Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
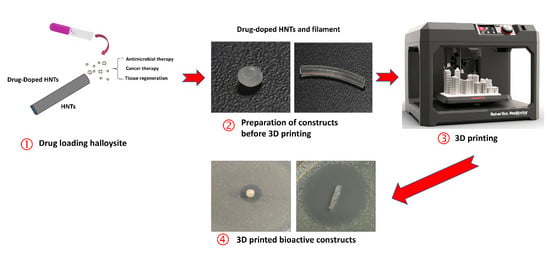
2.2. Methods
2.2.1. Vacuum Loading of Gentamicin
2.2.2. Preparation of PLA Filaments
2.2.3. PLA Filament Extrusion
2.2.4. 3D Printing
2.2.5. Gentamicin Release Profile
2.2.6. Bacterial Cultures
2.2.7. Liquid Broth Cultures
2.2.8. Statistical Analysis
3. Results
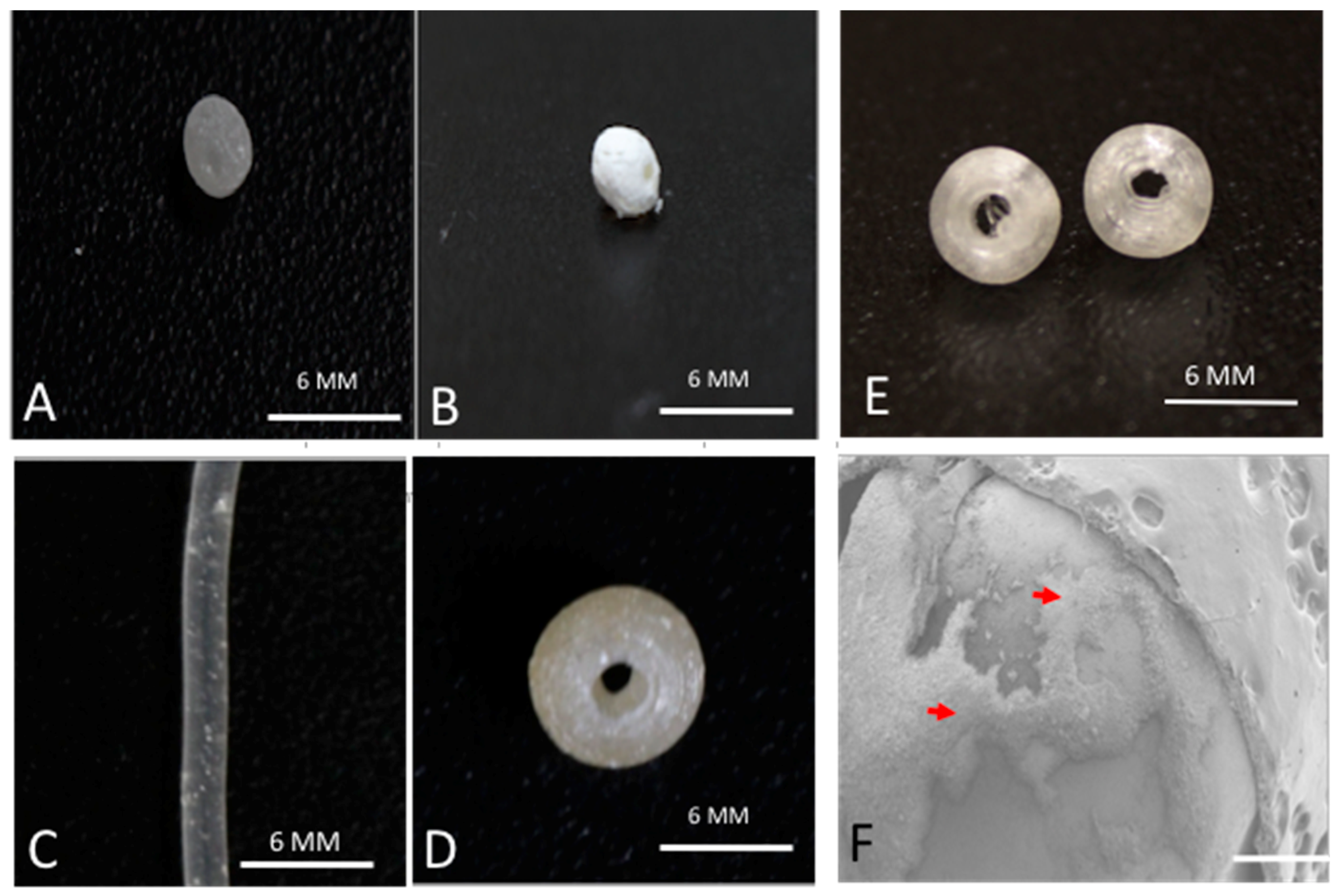
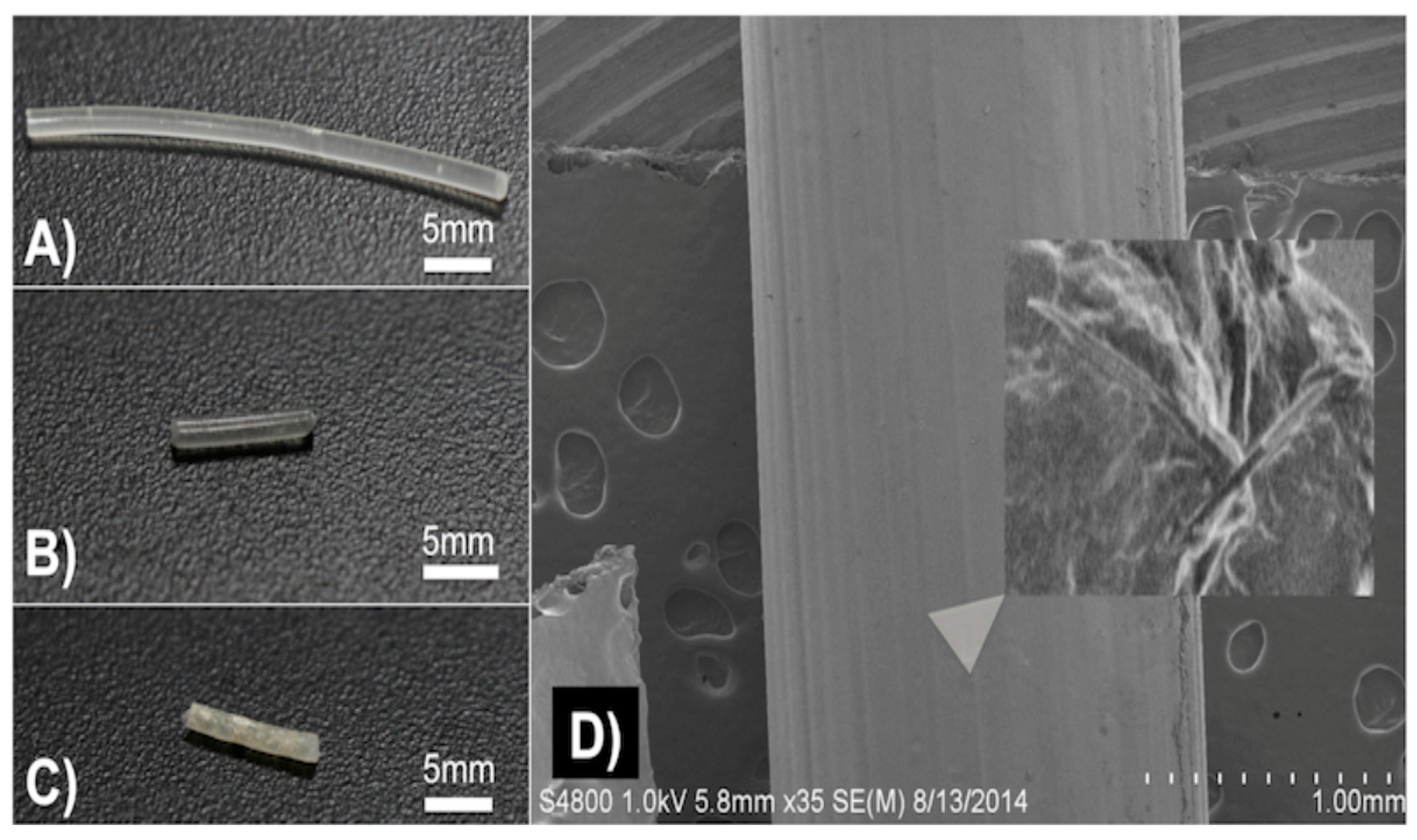
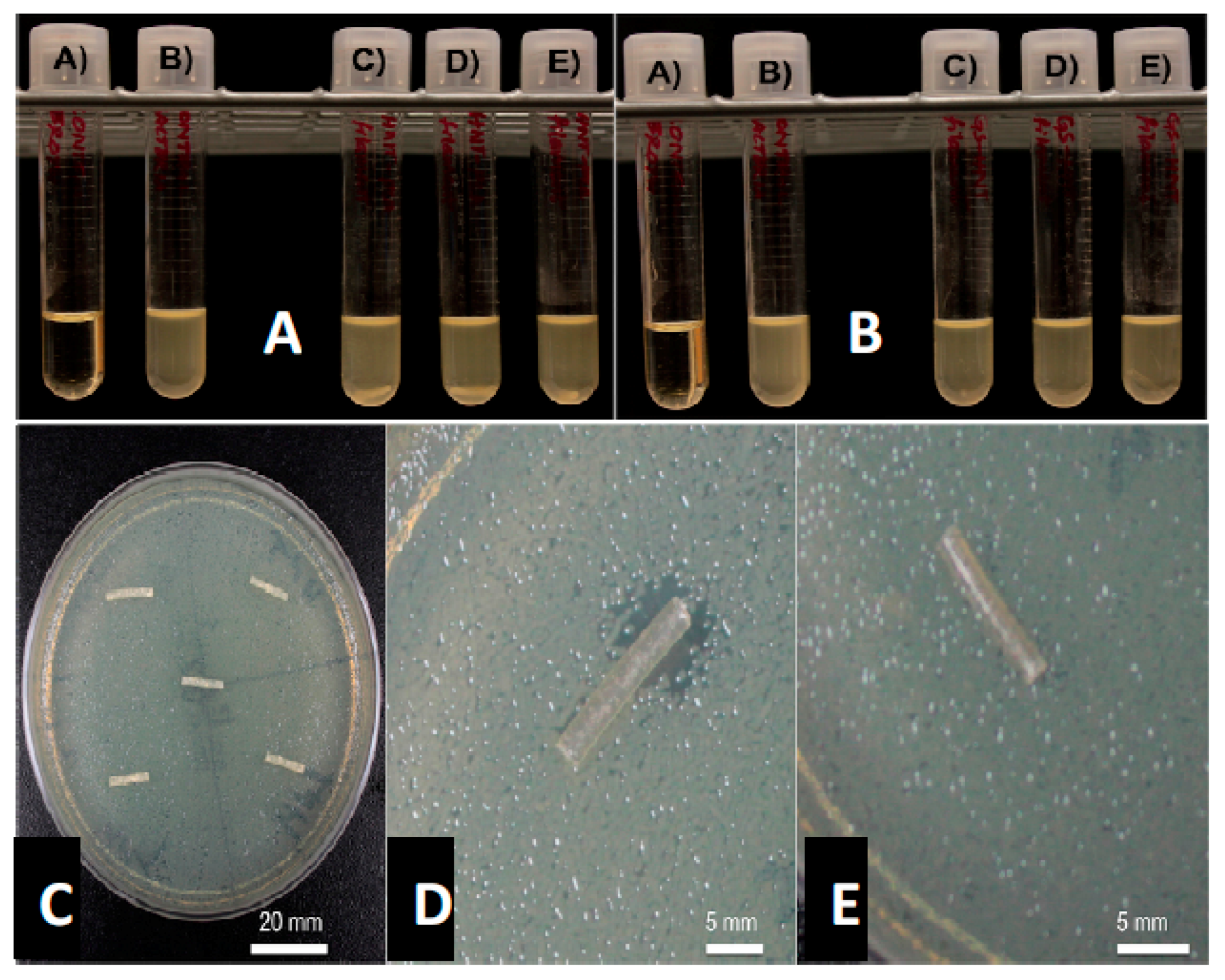
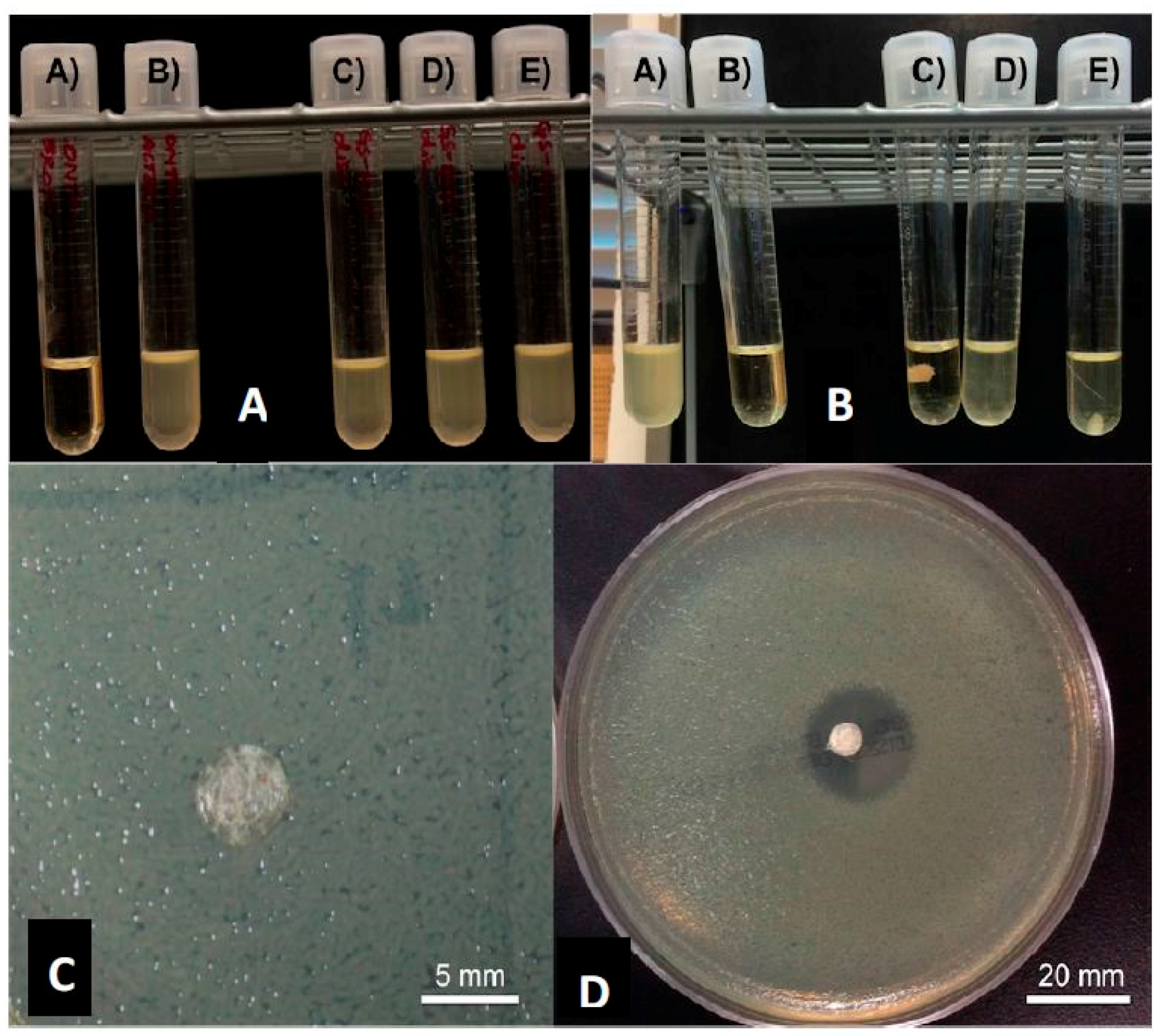
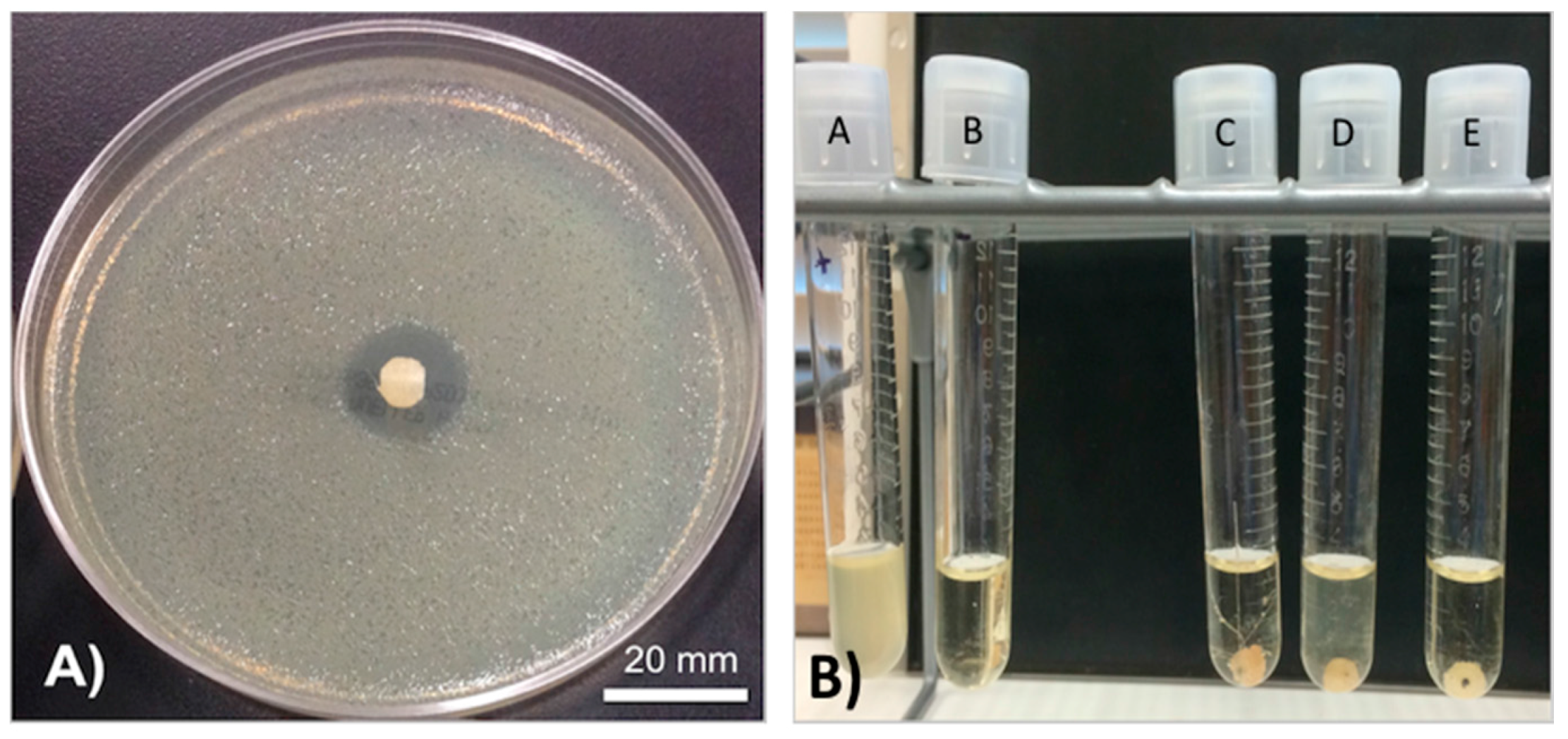
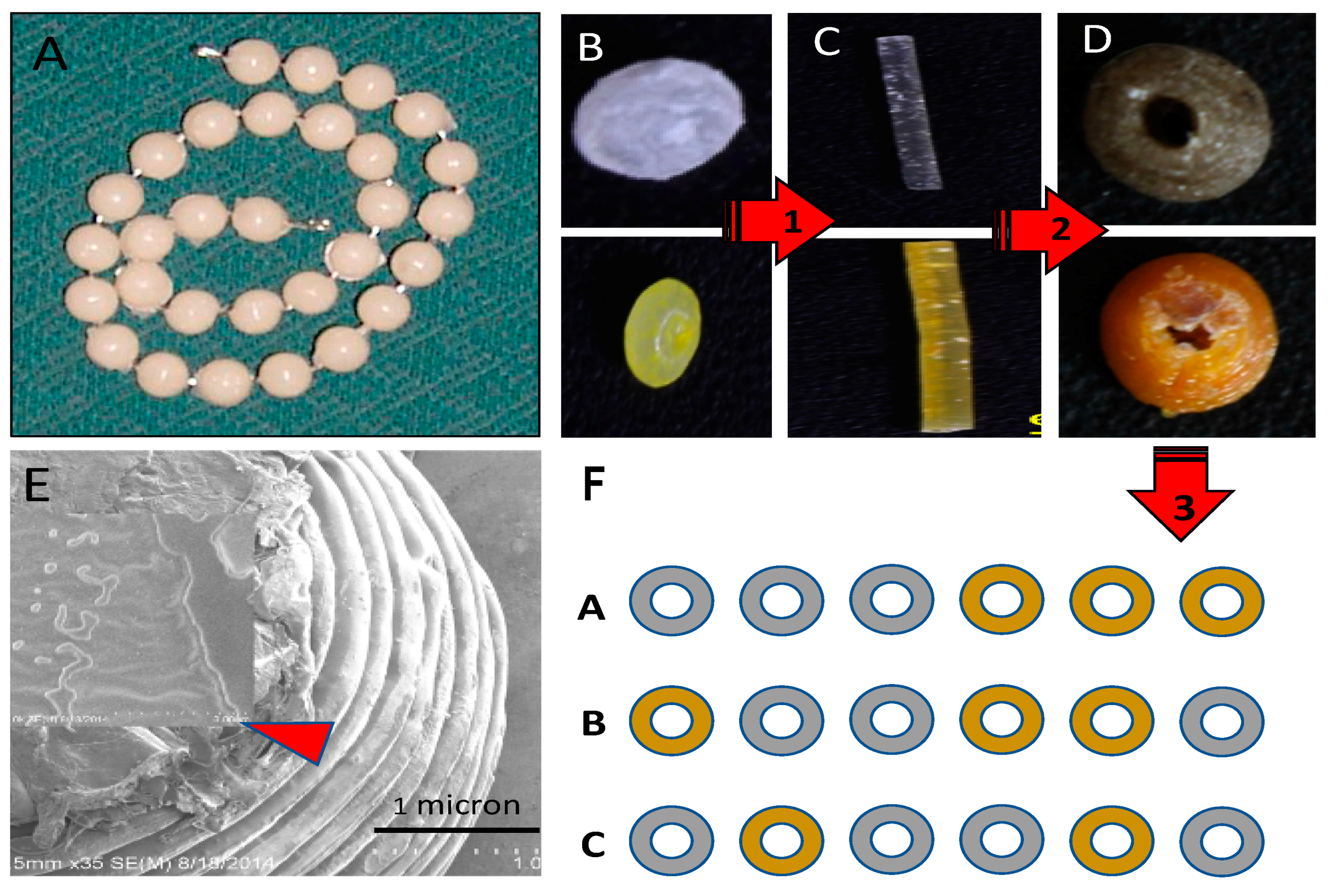
3.1. Fabrication of Antibacterial Disks and Filaments
3.2. SEM Analysis
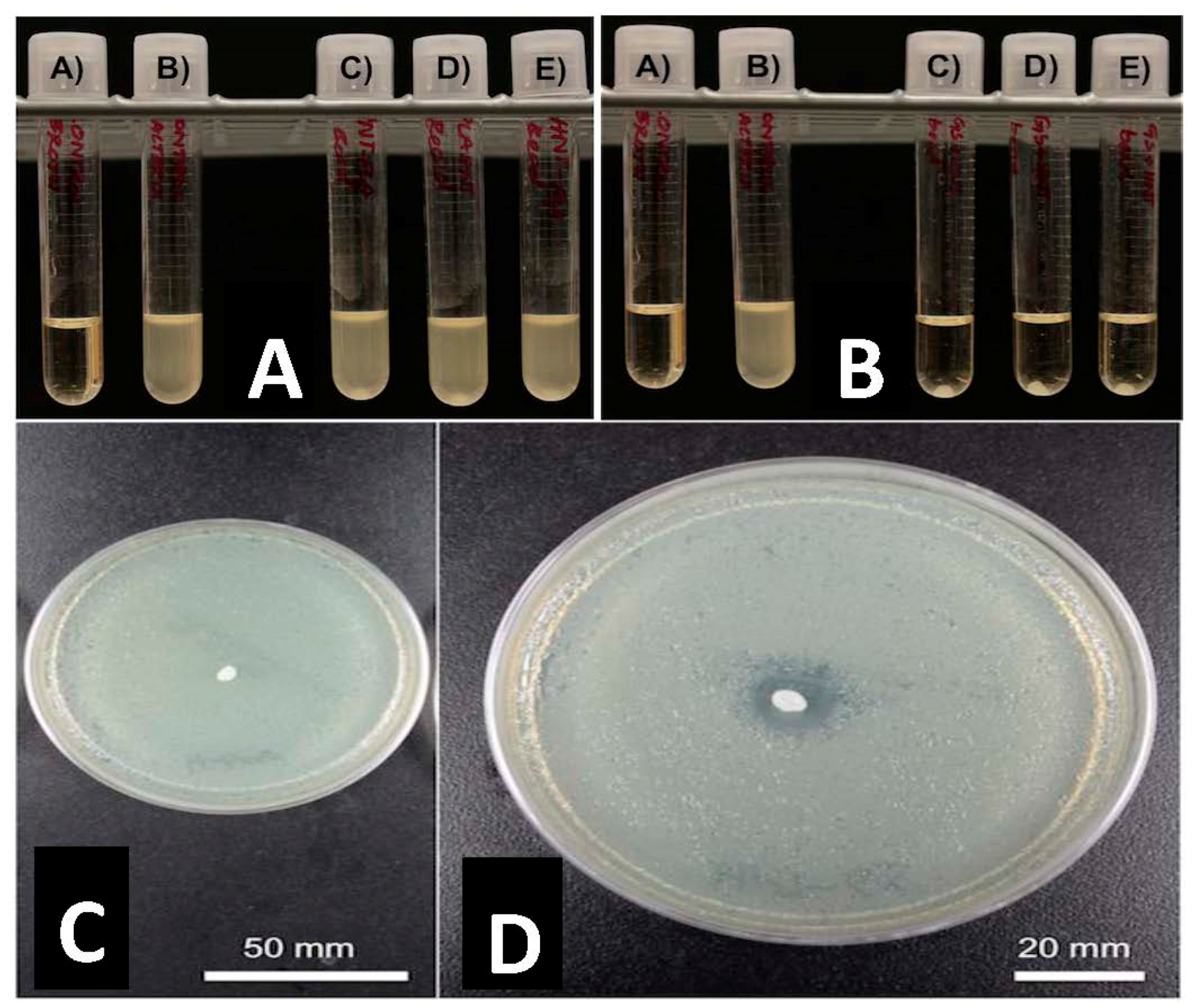
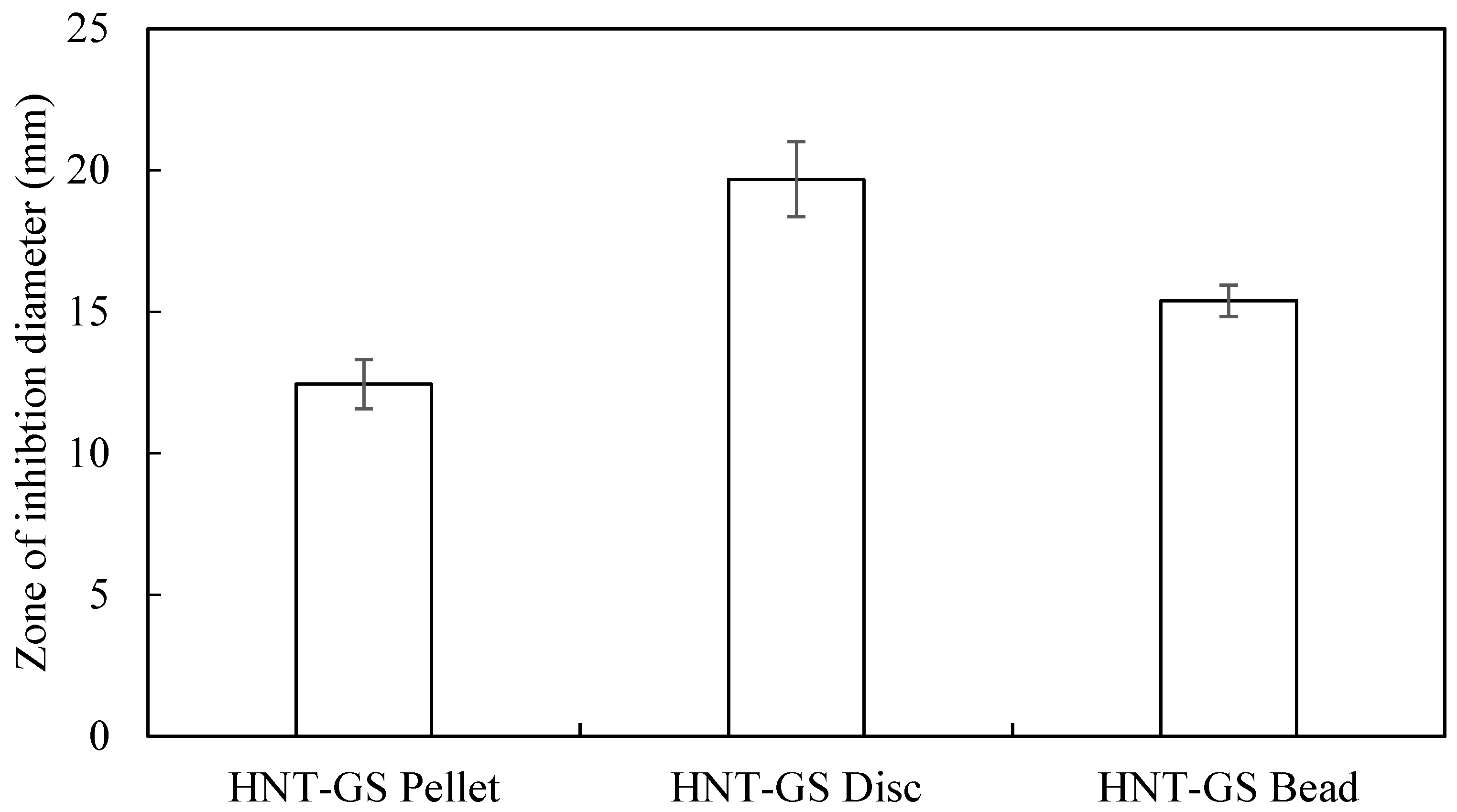
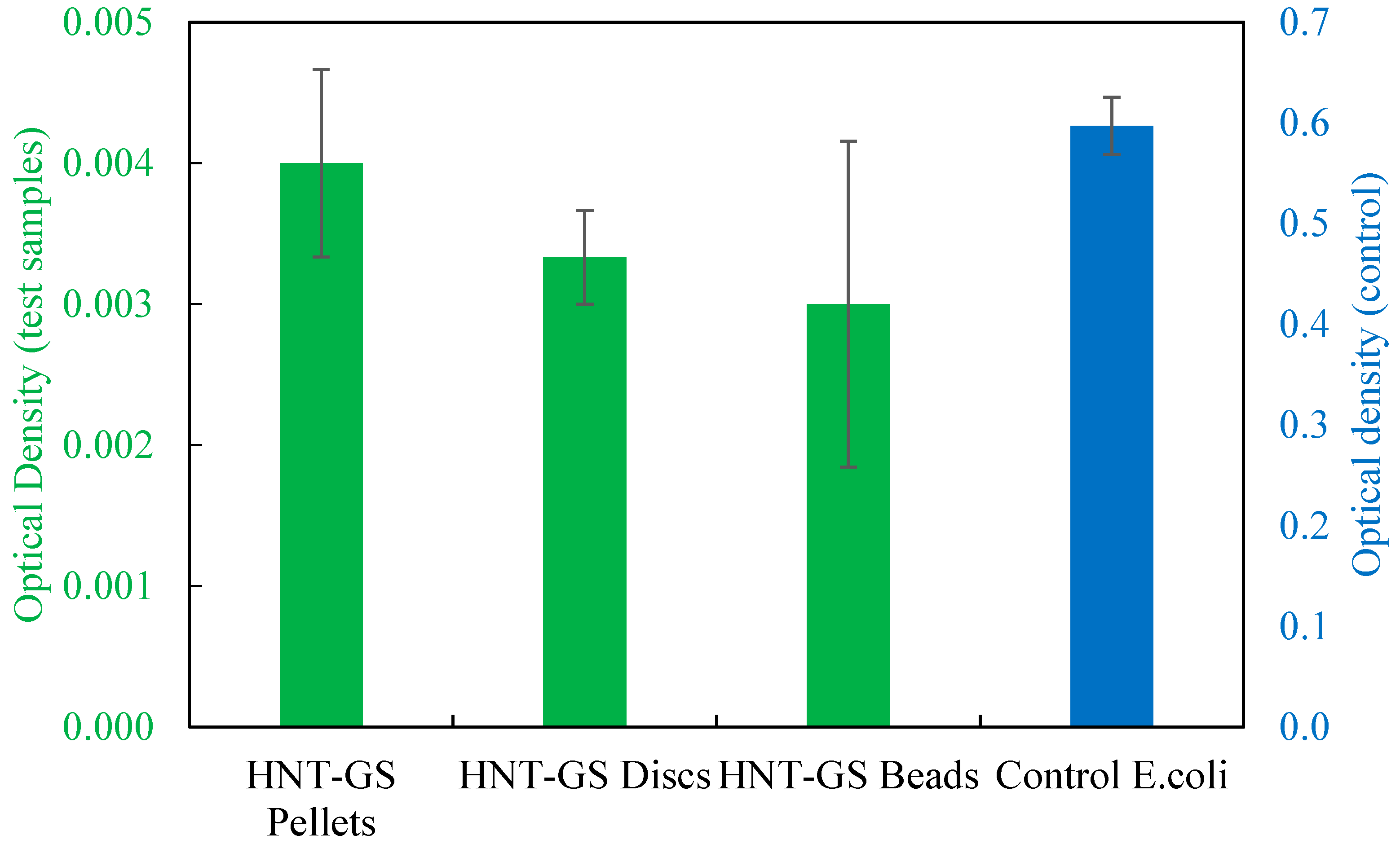
3.3. Growth Inhibition Studies
3.4. Drug Release Profile
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lew, D.P.; Waldvogel, F.A. Osteomyelitis. Lancet 2004, 364, 369–379. [Google Scholar] [CrossRef]
- Jorge, L.S.; Chueire, A.C.; Rossit, A.R. Osteomyelitis: A current challenge. Braz. J. Infect. Dis. 2010, 14, 310–315. [Google Scholar] [CrossRef]
- Sia, I.G.; Berbari, E.F. Osteomyelitis. Best Pract. Res. Clin. Rheumatol. 2006, 20, 1065–1081. [Google Scholar] [CrossRef] [PubMed]
- Hatzenbueler, J.; Oulling, T.J. Diagnosis and management of osteomyelitis. Am. Fam. Phys. 2011, 84, 1027–1033. [Google Scholar]
- Gomes, D.; Pereira, M.; Bettencourt, A.F. Osteomyelitis: An overview of antimicrobial therapy. Braz. J Pharm. Sci. 2013, 49, 13–17. [Google Scholar] [CrossRef]
- Dirschl, D.R.; Almekinders, L.C. Osteomyelitis: Common causes and treatment recommendations. Drugs 1993, 45, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Tuleubaev, T.; Saginov, D.; Abiyev, T.; Davletbaev, M.; Koshanova, A. Local antibiotic therapy of osteomyelitis using nonabsorbable implant. Georgian Med. News 2016, 255, 21–26. [Google Scholar]
- Kremers, H.M.; Nwojo, M.E.; Ransom, J.E.; Wood-Wentz, C.M.; Melton, L.J.; Huddleston, P.M. Trends in the Epidemiology of Osteomyelitis: A Population-Based Study, 1969 to 2009. J. Bone Jt. Surg. Am. Vol. 2015, 97, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.K.; Mukherjee, P.; Roy, S.; Kundi, B.; Kumar, D.; Basu, D. Local antibiotic delivery systems for the treatment of osteomyelitis—A review. Mater. Sci. Eng. C 2009, 29, 2478–2485. [Google Scholar] [CrossRef]
