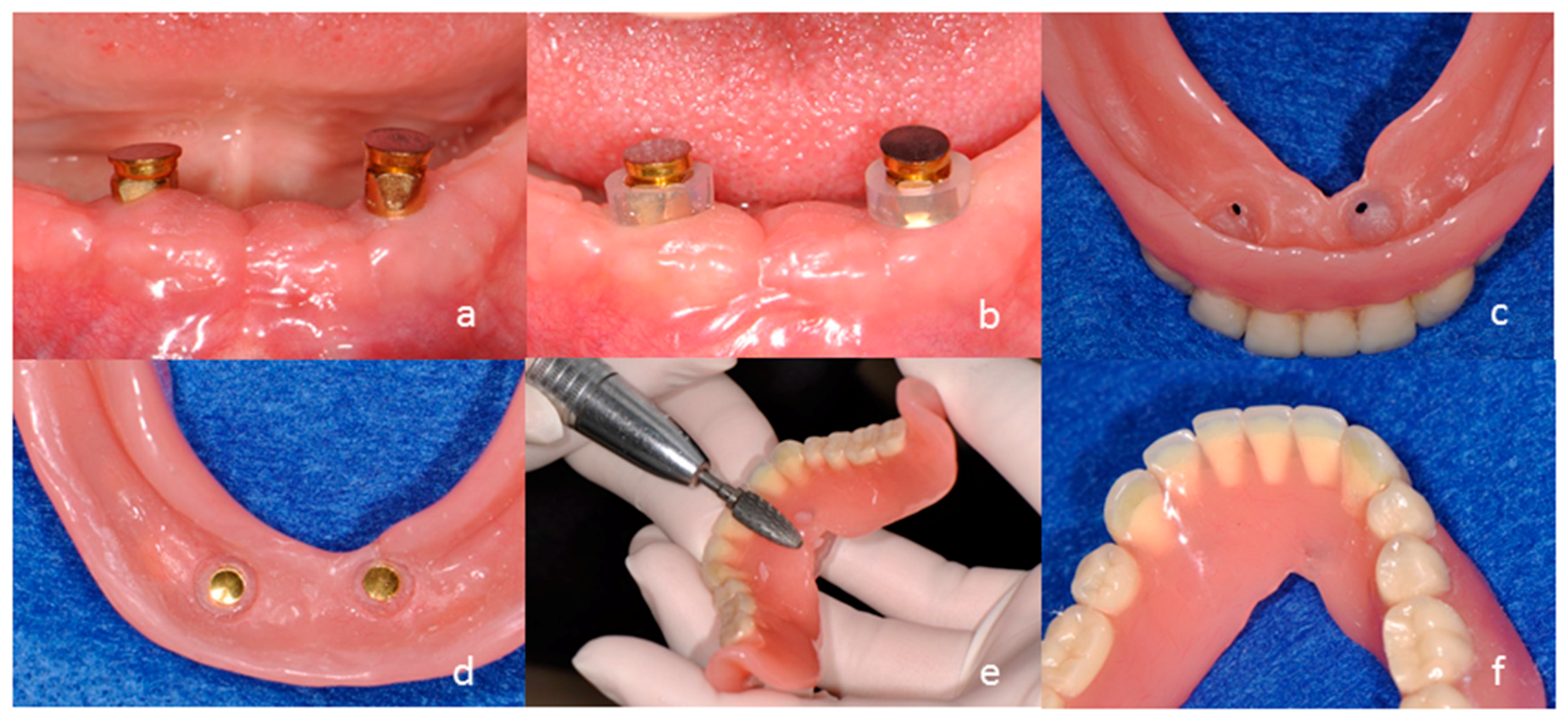
2. Case Presentation
3. Clinical and Mechanical Considerations
Author Contributions
Conflicts of Interest
References
- Vercruyssen, M.; Marcelis, K.; Coucke, W.; Naert, I.; Quirynen, M. Long-term, retrospective evaluation (implant and patient-centred outcome) of the two-implants-supported overdenture in the mandible. Part 1: Survival rate. Clin. Oral Implant. Res. 2010, 21, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Thomason, J.M.; Kelly, S.A.; Bendkowski, A.; Ellis, J.S. Two implant retained overdentures—A review of the literature supporting the McGill and York consensus statements. J. Dent. 2012, 40, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Geckili, O.; Cilingir, A.; Erdogan, O.; Kesoglu, A.C.; Bilmenoglu, C.; Ozdiler, A.; Bilhan, H. The influence of momentary retention forces on patient satisfaction and quality of life of two-implant-retained mandibular overdenture wearers. Int. J. Oral Maxillofac. Implant. 2015, 30, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Assunção, W.G.; Zardo, G.G.; Delben, J.A.; Barão, V.A. Comparing the efficacy of mandibular implant-retained overdentures and conventional dentures among elderly edentulous patients: Satisfaction and quality of life. Gerodontology 2007, 24, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Mundt, T.; Polzer, I.; Samietz, S.; Grabe, H.J.; Messerschmidt, H.; Dören, M.; Schwarz, S.; Kocher, T.; Biffar, R.; Schwahn, C. Socioeconomic indicators and prosthetic replacement of missing teeth in a working-age population: Results of the Study of Health in Pomerania (SHIP). Community Dent. Oral Epidemiol. 2009, 37, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Clavero, J.; Lundgren, S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: Comparison of donor site morbidity and complications. Clin. Implant Dent. Relat. Res. 2003, 5, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, B. Mini-implants: New possibilities in interdisciplinary treatment approaches. Case Rep. Dent. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, E.; Imre, M.; Preoteasa, C.T. A 3-year follow-up study of overdentures retained by mini-dental implants. Int. J. Oral Maxillofac. Implant. 2014, 29, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- De Souza, R.F.; Ribeiro, A.B.; Della Vecchia, M.P.; Costa, L.; Cunha, T.R.; Reis, A.C.; Albuquerque, R.F., Jr. Mini vs. Standard Implants for Mandibular Overdentures: A Randomized Trial. J. Dent. Res. 2015, 94, 1376–1384. [Google Scholar] [CrossRef] [PubMed]
