3D Printing and 3D Bioprinting in Pediatrics
Abstract
:1. Introduction
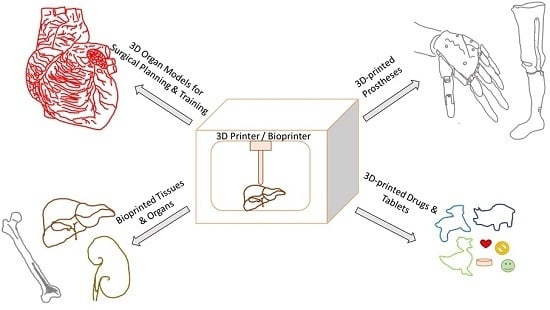
2. Applications in Pediatrics
2.1. Surgical Planning
2.1.1. Congenital Heart Disease (CHD)
2.1.2. Other Applications
2.1.3. Strengths and Limitations of 3D-Printed Organ Models
2.2. Prostheses
2.2.1. Hand Prostheses
2.2.2. Other Prostheses
2.2.3. Strengths and Limitations of 3D-Printed Prostheses
2.3. Tissue Constructs
2.4. Drug Printing
2.4.1. Product Complexity
2.4.2. Personalization
2.4.3. On-Demand Manufacturing
3. Conclusions
Author Contributions
Conflicts of Interest
References
- ASTM. Committee F42 on Additive Manufacturing Technologies; ASTM International: West Conshohocken, PA, USA, 2009. [Google Scholar]
- OED Online. Oxford University Press: Oxford, UK, 2016. Available online: http://www.oed.com/ (accessed on 16 June 2017).
- Vijayavenkataraman, S.; Lu, W.F.; Fuh, J.Y. 3D bioprinting of skin: A state-of-the-art review on modelling, materials, and processes. Biofabrication 2016, 8, 032001. [Google Scholar] [CrossRef] [PubMed]
- Vijayavenkataraman, S. A Perspective on Bioprinting Ethics. Artif. Organs 2016, 40, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Vijayavenkataraman, S.; Lu, W.F.; Fuh, J.Y. 3D bioprinting–An Ethical, Legal and Social Aspects (ELSA) framework. Bioprinting 2016, 1, 11–21. [Google Scholar] [CrossRef]
- Chimene, D.; Lennox, K.K.; Kaunas, R.R.; Gaharwar, A.K. Advanced bioinks for 3D printing: A materials science perspective. Ann. Biomed. Eng. 2016, 44, 2090. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Vahabzadeh, S.; Bandyopadhyay, A. Bone tissue engineering using 3D printing. Mater. Today 2013, 16, 496–504. [Google Scholar] [CrossRef]
- Sun, J.; Vijayavenkataraman, S.; Liu, H. An overview of scaffold design and fabrication technology for engineered knee meniscus. Materials 2017, 10, 29. [Google Scholar] [CrossRef]
- Yoo, S.J.; Thabit, O.; Kim, E.K.; Ide, H.; Yim, D.; Dragulescu, A.; Seed, M.; Grosse-Wortmann, L.; van Arsdell, G. 3D printing in medicine of congenital heart diseases. 3D Print. Med. 2015, 2, 3–5. [Google Scholar] [CrossRef]
- Gokuldoss, P.K.; Kolla, S.; Eckert, J. Additive Manufacturing Processes: Selective Laser Melting, Electron Beam Melting and Binder Jetting—Selection Guidelines. Materials 2017, 10, 672. [Google Scholar] [CrossRef]
- Jared, B.H.; Aguilo, M.A.; Beghini, L.L.; Boyce, B.L.; Clark, B.W.; Cook, A.; Kaehr, B.J.; Robbins, J. Additive manufacturing: Toward holistic design. Scr. Mater. 2017, 135, 141–147. [Google Scholar] [CrossRef]
- Cantinotti, M.; Valverde, I.; Kutty, S. Three-dimensional printed models in congenital heart disease. Int. J. Cardiovasc. Imaging 2016, 1, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ngan, E.M.; Rebeyka, I.M.; Ross, D.B.; Hirji, M.; Wolfaardt, J.F.; Seelaus, R.; Grosvenor, A.; Noga, M.L. The rapid prototyping of anatomic models in pulmonary atresia. J. Thorac. Cardiovasc. Surg. 2006, 132, 264–2699. [Google Scholar] [CrossRef] [PubMed]
- Noecker, A.M.; Chen, J.F.; Zhou, Q.; White, R.D.; Kopcak, M.W.; Arruda, M.J.; Duncan, B.W. Development of patient-specific three-dimensional pediatric cardiac models. ASAIO J. 2006, 52, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Sodian, R.; Weber, S.; Markert, M.; Rassoulian, D.; Kaczmarek, I.; Lueth, T.C.; Reichart, B.; Daebritz, S. Stereolithographic models for surgical planning in congenital heart surgery. Ann. Thorac. Surg. 2007, 83, 1854–1857. [Google Scholar] [CrossRef] [PubMed]