- Zimmerli, W. Infection and musculoskeletal conditions: Prosthetic-joint associated infections. Best Pract. Res. Clin. Rheumatol. 2006, 20, 1045–1063. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, B.A.; Berendt, A.R.; Cornia, P.B.; Pile, J.C.; Peters, E.J.G.; Armstrong, D.G.; Deery, H.G.; Embil, J.M.; Joseph, W.S.; Karchmer, A.W.; et al. Executive summary: 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin. Infect. Dis. 2012, 54, 1679–1684. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Age-Adjusted Hospital Discharge Rates for Non-Traumatic Lower Extremity Amputation per 1000 Diabetic Population, by Level of Amputation, United States, 1993–2009. 2010. Available online: http://www.cdc.gov/diabetes/statistics/lealevel/fig8.htm (accessed on 18 February 2017).
- Lavery, L.A.; Armstrong, D.G.; Wunderlich, R.P.; Mohler, M.J.; Wendel, C.S.; Lipsky, B.A. Risk factors for foot infections in individuals with diabetes. Diabetes Care 2006, 29, 1288–1293. [Google Scholar] [CrossRef] [PubMed]
- Steven, Y.; Tonga, C.; David, J.S.; Eichenberg, E.; Holland, T.L.; Fowler, V.G. Staphylococcus aureus Infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar]
- Hannan, C.M.; Attinger, C.E. Special Considerations in the Management of Osteomyelitis Defects (Diabetes, the Ischemic or Dysvascular Bed, and Irradiation). Semin. Plast. Surg. 2009, 23, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.K.; Bandyopadhyay, S.; Piyali, P.; Samanta, I.; Mukherjee, P.; Roy, S.; Kundu, B. Understanding osteomyelitis and its treatment through local drug delivery system. Biotechnol. Adv. 2016, 34, 1305–1317. [Google Scholar] [CrossRef] [PubMed]
- Melamed, E.A.; Peled, E. Antibiotic impregnated cement spacer for salvage of diabetic osteomyelitis. Foot Ankle Int. 2012, 33, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, K.; Kelm, J.; Regitz, T.; Schmitt, E.; Jung, W. In vitro evaluation of antibiotic release from and bacteria growth inhibition by antibiotic-loaded acrylic bone cement spacers. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 72B, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Thonse, R.; Conway, J.D. Antibiotic cement-coated nails for the treatment of infected nonunions and segmental bone defects. J. Bone Jt. Surg. Am. Vol. 2008, 90, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Campoccia, D.; Montanaro, D.; Speziale, P.; Arciola, C.R. Antibiotic-loaded biomaterials and the risks for the spread of antibiotic resistance following their prophylactic and therapeutic clinical use. Biomaterials 2010, 31, 6363–6377. [Google Scholar] [CrossRef] [PubMed]
