Application of the Superelastic NiTi Spring in Ankle Foot Orthosis (AFO) to Create Normal Ankle Joint Behavior
Abstract
:1. Introduction
2. Methods
2.1. Custom-Fit Ankle Foot Orthosis (AFO)
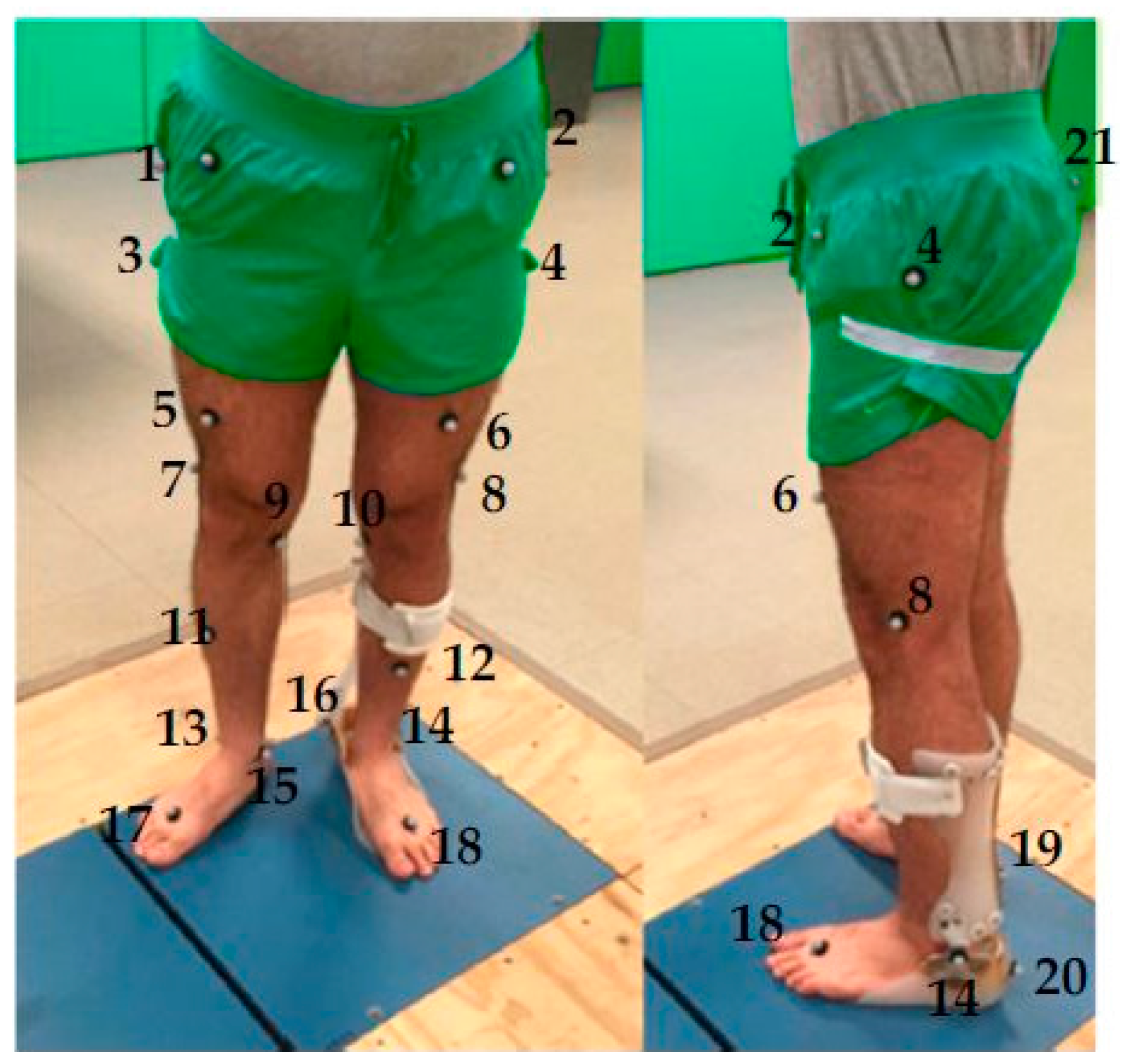
2.2. Motion Analysis and Data Analysis
2.3. Finite Element (FE) Modeling
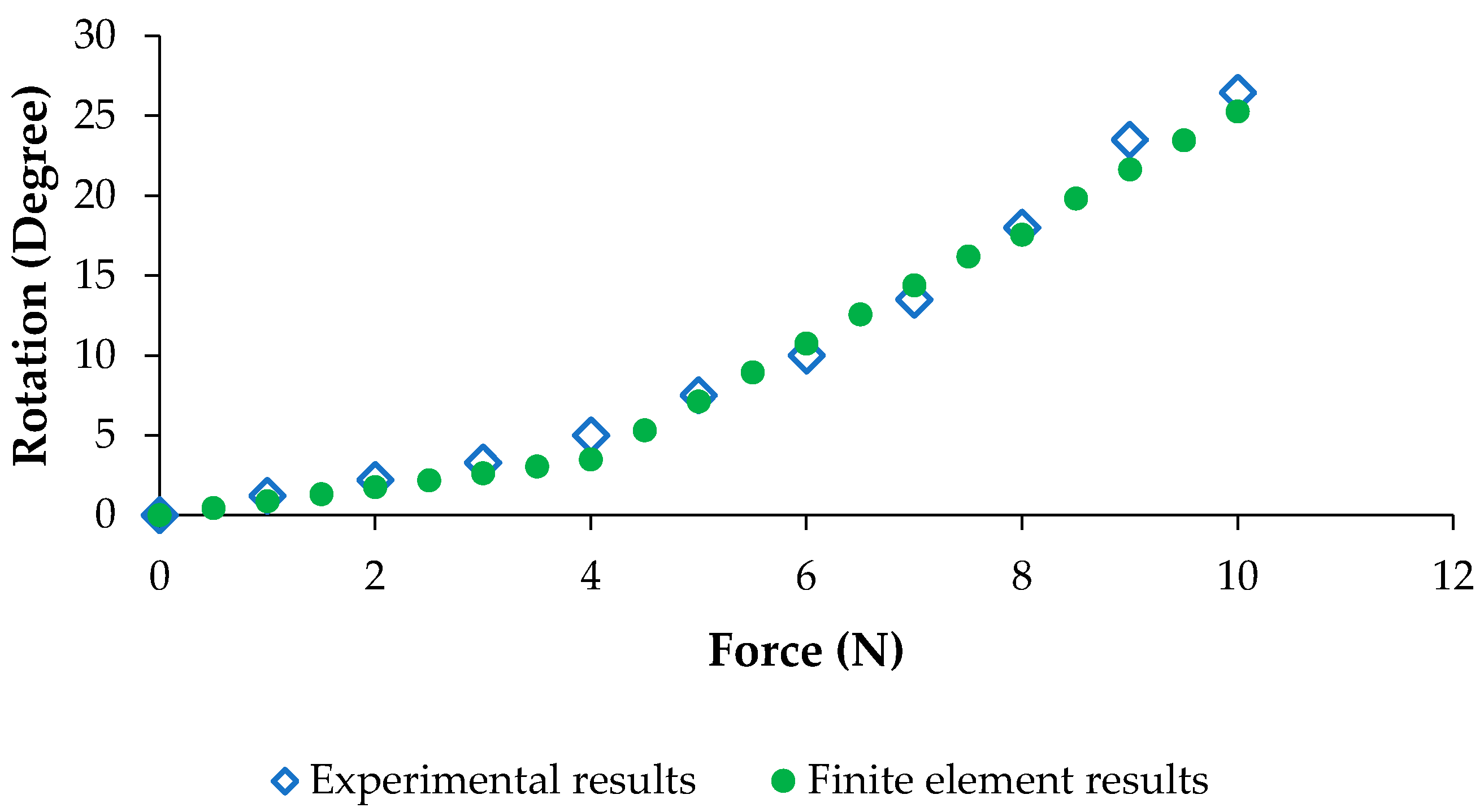
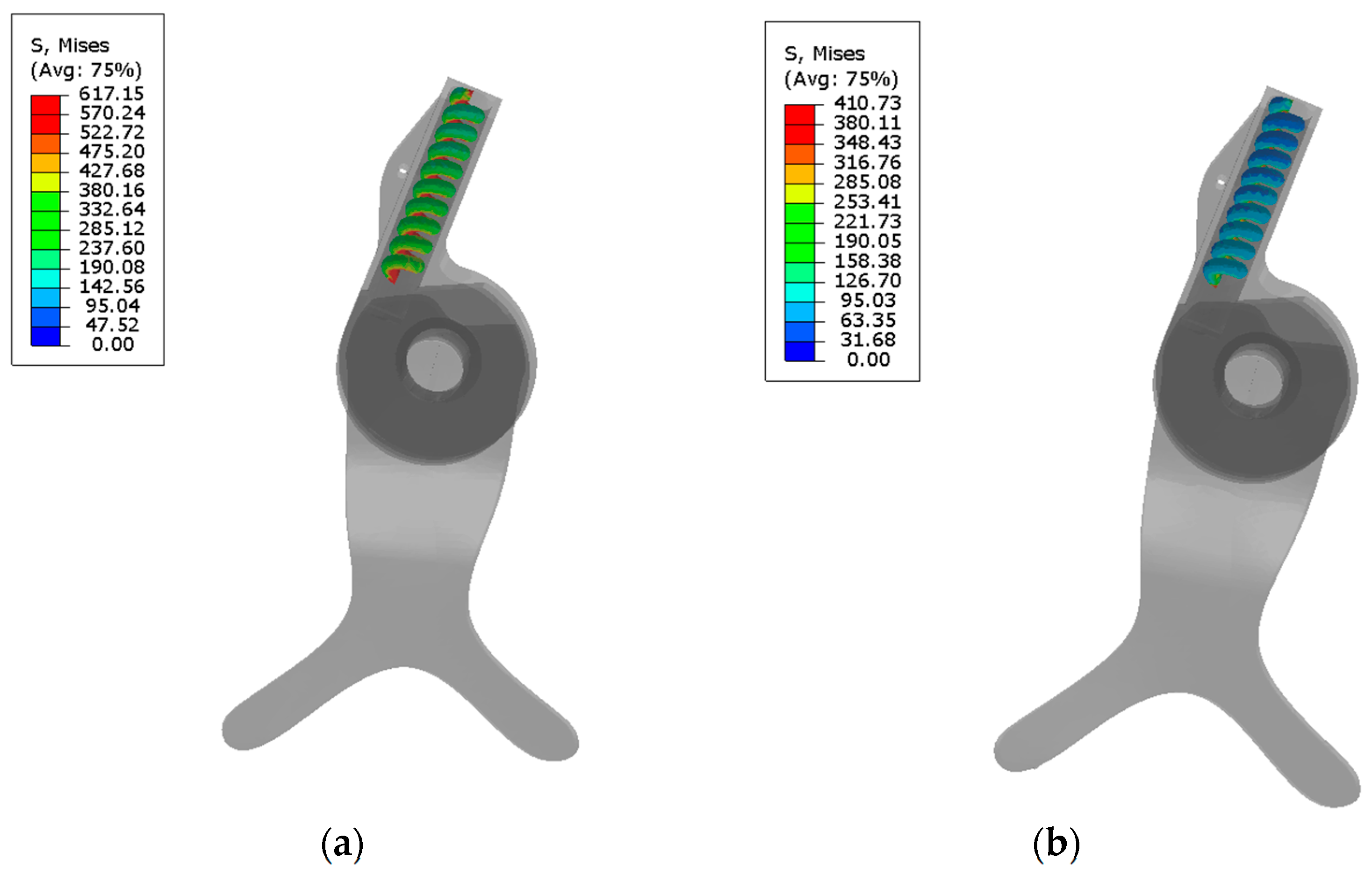
3. Results and Discussion
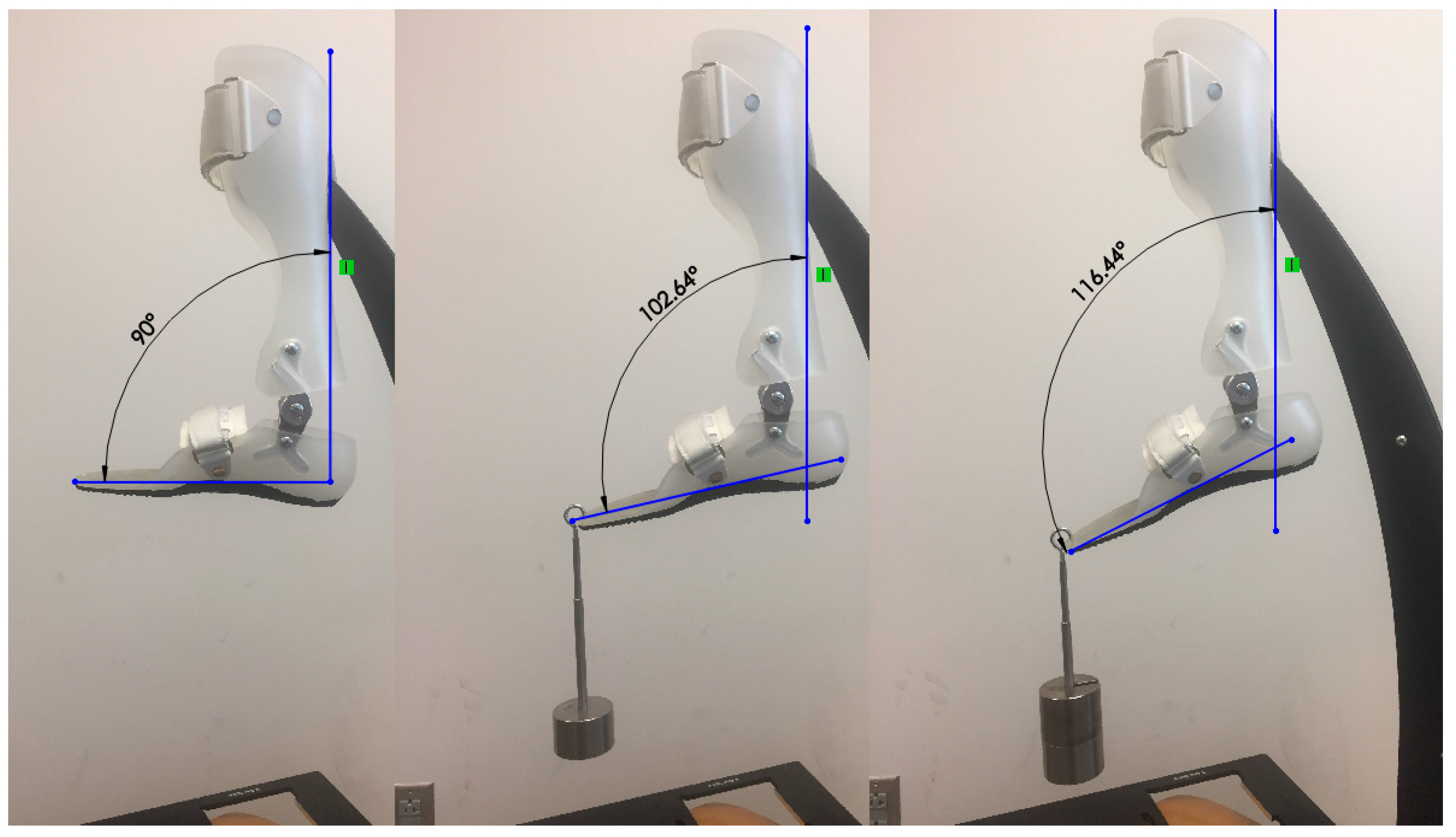
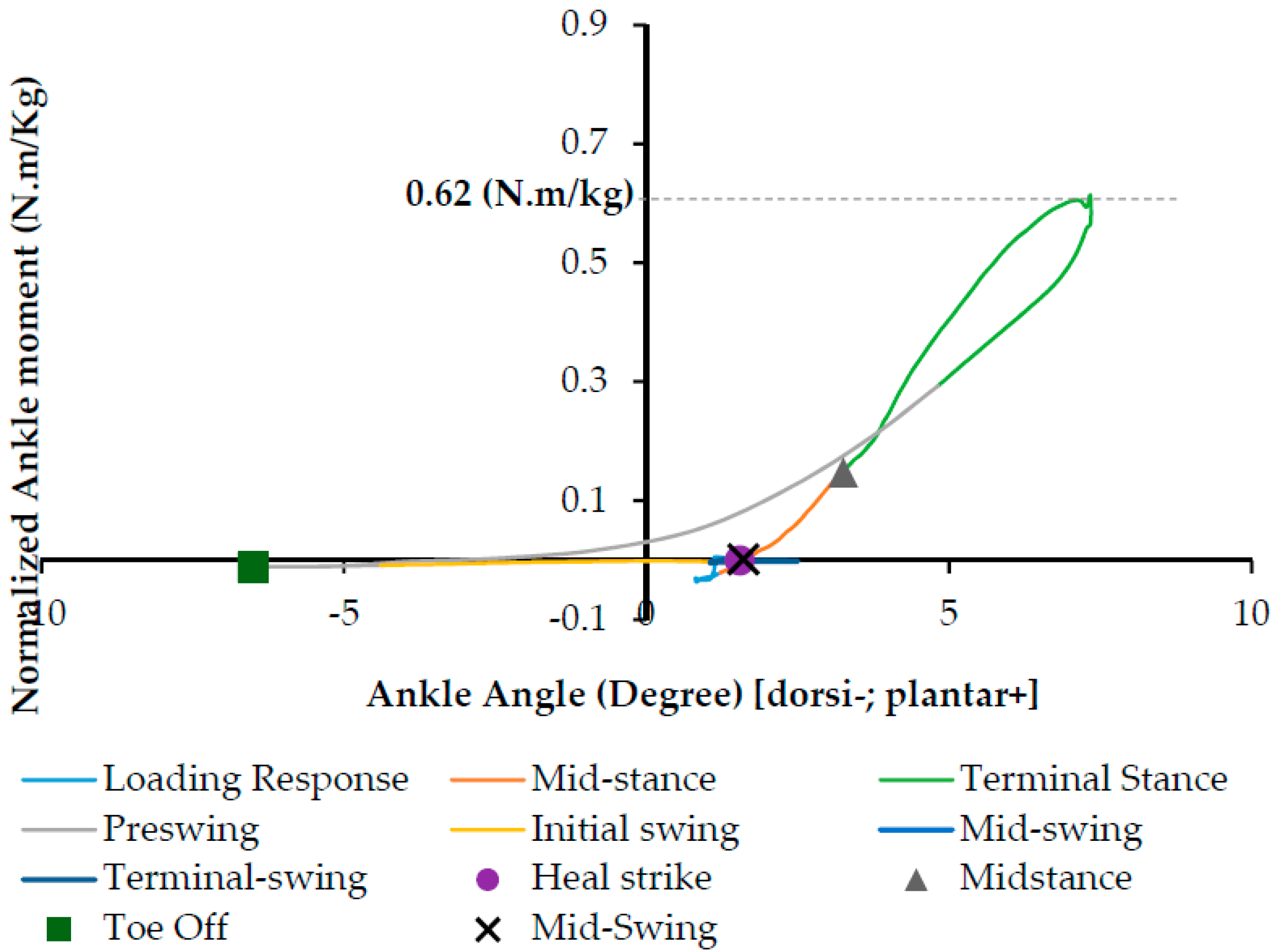
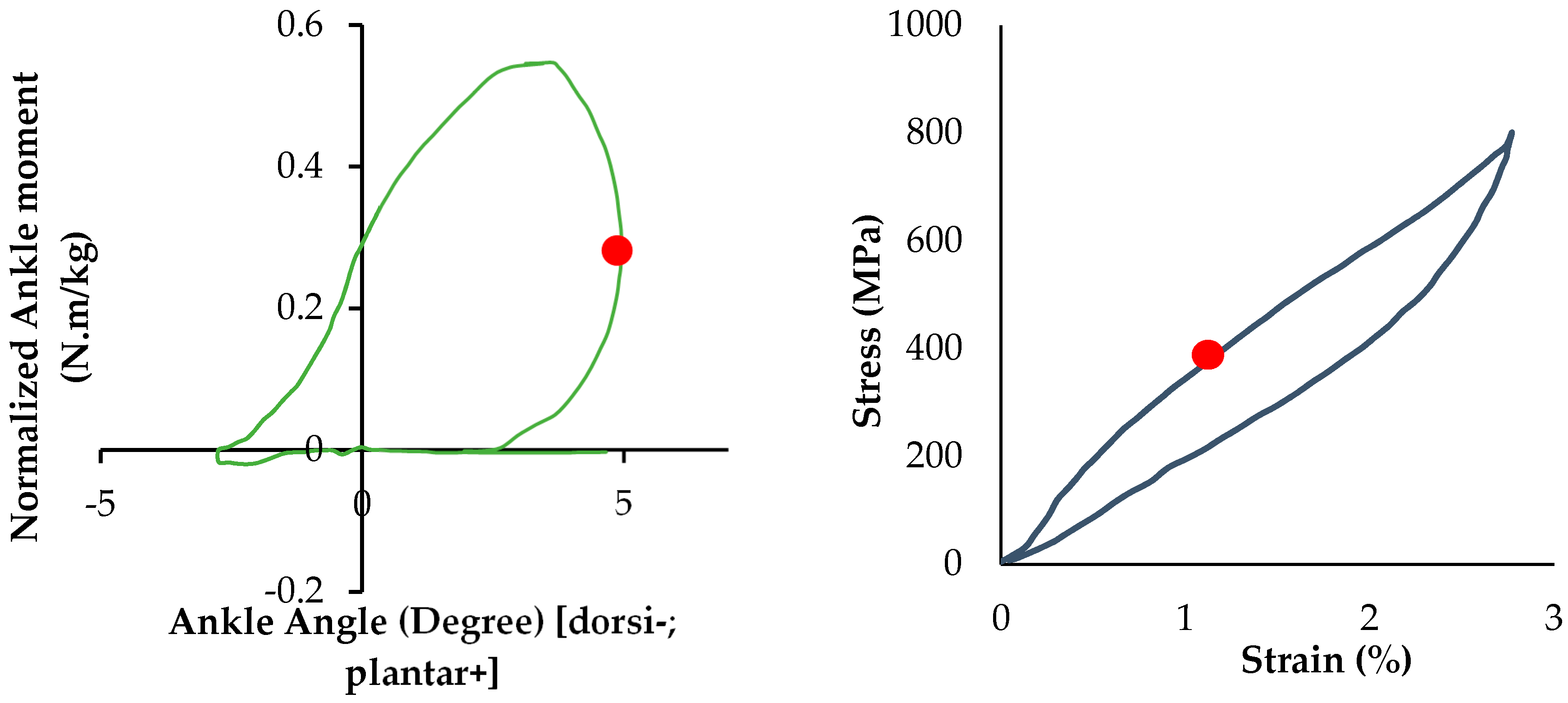
3.1. Ankle Torque-Angle Profile
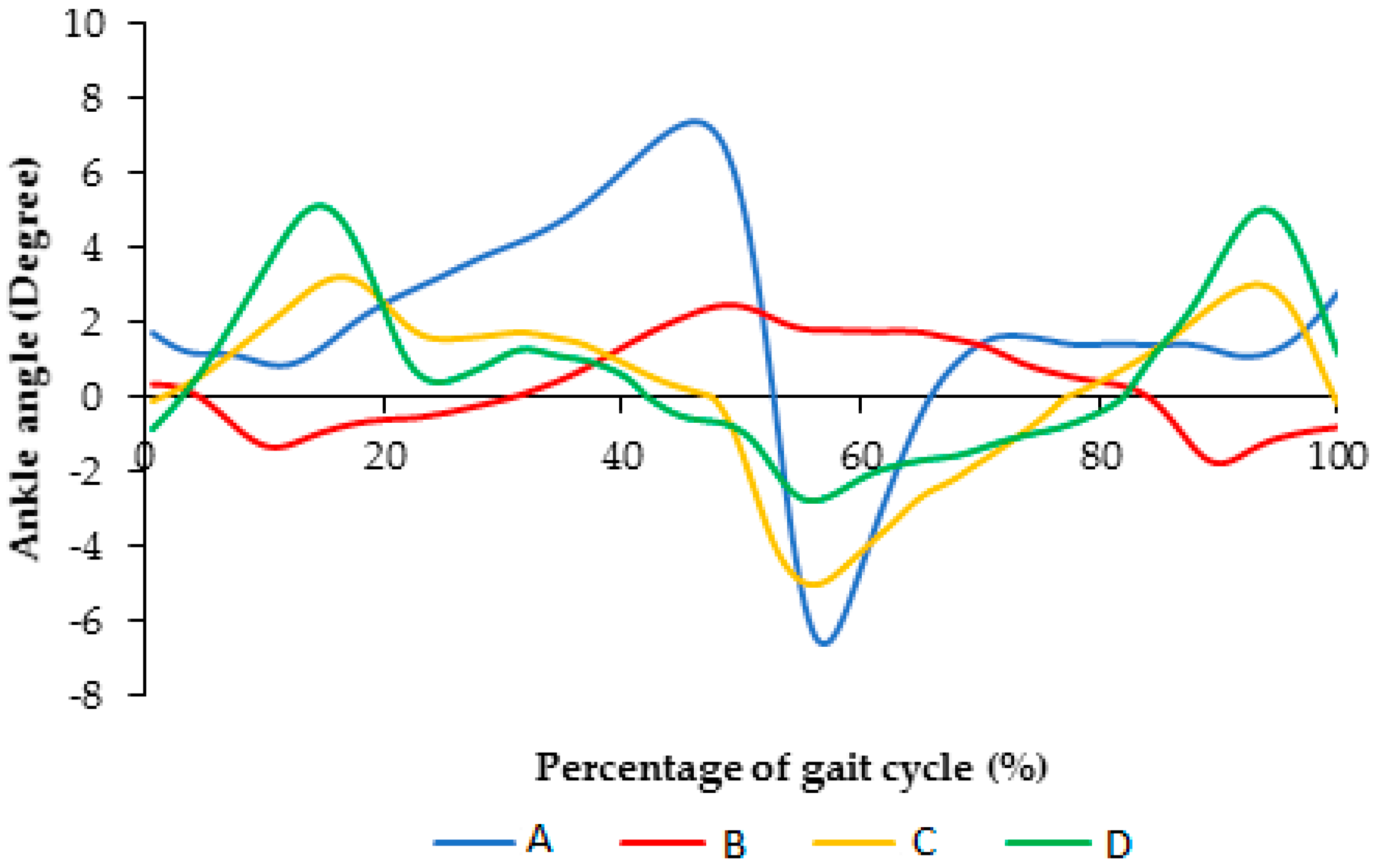
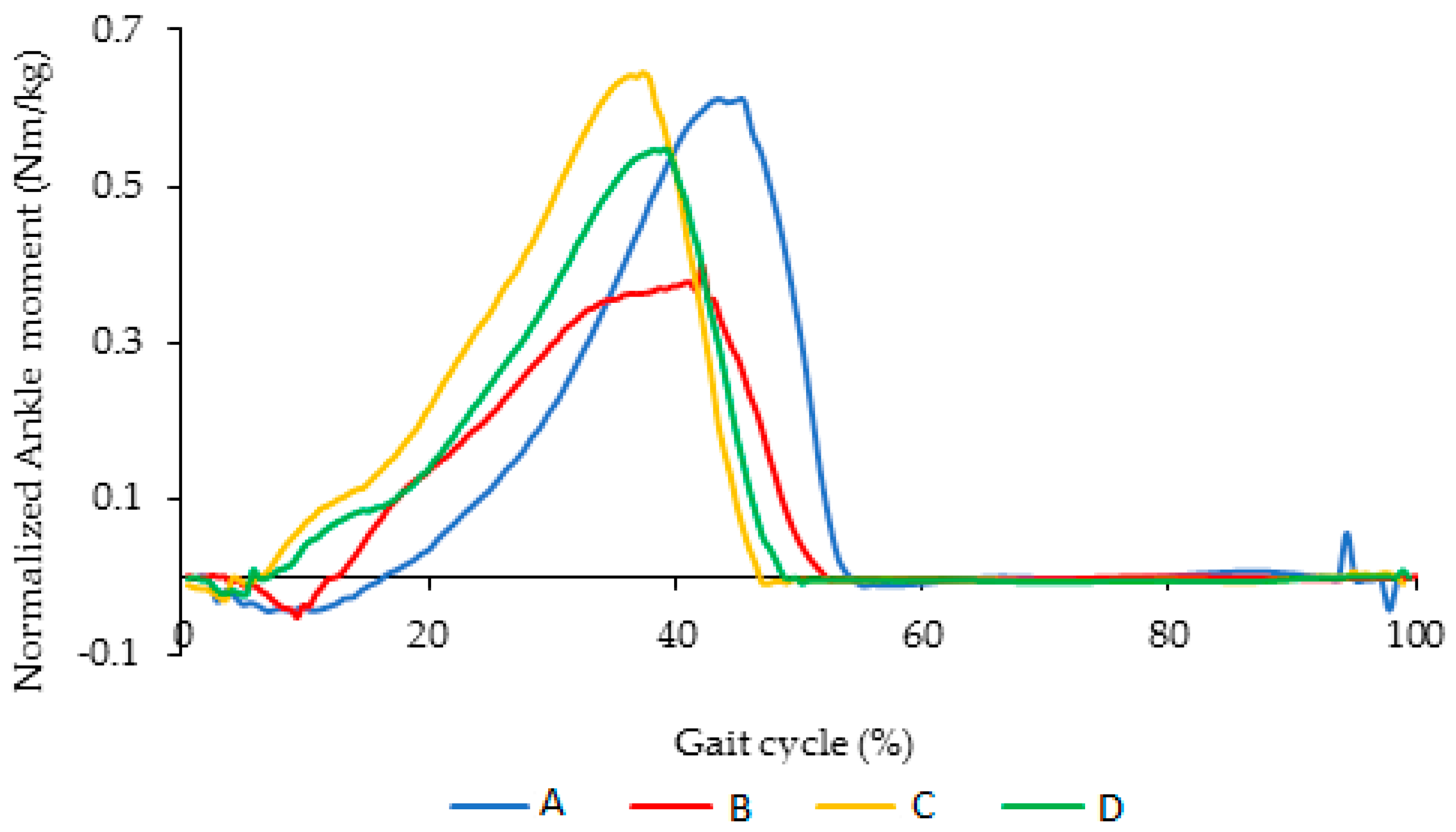
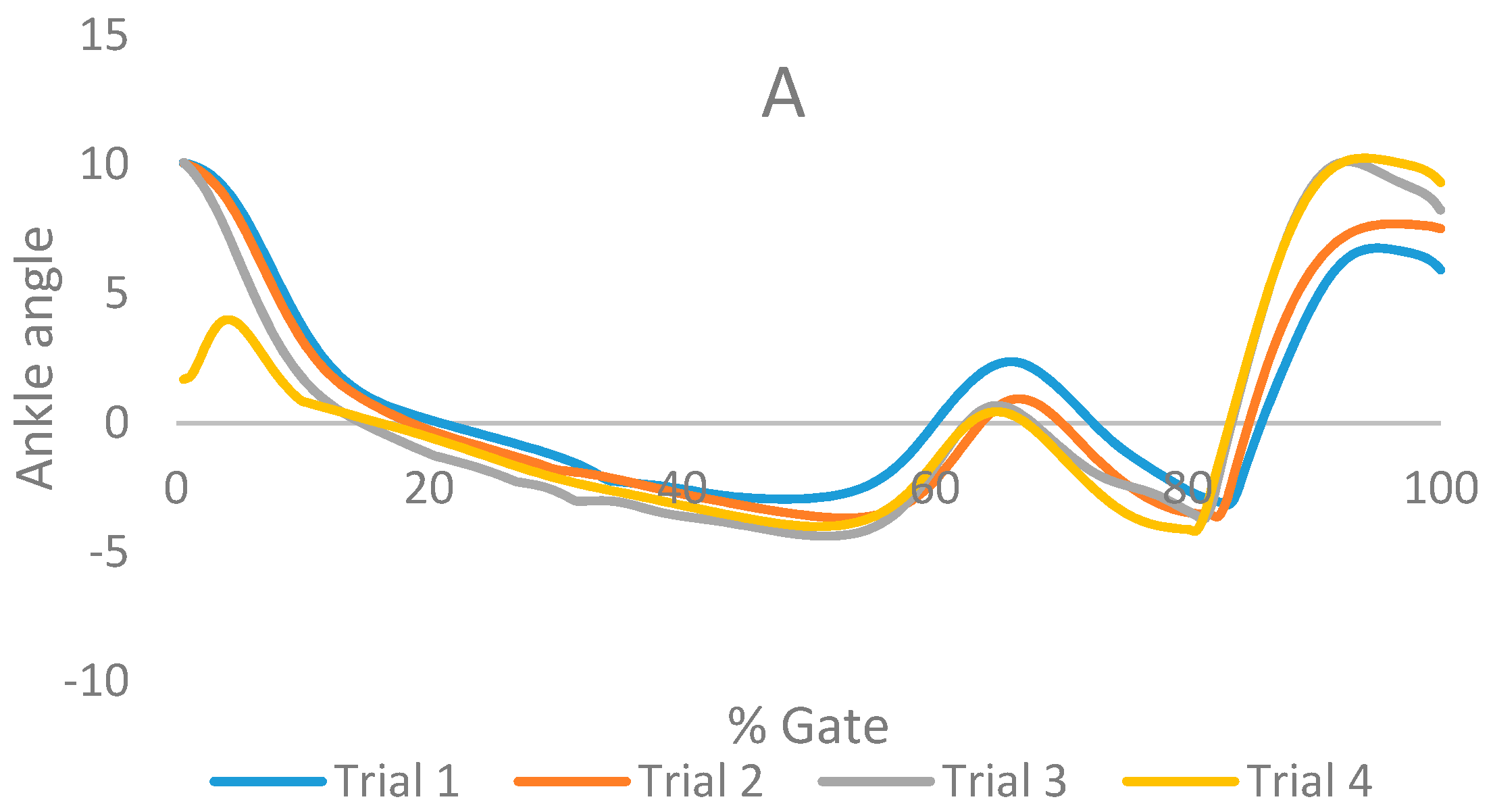
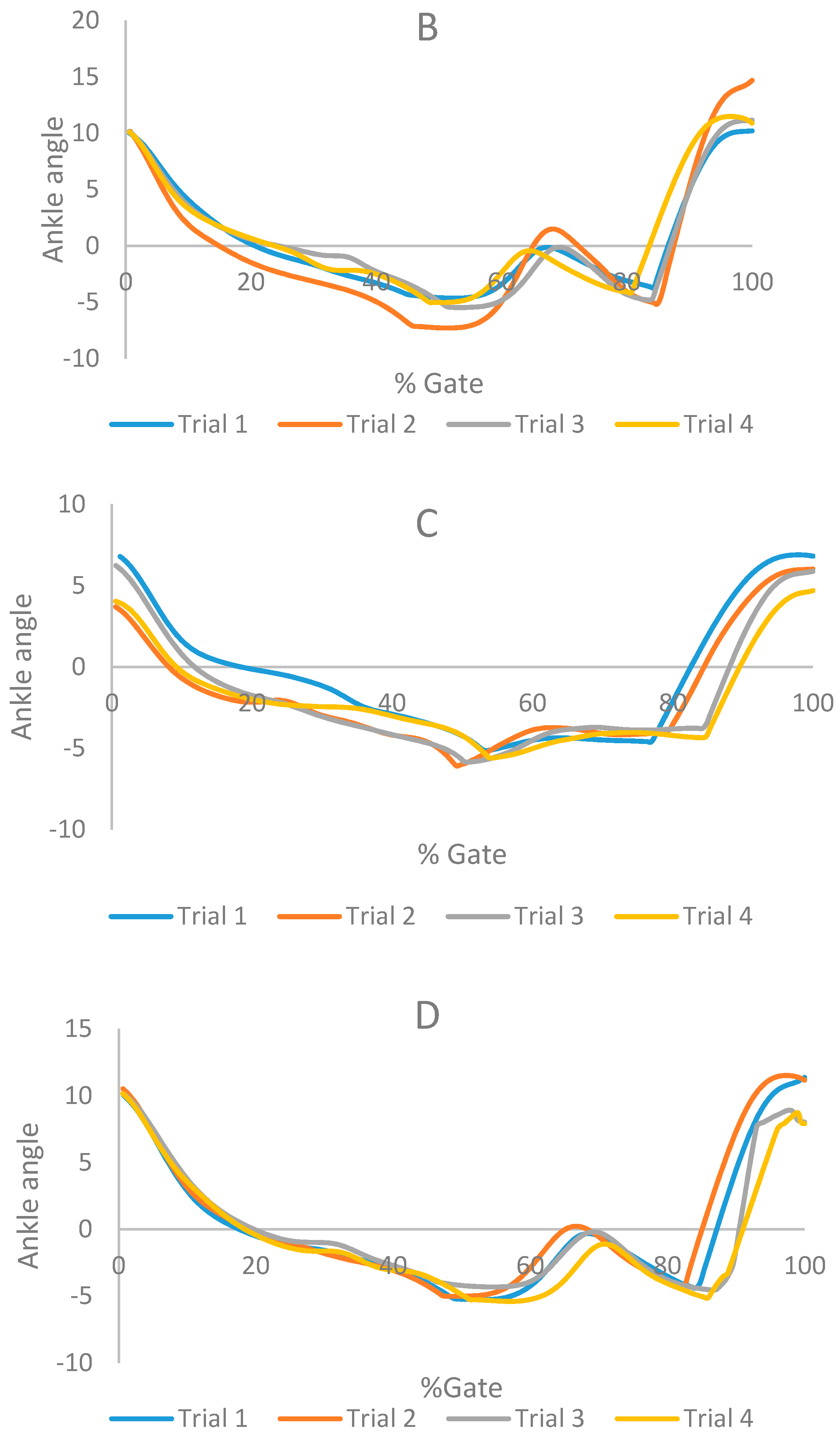
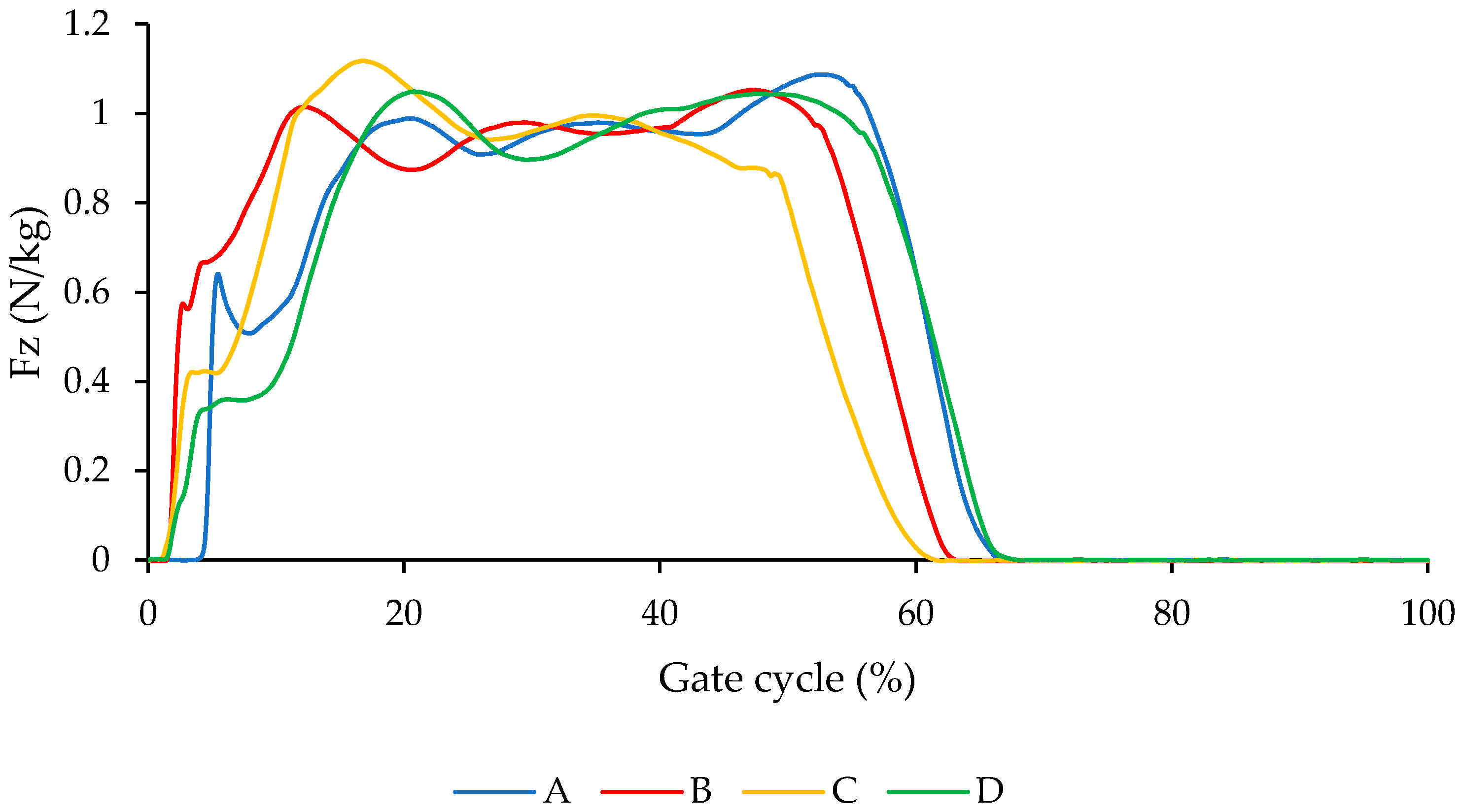
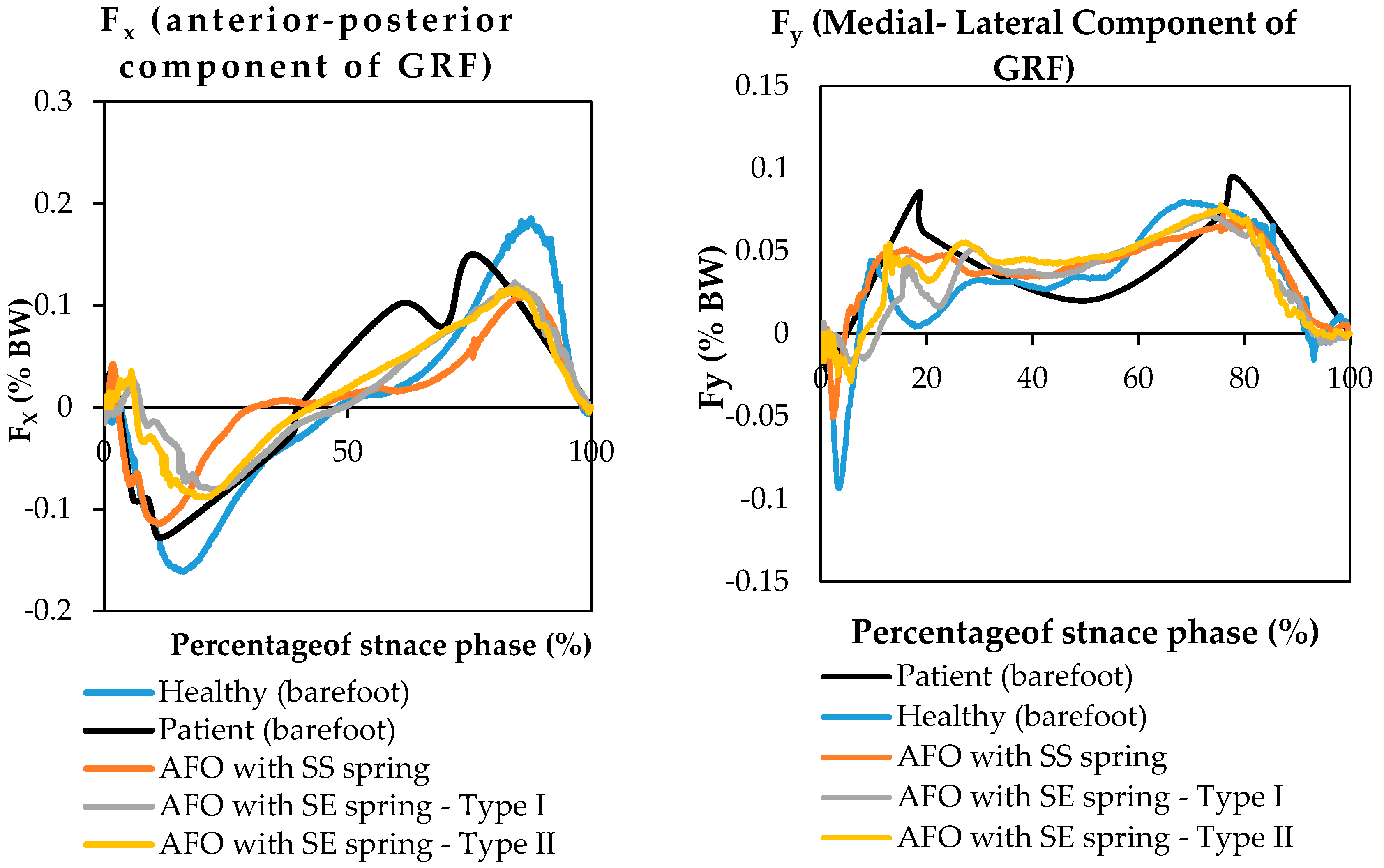
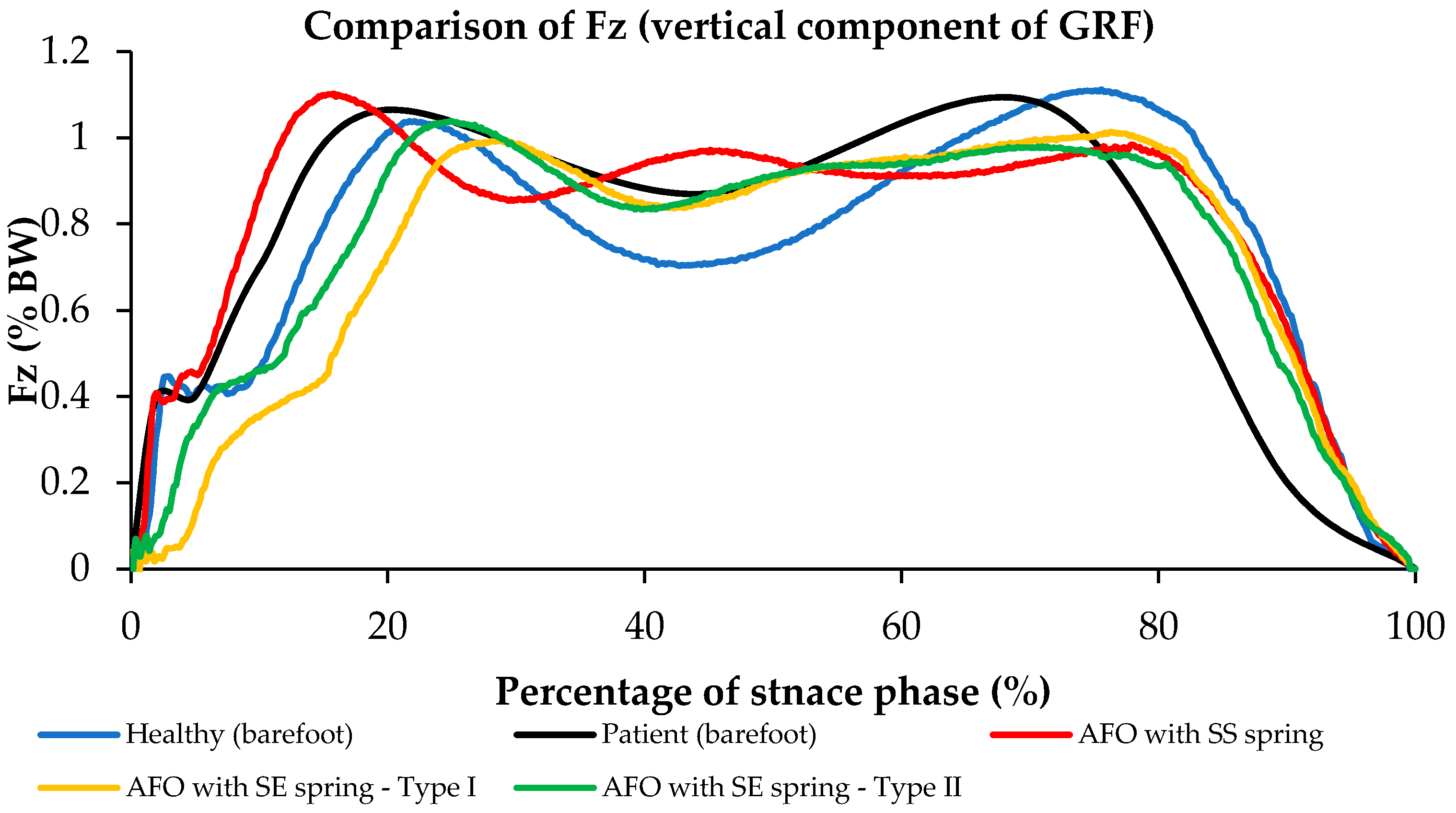
3.2. Evaluation of the Proposed AFO vs. Conventional AFO
4. Summary and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kirkup, J.R. A History of Limb Amputation; Springer Science & Business Media: New York, NY, USA, 2007. [Google Scholar]
- Trollinger, S.; Frazier, C.; Kunitz, S.; Miller, K.; Stout, A.; Fureman, B.; Jacobs, M.; Odenkirchen, J. National Institute of Neurological Disor-Ders and Stroke (Ninds), National Institutes of Health (Nih), Common Data Element (Cde) Project: Epilepsy Cde Update; Wiley-Blackwell Publishing, Inc.: Medford, MA, USA, 2009. [Google Scholar]
