Prostate Cancer: Is It a Battle Lost to Age?
Abstract
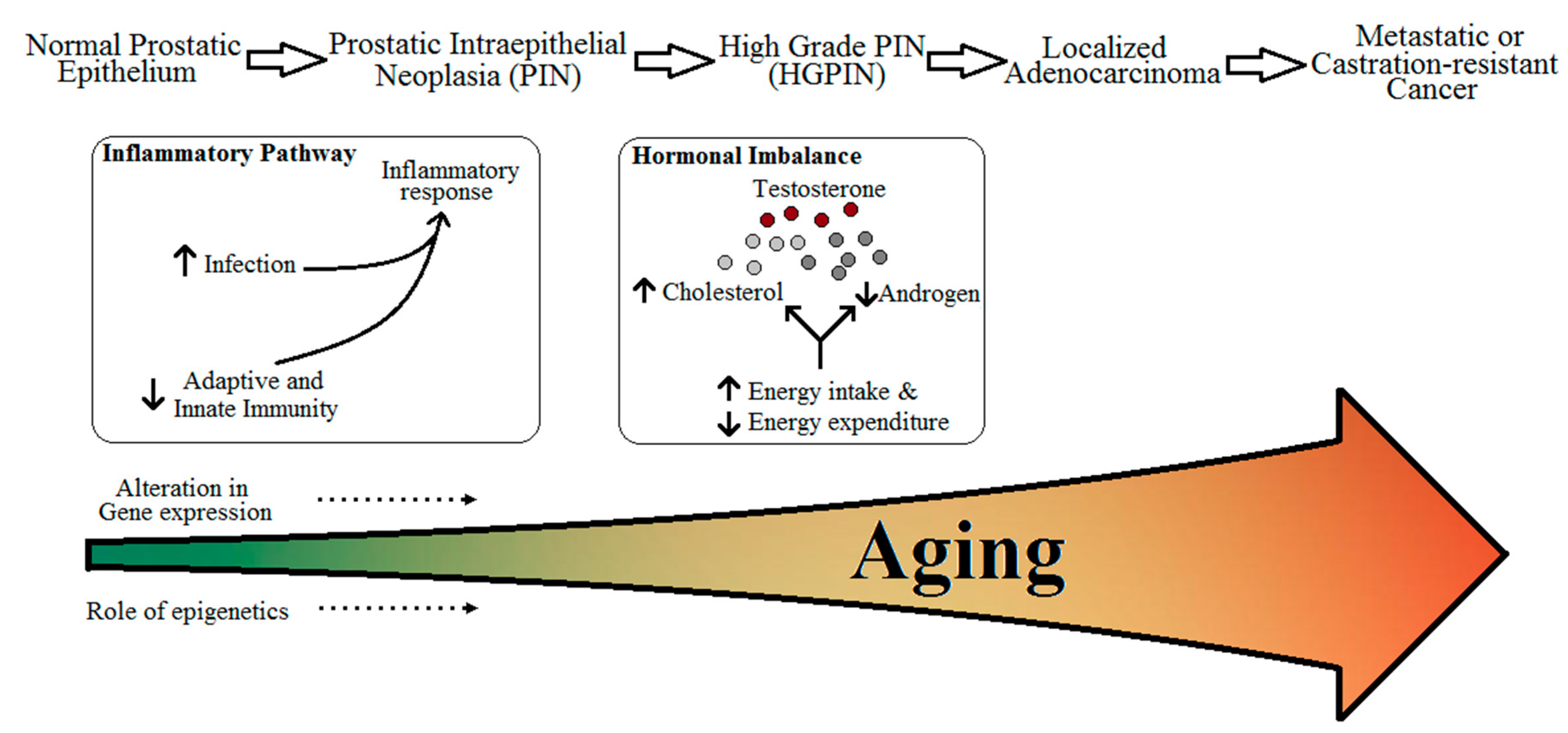
:1. Introduction
- (i)
- Immunity and inflammatory response,
- (ii)
- Cholesterol metabolism and obesity,
- (iii)
- Free testosterone levels,
- (iv)
- Genetic and epigenetic effects.
- Is PCa a gerontological disorder fuelled by an aging immune system, altered cellular metabolism, decreased levels of testosterone, and alterations in gene expression?
- Is there potential for slowing or reverting these changes?
- If the answer to question 1 is ‘yes’, can diagnostic tools distinguish aggressive PCa from non-aggressive PCa for possible early interventions?
