Individual Differences in Responsiveness to Acupuncture: An Exploratory Survey of Practitioner Opinion
Abstract
:1. Introduction
- A
- A survey of UK acupuncture practitioners to find why members of the profession think some patients respond better to acupuncture than others.
- B
- Use of self-report personality scales with around 100 participants who have taken part in acupuncture-related studies conducted at the University of Hertfordshire since 2011, to assess whether there are any meaningful associations between these traits and their electroencephalography (EEG), heart rate variability (HRV) and outcomes data already collected.
- C
- A (blinded) retrospective survey of acupuncture teaching clinic patients who have responded either well or poorly to acupuncture, using a variety of short, established self-report personality questionnaires to determine whether any of the traits assessed have a bearing on outcome.
- D
- A prospective study of patients using a smaller selection of self-report questionnaires (based on Phases A–C above), together with outcome measures such as the Measure Yourself Medical Outcome Profile (MYMOP) and perhaps a multiple measure of mood change similar to those developed and piloted by D.F.M. and other collaborators [29,30].
2. Materials and Methods
2.1. The Survey
2.2. Recruitment
2.3. Analysis
3. Results
3.1. The Respondents
3.2. The Questions
3.2.1. Questions Requiring “Yes” or “No” Responses—An Overview
3.2.2. On Specific Questions Requiring “Yes” or “No” Responses
3.2.3. Respondent Characteristics and Yes/No Responses
Age and Years in Practice
Gender
Main Profession
Professional Association Membership
Style of Practice
Prior Opinion That Patient Characteristics Might Affect Treatment Response
3.2.4. Associations between the 60 Main Questions in the Survey
3.2.5. Agreement between Respondents, Variability and Variance of Responses
3.2.6. Patterns in Survey Completion Assessed from Numbers of “Yes”, “No” and “Don’t know” Answers
3.3. Thematic Analysis of Free-Text Responses
3.3.1. Literal Analysis
3.3.2. Interpretive Analysis
3.3.3. Reflexive Analysis
4. Discussion
5. Conclusions
- 1
- If appropriate, reminders sent out a few weeks before a survey is closed could well increase uptake. Authors of acupuncture surveys should not expect enthusiastic uptake unless their survey is of particular relevance to their pool of potential respondents. In addition, members of smaller professional organisations may be more likely to respond than those of larger acupuncture associations.
- 2
- Practitioner age and gender influence how they view the importance of patient characteristics, as do the practitioner’s main profession and potentially their own ethnicity.
- 3
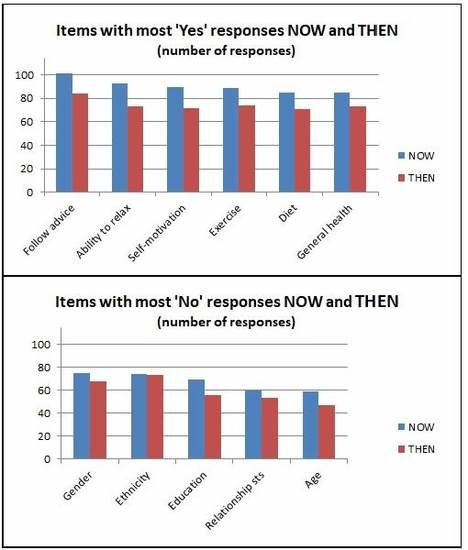
- Attributes most consistently reported to affect treatment outcome were diet, exercise and the ability to relax (Bob Flaws’ “Three frees”), together with general health, self-motivation and a willingness to follow advice.
- 4
- However, a lack of awareness of more complex or difficult psychological and social issues may have skewed the current findings, obscuring the potential importance of some less obvious attributes.
- 5
- Attempts to group characteristics according to item response patterns met with limited success, perhaps relating to the aforementioned skewing.
- 6
- Survey fatigue was observed in terms of numbers of “Yes” and “No” responses, as well as changes in response variability, over the course of completing the survey.
- 7
- Qualitative data may support different and subtler conclusions regarding acupuncturists’ appreciation of factors influencing their practice. A key example here is the varying views on belief and scepticism, which “fall through the net” of the quantitative arm of the study.
Limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| NOW | Gender | Ethnicity | Education |
| Gender | <0.0001 *1 | <0.0001 *2 | |
| Ethnicity | <0.0001 *2 | ||
| Education | |||
| THEN | Gender | Ethnicity | Education |
| Gender | <0.0001 | <0.0001 | |
| Ethnicity | <0.0001 | ||
| Education |
| NOW | Age | General Health |
| Age | 0.001 *3 | |
| General health | ||
| THEN | Age | General Health |
| Age | <0.0001 | |
| General health |
| NOW | Birth/Prenatal | Characteristics | Health | Family Health | Poverty |
| Birth/prenatal | <0.0001 *3 | <0.0001 *2 | <0.0001 *2 | <0.0001 *1 | |
| Characteristics | <0.0001 *3 | <0.0001 *3 | <0.0001 *3 | ||
| Health | <0.0001 *1 | <0.0001 *2 | |||
| Family health | <0.0001 *2 | ||||
| Poverty | |||||
| THEN | Birth/Prenatal | Characteristics | Health | Family Health | Poverty |
| Birth/prenatal | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| Characteristics | <0.0001 | <0.0001 | <0.0001 | ||
| Health | <0.0001 | <0.0001 | |||
| Family health | <0.0001 | ||||
| Poverty |
| NOW | Early Trauma | Later Trauma | Past Invasive Med |
| Early trauma | <0.0001 *1 | 0.023 *4 | |
| Later trauma | 0.045 *4 | ||
| Past invasive med | |||
| THEN | Early Trauma | Later Trauma | Past Invasive Med |
| Early trauma | <0.0001 | <0.0001 | |
| Later trauma | <0.0001 | ||
| Past invasive med |
| NOW | Relationship | Soc Support | Housing | Work | Finances |
| Relationship | <0.0001 *4 | <0.0001 *4 | <0.0001 *4 | <0.0001 *4 | |
| Soc support | <0.0001 *2 | <0.0001 *2 | <0.0001 *2 | ||
| Housing | <0.0001 *2 | <0.0001 *2 | |||
| Work | <0.0001 *1 | ||||
| Finances | |||||
| THEN | Relationship | Soc Support | Housing | Work | Finances |
| Relationship | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| Soc support | <0.0001 | <0.0001 | <0.0001 | ||
| Housing | <0.0001 | <0.0001 | |||
| Work | <0.0001 | ||||
| Finances |
| NOW | Religion | Nature/Technology |
| Religion | <0.0001 *2 | |
| Nature/technology | ||
| THEN | Religion | Nature/Technology |
| Religion | <0.0001 | |
| Nature/technology |
| NOW | Nutrition | Exercise |
| Nutrition | <0.0001 *1 | |
| Exercise | ||
| THEN | Nutrition | Exercise |
| Nutrition | <0.0001 | |
| Exercise |
| NOW | SensStress | Anxiety | RelaxAbil |
| SensStress | <0.0001 *1 | 0.002 *4 | |
| Anxiety | <0.0001 *4 | ||
| RelaxAbil | |||
| THEN | SensStress | Anxiety | RelaxAbil |
| SensStress | <0.0001 | <0.0001 | |
| Anxiety | <0.0001 | ||
| RelaxAbil |
| NOW | CentrSens | Neuroch |
| CentrSens | <0.0001 *1 | |
| Neuroch | ||
| THEN | CentrSens | Neuroch |
| CentrSens | <0.0001 | |
| Neuroch |
| NOW | MUS | Catastr | Hypoch | Psychosis a |
| MUS | <0.0001 *4 | 0.001 *4 | 0.002 *4 | |
| Catastr | <0.0001 *1 | <0.0001 *2 | ||
| Hypoch | <0.0001 *2 | |||
| Psychosis | ||||
| THEN | MUS | Catastr | Hypoch | Psychosis |
| MUS | <0.0001 | <0.0001 | <0.0001 | |
| Catastr | <0.0001 | <0.0001 | ||
| Hypoch | <0.0001 | |||
| Psychosis |
| NOW | Attachment | Addiction | Doctor Shopping | Gender Issues |
| Attachment | 0.007 *3 | <0.0001 *3 | <0.0001 *5 | |
| Addiction | 0.007 *1 | 0.001 *5 | ||
| Doctor shopping | 0.007 *5 | |||
| Gender issues | ||||
| THEN | Attachment | Addiction | Doctor shopping | Gender issues |
| Attachment | <0.0001 | <0.0001 | <0.0001 | |
| Addiction | <0.0001 | <0.0001 | ||
| Doctor shopping | <0.0001 | |||
| Gender issues |
| NOW | LifeSatis | Incontrol | S/Esteem | S/Efficacy | Resilience | Optim | Valency | S/Regul |
| LifeSatis | <0.0001 *1 | <0.0001 *1 | <0.0001 *5 | <0.0001 *2 | <0.0001 *4 | <0.0001 *4 | <0.0001 *5 | |
| InControl | <0.0001 *1 | <0.0001 *5 | <0.0001 *2 | <0.0001 *4 | <0.0001 *4 | <0.0001 *5 | ||
| S/Esteem | <0.0001 *5 | <0.0001 *2 | <0.0001 *4 | <0.0001 *4 | <0.0001 *5 | |||
| S/Efficacy | <0.0001 *5 | <0.0001 *5 | <0.0001 *5 | <0.0001 *1 | ||||
