The Impact of Endonasal Endoscopic Sinus Surgery on Patients with Chronic Pulmonary Diseases
Abstract
:1. Introduction
2. Materials and Methods
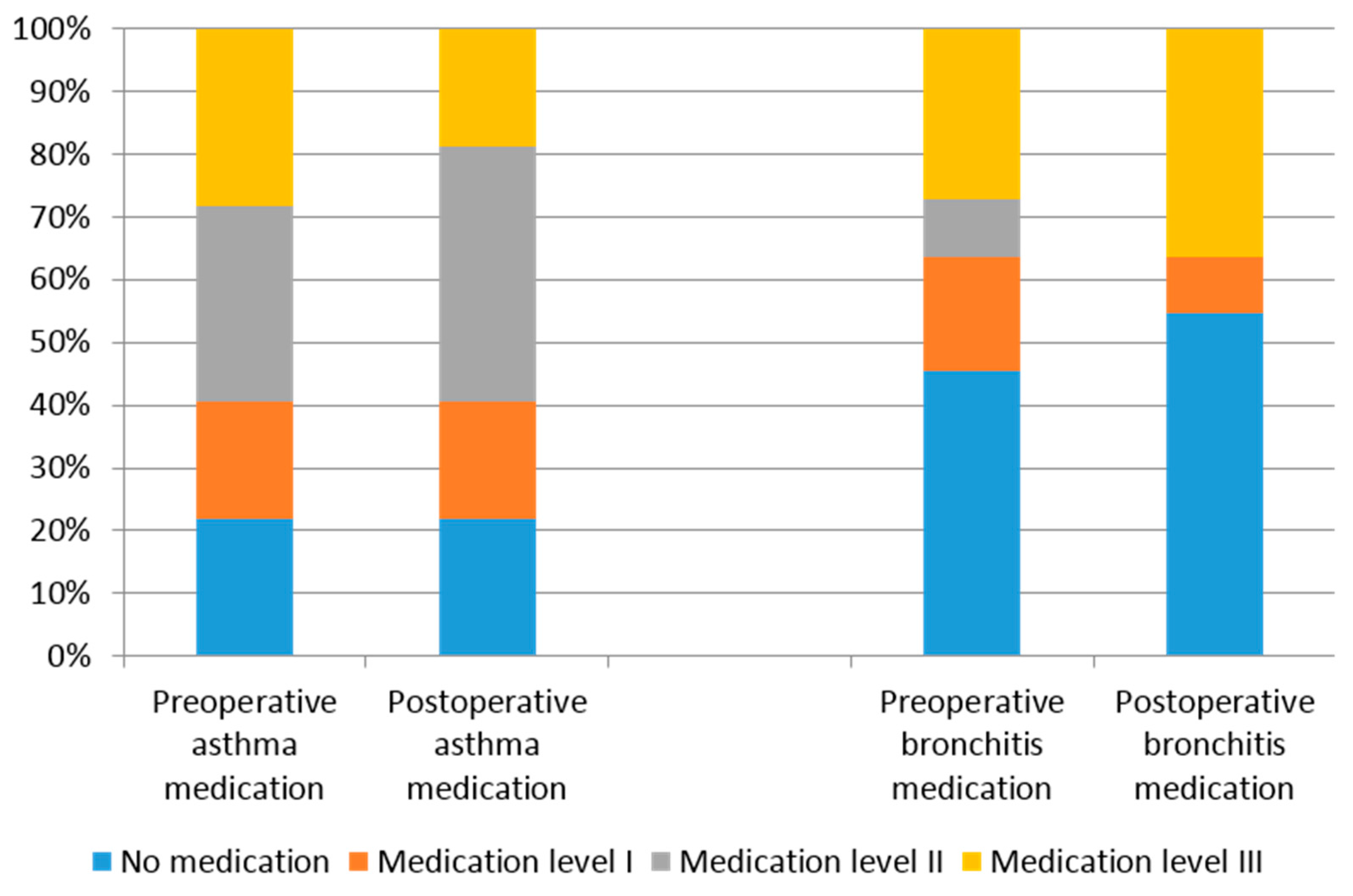