- Valverde, I.; Gomez, G.; Gonzalez, A.; Suarez-Mejias, C.; Adsuar, A.; Coserria, J.F.; Uribe, S.; Gomez-Cia, T.; Hosseinpour, A.R. Three-dimensional patient-specific cardiac model for surgical planning in Nikaidoh procedure. Cardiol. Young 2015, 25, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Valverde, I.; Gomez, G.; Coserria, J.F.; Suarez-Mejias, C.; Uribe, S.; Sotelo, J.; Velasco, M.N.; Santos De Soto, J.; Hosseinpour, A.R.; Gomez-Cia, T. 3D printed models for planning endovascular stenting in transverse aortic arch hypoplasia. Catheter. Cardiovasc. Interv. 2015, 85, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Weinstock, P.; Prabhu, S.P.; Flynn, K.; Orbach, D.B.; Smith, E. Optimizing cerebrovascular surgical and endovascular procedures in children via personalized 3D printing. J. Neurosurg. Pediatr. 2015, 16, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Hornung, A.; Kumpf, M.; Baden, W.; Tsiflikas, I.; Hofbeck, M.; Sieverding, L. Realistic 3D-Printed Tracheobronchial Tree Model from a 1-Year-Old Girl for Pediatric Bronchoscopy Training. Respiration 2017, 93, 293–295. [Google Scholar] [CrossRef] [PubMed]
- VanKoevering, K.K.; Morrison, R.J.; Prabhu, S.P.; Torres, M.F.L.; Mychaliska, G.B.; Treadwell, M.C.; Hollister, S.J.; Green, G.E. Antenatal three-dimensional printing of aberrant facial anatomy. Pediatrics 2015, 136, e1382–e1385. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.; Darwall, D.; Khalid, G.; Prabhu, R.; Kemp, A.; Arthurs, O.; Theobald, P. Development and validation of a physical model to investigate the biomechanics of infant head impact. Forens. Sci. Int. 2017, 276, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Xu, P.; Yao, Q.; Tang, K.; Lou, Y. 3D-printed navigation template in proximal femoral osteotomy for older children with developmental dysplasia of the hip. Sci. Rep. 2017, 7, 44993. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Yao, Q.; Xu, P.; Wang, L. Application of computer-aided design and 3D-printed navigation template in Locking Compression Pediatric Hip Plate™ placement for pediatric hip disease. Int. J. Comput. Assist. Radiol. Surg. 2017, 5, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Loke, Y.H.; Harahsheh, A.S.; Krieger, A.; Olivieri, L.J. Usage of 3D models of tetralogy of Fallot for medical education: Impact on learning congenital heart disease. BMC Med. Educ. 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Cromeens, B.P.; Ray, W.C.; Hoehne, B.; Abayneh, F.; Adler, B.; Besner, G.E. Facilitating surgeon understanding of complex anatomy using a three-dimensional printed model. J. Surg. Res. 2017, 216, 18–25. [Google Scholar] [CrossRef]
- Maragiannis, D.; Jackson, M.S.; Igo, S.R.; Chang, S.M.; Zoghbi, W.A.; Little, S.H. Functional 3D printed patient-specific modeling of severe aortic stenosis. J. Am. Coll. Cardiol. 2014, 64, 1066–1068. [Google Scholar] [CrossRef] [PubMed]
- Ten Kate, J.; Smit, G.; Breedveld, P. 3D-printed upper limb prostheses: A review. Disabil. Rehabilit. Assist. Technol. 2017, 12, 300–314. [Google Scholar]
- Burn, M.B.; Ta, A.; Gogola, G.R. Three-Dimensional Printing of Prosthetic Hands for Children. J. Hand Surg. 2016, 41, e103–e109. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K. Openly innovative entrepreneurship practice: Cost-effective 3D printing electronic prosthetic hand. Int. J. Teach. Case Stud. 2016, 7, 51–65. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Peck, J.; Srivastava, R.; Katsavelis, D.; Carson, A. An Open Source 3D-Printed Transitional Hand Prosthesis for Children. J. Prosthet. Orthot. 2016, 1, 1–4. [Google Scholar] [CrossRef]
- Hofmann, M.; Harris, J.; Hudson, S.E.; Mankoff, J. Helping Hands: Requirements for a Prototyping Methodology for Upper-limb Prosthetics Users. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems ACM 2016, San Jose, CA, USA, 7–12 May 2016; pp. 1769–1780. [Google Scholar]
- How Doctors Printed My New Face. Available online: http://www.telegraph.co.uk/news/9962798/How-doctors-printed-my-new-face.html (accessed on 6 December 2016).