- Griffitts, T.M.; Collins, C.P.; Collins, P.C. Mini dental implants: An adjunct for retention, stability, and comfort for the edentulous patient. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 100, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, T.; Horiuchi, M.; Wigianto, R.; Matsumoto, N. In vitro study of mandibular implant-retained overdentures: The influence of stud attachments on load transfer to the implant and soft tissue. Int. J. Prosthodont. 1996, 9, 394–399. [Google Scholar] [PubMed]
- Andreiotelli, M.; Att, W.; Strub, J.R. Prosthodontic complications with implant overdentures: A systematic literature review. Int. J. Prosthodont. 2010, 23, 195–203. [Google Scholar] [PubMed]
- Naert, I.; Gizani, S.; Vuylsteke, M.; Van Steenberghe, D. A 5-year prospective randomized clinical trial on the influence of splinted and unsplinted oral implants retaining a mandibular overdenture: Prosthetic aspects and patient satisfaction. J. Oral Rehabil. 1999, 26, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Heckmann, S.M.; Winter, W.; Meyer, M.; Weber, H.P.; Wichmann, M.G. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 2: A methodical study using five types of attachment. Clin. Oral Implant. Res. 2001, 12, 640–647. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y. Clinical complications with implants and implant prostheses. J. Prosthet. Dent. 2003, 90, 121–132. [Google Scholar] [CrossRef]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Lund, J.P.; MacEntee, M.; Mericske-Stern, R.; et al. The McGill consensus statement on overdentures. Int. J. Prosthodont. 2002, 15, 413–414. [Google Scholar] [PubMed]
- Thomason, J.M.; Feine, J.; Exley, C.; Moynihan, P.; Müller, F.; Naert, I.; Ellis, J.S.; Barclay, C.; Butterworth, C.; Scott, B.; et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients—The York Consensus Statement. Br. Dent. J. 2009, 207, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Tomasi, C.; Idmyr, B.O.; Wennström, J.L. Patient satisfaction with mini-implant stabilized full dentures. A 1-year prospective study. J. Oral Rehabil. 2013, 40, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Sfeir, E.; Nassif, N.; Moukarzel, C. Use of mini dental implants in ectodermal dysplasia children: Follow-up of three cases. Eur. J. Paediatr. Dent. 2014, 15, 207–212. [Google Scholar] [PubMed]
- Himmlová, L.; Dostálová, T.; Kácovský, A.; Konvicková, S. Influence of implant length and diameter on stress distribution: A finite element analysis. J. Prosthet. Dent. 2004, 91, 20–25. [Google Scholar] [CrossRef] [PubMed]
