Leaner, Healthier, Happier Together––A Family-Centred Approach to Weight Loss with the Overweight Dog and Her Caregivers
Abstract
:1. Introduction
2. Signalment, History and Assessments
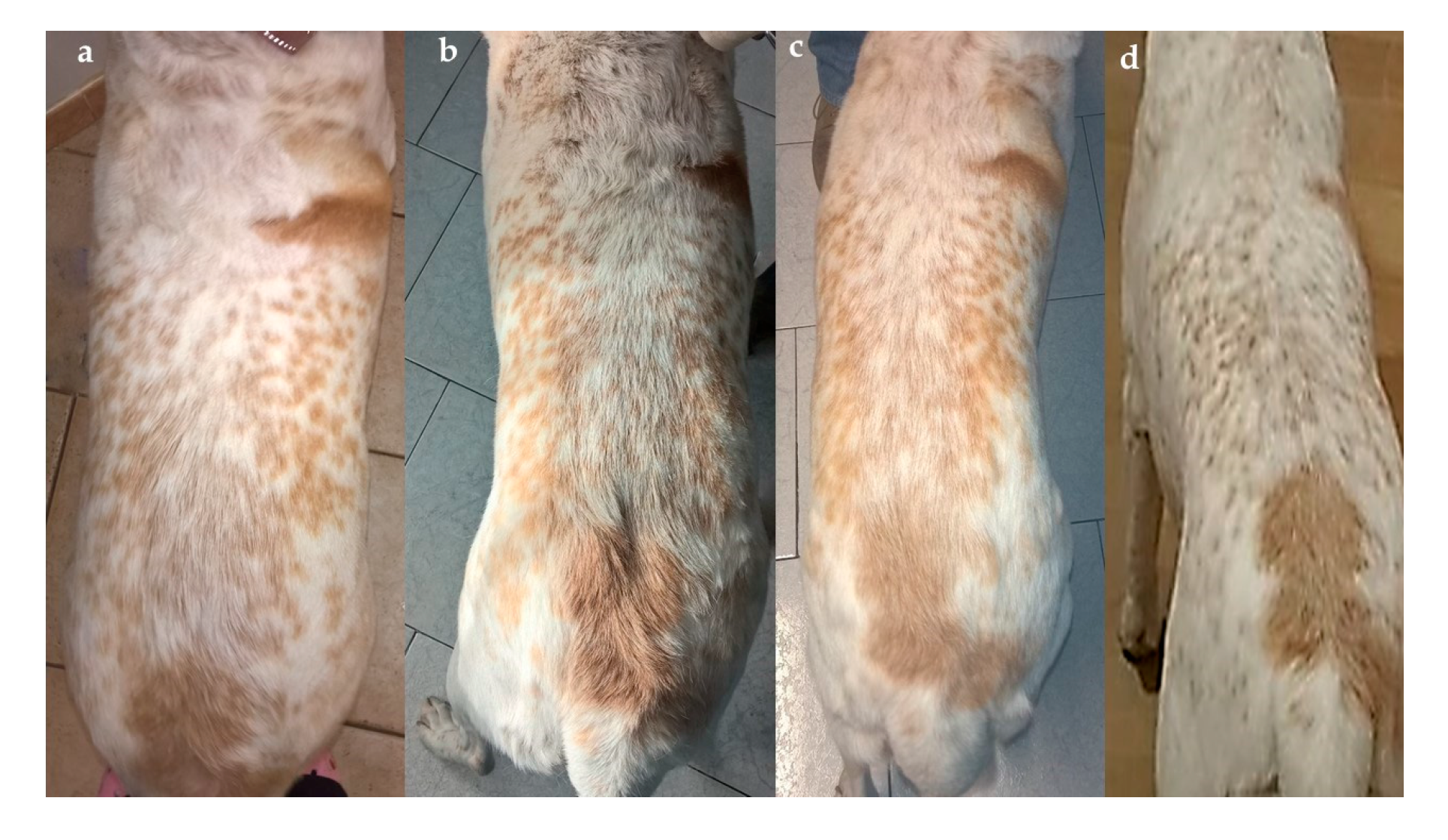