- Gogia, J.A.; Meehan, J.P.; Ceasare, P.E.; Jamali, A.A. Local antibiotic therapy in osteomyelitis. Semin. Plast. Surg. 2009, 23, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Aderibigbe, B.; Aderibigbe, I.; Popoola, P. Design and biological evaluation of delivery systems containing bisphosphonates. Pharmaceutics 2017, 9. [Google Scholar] [CrossRef] [PubMed]
- Kaya, M.; Simsek-Kaya, G.; Gursan, N.; Kirecci, E.; Dayi, E.; Gundogdu, B. Local treatment of chronic osteomyelitis with surgical debridement and tigecycline-impregnated calcium hydroxyapatite: An experimental study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2011, 113, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Miayai, T.; Ito, A.; Tamazawa, G.; Matsuno, T.; Sogo, Y.; Nakamura, C.; Yamazaki, A.; Satoh, T. Antibiotic-loaded poly-ε-caprolactone and porous β-tricalcium phosphate composite for treating osteomyelitis. Biomaterials 2008, 29, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Walenkamp, G.H.I.M. Self-mixed antibiotic bone cement: Western countries learn from developing countries. Acta Orthop. 2009, 80, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Zhan, X.; Jia, W.; Gu, Y.; Xiao, W.; Liu, X.; Wang, D.; Zhang, C.; Huang, W.; Rahaman, M.N.; Day, D.E.; et al. Teicoplanin-loaded borate bioactive glass implants for treating chronic bone infection in a rabbit tibia osteomyelitis model. Biomaterials 2010, 31, 5865–5874. [Google Scholar] [CrossRef] [PubMed]
- Koort, J.K.; Suokas, E.; Veiranto, M.; Mäkinen, T.J.; Jalava, J.; Törmälä, P.; Aro, H.T. In vitro and in vivo testing of bioabsorbable antibiotic containing bone filler for osteomyelitis treatment. J. Biomed. Mater. Res. Part A 2006, 78, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Soundrapandian, C.; Datta, S.; Sa, B. Drug-eluting implants for osteomyelitis. Crit. Rev. Ther. Drug Carr. Syst. 2006, 24, 493–545. [Google Scholar] [CrossRef]
- Lindfors, N.C.; Hyvonen, P.; Nyyssonen, M.; Kirjavainen, M.; Kankare, J.; Gullichsen, E.; Salo, J. Bioactive glass S53P4 as bone graft substitute in treatment of osteomyelitis. Bone 2010, 47, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Mäikinen, T.J.; Veiranto, M.; Lankinen, P.; Moritz, N.; Jalava, J.; Törmälä, P.; Aro, H.T. In vitro and in vivo release of ciprofloxacin from osteoconductive bone defect filler. J. Antimicrob. Chemother. 