- Lenhart, R.L.; Sumarriva, N. Design of Improved Ankle-Foot Orthosis; University of Tennessee Honors Program: Knoxville, TN, USA, 2008. [Google Scholar]
- Amerinatanzi, A.; Summers, R.; Ahmadi, K.; Goel, V.K.; Hewett, T.E.; Nyman, E., Jr. A novel 3d approach for determination of frontal and coronal plane tibial slopes from mr imaging. Knee 2017, 24, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J. Powered lower limb orthotics in paraplegia. Paraplegia 1972, 9, 191–193. [Google Scholar] [CrossRef] [PubMed]
- Vukobratovic, M.; Hristic, D.; Stojiljkovic, Z. Development of active anthropomorphic exoskeletons. Med. Biol. Eng. 1974, 12, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Townsend, M.; Lepofsky, R. Powered walking machine prosthesis for paraplegics. Med. Biol. Eng. Comput. 1976, 14, 436–444. [Google Scholar] [CrossRef]
- Redford, J.B.; Basmajian, J.V.; Trautman, P. Orthotics: Clinical Practice and Rehabilitation Technology; Churchill Livingstone: London, UK, 1995. [Google Scholar]
- Amerinatanzi, A.; Zamanian, H.; Moghaddam, N.S.; Ibrahim, H.; Hefzy, M.S.; Elahinia, M. On the Advantages of Superelastic Niti in Ankle Foot Orthoses. In Proceedings of the ASME 2016 Conference on Smart Materials, Adaptive Structures and Intelligent Systems, Stowe, VT, USA, 28–30 September 2016; American Society of Mechanical Engineers: Stowe, VT, USA, 2016. [Google Scholar]