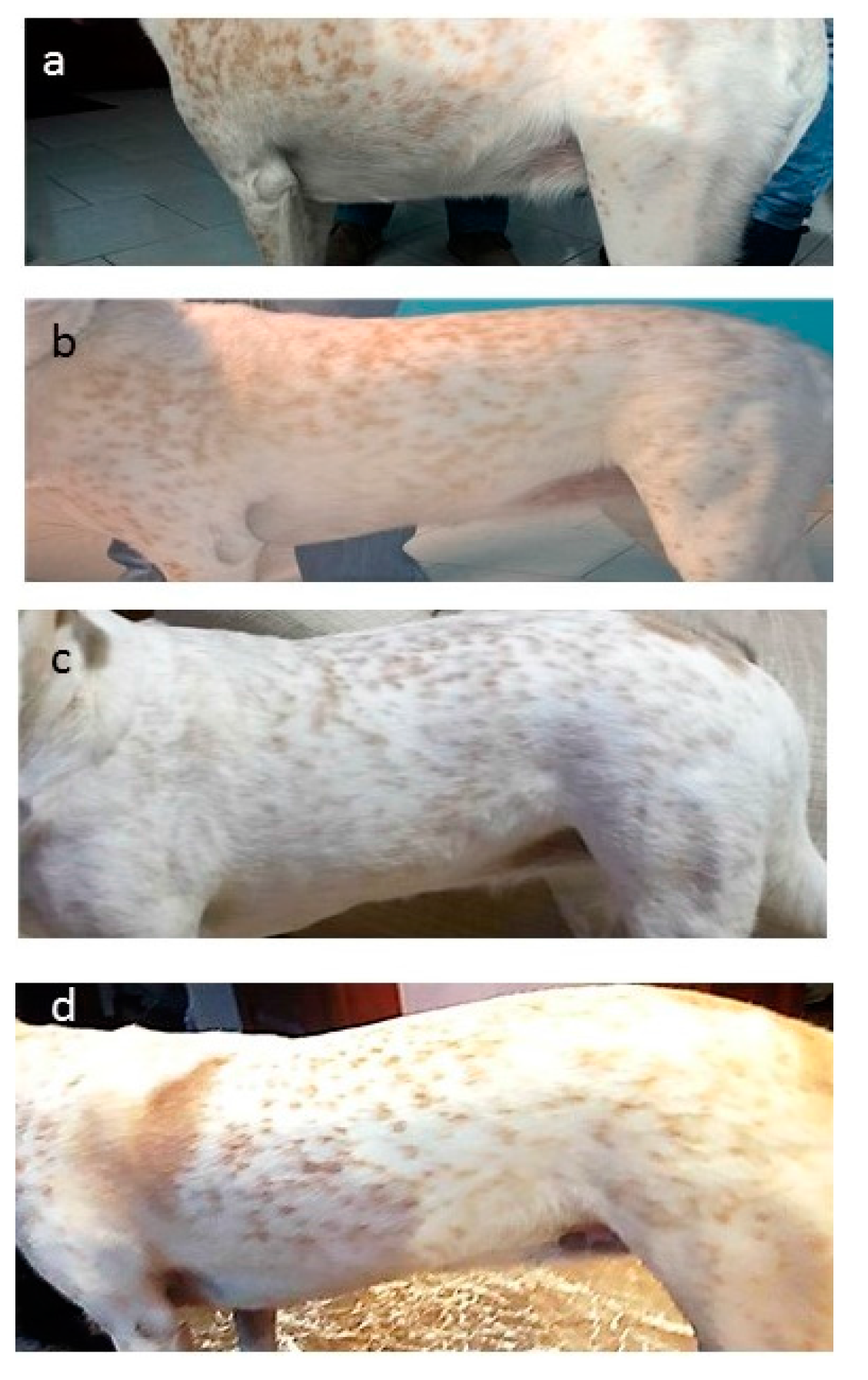
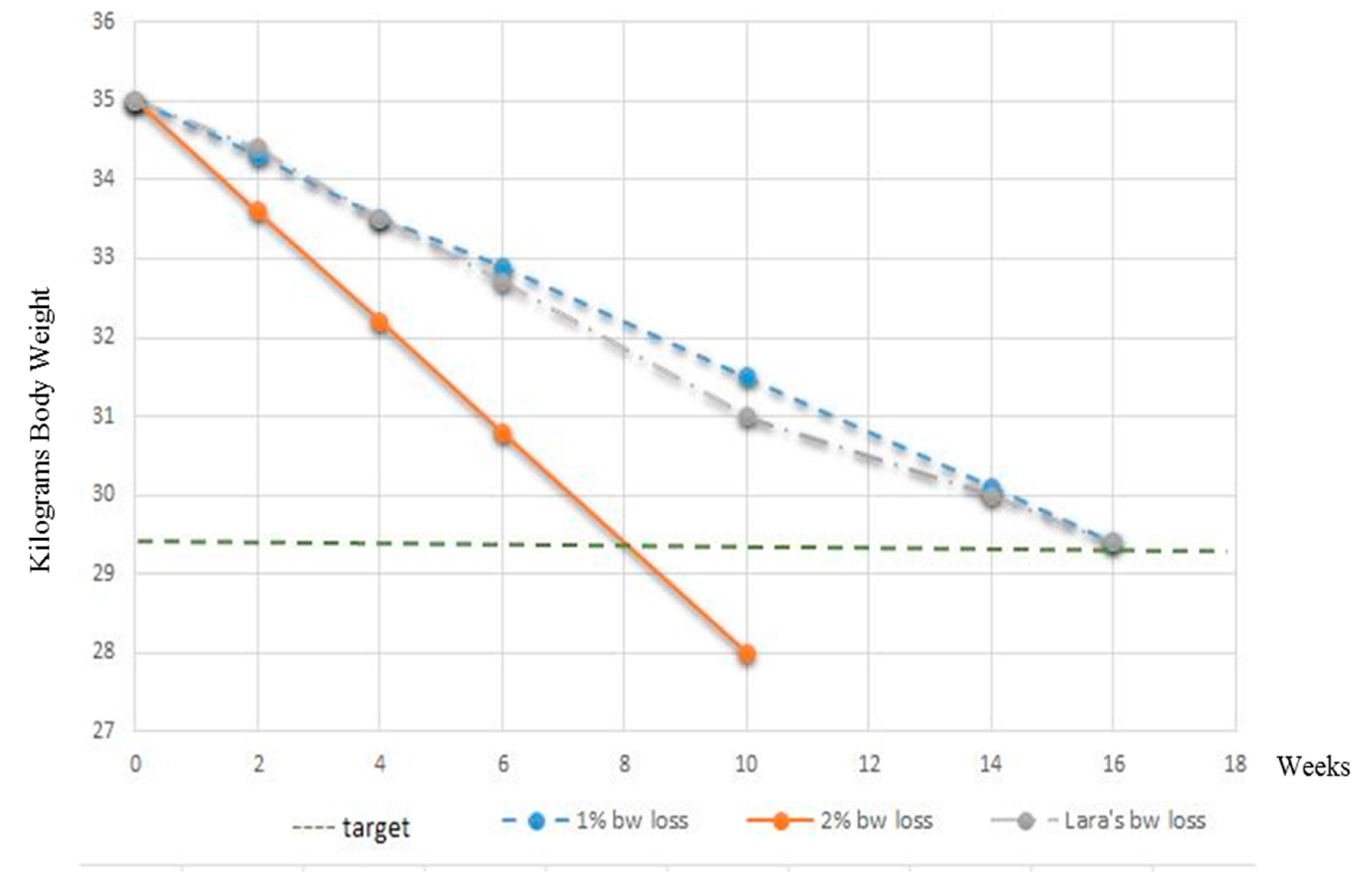
3. Results
4. Diagnosis, Treatment and Follow-Up
- (1)
- (2)
- Implementing physical activity by scheduling a daily-based work-out.
- (3)
- Directly involving all caregivers through communicating a family-centred approach targeted towards monitoring the effectiveness of the weight loss programme, and increasing their awareness on how treats and any extra calories would negatively influence the outcome.