2. Risk Factors for Prostate Cancer
3. Aging, Immunity, Inflammatory Response, and Prostate Cancer
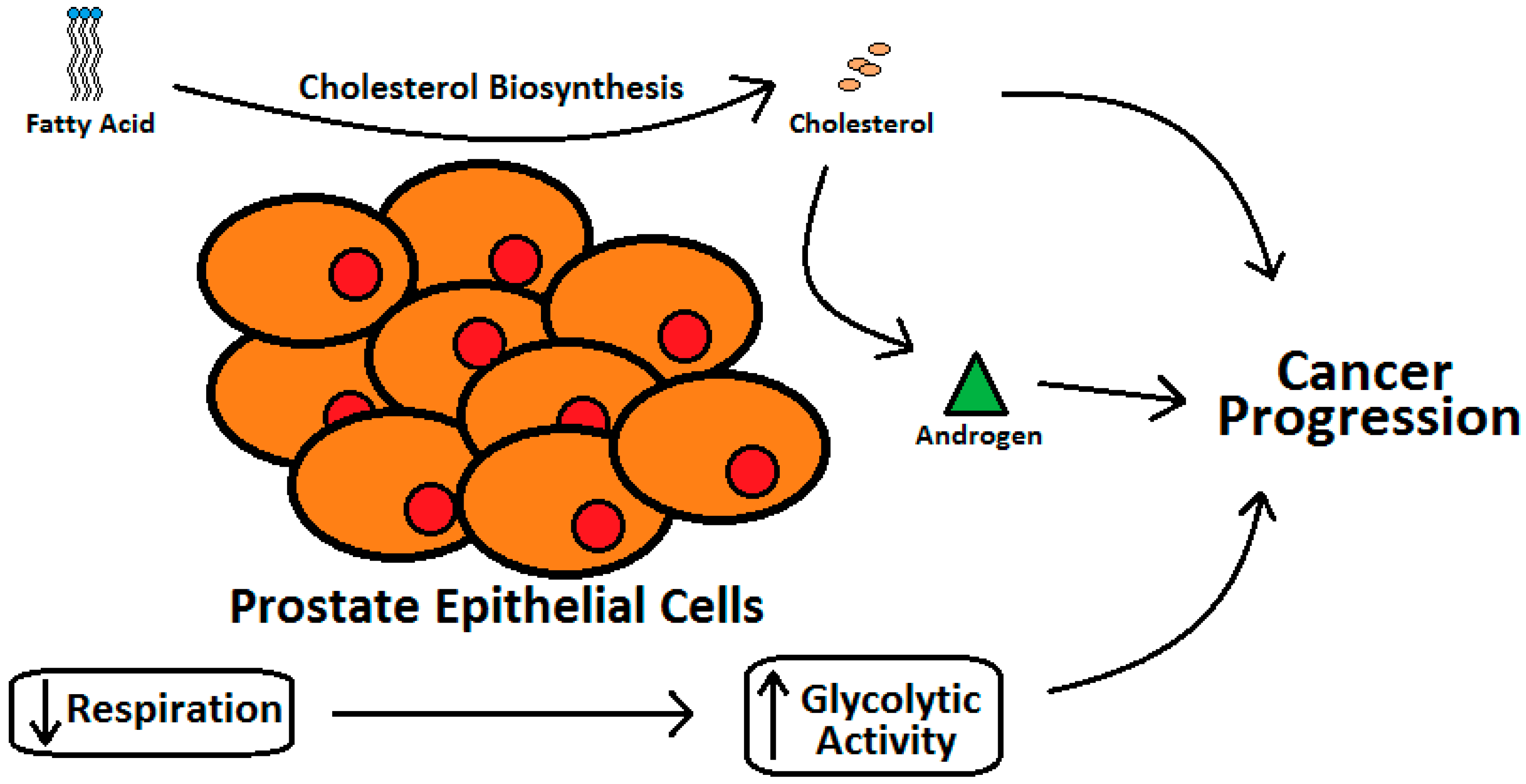
4. Aging, Cholesterol Metabolism, and Prostate Cancer
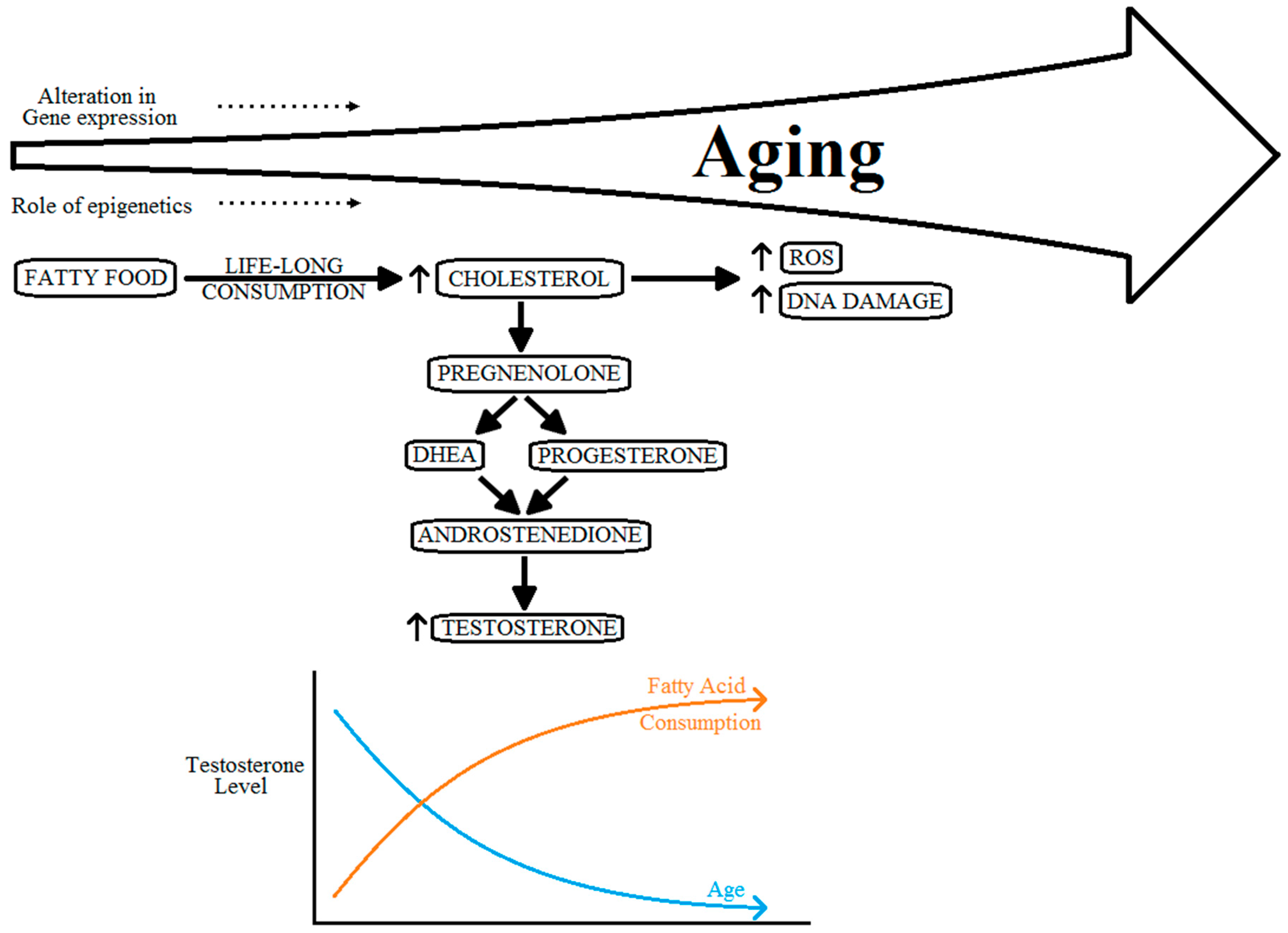
5. Aging, Testosterone Level and Prostate Cancer
6. Aging, Genetic and Epigenetic Effects and Prostate Cancer
7. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ANXA1 | Annexin A1 |
| CRISPR | clustered regularly interspaced short palindromic repeats |
| CRISPR/Cas9 | CRISPR associated protein 9 |
| DHEA | dehydroepiandrosterone |
| GDF15 | Growth differentiation factor 15 |
| GRN | Granulin |
| GST1 | Glutathione S-Transferase-1 |
| GSTP1 | Glutathione S-Transferase P |
| GWAS | genome-wide association studies |
| HDL | high-density lipoprotein |
| HFDs | high fat diets |
| IL10 | Interleukin -10 |
| IL1RN | Interleukin 1 receptor antagonist |
| IL8 | Interleukin -8 |
| LDL | low-density lipoprotein |
| lncRNAs | long non-coding RNAs |
| MIC-1 | Macrophage inhibitory cytokine-1 |
| miRNAs | microRNAs |
| MSR1 | Macrophage Scavenger Receptor 1 |
| PCa | prostate cancer |
| PSA | prostate-specific antigen |
| RNAs | ribonucleic acids |
| RNASEL | RNase L |
| ROS | reactive oxygen species |
| SNPs | single nucleotide polymorphisms |
| TLR4 | Toll-like receptor 4 |
References
- De Magalhaes, J.P.; Curado, J.; Church, G.M. Meta-analysis of age-related gene expression profiles identifies common signatures of aging. Bioinformatics (Oxford, England) 2009, 25, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Birbrair, A.; Zhang, T.; Wang, Z.M.; Messi, M.L.; Mintz, A.; Delbono, O. Type-1 pericytes participate in fibrous tissue deposition in aged skeletal muscle. Am. J. Physiol. Cell Physiol. 2013, 305, 25. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, T.; Atwal, J.K.; Steinberg, S.; Snaedal, J.; Jonsson, P.V.; Bjornsson, S.; Stefansson, H.; Sulem, P.; Gudbjartsson, D.; Maloney, J.; et al. A mutation in APP protects against Alzheimer's disease and age-related cognitive decline. Nature 2012, 488, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Finegold, J.A.; Asaria, P.; Francis, D.P. Mortality from ischaemic heart disease by country, region, and age: Statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2013, 168, 934–945. [Google Scholar] [CrossRef] [PubMed]
- Jani, B.; Rajkumar, C. Ageing and vascular ageing. Postgrad. Med. J. 2006, 82, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Pinto, E. Blood pressure and ageing. Postgrad. Med. J. 2007, 83, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Benz, C.C. Impact of aging on the biology of breast cancer. Crit. Rev. Oncol. Hematol. 2008, 66, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Brunet, A.; Berger, S.L. Epigenetics of aging and aging-related disease. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, S17–S20. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.L.; Chen, M.H.; Aizer, A.A.; Hattangadi, J.A.; D’Amico, A.V. Advancing age within established Gleason score categories and the risk of prostate cancer-specific mortality (PCSM). BJU Int. 2012, 110, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.B.; Sternberg, I.A.; Karen-Paz, G.; Kim, P.H.; Sjoberg, D.; Vargas, H.A.; Touijer, K.; Eastham, J.A.; Ehdaie, B. Age is Associated with Upgrading at Confirmatory Biopsy among Men with Prostate Cancer Treated with Active Surveillance. J. Urol. 2015, 194, 1607–1611. [Google Scholar] [CrossRef] [PubMed]
- Cooper, P.R.; McGuire, B.B.; Helfand, B.T.; Loeb, S.; Hu, Q.; Catalona, W.J. Prostate cancer risk alleles and their associations with other malignancies. Urology 2011, 78, 5. [Google Scholar] [CrossRef] [PubMed]
- Karunasinghe, N.; Lange, K.; Yeo Han, D.; Goudie, M.; Zhu, S.H.; Wang, A.; Bishop, K.R.; Ferguson, L.G.; Masters, J. Androgen Pathway Related Gene Variants and Prostate Cancer Association in Auckland Men. Curr. Pharmacog. Personal. Med. 2013, 11, 22–30. [Google Scholar] [CrossRef]