| Resilience | <0.0001 *4 | <0.0001 *4 | <0.0001 *5 | |||||
| Optim | <0.0001 *1 | <0.0001 *5 | ||||||
| Valency | <0.0001 *5 | |||||||
| S/Regul | ||||||||
| THEN | LifeSatis | InControl | S/ESteem | S/Efficacy | Resilience | Optim | Valency | S/Regul |
| LifeSatis | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| InControl | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| S/ESteem | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
| S/Efficacy | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||||
| Resilience | <0.0001 | <0.0001 | <0.0001 | |||||
| Optim | <0.0001 | <0.0001 | ||||||
| Valency | <0.0001 | |||||||
| S/Regul |
| NOW | Defensive | Open | Suggestible | Sceptical | Trusting | Placebo |
| Defensive | <0.0001 *5 | <0.0001 *1 | <0.0001 *6 | <0.0001 *4 | 0.001 *2 | |
| Open | <0.0001 *5 | 0.005 *5 | <0.0001 *3 | 0.003 *5 | ||
| Suggestible | <0.0001 *6 | <0.0001 *4 | <0.0001 *4 | |||
| Sceptical | <0.001 *4 | <0.001 *5 | ||||
| Trusting | 0.001 *4 | |||||
| Placebo | ||||||
| THEN | Defensive | Open | Suggestible | Sceptical | Trusting | Placebo |
| Defensive | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| Open | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| Suggestible | <0.0001 | <0.0001 | <0.0001 | |||
| Sceptical | <0.0001 | <0.0001 | ||||
| Trusting | <0.0001 | |||||
| Placebo |
| NOW | Depressive | Unstable | Extrav/Introv |
| Depressive | <0.0001 *2 | <0.0001 *5 | |
| Unstable | <0.0001 *5 | ||
| Extrav/Introv a | |||
| THEN | Depressive | Unstable | Extrav/Introv |
| Depressive | <0.0001 | <0.0001 | |
| Unstable | <0.0001 | ||
| Extrav/Introv a |
| NOW | Self-Motivated | Follows Advice | Commitment |
| Self-motivated | <0.0001 *1 | <0.001 *3 | |
| Follows advice | <0.0001 *3 | ||
| Commitment | |||
| THEN | Self-Motivated | Follows Advice | Commitment |
| Self-motivated | <0.0001 | <0.0001 | |
| Follows advice | <0.0001 | ||
| Commitment |
| NOW | Bodily Aware | Emotionally Aware | Alexithymic |
| Bodily aware | <0.0001 *1 | <0.0001 *5 | |
| Emotionally aware | <0.0001 *5 | ||
| Alexithymic | |||
| THEN | Bodily Aware | Emotionally Aware | Alexithymic |
| Bodily aware | <0.0001 | <0.0001 | |
| Emotionally aware | <0.0001 | ||
| Alexithymic |
| NOW | Qi Strong/Weak | TCM/5E Diagnosis |
|---|---|---|
| Qi strong/weak | <0.0001 | |
| TCM/5E diagnosis |
| NOW | Religion | Nature/Tech | Health | Neurochem | Central Sens | Nutrition | Exercise | Ability to Relax |
|---|---|---|---|---|---|---|---|---|
| Religion | <0.0001 | <0.0001 | 0.005 | 0.006 | n.s. | n.s. | n.s. | |
| Nature/Tech | <0.001 | 0.006 | <0.001 | 0.034 | n.s. | 0.010 | ||
| Health | <0.001 | 0.042 | <0.0001 | <0.0001 | n.s. | |||
| Neurochem | <0.0001 | n.s. | n.s. | n.s. | ||||
| Central Sens | n.s. | n.s. | 0.039 | |||||
| Nutrition | <0.0001 | 0.001 | ||||||
| Exercise | 0.014 | |||||||
| Ability to Relax |
| Grouping | NOW | THEN | ||||||
|---|---|---|---|---|---|---|---|---|
| Kappa | Median SE | npCV Yes | npCV No | Kappa | Median SE | npCV Yes | npCV No | |
| 1 | 0.22 | 1.29 | 18.97 | 4.05 | 0.14 | 1.36 | 32.14 | 12.50 |
| 2 | 0.29 | 1.13 | 27.41 | 51.28 | 0.14 | 1.37 | 21.31 | 54.10 |
| 3 | 0.01 | 1.57 | 45.45 | 7.89 | 0.02 | 1.54 | 69.23 | 29.27 |
| 4 | 0.13 | 1.40 | 3.03 | 23.08 | 0.04 | 1.52 | 4.72 | 23.08 |
| 5 | 0.09 | 1.43 | 40.38 | 24.00 | 0.02 | 1.55 | 41.45 | 15.91 |
| 6 | 0.03 | 1.54 | 6.38 | 2.38 | 0.00 | 1.58 | 11.11 | 13.16 |
| 7 | 0.43 | 1.00 | 1.71 | 8.57 | 0.21 | 1.30 | 1.37 | 5.56 |
| 8 | 0.33 | 1.22 | 14.38 | 32.14 | 0.14 | 1.41 | 13.11 | 16.00 |
| 9 | 0.11 | 1.40 | 9.91 | 10.34 | 0.01 | 1.55 | 8.43 | 9.09 |
| 10 | 0.15 | 1.37 | 14.18 | 21.79 | 0.04 | 1.51 | 10.85 | 38.64 |
| 11 | 0.06 | 1.46 | 42.38 | 41.94 | 0.03 | 1.52 | 59.15 | 47.83 |
| 12 | 0.14 | 1.38 | 14.45 | 14.29 | 0.03 | 1.54 | 12.87 | 19.40 |