5. Discussion
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sandøe, P.; Palmer, C.; Corr, S.; Astrup, A.; Reinhard Bjørnvad, C. Canine and feline obesity: A One Health perspective. Vet. Rec. 2014, 20, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Day, M.J. One Health approach to preventing obesity in people and their pets. J. Comp. Path. 2017, 150, 293–295. [Google Scholar] [CrossRef] [PubMed]
- White, G.A.; Ward, L.; Pink, C.; Craigon, J.; Millar, K.M. Who’s been a good dog?––Owner perceptions and motivations for treat giving. Prev. Vet. Med. 2016, 132, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, E.; Birch, L.; Endenburg, N.; German, A.J.; Neilson, J.; Seligmann, H.; Takashima, G.; Day, M.J. The financial costs, behavior and psychology of obesity: A One Health analysis. J. Comp. Path. 2017, 156, 310–325. [Google Scholar] [CrossRef] [PubMed]
- Chandler, M.; Cunningham, S.; Lund, E.M.; Khanna, C.; Naramore, R.; Patel, A.; Day, M.J. Obesity and associated comorbidities in people and companion animals: A One Health perspective. J. Comp. Path. 2017, 156, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Churchill, J.; Ward, E. Communicating with pet owners about obesity. Roles of the veterinary health care team. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 899–911. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.A.; Villaverde, C. Scope of the problem and perception by owners and veterinarian. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 761–772. [Google Scholar] [CrossRef] [PubMed]
- Toll, P.W.; Yamka, R.M.; Schoenherr, W.D.; Hand, M.S. Obesity. In Small Animal Clinical Nutrition, 5th ed.; Hand, M.S., Thatcher, C.D., Remillard, R.L., Roudebusch, P., Novotny, B.J., Eds.; Mark Morris Institute: Topeka, KS, USA, 2010; pp. 501–542. [Google Scholar]
- Health Implications of Obesity. NIH Consensus Statement Online 1985. Available online: https://consensus.nih.gov/1985/1985Obesity049html.htm (accessed on 5 February 2017).
- Armstrong, P.J.; Lund, E.M. Changes in body composition and energy balance with aging. Vet. Clin. Nutr. 1996, 3, 83–87. [Google Scholar]
- Lund, E.M.; Armstrong, P.J.; Kirk, C.A.; Klausner, J.S. Prevalence and risks factors for obesity in adult dogs from private US veterinary practices. Int. J. Appl. Res. Vet. Med. 2006, 4, 177–186. [Google Scholar]
- Lund, E.M.; Armstrong, P.J.; Kirk, C.A.; Klausner, J.S. Prevalence and risks factors for obesity in adult cats from private US veterinary practices. Int. J. Appl. Res. Vet. Med. 2005, 3, 88–95. [Google Scholar]
- Brooks, D.; Churchill, J.; Fein, K.; Linder, D.; Michel, K.E.; Tudor, K.; Ward, E.; Witzel, A. American Animal Hospital Association. AAHA weight management guidelines for dogs and cats. J. Am. Anim. Hosp. Assoc. 2014, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kealy, R.D.; Lawler, D.F.; Ballam, J.M.; Mantz, S.L.; Biery, D.N.; Greeley, E.H.; Lust, G.; Segre, M.; Smith, G.K.; Stowe, H.D. Effect of diet restriction on life span and age related changes in dogs. J. Am. Vet. Med. Assoc. 2002, 220, 1315–1320. [Google Scholar] [CrossRef] [PubMed]
- White, G.A.; Hobson-West, P.; Cobb, K.; Craigon, J.; Hammond, R.; Millar, K.M. Canine obesity: Is there a difference between veterinarian and owner perception? J. Small Anim. Pract. 2011, 52, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Laflamme, D.; Sidebottom-Nielsen, M. Owner perception of canine body condition score. J. Vet. Intern. Med. 2002, 16, 362. [Google Scholar]
- MacMartin, C.; Wheat, H.; Coe, J.; Adams, C.L. Effect of question design on dietary information solicited during veterinarian-client interactions in companion animal practice in Ontario, Canada. J. Am. Vet. Med. Assoc. 2015, 246, 1203–1213. [Google Scholar] [CrossRef] [PubMed]
- Morrisey, J.K.; Voiland, B. Difficult interactions with veterinary clinics: Working in the challenging zone. Vet. Clin. N. Am. Small Anim. Pract. 2007, 37, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Bartges, J.; Kushner, R.F.; Michel, K.E.; Sallis, R.; Day, M.J. One Health solutions to obesity in people and their pets. J. Comp. Pathol. 2017, 156, 326–333. [Google Scholar] [PubMed]
- Hamper, B. Current topics in canine and feline obesity. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Schauf, S.; Salas-Mani, A.; Torre, C.; Bosch, G.; Swarts, H.; Castrillo, C. Effect of sterilization and of dietary fat and carbohydrate content on food intake, activity level, and blood satiety–related hormones in female dogs. J. Anim. Sci. 2016, 94, 4239–4250. [Google Scholar] [CrossRef] [PubMed]
- Day, M. One Health: The small animal dimension. Vet. Rec. 2010, 167, 847–849. [Google Scholar] [CrossRef] [PubMed]
- WSAVA Nutrition toolkit. Available online: http://www.wsava.org/nutrition-toolkit (accessed on 1 February 2016).