2005, 56, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Liu, X.; Jia, W.; Zhang, C.; Huang, W.; Wang, J. Treatment of osteomyelitis and repair of bone defect by degradable bioactive borate glass releasing vancomycin. J. Control. Release 2009, 139, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Garvin, K.; Feschuk, C. Polylactide-polyglycolide antibiotic implants. Clin. Orthop. Relat. Res. 2005, 437, 105–110. [Google Scholar] [CrossRef]
- Tsourvakas, S. Local Antibiotic Therapy in the Treatment of Bone and Soft Tissue Infections; Selected Topics in Plastic Reconstructive Surgery; Danilla, S., Ed.; InTech: Rijeka, Crotia, 2012; ISBN 978-953-307-836-6. [Google Scholar]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. 2016, 15, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Gross, B.C.; Erkal, J.L.; Lockwood, S.Y.; Chen, C.; Spence, D.M. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal. Chem. 2014, 86, 3240–3253. [Google Scholar] [CrossRef] [PubMed]
- Farahani, R.D.; Dubé, M.; Therriault, D. Three-dimensional printing of multifunctional nanocomposites: Manufacturing techniques and applications. Adv. Mater. 2016, 28, 5794–5821. [Google Scholar] [CrossRef] [PubMed]
- Weisman, J.; Kaskas, N.; Green, A.H.; Ballard, D.; Ambrose, J.J.; Sun, L.; Mills, D.K. Three-dimensional printing of chemotherapeutic and antibiotic eluting fibers, seeds, and discs for localized drug delivery in cutaneous disease. J. Investig. Dermatol. 2015, 135, S87–S98. [Google Scholar]
- Ballard, D.H.; Weisman, J.A.; Jammalamadaka, U.; Tappa, K.; Alexander, S.; Griffen, F. Three-dimensional printing of bioactive hernia meshes: In vitro proof of principle. Surgery 2017, 161, 1479–1481. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Zheng, Q.; Sun, W.; Xu, H.; Yang, X. Levofloxacin implants with predefined microstructure fabricated by three-dimensional printing technique. Int. J. Pharm. 2007, 339, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Abdullayev, E.; Lvov, L. Halloysite clay nanotubes as a ceramic “skeleton” for functional biopolymer composites with sustained drug release. J. Mater. Chem. B 2013, 1, 2894–2903. [Google Scholar] [CrossRef]
- Zhang, Y.; Tang, A.; Yang, H.; Ouyanga, J. Applications and interfaces of halloysite nanocomposites. Appl. Clay Sci. 2016, 119, 8–17. [Google Scholar] [CrossRef]