| 13 | 0.17 | 1.43 | 28.75 | 32.35 | 0.07 | 1.51 | 4.85 | 25.00 |
| 14 | 0.15 | 1.31 | 30.28 | 31.03 | 0.06 | 1.47 | 28.33 | 26.79 |
| 15 | 0.52 | 0.91 | 8.79 | 36.67 | 0.26 | 1.29 | 9.59 | 32.14 |
| 16 | 0.22 | 1.30 | 35.71 | 25.86 | 0.09 | 1.50 | 37.27 | 14.00 |
| 17 | 0.07 | 1.48 | 30.69 | 4.92 | 0.02 | 1.54 | 25.00 | 16.13 |
| Grouping | Included | Not Included | % Included |
|---|---|---|---|
| 1 | 3 | 0 | 100 |
| 2 | 2 | 0 | 100 |
| 3 | 3 | 2 | 60 |
| 4 | 0 | 3 | 0 |
| 5 | 1 | 4 | 20 |
| 6 | 0 | 2 | 0 |
| 7 | 2 | 0 | 100 |
| 8 | 1 | 2 | 33 |
| 9 | 1 | 1 | 50 |
| 10 | 1 | 3 | 25 |
| 11 | 1 | 3 | 25 |
| 12 | 1 | 7 | 12.5 |
| 13 | 2 | 4 | 33 |
| 14 | 1 | 2 | 33 |
| 15 | 3 | 0 | 100 |
| 16 | 1 | 2 | 33 |
| 17 | 1 | 1 | 50 |
| Shannon Entropy (SE) | Free-Marginal Kappa | ||||
|---|---|---|---|---|---|
| NOW | THEN | NOW | THEN | ||
| SE Q3 | Birth/prenatal Char when young a Child poverty a Housing Attachment style Extravert/introvert | Religious beliefs Attitude to nature/t Self-efficacy Attachment style Self-regulation TCM diagnosis | κ Q1 | Birth/prenatal Character when young a Child poverty a Housing Attachment style TCM diagnosis | Family health young Religious beliefs Attitude to nature/t Self-efficacy Self-regulation TCM diagnosis |
| SE Q1 | General health b,d Diet b,d Exercise b,d Ability to relax b,d Self-motived b,d Will follow advice b,d | Ethnicity c General health b Exercise b Ability to relax b Self-motivated b Will follow advice b | κ Q3 | Diet b,d Exercise b,d Ability to relax b,d Self-motivated b,d Openness b,d Will follow advice b,d | Ethnicity c General health b Exercise b Self-motivated b Will follow advice b Commitment c |

References
- Baldry, P. Superficial versus deep dry needling. Acupunct. Med. 2002, 20, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.; Colaiaco, B.; Motala, A.; Shanman, R.M.; Sorbero, M.E.; Hempel, S. Needle Acupuncture for Posttraumatic Stress Disorder (PTSD): A Systematic Review; RAND Corporation: Santa Monica, CA, USA, 2017. [Google Scholar]
- Paterson, C.; Britten, N. The patient’s experience of holistic care: Insights from acupuncture research. Chronic Illn. 2008, 4, 264–277. [Google Scholar] [CrossRef] [PubMed]
- McPhail, P.; Sandhu, H.; Dale, J.; Stewart-Brown, S. Acupuncture in hospice settings: A qualitative exploration of patients’ experiences. Eur. J. Cancer Care 2018, 27. [Google Scholar] [CrossRef] [PubMed]
- White, P.; Bishop, F.L.; Prescott, P.; Scott, C.; Little, P.; Lewith, G. Practice, practitioner, or placebo? A multifactorial, mixed-methods randomized controlled trial of acupuncture. Pain 2012, 153, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Wojnarowska, F. Acupuncture for vulvodynia. J. R. Soc. Med. 1999, 92, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.J.; Park, J.W.; Leem, J.; Kaptchuk, T.J.; Napadow, V.; Kuo, B.; Gerber, J.; Dimisko, L.; Yeo, I.; Lee, J.; et al. Influence of the patient-practitioner interaction context on acupuncture outcomes in functional dyspepsia: Study protocol for a multicenter randomized controlled trial. BMC Complement. Altern. Med. 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Elliot, B.; Hopton, A.; Lansdown, H.; Birch, S.; Hewitt, C. Lifestyle advice and self-care integral to acupuncture treatment for patients with chronic neck pain: Secondary analysis of outcomes within a randomized controlled trial. J. Altern. Complement. Med. 2017, 23, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Karst, M.; Schneidewind, D.; Scheinichen, D.; Juettner, B.; Bernateck, M.; Molsberger, A.; Parlesak, A.; Passie, T.; Hoy, L.; Fink, M. Acupuncture induces a pro-inflammatory immune response intensified by a conditioning-expectation effect. Forsch. Komplementmed. 