- Wei, Y.; Li-Tsang, C.W.; Liu, J.; Xie, L.; Yue, S. 3D-printed transparent facemasks in the treatment of facial hypertrophic scars of young children with burns. Burns 2017, 43, e19–e26. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.S.; Lightdale-Miric, N. Advances in 3D-Printed Pediatric Prostheses for Upper Extremity Differences. J. Bone Jt. Surg. Am. 2016, 98, 1320–1326. [Google Scholar]
- Jie, S.; Haoyong, Y.; Chaw, T.L.; Chiang, C.C.; Vijayavenkataraman, S. An Interactive Upper Limb Rehab Device for Elderly Stroke Patients. Procedia CIRP 2017, 60, 488–493. [Google Scholar] [CrossRef]
- Davids, J.R.; Wagner, L.V.; Meyer, L.C.; Blackhurst, D.W. Prosthetic management of children with unilateral congenital below-elbow deficiency. J. Bone Jt. Surg. Am. 2006, 88, 1294–1300. [Google Scholar] [CrossRef]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Ozbolat, I.T.; Yu, Y. Bioprinting toward organ fabrication: Challenges and future trends. IEEE Trans. Biomed. Eng. 2013, 60, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Mironov, V.; Kasyanov, V.; Markwald, R.R. Organ printing: From bioprinter to organ biofabrication line. Curr. Opin. Biotechnol. 2011, 22, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Sears, N.A.; Seshadri, D.R.; Dhavalikar, P.S.; Cosgriff-Hernandez, E. A Review of Three-Dimensional Printing in Tissue Engineering. Tissue Eng. Part B Rev. 2016, 1, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, A.; Atala, A. Printing Technologies for Medical Applications. Trends Mol. Med. 2016, 22, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Vijayavenkataraman, S.; Wang, D.; Jing, L.; Sun, J.; He, K. Influence of electrohydrodynamic jetting parameters on the morphology of PCL scaffolds. Int. J. Bioprint. 2017, 3. [Google Scholar] [CrossRef]
- Cabrera, M.S.; Sanders, B.; Goor, O.J.; Driessen-Mol, A.; Oomens, C.W.; Baaijens, F.P. Computationally Designed 3D Printed Self-Expandable Polymer Stents with Biodegradation Capacity for Minimally Invasive Heart Valve Implantation: A Proof-of-Concept Study. 3D Print. Addit. Manuf. 2017, 4, 19–29. [Google Scholar] [CrossRef]
- Melocchi, A.; Parietti, F.; Maroni, A.; Foppoli, A.; Gazzaniga, A.; Zema, L. Hot-melt extruded filaments based on pharmaceutical grade polymers for 3D printing by fused deposition modeling. Int. J. Pharm. 2016, 509, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.; Madurawe, R.D.; Moore, C.M.; Khan, M.A.; Khairuzzaman, A. A new chapter in pharmaceutical manufacturing: 3D-printed drug products. Adv. Drug Deliv. Rev. 2016, 1, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, K. 3D printing: The future of manufacturing medicine. Pharm. J. 2015, 294, 598–600. [Google Scholar]