- Gant, P.; Holden, S.L.; Biourge, V.; German, A.J. Can you estimate body composition in dogs from photographs? BMC Vet. Res. 2016, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Eukanuba Veterinary Diet Restricted Calorie for Dogs, Spectrum Brands, Enterprise House, West Byfleet, Surrey, United Kingdom. Available online: http://www.eukanuba.eu/products/for-dogs/eukanuba-veterinary-diets-restricted-calorie-for-dogs (accessed on 16 August 2017).
- WALTHAM S.H.A.P.E.TM System for Dogs. Available online: https://www.waltham.com/document/nutrition/dog/dog-body-weight-management/273/ (accessed on 16 August 2017).
- German, A.J.; Holden, S.L.; Wiseman-Orr, M.L.; Reid, J.; Nolan, A.M.; Biourge, V.; Morris, P.J.; Scott, E.M. Quality of life is reduced in obese dogs but improves after successful weight loss. Vet. J. 2012, 192, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Eukanuba Adult Weight Control, Large Breed (Spectrum Brands, Enterprise House, West Byfleet, Surrey, United Kingdom). Available online: http://www.eukanuba.eu/products/for-dogs/eukanuba-adult-dry-dog-food-weight-control-for-large-breed,-chicken (accessed on 16 August 2017).
- German, A.J.; Holden, S.L.; Mather, N.J.; Morris, P.J.; Biourge, V. Low maintenance energy requirements of dogs after weight loss. Br. J. Nutr. 2011, 106, S93–S96. [Google Scholar] [CrossRef]
- National Research Council (NRC). Energy. In Nutrient Requirements of Dogs and Cats; The National Academies Press: Washington, DC, USA, 2006; pp. 28–48. [Google Scholar]
- German, A.J.; Holden, S.L.; Morris, P.J.; Biourge, V. Long-term follow-up after weight management in obese dogs: The role of diet in preventing regain. Vet. J. 2012, 192, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Klimentidis, Y.C.; Beasley, T.M.; Lin, H.Y.; Murati, G.; Glass, G.E.; Guyton, M.; Newton, W.; Jorgensen, M.; Heymsfield, S.B.; Kemnitz, J.; et al. Canaries in the coal mine: A cross-species analysis of the plurality of obesity epidemics. Proc. Biol. Sci. 2016, 278, 1626–1632. [Google Scholar] [CrossRef] [PubMed]
- Holst, B.S.; Gustavsson, M.H. Animal obesity: Causes, consequences and comparative aspects. Acta Vet. Scand. 2016, 58, 56. [Google Scholar] [CrossRef] [PubMed]
- Weeth, L.P. Other risks/Possible benefits of obesity. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.; Hoenig, M. Metabolic effects of obesity and its interaction with endocrine diseases. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 797–815. [Google Scholar] [CrossRef] [PubMed]
- Courcier, E.A.; Mellor, D.J.; Thomson, R.M. A cross sectional study of the prevalence and risk factors for owner misperception of canine body shape in first opinion practice in Glasgow. Prev. Vet. Med. 2011, 102, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Paul, I.M.; Williams, J.S.; Anzman-Frasca, S.; Beiler, J.S.; Makova, K.D.; Marini, M.E.; Hess, L.B.; Rzucidlo, S.E.; Verdiglione, N.; Mindell, J.A.; et al. The intervention nurses start infants growing on healthy trajectories (INSIGHT) study. BMC Pediatr. 2014, 14, 184. [Google Scholar] [CrossRef] [PubMed]