- Joussein, E.; Petit, S.; Churchman, J.; Theng, B.; Righi, B.; Delvaux, B. Halloysite clay minerals: A review. Clay Min. 2005, 40, 383–426. [Google Scholar] [CrossRef]
- Price, R.; Gaber, B.; Lvov, Y. Release characteristics of tetracycline, khellin and NAD from halloysite: A cylindrical mineral for delivery of biologically active agents. J. Microencapsul. 2001, 18, 713–723. [Google Scholar] [PubMed]
- Sun, L.; Boyer, C.; Grimes, R.; Mills, D.K. Drug coated clay nanoparticles for delivery of chemotherapeutics. Curr. Nanosci. 2016, 12, 207–214. [Google Scholar] [CrossRef]
- Karnik, S.; Mills, D.K. Nanoenhanced hydrogel system with sustained release capabilities. J. Biomed. Mater. Res. Part A 2015, 103, 2416–2426. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Abdllayev, E.; Goeders, A.; Hollister, A.; Lvov, Y.; Mills, D.K. Clay nanotube/poly(methyl methacrylate) bone cement composite with sustained antibiotic release. Macromol. Mater. Eng. 2012, 297, 645–653. [Google Scholar] [CrossRef]
- Wu, W.; Cao, X.; Luo, J.; He, G.; Zhang, Y. Morphology, thermal, and mechanical properties of poly(butylene succinate) reinforced with halloysite nanotube. Polym. Compos. 2014, 35, 847–855. [Google Scholar] [CrossRef]
- Lecouvet, B.; Gutierrez, J.; Sclavons, M.; Bailly, C. Structure property relationships in polyamide 12/halloysite nanotube nanocomposites. Polym. Degrad. Stab. 2011, 96, 226–235. [Google Scholar] [CrossRef]
- Guo, B.; Chen, F.; Lei, Y.; Liu, X.; Wan, J.; Jia, D. Styrene-butadiene rubber/halloysite nanotubes nanocomposites modified by sorbic acid. Appl. Surf. Sci. 2009, 255, 7329–7336. [Google Scholar] [CrossRef]
- Zhang, J.; Ye, L. Halloysite–epoxy nanocomposites with improved particle dispersion through ball mill homogenisation and chemical treatment. Compos. Sci. Technol. 2009, 69, 2497–2505. [Google Scholar]
- Liu, M.; Zhang, Y.; Wu, C.; Xiong, S.; Zhou, C. Chitosan/halloysite nanotubes bionanocomposites: Structure, mechanical properties and biocompatibility. Int. J. Biol. Macromol. 2012, 51, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Jammalamadaka, U.; Sun, L.; Tappa, K.; Mills, D.K. Sustained Release of Antibacterial Agents from Doped Halloysite Nanotubes. Bioengineering 2016, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Jammalamadaka, U.; Tappa, K.; Mills, D. Osteoinductive Calcium Phosphate Clay Nanoparticle Bone Cements (CPCs) with Enhanced Mechanical Properties. In Proceedings of the 2014 36th Annual International IEEE Engineering in Medicine and Biology Conference, Chicago, IL, USA, 26–30 August 2014; Volume 759, pp. 1–4. [Google Scholar]