- Bostwick, D.G.; Burke, H.B.; Djakiew, D.; Euling, S.; Ho, S.M.; Landolph, J.; Morrison, H.; Sonawane, B.; Shifflett, T.; Waters, D.J.; et al. Human prostate cancer risk factors. Cancer 2004, 101, 2371–2490. [Google Scholar] [CrossRef] [PubMed]
- Nelen, V. Epidemiology of prostate cancer. In Prostate Cancer; Ramon, J., Denis, L.J., Eds.; the series Recent Results in Cancer Research; Springer: Berlin/Heidelberg, Germany, 2007; Volume 175, pp. 1–8. [Google Scholar]
- Wu, X.; Gu, J. Biomarkers for Assessing Risk of Cancer. In The Molecular Basis of Cancer, 4th ed.; Mendelsohn, J., Howley, P.M., Israel, M.A., Gray, J.W., Thompson, C.B., Eds.; Elsevier Inc: New York, NY, USA, 2015; pp. 317–330. [Google Scholar]
- Ferguson, L.R. Meat and cancer. Meat Sci. 2010, 84, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Gann, P.H. Risk Factors for Prostate Cancer. Rev. Urol. 2002, 4, S3–S10. [Google Scholar] [PubMed]
- Goh, C.L.; Saunders, E.J.; Leongamornlert, D.A.; Tymrakiewicz, M.; Thomas, K.; Selvadurai, E.D.; Woode-Amissah, R.; Dadaev, T.; Mahmud, N.; Castro, E.; et al. Clinical implications of family history of prostate cancer and genetic risk single nucleotide polymorphism (SNP) profiles in an active surveillance cohort. BJU Int. 2013, 112, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Medzhitov, R.; Janeway, C., Jr. Innate immunity. N. Engl. J. Med. 2000, 343, 338–344. [Google Scholar] [CrossRef]
- Solana, R.; Tarazona, R.; Gayoso, I.; Lesur, O.; Dupuis, G.; Fulop, T. Innate immunosenescence: Effect of aging on cells and receptors of the innate immune system in humans. Semin. Immunol. 2012, 24, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Too old to fight? Aging and its toll on innate immunity. Mol. Oral Microbiol. 2010, 25, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Gomez, C.R.; Nomellini, V.; Faunce, D.E.; Kovacs, E.J. Innate immunity and aging. Exp. Gerontol. 2008, 43, 718–728. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Aging and its Impact on Innate Immunity and Inflammation: Implications for Periodontitis. J. Oral Biosci. 2014, 56, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Weng, N.P. Aging of the immune system: How much can the adaptive immune system adapt? Immunity 2006, 24, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Mahbub, S.; Brubaker, A.L.; Kovacs, E.J. Aging of the Innate Immune System: An Update. Curr. Immunol. Rev. 2011, 7, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Bonafe, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.C. Aging. Proc. Am. Thorac. Soc. 2005, 2, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef] [PubMed]
- Thun, M.J.; Henley, S.J.; Gansler, T. Inflammation and cancer: An epidemiological perspective. Novartis Found Symp. 2004, 256, 6–21. [Google Scholar] [PubMed]
- Mantovani, A. Cancer: Inflaming metastasis. Nature 2009, 457, 36–37. [Google Scholar] [CrossRef] [PubMed]
- Sikora, E.; Scapagnini, G.; Barbagallo, M. Curcumin, inflammation, ageing and age-related diseases. Immun. Ageing 2010, 7, 1742–4933. [Google Scholar] [CrossRef] [PubMed]
- De Nunzio, C.; Kramer, G.; Marberger, M.; Montironi, R.; Nelson, W.; Schroder, F.; Sciarra, A.; Tubaro, A. The controversial relationship between benign prostatic hyperplasia and prostate cancer: The role of inflammation. Eur. Urol. 2011, 60, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Kazma, R.; Mefford, J.A.; Cheng, I.; Plummer, S.J.; Levin, A.M.; Rybicki, B.A.; Casey, G.; Witte, J.S. Association of the innate immunity and inflammation pathway with advanced prostate cancer risk. PLoS ONE 2012, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Bortner, J.D., Jr.; Aliaga, C.A.; Baker, A.; Stanley, A.; Stanley, B.A.; Kaag, M.; Richie, J.P., Jr.; El-Bayoumy, K. Changes in proteomic profiles in different prostate lobes of male rats throughout growth and development and aging stages of the life span. Prostate 2013, 73, 363–375. [Google Scholar] [CrossRef] [PubMed]