- Ingels, M.L.; Amerinatanzi, A.; Summers, R.K.; Hewett, T.E.; Goel, V.K.; Nyman, E., Jr. Finite element evaluation of the effect of medial and lateral tibial slope on anterior cruciate ligament strain: 3122 Board# 187 June 3, 2: 00 PM–3: 30 PM. Med. Sci. Sports Exerc. 2016, 48 (Suppl. S1), 887. [Google Scholar]
- Yamamoto, S.; Ebina, M.; Iwasaki, M.; Kubo, S.; Kawai, H.; Hayashi, T. Comparative Study of Mechanical Characteristics of Plastic AFOs. JPO J. Prosthet. Orthot. 1993, 5, 59. [Google Scholar] [CrossRef]
- Sumiya, T.; Suzuki, Y.; Kasahara, T. Stiffness control in posterior-type plastic ankle-foot orthoses: Effect of ankle trimline Part 2: Orthosis characteristics and orthosis/patient matching. Prosthet. Orthot. Int. 1996, 20, 132–137. [Google Scholar] [PubMed]
- Mulroy, S.J.; Eberly, V.J.; Gronely, J.K.; Weiss, W.; Newsam, C.J. Effect of AFO design on walking after stroke: Impact of ankle plantar flexion contracture. Prosthet. Orthot. Int. 2010, 34, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Choudhury, I.A.; Mamat, A.B. Mechanism and design analysis of articulated ankle foot orthoses for drop-foot. Sci. World J. 2014, 2014, 867869. [Google Scholar] [CrossRef] [PubMed]
- Yoshizawa, N. Gait trials of an active AFO for Achilles tendon ruptures. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009. [Google Scholar]
- Dollar, A.M.; Herr, H. Lower extremity exoskeletons and active orthoses: Challenges and state-of-the-art. IEEE Trans. Robot. 2008, 24, 144–158. [Google Scholar] [CrossRef]