2010, 17, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Wang, Z.; Leiser, J.; Minicucci, D.; Edwards, R.; Kirsch, I.; Wasan, A.D.; Lang, C.; Gerber, J.; Yu, S.; et al. Enhancing treatment of osteoarthritis knee pain by boosting expectancy: A functional neuroimaging study. Neuroimage Clin. 2018, 18, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Mayor, D.F.; McClure, L.S.; McClure, J.H.C. Nonspecific feelings expected and experienced during or immediately after electroacupuncture: A pilot study in a teaching situation. Medicines 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Mann, F. Reinventing Acupuncture: A New Concept of Ancient Medicine, 2nd ed.; Butterworth-Heinemann: Oxford, UK, 2000; ISBN 9780702038280. [Google Scholar]
- Campbell, A. The limbic system and emotion in relation to acupuncture. Acupunct. Med. 1999, 17, 124–130. [Google Scholar] [CrossRef]
- Johnson, M.I.; Ashton, C.H.; Thompson, J.W. The consistency of pulse frequencies and pulse patterns of transcutaneous nerve stimulation (TENS) used by chronic pain patients. Pain 1991, 44, 231–234. [Google Scholar] [CrossRef]
- Campbell, A. Acupuncture: Where to place the needles and for how long. Acupunct. Med. 1999, 17, 113–117. [Google Scholar] [CrossRef]
- Alborzi, A.; Hashempour, T.; Moayedi, J.; Musavi, Z.; Pouladfar, G.; Merat, S. Role of serum level and genetic variation of IL-28B in interferon responsiveness and advanced liver disease in chronic hepatitis C patients. Med. Microbiol. Immunol. 2017, 206, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Wang, Y. Viral and host factors associated with outcomes of hepatitis C virus infection (Review). Mol. Med. Rep. 2017, 15, 2909–2924. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.T.; Loscalzo, J.; Kaptchuk, T.J. Genetics and the placebo effect: The placebome. Trends Mol. Med. 2015, 21, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.S.; Hall, K.T.; Giulianini, F.; Passow, D.; Kaptchuk, T.J.; Loscalzo, J. Network analysis of the genomic basis of the placebo effect. JCI Insight 2017, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.J.; Kim, S.T.; Yoon, D.H.; Jin, S.H.; Lee, S.J.; Lee, H.J.; Lim, S. The association between the DRD2 TaqI A polymorphism and smoking cessation in response to acupuncture in Koreans. J. Altern. Complement. Med. 2005, 11, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.L.; Sun, J.H.; Liu, L.Y.; Fu, H.Y.; Jiao, D.Y.; Shu, Y.Y.; Chen, D.; Liu, C.Y.; Zhan, D.W.; Zhang, W. A feasibility analysis on individualized acupuncture treatment of irritable bowel syndrome under help of genetic polymorphism technique. Zhen Ci Yan Jiu 2014, 39, 252–255. [Google Scholar] [PubMed]
- Yang, X.; Gong, J.; Jin, L.; Liu, L.; Sun, J.; Qin, W. Effect of catechol-O-methyltransferase Val158Met polymorphism on resting-state brain default mode network after acupuncture stimulation. Brain Imaging Behav. 2017, 12, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Magarelli, P.; Cridennda, D. Acupuncture & IVF poor responders: A cure? Fertil. Steril. 2004, 81. [Google Scholar] [CrossRef]
- Jo, J.; Lee, Y.J.; Lee, H. Acupuncture for polycystic ovarian syndrome: A systematic review and meta-analysis. Medicine 2017, 96. [Google Scholar] [CrossRef] [PubMed]
- Han, J.S. The Neurochemical Basis of Pain Relief by Acupuncture. A Collection of Papers 1973–1987; Beijing Medical University: Beijing, China, 1987. [Google Scholar]
- Han, J.S. The Neurochemical Basis of Pain Relief by Acupuncture; Hubei Science and Technology Press: Xianning, China, 1998; Volume 2, ISBN 9787535221995. [Google Scholar]
- Kelley, J.M.; Lembo, A.J.; Ablon, J.S.; Villanueva, J.J.; Conboy, L.A.; Levy, R.; Marci, C.D.; Kerr, C.E.; Kirsch, I.; Jacobson, E.E.; et al. Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosom. Med. 2009, 71, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Sochos, A.; Bennett, A. Psychological distress, physical symptoms, and the role of attachment Style in acupuncture. Altern. Ther. Health Med. 2016, 22, 8–16. [Google Scholar] [PubMed]