- Shanmugasundaram, K.R.; Visvanathan, A.; Dhandapani, K.; Srinivasan, N.; Rasappan, P.; Gilbert, R.; Alladi, S.; Kancharla, S.; Vasanthi, N. Effect of high-fat diet on cholesterol distribution in plasma lipoproteins, cholesterol esterifying activity in leucocytes, and erythrocyte membrane components studied: Importance of body weight. Am. J. Clin. Nutr. 1986, 44, 805–815. [Google Scholar] [PubMed]
- Elmslie, J.L.; Sellman, J.D.; Schroder, R.N.; Carter, F.A. The NEEDNT Food List: Non-essential, energy-dense, nutritionally-deficient foods. N. Zeal. Med. J. 2012, 125, 84–92. [Google Scholar]
- Zhuang, L.; Kim, J.; Adam, R.M.; Solomon, K.R.; Freeman, M.R. Cholesterol targeting alters lipid raft composition and cell survival in prostate cancer cells and xenografts. J. Clin. Investig. 2005, 115, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Currie, E.; Schulze, A.; Zechner, R.; Walther, T.C.; Farese, R.V., Jr. Cellular fatty acid metabolism and cancer. Cell Metab. 2013, 18, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.J. Cholesterol, statins and cancer. Clin. Exp. Pharmacol. Physiol. 2007, 34, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Krycer, J.R.; Brown, A.J. Cholesterol accumulation in prostate cancer: A classic observation from a modern perspective. Biochim. Biophys. Acta 2013, 2, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, A.V.; Krycer, J.R.; Brown, A.J. Overexpression of a key regulator of lipid homeostasis, Scap, promotes respiration in prostate cancer cells. FEBS Lett. 2013, 587, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Freter, C. Lipid Metabolism, Apoptosis and Cancer Therapy. Int. J. Mol. Sci. 2015, 16, 924–949. [Google Scholar] [CrossRef] [PubMed]
- Rosca, M.G.; Vazquez, E.J.; Chen, Q.; Kerner, J.; Kern, T.S.; Hoppel, C.L. Oxidation of fatty acids is the source of increased mitochondrial reactive oxygen species production in kidney cortical tubules in early diabetes. Diabetes 2012, 61, 2074–2083. [Google Scholar] [CrossRef]
- Dalleau, S.; Baradat, M.; Gueraud, F.; Huc, L. Cell death and diseases related to oxidative stress: 4-hydroxynonenal (HNE) in the balance. Cell Death Differ. 2013, 20, 1615–1630. [Google Scholar] [CrossRef] [PubMed]
- Platz, E.A.; Leitzmann, M.F.; Visvanathan, K.; Rimm, E.B.; Stampfer, M.J.; Willett, W.C.; Giovannucci, E. Statin drugs and risk of advanced prostate cancer. J. Natl. Cancer Inst. 2006, 98, 1819–1825. [Google Scholar] [CrossRef] [PubMed]
- Murtola, T.J.; Tammela, T.L.; Lahtela, J.; Auvinen, A. Cholesterol-lowering drugs and prostate cancer risk: A population-based case-control study. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cospons. Am. Soc. Prev. Oncol. 2007, 16, 2226–2232. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Ross, R.K.; Bernstein, L.; Yatani, R.; Henderson, B.E.; Mack, T.M. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br. J. Cancer 1991, 63, 963–966. [Google Scholar] [CrossRef] [PubMed]
- Ohvo-Rekila, H.; Ramstedt, B.; Leppimaki, P.; Slotte, J.P. Cholesterol interactions with phospholipids in membranes. Prog. Lipid Res. 2002, 41, 66–97. [Google Scholar] [CrossRef]
- Lin, P.H.; Aronson, W.; Freedland, S.J. Nutrition, dietary interventions and prostate cancer: The latest evidence. BMC Med. 2015, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.T. An evolutionary review of human telomere biology: The thrifty telomere hypothesis and notes on potential adaptive paternal effects. Am. J. Hum. Biol. 2011, 23, 149–167. [Google Scholar] [CrossRef] [PubMed]