- Blaya, J.A.; Herr, H. Adaptive control of a variable-impedance ankle-foot orthosis to assist drop-foot gait. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Herr, H.; Blaya, J.; Pratt, G.A. Active Ankle Foot Orthosis. Google Patents US8,808,214 B2, 19 August 2014. [Google Scholar]
- Blaya, J.A. Force-Controllable Ankle Foot Orthosis (AFO) to Assist Drop Foot Gait; Massachusetts Institute of Technology: Cambridge, MA, USA, 2002. [Google Scholar]
- Ferris, D.P.; Czerniecki, J.M.; Hannaford, B. An ankle-foot orthosis powered by artificial pneumatic muscles. J. Appl. Biomech. 2005, 21, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.; Sawicki, G.; Domingo, A. Powered lower limb orthoses for gait rehabilitation. Top. Spinal Cord Inj. Rehabil. 2005, 11, 34–49. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.P.; Gordon, K.E.; Sawicki, G.S.; Peethambaran, A. An improved powered ankle-foot orthosis using proportional myoelectric control. Gait Posture 2006, 23, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, G.S.; Ferris, D.P. Mechanics and energetics of level walking with powered ankle exoskeletons. J. Exp. Biol. 2008, 211, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Mataee, M.G.; Andani, M.T.; Elahinia, M. Adaptive ankle-foot orthoses based on superelasticity of shape memory alloys. J. Intell. Mater. Syst. Struct. 2015, 26, 639–651. [Google Scholar] [CrossRef]
- Bhadane-Deshpande, M. Towards a Shape Memory Alloy Based Variable Stiffness Ankle Foot Orthosis. Ph.D. Thesis, The University of Toledo, Toledo, OH, USA, 2012. [Google Scholar]