- Mayor, D.; Steffert, T. Measuring mood—Relative sensitivity of numerical rating and Likert scales in the context of teaching electroacupuncture. Initial findings and the influence of response style on results. In Proceedings of the 18th ARRC International Acupuncture Research Symposium, London, UK, 19 March 2016. [Google Scholar] [CrossRef]
- Mayor, D.; Steffert, T. Personality and treatment response to electroacupuncture. A new measure of mood change and further analysis of questionnaire response styles. In Proceedings of the 20th ARRC International Acupuncture Research Symposium, London, UK, 17 March 2018. [Google Scholar] [CrossRef]
- Steffert, T.; Mayor, D. Mood changes in response to electroacupuncturetreatment in a classroom situation. Personality type, emotional intelligence and prior acupuncture experience, with an exploration of Shannon entropy, response style and graphology variables. In Proceedings of the 19th ARRC International Acupuncture Research Symposium, London, UK, 25 March 2017. [Google Scholar] [CrossRef]
- Mayor, D.F. The teaching of electroacupuncture in North America: An informal survey. Clin. Acupunt. Orient. Med. 2001, 2, 116–128. [Google Scholar] [CrossRef]
- Mayor, D.; Bovey, M. An international survey on the current use of electroacupuncture. Acupunct. Med. 2017, 35, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6. [Google Scholar] [CrossRef] [PubMed]
- Randolph, J.J. Free-Marginal Multi-Rater kappa: An Alternative to Fleiss’ Fixed-Marginal Multi-Rater Kappa. Ph.D. Thesis, University of Joensuu, Joensuu, Finland, 2005. [Google Scholar]
- Randolph, J.J. Online Kappa Calculator. Available online: http://justus.randolph.name/kappa (accessed on 10 May 2018).
- Fleiss, J.L.; Levin, B.; Paik, M.C. Statistical Methods for Rates and Proportions, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2004; ISBN 9780471526292. [Google Scholar]
- Shannon, C.E.; Weaver, W. The Mathematical Theory of Communication; University of Illinois Press: Chicago, IL, USA, 1949; ISBN 9780252725487. [Google Scholar]
- Silverman, D. Interpreting Qualitative Data, 5th ed.; Sage: London, UK, 2015; ISBN 9781446295434. [Google Scholar]
- Peräkylä, A.; Ruusuvuori, J. Analyzing talk and text. In The Sage Handbook of Qualitative Research, 5th ed.; Denzin, N.K., Lincoln, Y.S., Eds.; Sage: London, UK, 2017; pp. 669–690. ISBN 9781483349800. [Google Scholar]
- Croke, S. The Need for Novel Methodologies and Introduction to Theatricality; Research Council for Complementary Medicine (CAMSTRAND): Manchester, UK, Unpublished Conference Paper; 2018. [Google Scholar]
- Mason, J. Qualitative Researching, 3rd ed.; Sage: London, UK, 2018; ISBN 9781473912182. [Google Scholar]
- Saldaña, J. The Coding Manual for Qualitative Researchers, 3rd ed.; Sage: London, UK, 2015; ISBN 9781473902497. [Google Scholar]
- O’Reilly-Shah, V.N. Factors influencing healthcare provider respondent fatigue answering a globally-administered in-app survey. PeerJ 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Fisher, P.; Van Haselen, R.; Hardy, K.; Berkovitz, S.; McCarney, R. Effectiveness gaps: A new concept for evaluating health service and research needs applied to complementary and alternative medicine. J. Altern. Complement. Med. 2004, 10, 627–632. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.; Janz, S. The Acupuncture Evidence Project: A Comparative Literature Review, rev ed.; Brisbane: Australian Acupuncture and Chinese Medicine Association: Brisbane, Australia, 2017. Available online: https://www.acupuncture.org.au/wp-content/uploads/2017/11/28-NOV-The-Acupuncture-Evidence-Project_Mcdonald-and-Janz_-REISSUED_28_Nov.pdf (accessed on 2 July 2018).