- Stanworth, R.D.; Jones, T.H. Testosterone for the aging male; current evidence and recommended practice. Clin. Interv. Aging 2008, 3, 25–44. [Google Scholar] [PubMed]
- Ellison, P.T.; Bribiescas, R.G.; Bentley, G.R.; Campbell, B.C.; Lipson, S.F.; Panter-Brick, C.; Hill, K. Population variation in age-related decline in male salivary testosterone. Hum. Reprod. (Oxf. Engl.) 2002, 17, 3251–3253. [Google Scholar] [CrossRef]
- Denti, L.; Pasolini, G.; Sanfelici, L.; Benedetti, R.; Cecchetti, A.; Bruschieri, L.; Ablondi, F.; Valenti, G. The contribution of androgen decline to the aging-related changes of body composition and lipoprotein in the healthy man. J. Endocrinol. Investig. 1999, 22, 68–69. [Google Scholar]
- Vermeulen, A.; Goemaere, S.; Kaufman, J.M. Testosterone, body composition and aging. J. Endocrinol. Investig. 1999, 22, 110–116. [Google Scholar]
- Kenny, A.M.; Prestwood, K.M.; Marcello, K.M.; Raisz, L.G. Determinants of bone density in healthy older men with low testosterone levels. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M492–M497. [Google Scholar] [CrossRef]
- van den Beld, A.W.; de Jong, F.H.; Grobbee, D.E.; Pols, H.A.; Lamberts, S.W. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J. Clin. Endocrinol. Metab. 2000, 85, 3276–3282. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.K.; Lavrovsky, Y.; Song, C.S.; Chen, S.; Jung, M.H.; Velu, N.K.; Bi, B.Y.; Chatterjee, B. Regulation of androgen action. Vitam. Horm 1999, 55, 309–352. [Google Scholar] [PubMed]
- Harman, S.M.; Metter, E.J.; Tobin, J.D.; Pearson, J.; Blackman, M.R. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J. Clin. Endocrinol. Metab. 2001, 86, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Feldman, H.A.; Longcope, C.; Derby, C.A.; Johannes, C.B.; Araujo, A.B.; Coviello, A.D.; Bremner, W.J.; McKinlay, J.B. Age trends in the level of serum testosterone and other hormones in middle-aged men: Longitudinal results from the Massachusetts male aging study. J. Clin. Endocrinol. Metab. 2002, 87, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.T. DHEA metabolism in prostate: For better or worse? Mol. Cell Endocrinol. 2009, 301, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.C.; Tajar, A.; Pye, S.R.; Silman, A.J.; Finn, J.D.; O’Neill, T.W.; Bartfai, G.; Casanueva, F.; Forti, G.; Giwercman, A.; et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: The European Male Aging Study. J. Clin. Endocrinol. Metab. 2008, 93, 2737–2745. [Google Scholar] [CrossRef] [PubMed]
- Araujo, A.B.; Wittert, G.A. Endocrinology of the aging male. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 303–319. [Google Scholar] [CrossRef] [PubMed]
- Belanger, A.; Candas, B.; Dupont, A.; Cusan, L.; Diamond, P.; Gomez, J.L.; Labrie, F. Changes in serum concentrations of conjugated and unconjugated steroids in 40- to 80-year-old men. J. Clin. Endocrinol. Metab. 1994, 79, 1086–1090. [Google Scholar] [CrossRef] [PubMed]
- Shin, B.S.; Hwang, E.C.; Im, C.M.; Kim, S.; Jung, S.I.; Kang, T.W.; Kwon, D.D.; Park, K.; Ryu, S.B. Is a Decreased Serum Testosterone Level a Risk Factor for Prostate Cancer? A Cohort Study of Korean Men. Korean J. Urol. 2010, 51, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.A.; DeWolf, W.C.; Morgentaler, A. Is low serum free testosterone a marker for high grade prostate cancer? J. Urol. 2000, 163, 824–827. [Google Scholar] [CrossRef]