- Kelnar, I.; Kratochvíl, J.; Forteln, I.; Kaprálková, L.; Zhigunov, A.; Khunová, V.; Nevoralová, M. Effect of halloysite on structure and properties of melt-drawn PCL/PLA microfibrillar composites. Express Polym. Lett. 2016, 10, 381–393. [Google Scholar] [CrossRef]
- Sukeik, M.; Haddad, F.S. Two-stage procedure in the treatment of late chronic hip infections-spacer implantation. Int. J. Med. Sci. 2009, 6, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Romanò, C.L.; Logoluso, N.; Meani, E.; Romanò, D.; De Vecchi, E.; Vassena, C.; Drago, L. A comparative study of the use of bioactive glass S53P4 and antibiotic-loaded calcium-based bone substitutes in the treatment of chronic osteomyelitis: A retrospective comparative study. Bone Jt. J. 2014, 96-B, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, A.K.; Roberts, C.S. Indications for antibiotic cement nails. J. Orthop. Trauma 2009, 23, S26–S30. [Google Scholar] [CrossRef] [PubMed]
- Zilberman, M.; Elsner, J.J. Antibiotic-eluting medical devices for various applications. J. Control. Release 2008, 130, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Hake, M.E.; Young, H.; Hak, D.J.; Stahel, P.F.; Hammerberg, E.M.; Mauffrey, C. Local antibiotic therapy strategies in orthopaedic trauma: Practical tips and tricks and review of the literature. Injury 2015, 46, 1447–1456. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.L.; Li, Y.F.; Fang, T.L.; Zhou, J.; Li, X.L.; Wang, Y.C.; Dong, J. Vancomycin-loaded nano-hydroxyapatite pellets to treat MRSA-induced chronic osteomyelitis with bone defect in rabbits. Inflamm. Res. 2012, 61, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Schmidmaier, G.; Lucke, M.; Wildemann, B.; Haas, N.P.; Raschke, M. Prophylaxis and treatment of implant-related infections by antibiotic-coated implants: A review. Injury 2006, 37, S105–S112. [Google Scholar] [CrossRef] [PubMed]
- Kanellakopoulou, K.; Galanopoulos, I.; Soranoglou, V.; Tsaganos, T.; Tziortzioti, V.; Maris, I.; Papalois, A.; Giamarellou, H.; Giamarellos-Bourboulis, E.J. Treatment of experimental osteomyelitis caused by methicillin-resistant Staphylococcus aureus with a synthetic carrier of calcium sulphate (Stimulan®) releasing moxifloxacin. Int. J. Antimicrob. Agents 2009, 33, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Logoluso, N.; Drago, L.; Gallazzi, E.; George, DA.; Morelli, I.; Romanò, C.L. Calcium-based, antibiotic-loaded bone substitute as an implant coating: A pilot clinical study. J. Bone Jt Infect. 