- Wenham, A.; Atkin, K.; Woodman, J.; Ballard, K.; MacPherson, H. Self-efficacy and embodiment associated with Alexander Technique lessons or with acupuncture sessions: A longitudinal qualitative sub-study within the ATLAS trial. Complement. Ther. Clin. Pract. 2018, 31, 308–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, A. Hunting the Snark: The quest for the perfect acupuncture placebo. Acupunct. Med. 1991, 9, 83–84. [Google Scholar] [CrossRef]
- Birch, S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J. Altern. Complement. Med. 2006, 12, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Itoh, K.; Kitakoji, H. Acupuncture for chronic pain in Japan: A review. Evid. Based Complement. Alternat. Med. 2007, 4, 431–438. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Tilbrook, H.; Bland, J.M.; Bloor, K.; Brabyn, S.; Cox, H.; Kang’ombe, A.R.; Man, M.-S.; Stuardi, T.; Torgerson, D.; et al. Acupuncture for irritable bowel syndrome: Primary care based pragmatic randomised controlled trial. BMC Gastroenterol. 2012, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacPherson, H.; Richmond, S.; Bland, M.; Brealey, S.; Gabe, R.; Hopton, A.; Keding, A.; Lansdown, H.; Perren, S.; Sculpher, M.; et al. Acupuncture and counselling for depression in primary care: A randomised controlled trial. PLoS Med. 2013, 10. [Google Scholar] [CrossRef] [PubMed]
- Paterson, C.; Britten, N. Acupuncture as a complex intervention: A holistic model. J. Altern. Complement. Med. 2004, 10, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Linde, K.; Niemann, K.; Schneider, A.; Meissner, K. How large are the nonspecific effects of acupuncture? A meta-analysis of randomised controlled trials. BMC Med. 2010, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Robinson, N.; London South Bank University. Personal communication, 2018.
- Longhurst, J. Acupuncture’s cardiovascular actions: A mechanistic perspective. Med. Acupunct. 2013, 25, 101–113. [Google Scholar] [CrossRef]
- Villas-Boas, J.D.; Dias, D.P.; Trigo, P.I.; Almeida, N.A.; de Almeida, F.Q.; de Medeiros, M.A. Acupuncture affects autonomic and endocrine but not behavioural responses induced by startle in horses. Evid. Based Complement. Alternat. Med. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Uchida, C.; Waki, H.; Minakawa, Y.; Tamai, H.; Hisajima, T.; Imai, K. Evaluation of autonomic nervous system function using heart rate variability analysis during transient heart rate reduction caused by acupuncture. Med. Acupunct. 2018, 30, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Barlow, T. Acupuncture in the Treatment of Children, 3rd ed.; Eastland Press: Seattle, WA, USA, 1999; ISBN 9780939616305. [Google Scholar]
- Loo, M. Pediatric Acupuncture; Churchill Livingstone: Edinburgh, UK, 2002; ISBN 9780443070327. [Google Scholar]
- Maciocia, G. The Foundations of Chinese Medicine. A comprehensive Test for Acupuncturists and Herbalists; Churchill Livingstone: Edinburgh, UK, 1989; ISBN 9780443039805. [Google Scholar]
- Franglen, N. The Handbook of Five Element Practice, rev ed.; Singing Dragon: London, UK, 2014; ISBN 9781848191884. [Google Scholar]
- Marmot, M. Status Syndrome: How Your Place on the Social Gradient Directly Affects Your Health; Bloomsbury: London, UK, 2015; ISBN 9781408872680. [Google Scholar]
- Náfrádi, L.; Nakamoto, K.; Schulz, P.J. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Pashang, S.; Khanlou, N.; Clarke, J. Today’s Youth and Mental Health: Hope, Power, and Resilience; Springer: Cham, Switzerland, 2018; ISBN 9783319648361. [Google Scholar]
- Meade, R.D.; Barnard, W.A. Conformity and Anticonformity among Americans and Chinese. J. Soc. Psychol. 2010, 89, 15–24. [Google Scholar] [CrossRef]
- Glynn, L.M.; Howland, M.A.; Sandman, C.A.; Davis, E.P.; Phelan, M.; Baram, T.Z.; Stern, H.S. Prenatal maternal mood patterns predict child temperament and adolescent mental health. J. Affect. Disord. 2018, 228, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Handayani, P.W.; Hidayanto, A.N.; Pinem, A.A.; Sandhyaduhita, P.I.; Budi, I. Hospital nformation system user acceptance factors: User group perspectives. Inform. Health Soc. Care 2018, 43, 84–107. [Google Scholar] [CrossRef] [PubMed]