- Stattin, P.; Lumme, S.; Tenkanen, L.; Alfthan, H.; Jellum, E.; Hallmans, G.; Thoresen, S.; Hakulinen, T.; Luostarinen, T.; Lehtinen, M.; et al. High levels of circulating testosterone are not associated with increased prostate cancer risk: A pooled prospective study. Int. J. Cancer J. Int. Du Cancer 2004, 108, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.L.; Wadhwa, S.N.; Kumar, V.; Farooq, A. Androgen, estrogen, and progesterone receptor contents and serum hormone profiles in patients with benign hypertrophy and carcinoma of the prostate. J. Surg. Oncol. 1990, 44, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Schatzl, G.; Madersbacher, S.; Thurridl, T.; Waldmuller, J.; Kramer, G.; Haitel, A.; Marberger, M. High-grade prostate cancer is associated with low serum testosterone levels. Prostate 2001, 47, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Munetomo, A.; Hojo, Y.; Higo, S.; Kato, A.; Yoshida, K.; Shirasawa, T.; Shimizu, T.; Barron, A.; Kimoto, T.; Kawato, S. Aging-induced changes in sex-steroidogenic enzymes and sex-steroid receptors in the cortex, hypothalamus and cerebellum. J. Physiol. Sci. 2015, 65, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Pomerantz, M.M.; Li, F.; Takeda, D.Y.; Lenci, R.; Chonkar, A.; Chabot, M.; Cejas, P.; Vazquez, F.; Cook, J.; Shivdasani, R.A.; et al. The androgen receptor cistrome is extensively reprogrammed in human prostate tumorigenesis. Nat. Genet. 2015, 47, 1346–1351. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Richardson, M.; Reddy, V.; Menon, M.; Barrack, E.R.; Reddy, G.P.; Kim, S.H. Structural and functional association of androgen receptor with telomeres in prostate cancer cells. Aging 2013, 5, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, L.M.; Heaphy, C.M.; Joshu, C.E.; Isaacs, W.B.; Konishi, Y.; De Marzo, A.M.; Isaacs, S.D.; Wiley, K.E.; Platz, E.A.; Meeker, A.K. Telomere length as a risk factor for hereditary prostate cancer. Prostate 2014, 74, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Ammerpohl, O.; Bens, S.; Appari, M.; Werner, R.; Korn, B.; Drop, S.L.; Verheijen, F.; van der Zwan, Y.; Bunch, T.; Hughes, I.; et al. Androgen receptor function links human sexual dimorphism to DNA methylation. PLoS ONE 2013, 8, e73288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwabi-Addo, B.; Chung, W.; Shen, L.; Ittmann, M.; Wheeler, T.; Jelinek, J.; Issa, J.P. Age-related DNA methylation changes in normal human prostate tissues. Clin. Cancer Res. 2007, 13, 3796–3802. [Google Scholar] [CrossRef] [PubMed]
- Osorio, F.G.; Varela, I.; Lara, E.; Puente, X.S.; Espada, J.; Santoro, R.; Freije, J.M.; Fraga, M.F.; Lopez-Otin, C. Nuclear envelope alterations generate an aging-like epigenetic pattern in mice deficient in Zmpste24 metalloprotease. Aging Cell 2010, 9, 947–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, M.; Pfeifer, G.P. Aging and DNA methylation. BMC Biol. 2015, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Ida, H.; Boylan, S.A.; Weigel, A.L.; Hjelmeland, L.M. Age-related changes in the transcriptional profile of mouse RPE/choroid. Physiol. Genomics 2003, 15, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Weindruch, R.; Kayo, T.; Lee, C.K.; Prolla, T.A. Gene expression profiling of aging using DNA microarrays. Mech. Ageing Dev. 2002, 123, 177–193. [Google Scholar] [CrossRef]
- Rodwell, G.E.; Sonu, R.; Zahn, J.M.; Lund, J.; Wilhelmy, J.; Wang, L.; Xiao, W.; Mindrinos, M.; Crane, E.; Segal, E.; et al. A transcriptional profile of aging in the human kidney. PLoS Biol. 2004, 2, 30. [Google Scholar] [CrossRef] [PubMed]
- Thum, T. Noncoding RNAs and myocardial fibrosis. Nat. Rev. Cardiol. 2014, 11, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Devaux, Y.; Zangrando, J.; Schroen, B.; Creemers, E.E.; Pedrazzini, T.; Chang, C.P.; Dorn, G.W., II; Thum, T.; Heymans, S. Long noncoding RNAs in cardiac development and ageing. Nat. Rev. Cardiol. 2015, 12, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.J.; Suh, Y. MicroRNA in Aging: From Discovery to Biology. Curr. Genomics 2012, 13, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Ingolia, N.T.; Weissman, J.S.; Bartel, D.P. Mammalian microRNAs predominantly act to decrease target mRNA levels. Nature 2010, 466, 835–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Otin, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [PubMed]