2016, 1, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Lalidou, F.; Kolios, G.; Drosos, G.I. Bone infections and bone graft substitutes for local antibiotic therapy. Surg. Technol. Int. 2014, 24, 353–362. [Google Scholar] [PubMed]
- Marques, M.R.; Loebenberg, R.; Almukainzi, M. Simulated biologic fluids with possible application in dissolution testing. Dissolution Technol. 2011, 18, 15–28. [Google Scholar] [CrossRef]
- Ventola, C.L. Medical applications for 3D printing: Current and projected uses. Pharm. Therap. 2014, 39, 702–711. [Google Scholar]
- Zadpoor, A.A.; Malda, J. Additive manufacturing of biomaterials, tissues, and organs. Ann. Biomed. Eng. 2016, 45, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gbureck, U.; Vorndran, E.; Müller, F.A.; Barralet, J.E. Low temperature direct 3D printed bioceramics and biocomposites as drug release matrices. J. Control. Release 2007, 122, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.G.; Branford-White, C.; Yang, Y.C.; Zhu, L.; Welbeck, E.W.; Yang, X. A novel fast disintegrating tablet fabricated by three-dimensional printing. Drug Dev. Ind. Pharm. 2009, 35, 1530–1536. [Google Scholar] [CrossRef] [PubMed]
- Katstra, W.E.; Palazzolo, R.D.; Rowe, C.W.; Giritlioglu, B.; Teung, P.; Cima, M.J. Oral dosage forms fabricated by three-dimensional printing. J. Control. Release 2000, 66, 1–9. [Google Scholar] [CrossRef]
- Fukushima, K.; Tabuani, D.; Camino, G. Nanocomposites of PLA and PCL based on montmorillonite and Sepiolite. Mater. Sci. Eng. C 2009, 29, 1433–1441. [Google Scholar] [CrossRef]
- Rhim, J.W.; Hong, S.; Ha, C.S. Tensile, water vapor barrier and antimicrobial properties of PLA/nanoclay composite films. Food Sci. Technol. 2009, 42, 612–617. [Google Scholar] [CrossRef]
- Dong, Y.; Marshall, J.; Haroosh, H.J.; Mohammadzadehmoghadama, S.; Liu, D.; Xiaowen, Q.; Lau, K.T. Polylactic acid (PLA)/halloysite nanotube (HNT) composite mats: Influence of HNT content and modification. Compos. Part A Appl. Sci. Manuf. 2015, 76, 28–36. [Google Scholar] [CrossRef]
- Gaaz, T.; Sulong, A.; Kadhum, A.; Al-Amiery, A.; Nassir, M.; Jaaz, A. The impact of halloysite on the thermo-mechanical properties of polymer composites. Molecules 2017, 22, 838. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhang, Y.; Zhou, C. Nanocomposites of halloysite and polylactide. Appl. Clay Sci. 2013, 52, 75–76. [Google Scholar]
