1. Introduction
The relationship of paranasal sinus pneumatization with chronic rhinosinusitis (CRS) has been incompletely studied. Among cystic fibrosis (CF) patients, for whom sinus mucosal inflammation is nearly universal [
1,
2], sinus hypoplasia is well documented [
2,
3,
4,
5,
6]. Because of these findings in CF, it has been suggested that mucosal disease and infection may lead to arrested sinus development [
6,
7,
8]. Previous studies using radiographic instruments have been successful at differentiating sinus hypoplasia in CF [
3,
4,
5], but have not been able to discern a difference in CRS without CF from unaffected controls [
4,
6].
Studying paranasal sinus pneumatization in CRS has been hindered by the lack of a validated measure for sinus pneumatization. The instruments used to discern sinus hypoplasia in previous studies of CF patients are incompletely validated for use in a general population of sinus computed tomography (CT) scans [
3,
4,
5]. Furthermore, volumetric or dimensional analysis of sinus CT tends to be too cumbersome for the large populations that may be necessary to detect small differences [
6]. The Assessment of Pneumatization of the Paranasal Sinuses (APPS) score was recently validated for evaluating the extent of sinus pneumatization [
9,
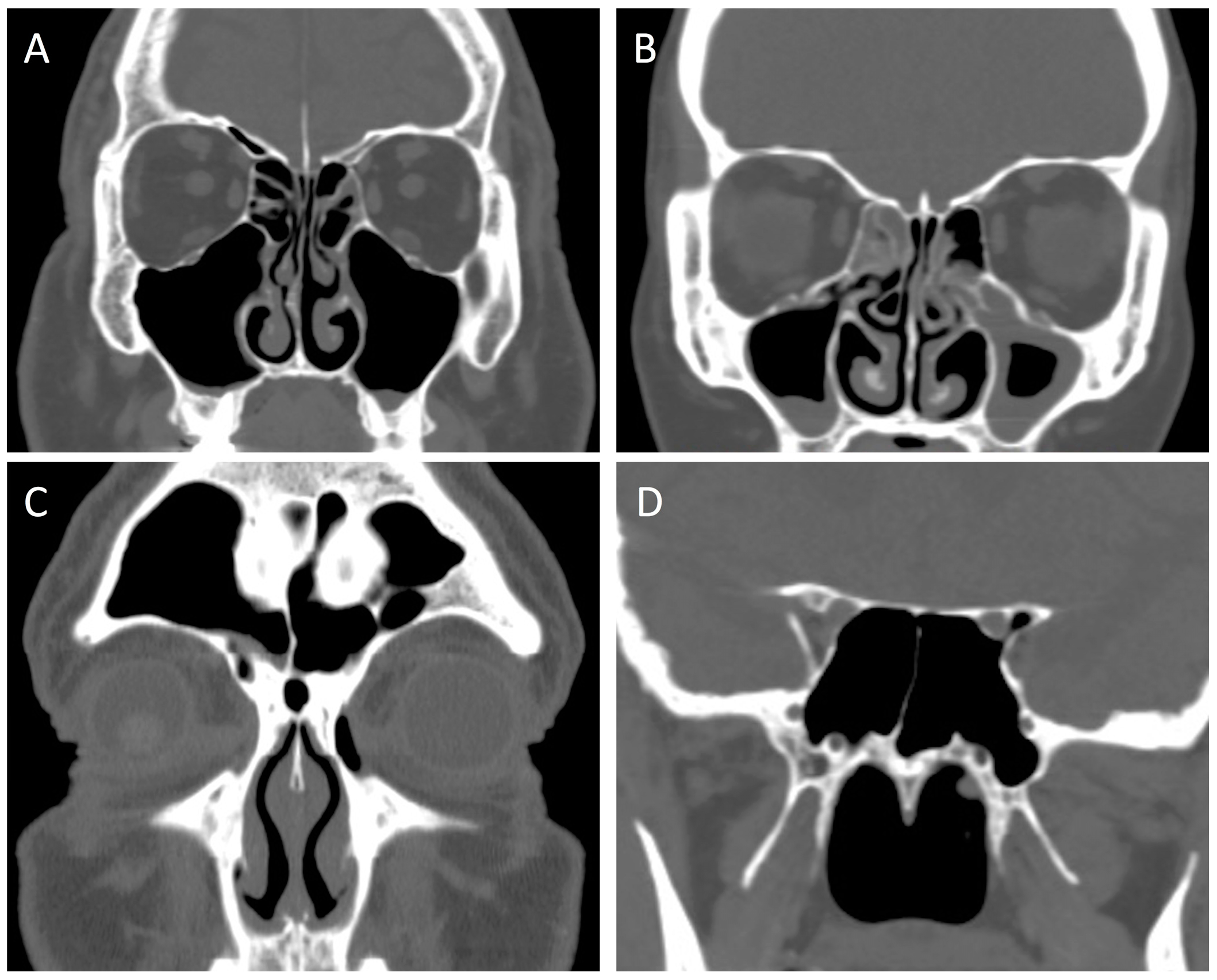
10]. The APPS score evaluates for the presence of nine anatomic variants bilaterally (
Table 1,
Figure 1), and can be used for clinician assessment of paranasal sinus pneumatization. This method of determining the extent of sinus pneumatization has not been previously applied to CF or CRS patients.