- Noren Hooten, N.; Abdelmohsen, K.; Gorospe, M.; Ejiogu, N.; Zonderman, A.B.; Evans, M.K. microRNA Expression Patterns Reveal Differential Expression of Target Genes with Age. PLoS ONE 2010, 5, e10724. [Google Scholar] [CrossRef] [PubMed]
- Rottiers, V.; Naar, A.M. MicroRNAs in metabolism and metabolic disorders. Nat. Rev. Mol. Cell Biol. 2012, 13, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Walter, B.A.; Valera, V.A.; Pinto, P.A.; Merino, M.J. Comprehensive microRNA Profiling of Prostate Cancer. J. Cancer 2013, 4, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Amankwah, E.K.; Anegbe, E.; Park, H.; Pow-Sang, J.; Hakam, A.; Park, J.Y. miR-21, miR-221 and miR-222 expression and prostate cancer recurrence among obese and non-obese cases. Asian J. Androl. 2013, 15, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Vinciguerra, M.; Sgroi, A.; Veyrat-Durebex, C.; Rubbia-Brandt, L.; Buhler, L.H.; Foti, M. Unsaturated fatty acids inhibit the expression of tumor suppressor phosphatase and tensin homolog (PTEN) via microRNA-21 up-regulation in hepatocytes. Hepatology (Baltimore, Md) 2009, 49, 1176–1184. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, V.; Krishnamoorthy, V.; Karunasinghe, N.; Jabed, A.; Pallati, R.; Kao, C.; Wang, A.; Marlow, G.; Ferguson, L. Are We Eating Our Way to Prostate Cancer—A Hypothesis Based on the Evolution, Bioaccumulation, and Interspecific Transfer of miR-150. Non-Coding RNA 2016, 2, 2. [Google Scholar] [CrossRef]
- Vaidyanathan, V.; Krishnamoorthy, V.; Karunasinghe, N.; Jabed, A.; Pallati, R.; Kao, C.; Wang, A.; Marlow, G.; Ferguson, L. Correction: Vaidyanathan et al. Are We Eating Our Way to Prostate Cancer—A Hypothesis Based on the Evolution, Bioaccumulation, and Interspecific Transfer of miR-150. Non-Coding RNA 2016, 2, 2. Non-Coding RNA 2016, 2, 6. [Google Scholar] [CrossRef]
- Noren Hooten, N.; Fitzpatrick, M.; Wood, W.H., 3rd; De, S.; Ejiogu, N.; Zhang, Y.; Mattison, J.A.; Becker, K.G.; Zonderman, A.B.; Evans, M.K. Age-related changes in microRNA levels in serum. Aging 2013, 5, 725–740. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.J.; Murad, A.; Chen, L.; Davey Smith, G.; Donovan, J.; Palmer, T.; Hamdy, F.; Neal, D.; Lane, J.A.; Davis, M.; et al. Associations between an obesity related genetic variant (FTO rs9939609) and prostate cancer risk. PLoS ONE 2010, 5, 0013485. [Google Scholar] [CrossRef] [PubMed]
- Kanherkar, R.R.; Bhatia-Dey, N.; Csoka, A.B. Epigenetics across the human lifespan. Front Cell Dev. Biol. 2014, 2, 49. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.P.; Burge, C.B.; Bartel, D.P. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 2005, 120, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Ran, F.A.; Hsu, P.D.; Lin, C.Y.; Gootenberg, J.S.; Konermann, S.; Trevino, A.E.; Scott, D.A.; Inoue, A.; Matoba, S.; Zhang, Y.; et al. Double nicking by RNA-guided CRISPR Cas9 for enhanced genome editing specificity. Cell 2013, 154, 1380–1389. [Google Scholar] [CrossRef] [PubMed]
- Mali, P.; Yang, L.; Esvelt, K.M.; Aach, J.; Guell, M.; DiCarlo, J.E.; Norville, J.E.; Church, G.M. RNA-guided human genome engineering via Cas9. Science 2013, 339, 823–826. [Google Scholar] [CrossRef] [PubMed]
- Karunasinghe, N.; Zhu, Y.; Han, D.Y.; Lange, K.; Zhu, S.; Wang, A.; Ellett, S.; Masters, J.; Goudie, M.; Keogh, J.; et al. Quality of life effects of androgen deprivation therapy in a prostate cancer cohort in New Zealand: Can we minimize effects using a stratification based on the aldo-keto reductase family 1, member C3 rs12529 gene polymorphism? BMC Urol. 2016, 16, 48. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.-C.; Huang, S.-P.; Lee, Y.-C.; Huang, C.-Y.; Liu, C.-C.; Hour, T.-C.; Huang, C.-N.; You, B.-J.; Chang, T.-Y.; Huang, C.-H.; et al. Molecular Markers in Sex Hormone Pathway Genes Associated with the Efficacy of Androgen-Deprivation Therapy for Prostate Cancer. PLoS ONE 2013, 8, e54627. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.J. Screening for Prostate Cancer—The Controversy That Refuses to Die. N. Engl. J. Med. 2009, 360, 1351–1354. [Google Scholar] [CrossRef] [PubMed]