- Bhadane, M.Y.; Armstrong, C.; Hefzy, M.S.; Elahinia, M.H. An Automated Testing Assembly for characterizing Stiffness of AN Ankle Foot Orthosis. In Proceedings of the ASME 2011 Conference on Smart Materials, Adaptive Structures and Intelligent Systems, Scottsdale, AZ, USA, 18–21 September 2011; American Society of Mechanical Engineers: Scottsdale, AZ, USA, 2011. [Google Scholar]
- Bhadane, M.Y.; Elahinia, M.H. Stiffness control of a sma actuator. In Proceedings of the ASME 2009 Conference on Smart Materials, Adaptive Structures and Intelligent Systems, Oxnard, CA, USA, 21–23 September 2009; American Society of Mechanical Engineers: Oxnard, CA, USA, 2009. [Google Scholar]
- Yamamoto, S.; Ebina, M.; Miyazaki, S.; Kawai, H.; Kubota, T. Development of a new ankle-foot orthosis with dorsiflexion assist, Part 1: Desirable characteristics of ankle-foot orthoses for hemiplegic patients. JPO J. Prosthet. Orthot. 1997, 9, 174–179. [Google Scholar] [CrossRef]
- Yamamoto, S.; Hagiwara, A.; Mizobe, T.; Yokoyama, O.; Yasui, T. Development of an ankle-foot orthosis with an oil damper. Prosthet. Orthot. Int. 2005, 29, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Irby, S.E.; Kaufman, K.R.; Wirta, R.W.; Sutherland, D.H. Optimization and application of a wrap-spring clutch to a dynamic knee-ankle-foot orthosis. IEEE Trans. Rehabil. Eng. 1999, 7, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Cullell, A.; Moreno, J.C.; Rocon, E.; Forner-Cordero, A.; Pons, J.L. Biologically based design of an actuator system for a knee-ankle-foot orthosis. Mech. Mach. Theory 2009, 44, 860–872. [Google Scholar] [CrossRef]