- Eirmann, L. Nutritional Assessment. Vet. Clin. N. Am. Small Anim. Pract. 2016, 46, 855–867. [Google Scholar] [CrossRef] [PubMed]
- Kushner, R.F.; Blatner, D.J.; Jewell, D.E.; Rudloff, K. The PPET Study: People and pets exercising together. Obesity 2006, 14, 1762–1770. [Google Scholar] [CrossRef] [PubMed]
| Patient Assessment | At Admission | After 2 Weeks | After 4 Weeks | After 6 Weeks | After 10 Weeks | After 14 Weeks | After 16 Weeks | |
|---|---|---|---|---|---|---|---|---|
| Mentation | QAR | QAR | BAR | BAR | BAR | BAR | BAR | |
| Weight (kg) | 35 | 34.4 | 33.5 | 32.7 | 31 | 30 | 29.5 | |
| BCS (1–9) | 7–7.5 | 7 | 6.5 | 6 | 5.5 | 5.5 | 5.0 | |
| MMI | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| Morphometric measurements (cm): | ||||||||
| “Hock to stifle” (HS) | 24.5 | - | - | - | - | - | - | |
| Pelvic circumference (cms) | 76 | 74 | 71.8 | 70.2 | 69.5 | 68 | 67.3 | |
| Rectal temperature (Celsius degree) | 38.6 | 38.3 | 38.8 | 38.7 | 38.3 | 38.5 | 38.6 | |
| RR (bpm) | 26 | 24 | 25 | 22 | 24 | 22 | 20 | |
| HR (bpm) | 82 | 80 | 79 | 84 | 80 | 81 | 80 | |
| CRT (s) | <2 | <2 | <2 | <2 | <2 | <2 | <2 | |
| Mucous membranes | pink | pink | pink | pink | pink | pink | pink | |
| Hydration | adequate | adequate | adequate | adequate | adequate | adequate | adequate | |
| Peripheral lymph nodes | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| CV | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| EENT | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| GI | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| GU | wnl | wnl | wnl | wnl | wnl | wnl | wnl | |
| INTEG | wnl, with the exception of a focal exfoliative dermatitis in the back region | wnl. No signs of dermatitis | wnl | wnl | wnl | wnl | wnl | |
| M/S | Lethargy and reluctance to walk reported by the owner. Occasional stiffness, especially while climbing stairs. No musculo-skeletal abnormalities detected during physical examination | Lethargy and reluctance to walk still reported, but reduced in severity and frequency | Increased mobility. Climbing stairs became easier. | No problem in climbing stairs. The dog is more active and playful | No problem in climbing stairs. The dog is more active | No problem in climbing stairs. The dog is more active and playful | No problem in climbing stairs. The dog is more active and playful | |
| NERV | wnl | wnl | wnl | wnl | wnl | wnl | wnl | wnl |
| RESP | wnl | wnl | wnl | wnl | wnl | wnl | wnl | wnl |
| Haemato-Biochemical Parameters | At Admission | After 16 Weeks | Reference Range |
|---|---|---|---|
| WBC (×103/μL) | 16.2 | 14.3 | 6.0–17.0 |
| RBC (×106/μL) | 6.5 | 6.8 | 5.5–8.5 |
| HGB (g/dL) | 13.7 | 14.2 | 11.0–19.0 |
| HCT (%) | 46 | 47 | 39.0–56.0 |
| PLT(×103/μL) | 311 | 386 | 117–460 |
| BUN (mg/dL) | 22 | 23 | 7–25 |
| CREA (mg/dL) | 1.1 | 1.0 | 0.3–1.4 |
| Total bilirubin (mg/dL) | 0.3 | 0.2 | 0.1–0.6 |
| Total proteins (g/dL) | 7.3 | 7.7 | 5.4–8.2 |
| Albumin (g/dL) | 3.8 | 3.9 | 2.5–4.4 |
| Globulin (g/dL) | 3.5 | 3.8 | 2.3–5.2 |
| ALT (IU/L) | 46 | 39 | 10–118 |
| ALP (IU/L) | 24 | 32 | 20–150 |
| Cholesterol (mg/dL) | 350 | 200 | 130–370 |
| Triglyceride (mg/dL) | 98 | 57 | 10–100 |