The purpose of this study was to apply the APPS score to a large population of CRS patients and healthy controls in order to determine if paranasal sinus pneumatization differs between these two groups. Understanding sinus pneumatization in CRS patients might help to understand if sinus disease and anatomy are related in a generalizable way.
2. Materials and Methods
Sinus and maxillofacial CT scans performed at the Ochsner Clinic Foundation were considered for inclusion in the study. An adolescent cohort (
n = 303), defined as patients age 13–18 at the date of service, was assembled from all CT scans performed between 1 January 2010 and 31 December 2014. Only scans with axial and coronal orientations available were included. A similarly-sized cohort of adults (
n = 288), defined as patients over 18 years of age, was assembled for all sinus and maxillofacial CT scans acquired from 6 July 2015 to 6 August 2015. All CT scans were evaluated for APPS and Lund-Mackay scores. A diagnosis of CRS or CF, as determined by the treating physician, was then retrospectively gathered from the medical record for each scored CT scan. CRS phenotype was also determined and recorded as chronic rhinosinusitis with nasal polyposis (CRSwNP), chronic rhinosinusitis without nasal polyposis (CRSsNP), or allergic fungal rhinosinusitis (AFRS). The diagnosis of CRS or CF was assigned independent of Lund-MacKay score. Patients without a diagnosis of CRS or CF were included in the unaffected control group. CT scans in the control group were typically acquired for the evaluation of facial trauma without positive findings, or as part of the diagnostic workup to rule out CRS in the primary care setting. Radiographic scoring and diagnostic information were stored in a secure, web-based Research Electronic Data Capture (REDCap) database (version 6.6.2, REDCap, Nashville, TN, USA) for management and analysis [
11].
The CRS and CF groups were compared to the unaffected control group for both APPS and Lund-Mackay scores. Subgroup analysis was then performed for each comparison within both the adolescent and adult subgroups. Separate analysis was conducted within the CRS population for patients with a Lund-Mackay score ≥3, while the control population was limited to individuals with a Lund-Mackay score <3. This value was selected for restricting the two groups since it has previously been described as the incidental score [
12,
13]. The incidental score was determined from patients without sinonasal disorders or facial skeletal trauma [
12,
13], and reflects the degree of sinus opacification that may be encountered in healthy subjects. Continuous variables were analyzed using two-sample independent
t-tests. One-way analysis of variance was used when more than two groups were compared simultaneously.
p-values less than 0.05 were considered significant. Statistical analysis was performed using SAS software (version 9.3, SAS Institute Inc., Cary, NC, USA). The study was approved by the Institutional Research Board of the Ochsner Clinic Foundation.
3. Results
Demographic data for the total study population and each of the subgroups is presented in
Table 2. There were no significant age differences between the CRS cohort and the control group for the total study population, or for the adult and adolescent subgroups. The CF cohort was significantly younger than controls within the adult subgroup (
p < 0.001), but there were no statistical age differences in the total study population or the adolescent subgroup. There were no significant gender differences between the CRS group and controls for the total study population or within the adolescent subgroup. The adult subgroup, however, had significantly more males in the CRS population compared to controls (
p = 0.004). No significant gender differences were found between the CF cohort and controls for the total study population, or within the adult and adolescent subgroups. APPS scores in the entire study group were normally distributed with a mean score of 9.47 and standard deviation of 3.43. Therefore 95% of all scores were between 3 and 16.
APPS scores were significantly higher for CRS patients compared to unaffected controls, and this effect was preserved within both the adult and adolescent subgroups (
Table 3). When the CRS group was restricted to patients with a Lund-Mackay score ≥3 and the control group was restricted to Lund-Mackay scores <3, the CRS group again had a higher mean APPS score (
Table 4). This result reached significance in the adult and adolescent subgroups. According to the normal distribution of APPS scores, the mean CRS score was in the 63rd percentile of all subjects. Subgroup analysis by CRS phenotype did not reveal any statistical difference of sinus pneumatization between patients with CRSwNP, CRSsNP, and AFRS, a finding that was consistent among adults and adolescents (
Table 5). CF patients were found to have decreased sinus pneumatization by the APPS score when compared to healthy controls (
Table 6). Subgroup analysis of adults and adolescents was also significant for sinus hypoplasia in the CF group. The mean APPS score in CF patients was in the 4th percentile of all subjects. As expected, Lund-Mackay scores were higher in the CRS and CF groups compared to unaffected control patients (
Table 3 and
Table 6).