- Tian, F.; Hefzy, M.S.; Elahinia, M. State of the Art Review of Knee-Ankle-Foot Orthoses. Ann. Biomed. Eng. 2015, 43, 427–441. [Google Scholar] [CrossRef] [PubMed]
- Zamanian, H. Toward Creating Normal Ankle Joint Behavior for Drop Foot Patients Using an Ankle Foot Orthosis (AFO) with Superplastic NiTi Springs; The University of Toledo: Toledo, OH, USA, 2017. [Google Scholar]
- Pittaccio, S.; Viscuso, S.; Beretta, E.; Turconi, A.C.; Strazzer, S. Pilot studies suggesting new applications of NiTi in dynamic orthoses for the ankle joint. Prosthet. Orthot. Int. 2010, 34, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Pittaccio, S.; Viscuso, S.; Rossini, M.; Magoni, L.; Pirovano, S.; Villa, E.; Besseghini, S.; Molteni, F. SHADE: A shape-memory-activated device promoting ankle dorsiflexion. J. Mater. Eng. Perform. 2009, 18, 824–830. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Y.; Yang, D.; Qi, M. The effect of ageing treatment on shape-setting and superelasticity of a nitinol stent. Mater. Charact. 2008, 59, 402–406. [Google Scholar] [CrossRef]
- Jahadakbar, A.; Shayesteh Moghaddam, N.; Amerinatanzi, A.; Dean, D.; Karaca, H.E.; Elahinia, M. Finite element simulation and additive manufacturing of stiffness-matched niti fixation hardware for mandibular reconstruction surgery. Bioengineering 2016, 3, 36. [Google Scholar] [CrossRef] [PubMed]