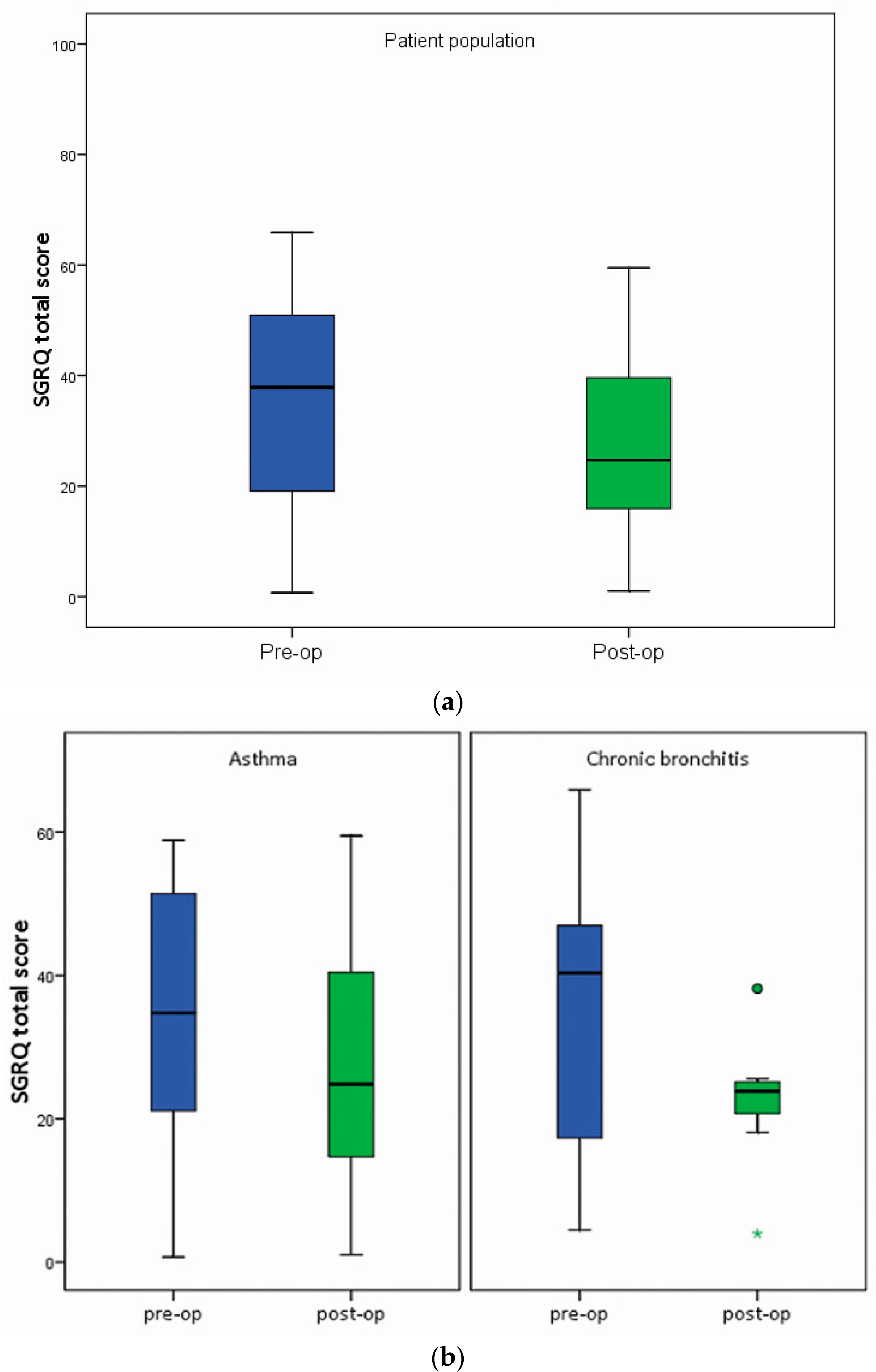
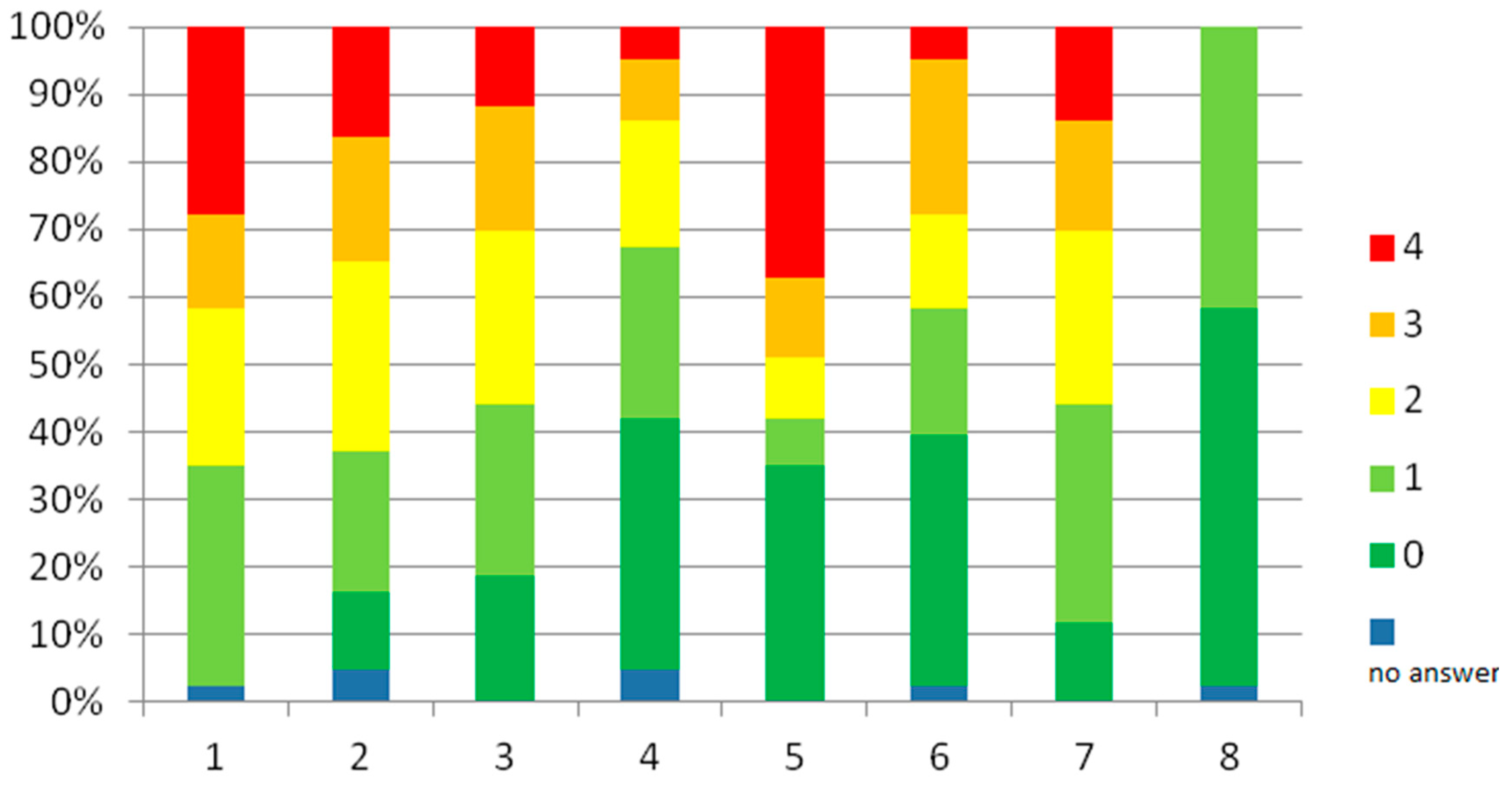
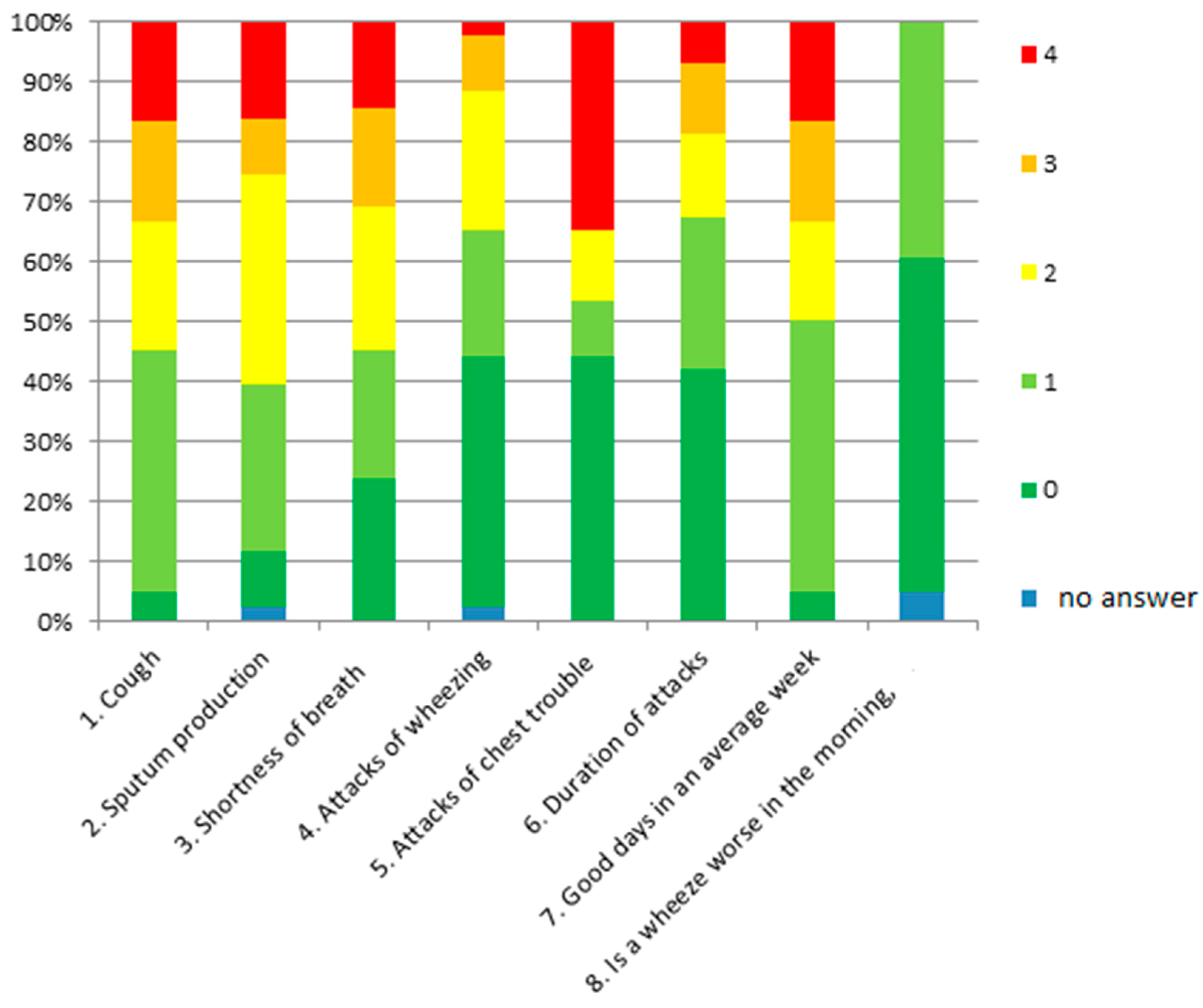
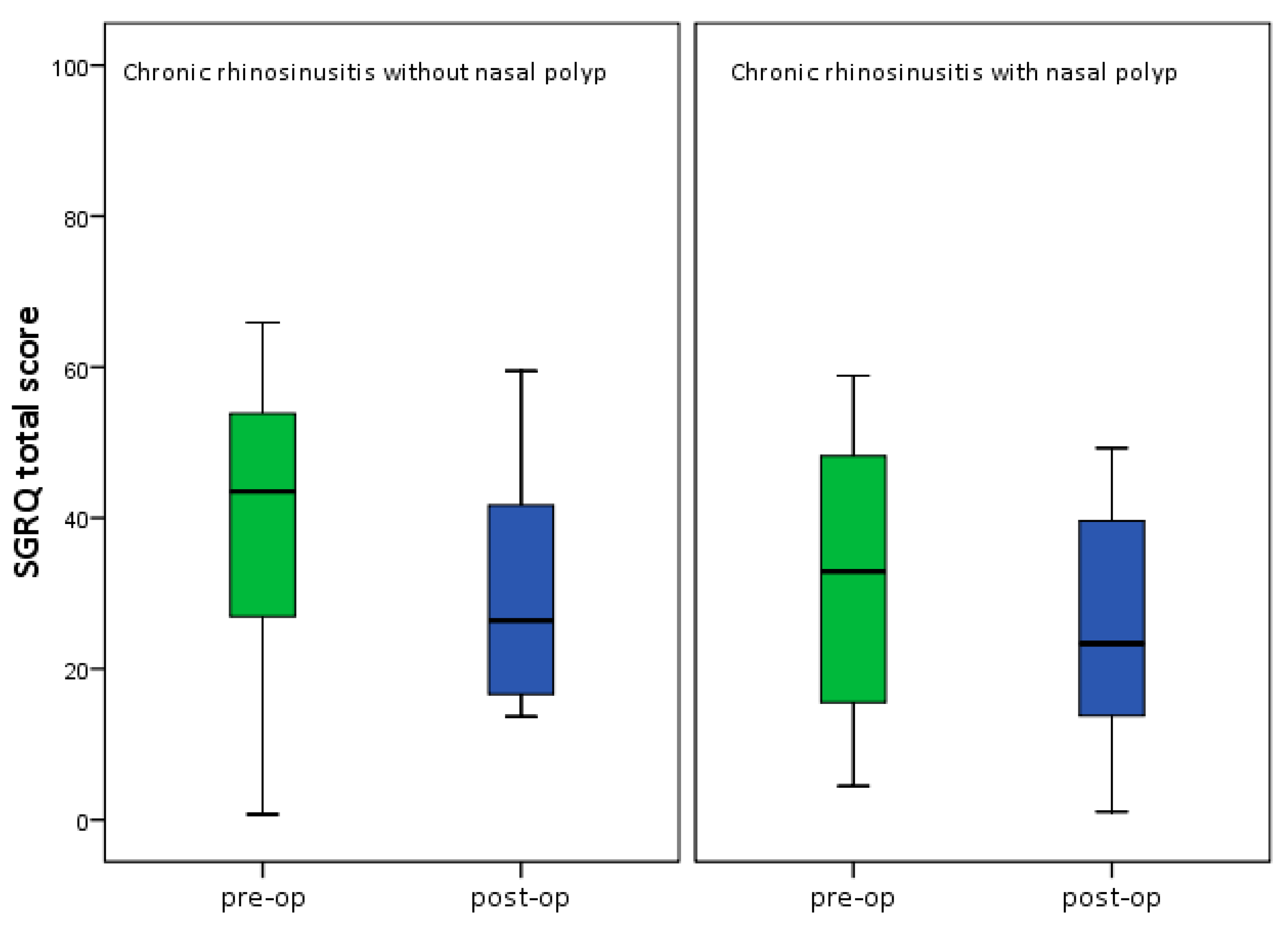