- De Silva, R.T.; Soheilmoghaddam, M.; Goh, K.; Wahit, M.U.; Hamid, S.; Chai, S.P.; Pasbakhsh, P. Influence of the processing methods on the properties of poly(lactic acid)/halloysite nanocomposites. Polym. Compos. 2014, 37, 861–869. [Google Scholar] [CrossRef]
- De Silva, R.; Pasbakhsh, P.; Goh, K.; Chai, S.-P.; Chen, J. Synthesis and characterisation of poly(lactic acid)/halloysite bionanocomposite films. J. Compos. Mater. 2013, 48, 3705–3717. [Google Scholar] [CrossRef]
- Jeffery, A.W. Nanotechnology and Additive Manufacturing Platforms for Clinical Medicine: An Investigation of 3D Printing Bioactive Constructs and Halloysite Nanotubes for Drug Delivery and Biomaterials; Louisiana Tech University; ProQuest Dissertations Publishing: Ruston, LA, USA, 2014; Volume 287, p. 3662483. [Google Scholar]
- Mills, D.K. Future Medicine: The Impact of 3D Printing. J. Nanomater. Mol. Nanotechnol. 2015, 4, 1–3. [Google Scholar] [CrossRef]
- Kim, S.B.; Kim, Y.J.; Yoon, T.L.; Park, S.A.; Cho, I.H.; Kim, E.J.; Kim, I.A.; Shin, J. The characteristics of a hydroxyapatite-chitosan-PMMA bone cement. Biomaterials 2014, 25, 5715–5723. [Google Scholar] [CrossRef] [PubMed]
- Virto, M.R.; Frutos, P.; Torrado, S.; Frutos, G. Gentamicin release from modified acrylic bone cements with lactose and hydroxypropylmethylcellulose. Biomaterials 2003, 24, 79–87. [Google Scholar] [CrossRef]
- Van de Belt, H.; Neut, D.; Schenk, W.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J. Gentamicin release from polymethylmethacrylate bone cements and Staphylococcus aureus Biofilm Formation. Acta Orthop. Scand. 2000, 71, 625–629. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weisman, J.A.; Jammalamadaka, U.; Tappa, K.; Mills, D.K. Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices. Bioengineering 2017, 4, 96. https://doi.org/10.3390/bioengineering4040096
Weisman JA, Jammalamadaka U, Tappa K, Mills DK. Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices. Bioengineering. 2017; 4(4):96. https://doi.org/10.3390/bioengineering4040096
Chicago/Turabian StyleWeisman, Jeffery A., Udayabhanu Jammalamadaka, Karthik Tappa, and David K. Mills. 2017. "Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices" Bioengineering 4, no. 4: 96. https://doi.org/10.3390/bioengineering4040096