- Shayesteh Moghaddam, N.; Jahadakbar, A.; Amerinatanzi, A.; Skoracki, R.; Miller, M.; Dean, D.; Elahinia, M. Fixation Release and the Bone Bandaid: A New Bone Fixation Device Paradigm. Bioengineering 2017, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, N.S.; Andani, M.T.; Amerinatanzi, A.; Haberland, C.; Huff, S.; Miller, M.; Elahinia, M.; Dean, D. Metals for bone implants: Safety, design, and efficacy. Biomanuf. Rev. 2016, 1, 1. [Google Scholar] [CrossRef]
- Tehrani, M.; Sarvestani, A. Effect of chain length distribution on mechanical behavior of polymeric networks. Eur. Polym. J. 2017, 87, 136–146. [Google Scholar] [CrossRef]
- Moghaddam, N.S.; Jahadakbar, A.; Amerinatanzi, A.; Elahinia, M.; Miller, M.; Dean, D. Metallic fixation of mandibular segmental defects: Graft immobilization and orofacial functional maintenance. Plast. Reconstr. Surg. Glob. Open 2016, 4, e858. [Google Scholar] [CrossRef] [PubMed]
- Jamshidi, N.; Rostami, M.; Najarian, S.; Menhaj, M.B.; Saadatnia, M.; Salami, F. Assessment of ground reaction forces of steppage gait in comparison with normal gait. J. Musculoskelet. Res. 2009, 12, 45–52. [Google Scholar] [CrossRef]








| Model Component | Element | |
|---|---|---|
| Type of Element | Number of Element | |
| AFO (Bottom) | 3D, Solid, Tetrahedral, Deformable | 26,437 |
| AFO (Top) | 3D, Solid, Tetrahedral, Deformable | 65,179 |
| Spring (4 components) | 3D, Solid, Tetrahedral, Deformable | 26,058 |