- Pincus, S.M.; Schmidt, P.J.; Palladino-Negro, P.; Rubinow, D.R. Differentiation of women with premenstrual dysphoric disorder, recurrent brief depression, and healthy controls by daily mood rating dynamics. J. Psychiatr. Res. 2008, 42, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Tastle, W.J.; Wierman, M.J. An information theoretic measure for the evaluation of ordinal scale data. Behav. Res. Methods 2006, 38, 487–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tastle, W.J.; Wierman, M.J. Consensus and dissention: A measure of ordinal dispersion. Int. J. Approx. Reason. 2007, 45, 531–545. [Google Scholar] [CrossRef]
- Lavrakas, P.J. Encyclopedia of Survey Research Methods; Sage: Thousand Oaks, CA, USA, 2008; ISBN 9781412918084. [Google Scholar]
- Lesne, A. Shannon entropy: A rigorous notion at the crossroads between probability, information theory, dynamical systems and statistical physics. Math. Struct. Comput. Sci. 2014, 24. [Google Scholar] [CrossRef]






| Association/Institution | Membership M | Respondents R | R/M (%) |
|---|---|---|---|
| Acupuncture Association of Chartered Physiotherapists (AACP) | 6000 | 5 | 0.08% |
| Acupuncture Society (AS) | 1000 | 20 | 2.0% |
| Association of Traditional Chinese Medicine (ATCM) | 700 | 10 | 1.43% |
| British Academy of Western Medical Acupuncture (BAWMA) | 150 | 12 | 8.00% |
| British Acupuncture Council (BAcC) | 3000 | 56 | 1.87% |
| British Medical Acupuncture Society (BMAS) | 2300 | 10 | 0.43% |
| Chinese Medical Institute and Register (CMIR) | 240 | 1 | 0.42% |
| College of Chinese Medicine (CCM) | unknown | n/a | |
| College of Integrated Chinese Medicine (CICM) | unknown | n/a | |
| Northern College of Acupuncture (NCA) | unknown | n/a |
| “Now” or “Then” | How counted | “Yes” responses | “No” responses | “DK” responses |
|---|---|---|---|---|
| NOW | By respondent | 53.3 (35.4–66.7) | 25.0 (8.3–38.3) | 15.0 (6.7–29.6) |
| By question | 53.1 (40.6–62.3) | 25.4 (19.5–31.8) | 16.2 (12.8–26.5) | |
| THEN | By respondent | 42.5 (18.8–63.3) | 21.7 (5.0–44.2) | 13.3 (1.7–47.9) |
| By question | 43.9 (35.3–49.8) | 25.4 (20.8–33.1) | 28.9 (23.7–34.2) |
| NOW | THEN | |||
|---|---|---|---|---|
| Most responses | Fewest responses | Most responses | Fewest responses | |
| Yes | Willing to follow advice (101) Able to relax (93) Self-motivated (90) Exercise (89) Diet (85) General health (85) Openness (85) | Gender issues (17) Ethnicity (21) Alexithymia (21) Education (28) Relnship status (30) (and 4 others, a tied 31) | Willing to follow advice (84) Exercise (74) Able to relax (73) General health (73) Self-motivated (72) Diet (71) | Ethnicity (13) Alexithymia (15) Gender issues (16) Character when young (22) Birth/prenatal (23) Child poverty (26) |
| No | Gender (75) Ethnicity (74) Education (69) Relnship status (60) Age (59) Sceptical (57) | Willing to follow advice (9) Central sensitisn (13) Able to relax (14) Alexithymia (15) Psychotic (15) Self-motivated (15) | Ethnicity (73) Gender (68) Education (56) Relnship status (53) Gender issues (50) Age (47) | Willing to follow advice (7) Commitment (14) General health (14) Openness (16) Self-motivated (16) Exercise (17) |
| DK | Alexithymia (78) Gender issues (52) Central sensitsn (51) TCM pattern (47) Child poverty (45) Character when young (44) | Willing to follow advice (5) Able to relax (6) Age (6) Negativity (7) Gender (7) Self-motivated (8) | ||
| NOW | THEN | |||||
|---|---|---|---|---|---|---|
| Gender | Yes | No | DK | Yes | No | DK |
| Female | 33 (22–42) | 15 (4–21) | 10 (4–17) | 31 * (15–40) | 16 (3–27) | 6 * (1–21) |
| Male | 27 (20–36) | 15 (6–30) | 8 (3–21) | 20 * (0–34) | 8 (0–27) | 19 * (2–59) |
| Profession | Yes-To-No Count Ratios NOW | Yes-To-No Count Ratios THEN |
|---|---|---|
| Acupuncturists | 1.7 (0.9–5.1) | 1.4 (0.6–4.9) |
| Medical doctors | 2.3 (2–2.7) | 2.4 (1.3–2.5) |
| Physiotherapists | 6.2 (1.8–17.6) | 2.9 (1.7–4.1) |
| Nurses (and midwives) | 4.8 (1.3–12.5) | 3.5 (2.5–5.1) |
| Others | 2.4 (1.5–2.9) | 2.1 (1.0–3.1) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayor, D.F.; McClure, L.S.; Clayton McClure, J.H. Individual Differences in Responsiveness to Acupuncture: An Exploratory Survey of Practitioner Opinion. Medicines 2018, 5, 85. https://doi.org/10.3390/medicines5030085
Mayor DF, McClure LS, Clayton McClure JH. Individual Differences in Responsiveness to Acupuncture: An Exploratory Survey of Practitioner Opinion. Medicines. 2018; 5(3):85. https://doi.org/10.3390/medicines5030085
Chicago/Turabian StyleMayor, David F., Lara S. McClure, and J. Helgi Clayton McClure. 2018. "Individual Differences in Responsiveness to Acupuncture: An Exploratory Survey of Practitioner Opinion" Medicines 5, no. 3: 85. https://doi.org/10.3390/medicines5030085