| Calcium (mg/dL) | 10.9 | 10.8 | 8.6–11.8 |
| Phosphorus (mg/dL) | 5.2 | 4.7 | 2.9–6.6 |
| Sodium (mEq/L) | 147 | 152 | 138–160 |
| Potassium (mEq/L) | 5.6 | 5.0 | 3.7–5.8 |
| Urinalysis * | At admission | After 16 weeks | Reference range |
| pH | 6.5 | 6.0 | 5.5–7.5 |
| Specific gravity | 1.035 | 1.045 | 1.001–1.050 |
| Colour | Amber yellow | Amber yellow | / |
| Turbidity | Transparent | Transparent | / |
| Protein | Traces | Absent | ≤10 mg/dL |
| Glucose | Negative | Negative | Negative |
| Ketones | Negative | Negative | Negative |
| Sediment (Casts, WBC, RBC, cells, crystals, bacteria) | Unremarkable, except from Cocci/few (due to contamination at collection) | Unremarkable | / |
| Thyroid function | At admission | After 16 weeks | Reference range |
| Free T4 (pmol/L) | 27 | 33 | 15–45 |
| Total T4 (µg/dL) | 1.8 | 2.1 | 1.0–4.0 |
| TSH (ng/mL) | <0.5 | Not performed | <0.5 |
| Nutrient | Canine Dry Food | Canine Canned Food |
|---|---|---|
| Water | 8.00% | 77.00% |
| Protein | 28.80% | 8.00% |
| Fat content | 8.00% | 4.50% |
| Omega-6 fatty acids | 1.50% | 0.62% |
| Omega-3 fatty acids | 0.20% | 0.12% |
| Crude ash | 6.70% | 1.60% |
| Crude Fibres | 2.10% | 0.50% |
| Calcium | 1.20% | 0.25% |
| Phosphorus | 1.00% | 0.20% |
| Vitamin A | 70,000 IU/kg | 18,000 IU/kg |
| Vitamin D3 | 900 IU/kg | 300 IU/kg |
| Vitamin E (α-tocopherol) | 100 mg/kg | 50 mg/kg |
| L-carnitine | 50 mg/kg | 10 mg/kg |
| Glucosamine * | 475 mg/kg | - |
| Chondroitin sulphate * | 45 mg/kg | - |
| Fibre source | Beet pulp | Beet pulp |
| Energy Kcal/Kg (calculated with modified Atwater) | 3334 | 1009 |
| After 4 Weeks | After 8 Weeks | After 12 Weeks | After 16 Weeks | |
|---|---|---|---|---|
| Results of WALTHAM S.H.A.P.E.TM | Score F | Score E | Score D | Score D |
| Descriptor Items | At the Beginning of the Weight Loss Programme | At the End of the 16-Week Weight Loss Programme | Reference Range |
|---|---|---|---|
| Level of spontaneous physical activity, directly related to physical wellness | 3 | 5 | 0–6 |
| Level of happiness, directly related to emotional wellness | 4 | 6 | 0–6 |
| Level of vitality, directly related to overall wellness | 2 | 5 | 0–6 |
| Level of anxiety, directly related to emotional disturbance | 5 | 5 | 0–6 |
| Level of food request, directly related to hunger and satiety | 6 | 4 | 0–6 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Candellone, A.; Morgan, D.; Buttignol, S.; Meineri, G. Leaner, Healthier, Happier Together––A Family-Centred Approach to Weight Loss with the Overweight Dog and Her Caregivers. Vet. Sci. 2017, 4, 41. https://doi.org/10.3390/vetsci4030041
Candellone A, Morgan D, Buttignol S, Meineri G. Leaner, Healthier, Happier Together––A Family-Centred Approach to Weight Loss with the Overweight Dog and Her Caregivers. Veterinary Sciences. 2017; 4(3):41. https://doi.org/10.3390/vetsci4030041
Chicago/Turabian StyleCandellone, Alessia, David Morgan, Simona Buttignol, and Giorgia Meineri. 2017. "Leaner, Healthier, Happier Together––A Family-Centred Approach to Weight Loss with the Overweight Dog and Her Caregivers" Veterinary Sciences 4, no. 3: 41. https://doi.org/10.3390/vetsci4030041