| Hinge (Top) | 3D, Solid, Tetrahedral, Deformable | 13,090 |
| Hinge (Bottom) | 3D, Solid, Tetrahedral, Deformable | 21,037 |
| Component | Hinge | AFO | SE Spring | SS Spring |
|---|---|---|---|---|
| Material | Stainless steel | Plastic | Superelastic NiTi | Stainless steel |
| Young’s Modulus (GPa) | 220 | 20 | 30 */40 ** | 210 |
| Poisson’s Ratio | 0.33 | 0.27 | 0.33 | 0.33 |
| Martensitic Start (Ms) | - | - | −65 | - |
| Austenitic Start (As) | - | - | −23 | - |
| Martensitic Finish (Mf) | - | - | −88 | - |
| Austenitic Finish (Af) | - | - | −8 | - |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amerinatanzi, A.; Zamanian, H.; Shayesteh Moghaddam, N.; Jahadakbar, A.; Elahinia, M. Application of the Superelastic NiTi Spring in Ankle Foot Orthosis (AFO) to Create Normal Ankle Joint Behavior. Bioengineering 2017, 4, 95. https://doi.org/10.3390/bioengineering4040095
Amerinatanzi A, Zamanian H, Shayesteh Moghaddam N, Jahadakbar A, Elahinia M. Application of the Superelastic NiTi Spring in Ankle Foot Orthosis (AFO) to Create Normal Ankle Joint Behavior. Bioengineering. 2017; 4(4):95. https://doi.org/10.3390/bioengineering4040095
Chicago/Turabian StyleAmerinatanzi, Amirhesam, Hashem Zamanian, Narges Shayesteh Moghaddam, Ahmadreza Jahadakbar, and Mohammad Elahinia. 2017. "Application of the Superelastic NiTi Spring in Ankle Foot Orthosis (AFO) to Create Normal Ankle Joint Behavior" Bioengineering 4, no. 4: 95. https://doi.org/10.3390/bioengineering4040095