- MacEntee, M.I.; Walton, J.N.; Glick, N. A clinical trial of patient satisfaction and prosthodontic needs with ball and bar attachments for implant-retained complete overdentures: Three-year results. J. Prosthet. Dent. 2005, 93, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Duran, I.; Yilmaz, B.; Ural, C. A technique for removing implant-retained denture: Direct relining complication. Case Rep. Dent. 2015, 2015, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Jofre, J.; Cendoya, P.; Munoz, P. Effect of splinting mini-implants on marginal bone loss: A biomechanical model and clinical randomized study with mandibular overdentures. Int. J. Oral Maxillofac. Implant. 2010, 25, 1137–1144. [Google Scholar]
- Naert, I.; Koutsikakis, G.; Quirynen, M.; Duyck, J.; van Steenberghe, D.; Jacobs, R. Biologic outcome of implant-supported restorations in the treatment of partial edentulism. Part 2: A longitudinal radiographic study. Clin. Oral Implant. Res. 2002, 13, 390–395. [Google Scholar] [CrossRef]
- Nissan, J.; Ghelfan, O.; Gross, M.; Chaushu, G. Analysis of load transfer and stress distribution by splinted and unsplinted implant-supported fixed cemented restorations. J. Oral Rehabil. 2010, 37, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Baggi, L.; Cappelloni, I.; Di Girolamo, M.; Maceri, F.; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J. Prosthet. Dent. 2008, 100, 422–431. [Google Scholar] [CrossRef] [Green Version]
- Frost, H.M. Bone’s mechanostat: A 2003 update. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 2003, 275, 1081–1101. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A.; Khairallah, A.S. Chewing efficiency and maximum bite force with different attachment systems of implant overdentures: A crossover study. Clin Oral Implant. Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Nagao, K.; Ishida, Y.; Tomotake, Y.; Ichikawa, T. Influence of matrix attachment installation load on movement and resultant forces in implant overdentures. J. Prosthodont. 2015, 24, 156–163. [Google Scholar] [CrossRef] [PubMed]




© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishida, Y.; Kumar, H.S.K.; Goto, T.; Watanabe, M.; Wigianto, R.; Ichikawa, T. Magnet-Retained Two-Mini-Implant Overdenture: Clinical and Mechanical Consideration. Dent. J. 2016, 4, 35. https://doi.org/10.3390/dj4040035
Ishida Y, Kumar HSK, Goto T, Watanabe M, Wigianto R, Ichikawa T. Magnet-Retained Two-Mini-Implant Overdenture: Clinical and Mechanical Consideration. Dentistry Journal. 2016; 4(4):35. https://doi.org/10.3390/dj4040035
Chicago/Turabian StyleIshida, Yuichi, H. S. Kiran Kumar, Takaharu Goto, Megumi Watanabe, Rudi Wigianto, and Tetsuo Ichikawa. 2016. "Magnet-Retained Two-Mini-Implant Overdenture: Clinical and Mechanical Consideration" Dentistry Journal 4, no. 4: 35. https://doi.org/10.3390/dj4040035