4. Discussion
There appears to be wide variation in paranasal sinus anatomy [
14,
15], but the cause for these differences and their impact on sinonasal disease is unclear. CF is associated with sinus hypoplasia [
2,
3,
4,
5], and is frequently associated with chronic sinus disease [
1,
2]. This raises the relevant question of whether the relationship between sinus pneumatization and mucosal disease can applied as a generalization. This remains incompletely resolved because paranasal sinus pneumatization has been difficult to quantify. Furthermore, while sinus hypoplasia tends to be dramatic in CF, anatomical differences in other disease processes may be more subtle.
Previous studies indicate that while sinus hypoplasia is present in CF, this effect may be independent of mucosal disease. A porcine model of CF indicated that impaired sinus development was present in utero, prior to clinical sinus disease [
2]. Woodworth et al. found that CF patients with homozygous delta F508 mutations had more pronounced underdevelopment of the paranasal sinuses compared to patients with other mutations of the cystic fibrosis transmembrane conductance regulator (
CFTR) gene [
3]. Delta F508 homozygosity has also been associated with increased, rather than impaired, temporal bone pneumatization [
4]. Overall, these findings suggest that mucosal disease is not a sufficient condition alone to explain impaired paranasal sinus development, and genetic abnormalities may underlie sinus hypoplasia.
The role of decreased paranasal sinus pneumatization in the development of CRS is also unclear. Kim et al. found that CRS patients had similar paranasal sinus pneumatization compared to healthy controls, although CF patients demonstrated impaired sinus development [
6]. That study, however, was restricted to volumetric and dimensional analysis of the maxillary sinus in children and adolescents, age 4 to 17. In a study of frontal sinus coronal CT, Meyer et al. indicated that the presence of frontal cells was associated with middle turbinate concha bullosa and hyperpneumatizion of the frontal sinus [
16]. Frontal cells were also found to be associated with increased frontal sinus mucosal thickening [
16]. Alternatively, there have been reports of decreased maxillary sinus volume in patients with CRS [
17,
18]. These studies, however, did not measure the volumes of the other paranasal sinuses or did not find differences outside of the maxillary sinus. On the whole, sinus hypoplasia does not appear to be a universal factor in the development of sinusitis.
In the present study, CRS is associated with increased paranasal sinus pneumatization compared to unaffected controls. This further supports other work suggesting that mucosal disease may not be a sufficient condition for the development of sinus hypoplasia [
2,
3,
4]. Our findings also indicate that impaired sinus pneumatization is not a universal factor in the development of sinusitis, and is consistent with some previous studies of CRS patients [
6,
16]. Paranasal sinus pneumatization was not different between CRS phenotypes (
Table 5). The finding of increased pneumatization does not appear to be restricted to patients with CRSwNP and AFRS where expansile disease might lead to bony remodeling. The novel approach used to quantify paranasal sinus pneumatization, however, distinguishes this study from prior work. Because the APPS score can be performed quickly, this was applied to a large population in order to detect subtle differences between CRS patients and healthy controls. The APPS score is also a comprehensive instrument of variations affecting each of the four paired paranasal sinuses, and is validated for rater reliability. Previous studies have been limited to individual anatomical variations [
16], or volumetric and dimensional analysis of individual sinuses [
6,
17,
18]. Finally, the APPS score simultaneously estimates total paranasal sinus volume, and lower scores are indicative of impaired development globally [
10].
A limitation of this study is that the diagnosis of CRS was discerned retrospectively. Because numerous practitioners, with differing qualifications across a large health system, made the diagnosis, there was likely some degree of inconsistency. While CT findings alone are not diagnostic for CRS, 144 patients who did not have a diagnosis of CRS were found to have Lund-Mackay scores ≥3. Conversely, 27 patients who were diagnosed with CRS had Lund-Mackay scores <3. Nevertheless, the APPS score has only been validated recently and could be easily applied to an existing population for initial impressions on paranasal sinus pneumatization in CRS. The findings were also consistent in a subgroup of patients with both a diagnosis of CRS and radiographic evidence of disease, compared to a cohort without a diagnosis of CRS and no radiographic evidence of disease. Future studies would benefit from a cross-sectional or prospective design for assigning the diagnosis of CRS, and restricting the assignment of that diagnosis to a single physician or group of physicians with advanced training in rhinology. Furthermore, future study would benefit from more sophisticated classification of CRS, rather than the somewhat simplistic delineation of phenotypes according to CRSwNP, CRSsNP, and AFRS. Severe Chronic Upper Airway Disease (SCUAD) has been described to highlight that complex pathophysiological mechanisms contribute to sinonasal mucosal inflammatory disease [
19]. Observed anatomical differences may be a manifestation of disease categorization that is only recently being acknowledged. Another limitation of this study is that in the adult subgroup there were significantly more males than females in the CRS group compared to the control population (
Table 2). This may confound the finding that CRS patients have increased sinus pneumatization, since this might be attributable to male gender. The result, however, was reproducible in the adolescent subgroup and total study population, in which there were no significant differences in gender between the CRS population and unaffected patients.