- Bell, N.; Connor Gorber, S.; Shane, A.; Joffres, M.; Singh, H.; Dickinson, J.; Shaw, E.; Dunfield, L.; Tonelli, M. Recommendations on screening for prostate cancer with the prostate-specific antigen test. Cmaj 2014, 186, 1225–1234. [Google Scholar] [CrossRef] [PubMed]
- Moyer, V.A. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2012, 157, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Calonge, N.; Petitti, D.B.; DeWitt, T.G.; Dietrich, A.J.; Gregory, K.D.; Harris, R.; Isham, G.J.; LeFevre, M.L.; Leipzig, R.; Loveland-Cherry, C.; et al. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2008, 149, 185–191. [Google Scholar]
- Weiner, A.B.; Matulewicz, R.S.; Eggener, S.E.; Schaeffer, E.M. Increasing incidence of metastatic prostate cancer in the United States (2004–2013). Prostate Cancer Prost. Dis. 2016, 19, 30. [Google Scholar] [CrossRef] [PubMed]
- Duggan, D.; Zheng, S.L.; Knowlton, M.; Benitez, D.; Dimitrov, L.; Wiklund, F.; Robbins, C.; Isaacs, S.D.; Cheng, Y.; Li, G.; et al. Two Genome-wide Association Studies of Aggressive Prostate Cancer Implicate Putative Prostate Tumor Suppressor Gene DAB2IP. J. Natl. Cancer Inst. 2007, 99, 1836–1844. [Google Scholar] [CrossRef] [PubMed]
- Amin Al Olama, A.; Kote-Jarai, Z.; Schumacher, F.R.; Wiklund, F.; Berndt, S.I.; Benlloch, S.; Giles, G.G.; Severi, G.; Neal, D.E.; Hamdy, F.C.; et al. A meta-analysis of genome-wide association studies to identify prostate cancer susceptibility loci associated with aggressive and non-aggressive disease. Hum. Mol. Genet. 2013, 22, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Knipe, D.W.; Evans, D.M.; Kemp, J.P.; Eeles, R.; Easton, D.F.; Kote-Jarai, Z.; Al Olama, A.A.; Benlloch, S.; Donovan, J.L.; Hamdy, F.C.; et al. Genetic variation in prostate-specific antigen-detected prostate cancer and the effect of control selection on genetic association studies. Cancer Epidemiol. Biomark. Prev.: Publ. Am. Assoc. Cancer Res. Cospons. Am. Soc. Prev. Oncol. 2014, 23, 1356–1365. [Google Scholar] [CrossRef] [PubMed]
- Easton, D.F.; Eeles, R.A. Genome-wide association studies in cancer. Hum. Mol. Genet. 2008, 17, R109–R115. [Google Scholar] [CrossRef] [PubMed]
- Kinseth, M.A.; Jia, Z.; Rahmatpanah, F.; Sawyers, A.; Sutton, M.; Wang-Rodriguez, J.; Mercola, D.; McGuire, K.L. Expression between African American and Caucasian Prostate Cancer Tissue Reveals that Stroma is the Site of Aggressive Changes. Int. J. Cancer 2014, 134, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Bensen, J.T.; Xu, Z.; Smith, G.J.; Mohler, J.L.; Fontham, E.T.; Taylor, J.A. Genetic polymorphism and prostate cancer aggressiveness: A case-only study of 1536 GWAS and candidate SNPs in African-Americans and European-Americans. Prostate 2013, 73, 11–22. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaidyanathan, V.; Karunasinghe, N.; Jabed, A.; Pallati, R.; Kao, C.H.-J.; Wang, A.; Marlow, G.; Ferguson, L.R. Prostate Cancer: Is It a Battle Lost to Age? Geriatrics 2016, 1, 27. https://doi.org/10.3390/geriatrics1040027
Vaidyanathan V, Karunasinghe N, Jabed A, Pallati R, Kao CH-J, Wang A, Marlow G, Ferguson LR. Prostate Cancer: Is It a Battle Lost to Age? Geriatrics. 2016; 1(4):27. https://doi.org/10.3390/geriatrics1040027
Chicago/Turabian StyleVaidyanathan, Venkatesh, Nishi Karunasinghe, Anower Jabed, Radha Pallati, Chi Hsiu-Juei Kao, Alice Wang, Gareth Marlow, and Lynnette R. Ferguson. 2016. "Prostate Cancer: Is It a Battle Lost to Age?" Geriatrics 1, no. 4: 27. https://doi.org/10.3390/geriatrics1040027