- Khaled, S.A.; Burley, J.C.; Alexander, M.R.; Roberts, C.J. Desktop 3D printing of controlled release pharmaceutical bilayer tablets. Int. J. Pharm. 2014, 461, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Kommanaboyina, B.; Rhodes, C.T. Trends in stability testing, with emphasis on stability during distribution and storage. Drug Dev. Ind. Pharm. 1999, 25, 857–868. [Google Scholar] [CrossRef] [PubMed]

| Category | Description | Examples |
|---|---|---|
| Vat Polymerization | Liquid photopolymer in a vat is selectively cured by light-activated polymerization | Stereolithography (SLA), micro-SLA, Digital Light Processing (DLP) |
| Material Jetting | Droplets of build material are selectively deposited | Objet PolyJet, 3D Systems Projet |
| Binder Jetting | Liquid bonding agent is selectively deposited to join powder materials | Zcorp, Voxeljet, ProMetal/ExOne |
| Material Extrusion | Material is selectively dispensed through a nozzle or orifice | Stratasys Fused Deposition Modeling (FDM) |
| Powder Bed Fusion | Thermal energy selectively fuses regions of a powder bed | Selective Laser Sintering (SLS), Selective Laser Melting (SLM) |
| Sheet Lamination | Sheets of material are bonded to form an object | Laminated Object Manufacturing (LOM) |
| Directed Energy Deposition | Focused thermal energy is used to fuse materials by melting as they are being deposited | Laser Engineered Net Shaping (LENS) |
| Category | Materials | Pros | Cons |
|---|---|---|---|
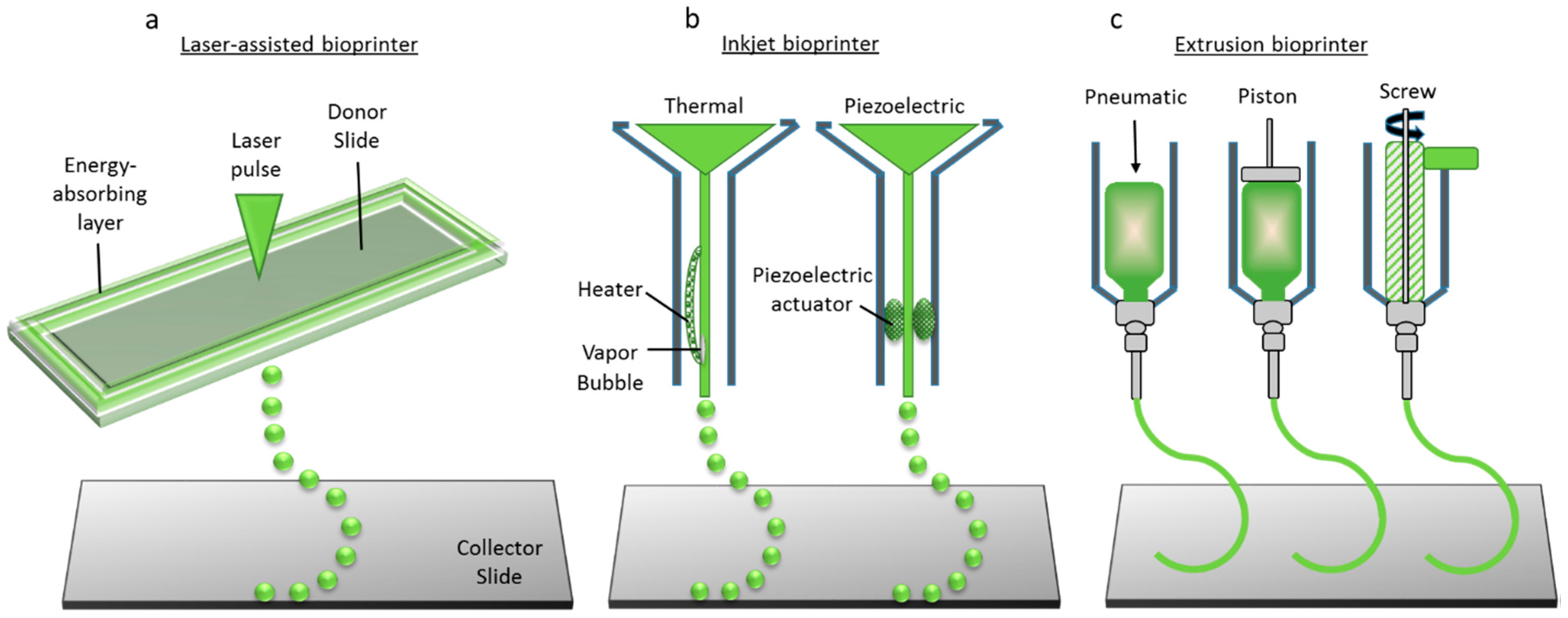
| Laser-assisted bioprinting | Cells in media | High accuracy | Low structural integrity |
| High resolution | Long printing time | ||
| Capable of single-cell level control printing | Low scalability | ||
| Inkjet printing | Liquids, Hydrogels | High throughput (Scalable) | Low structural integrity |
| High cell viability | Moderate accuracy | ||
| Affordable | Moderate precision | ||
| Extrusion or robotic dispensing bioprinting | Hydrogels, Cell aggregates | High structural integrity | Low accuracy |
| Short printing time | Low precision | ||
| Multi-nozzle multi-material printing feasible | Cells undergo shear stress at nozzle tip |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vijayavenkataraman, S.; Fuh, J.Y.H.; Lu, W.F. 3D Printing and 3D Bioprinting in Pediatrics. Bioengineering 2017, 4, 63. https://doi.org/10.3390/bioengineering4030063
Vijayavenkataraman S, Fuh JYH, Lu WF. 3D Printing and 3D Bioprinting in Pediatrics. Bioengineering. 2017; 4(3):63. https://doi.org/10.3390/bioengineering4030063
Chicago/Turabian StyleVijayavenkataraman, Sanjairaj, Jerry Y H Fuh, and Wen Feng Lu. 2017. "3D Printing and 3D Bioprinting in Pediatrics" Bioengineering 4, no. 3: 63. https://doi.org/10.3390/bioengineering4030063