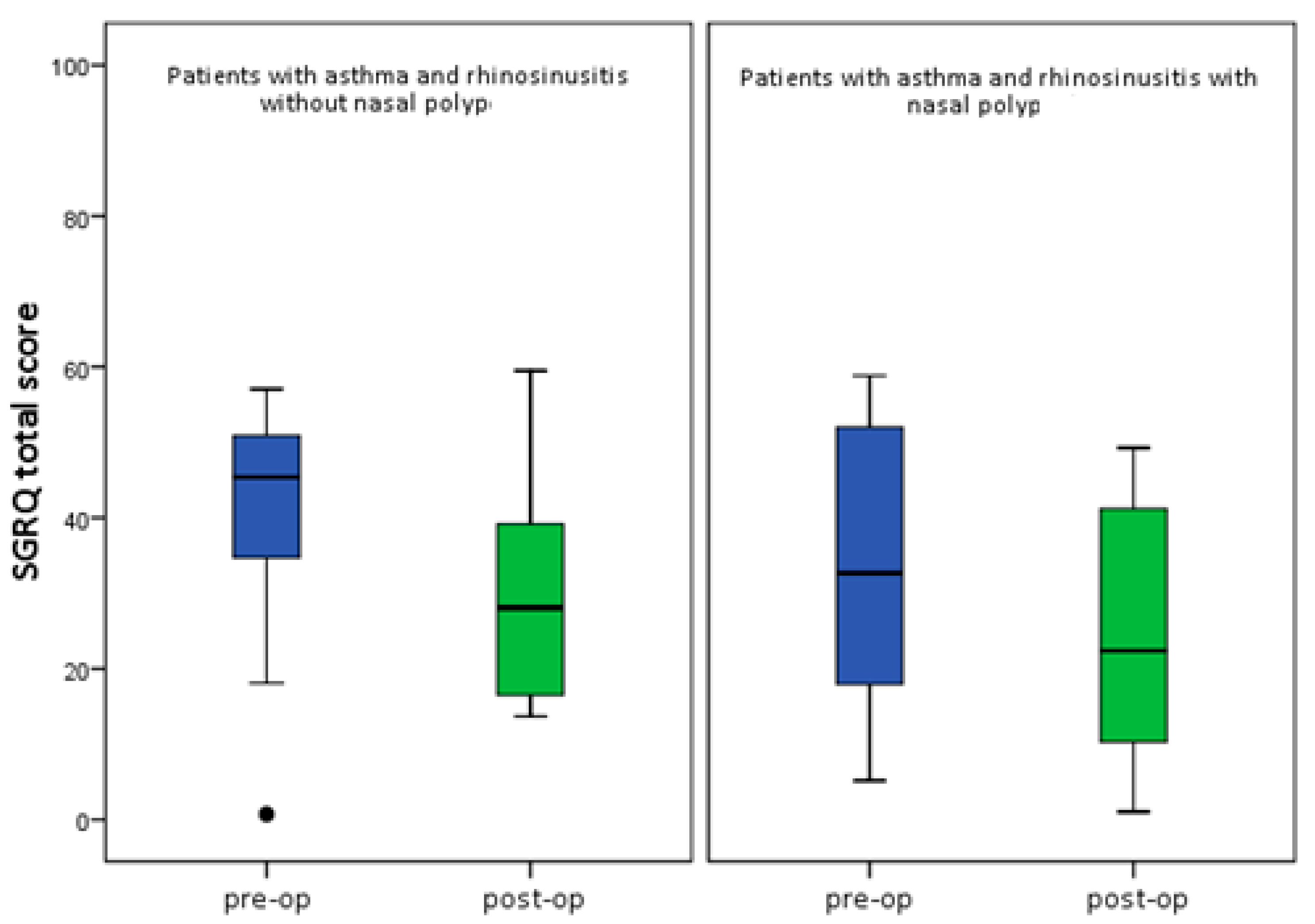
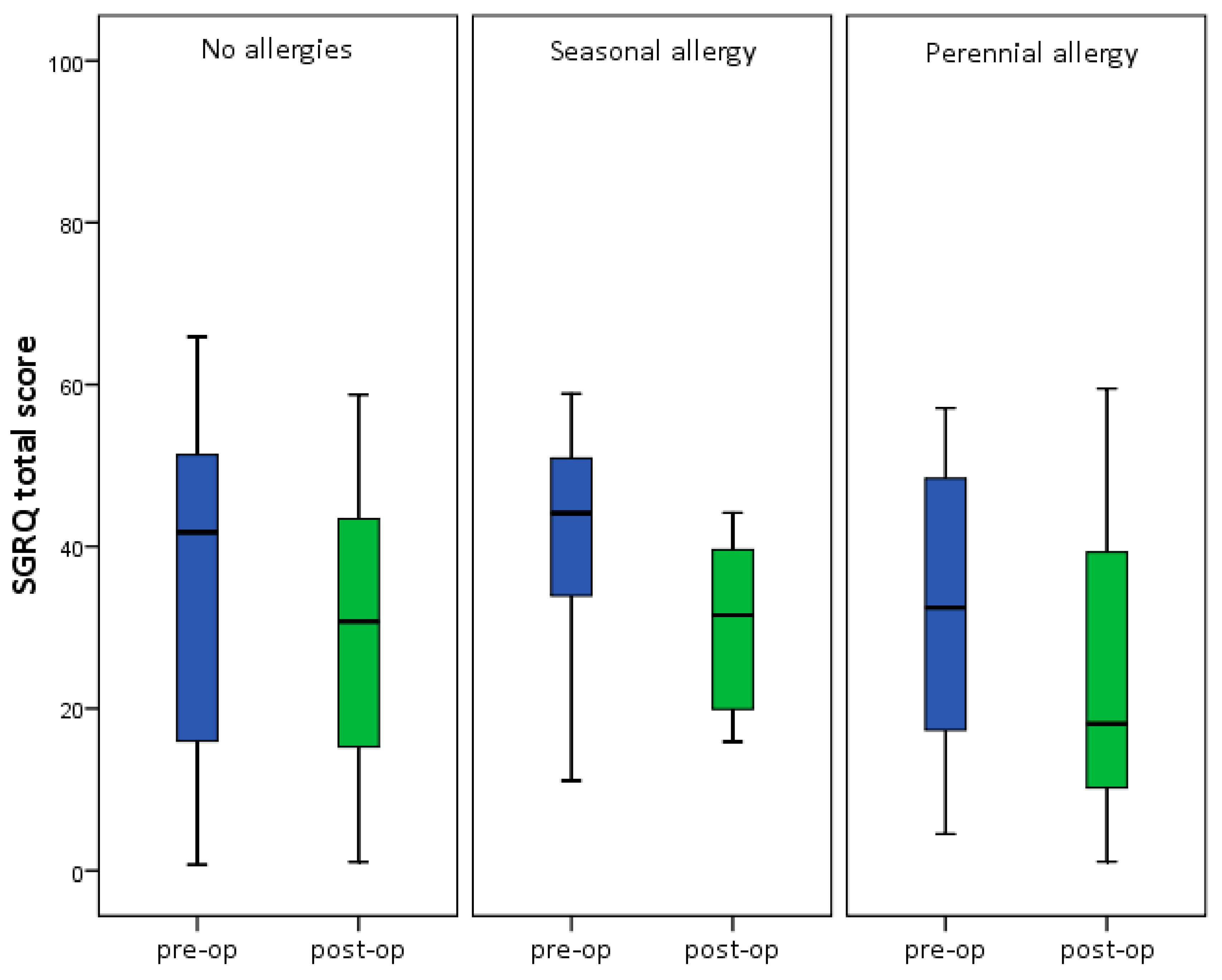
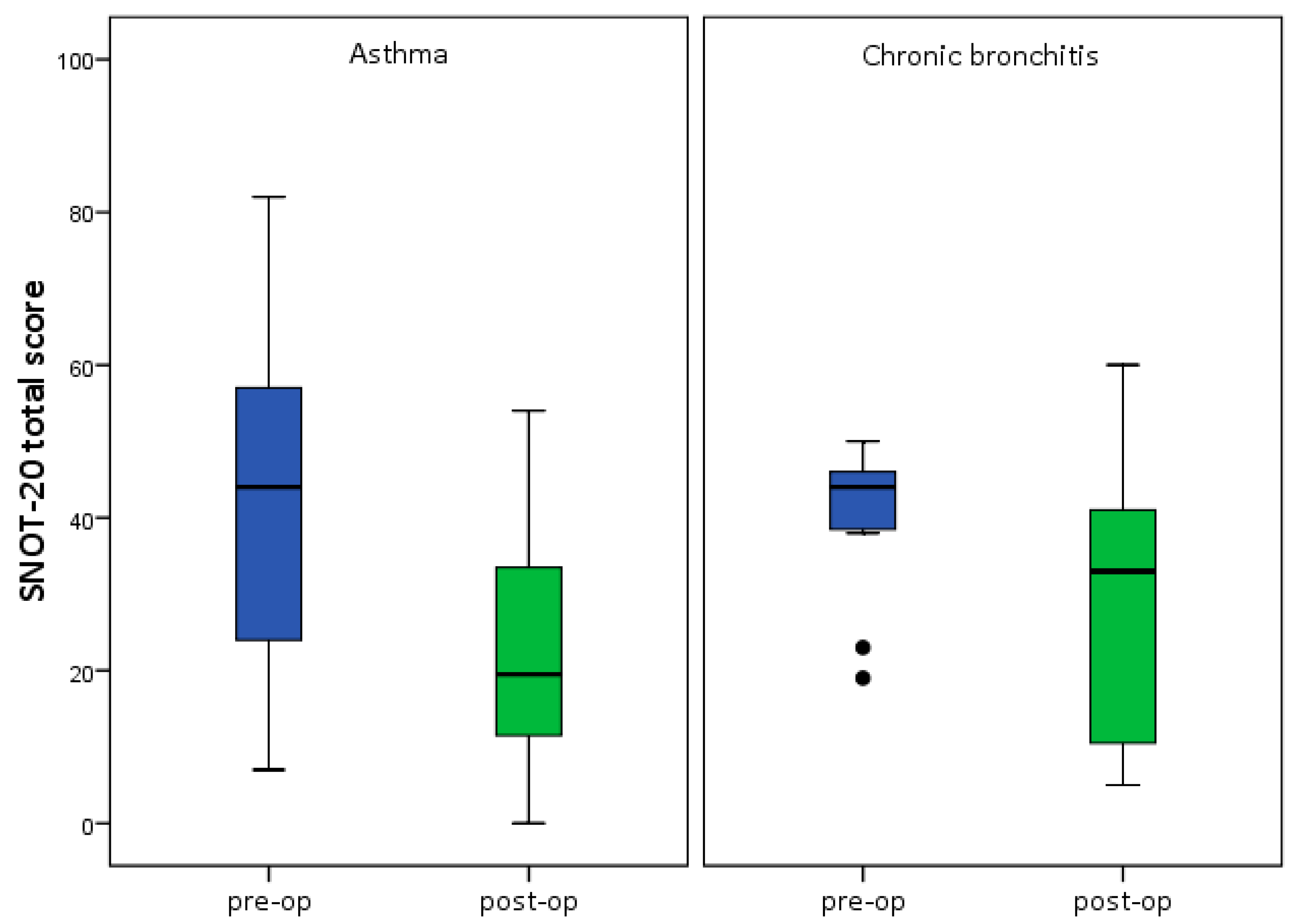
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Huzly, A. Sinobronchial Syndrome. Beitr. Klin. Tuberk. 1969, 139, 265–282. [Google Scholar] [CrossRef]
- Singleton, M.A. The sinobronchial syndrome: An old fashioned, modern-day entity. South Med. J. 1971, 64, 754–756. [Google Scholar] [CrossRef] [PubMed]
- Stuck, B.A.; Bachert, C.; Federspil, P.; Hosemann, W.; Klimek, L.; Mösges, R.; Pfaar, O.; Rudack, C.; Sitter, H.; Wagenmann, M.; et al. German Society of Otorhinolaryngology, Head and Neck Surgery. Rhinosinusitis guidelines—unabridged version: S2 guidelines from the German Society of Otorhinolaryngology, Head and Neck Surgery. HNO 2012, 60, 141–162. [Google Scholar] [CrossRef] [PubMed]
- Ehnhage, A.; Olsson, P.; Kolbeck, K.G.; Skedinger, M.; Stjärne, P. One year after endoscopic sinus surgery in polyposis: Asthma, olfaction, and quality-of-life outcomes. Otolaryngol. Head Neck Surg. 2012, 146, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Hurst, J.R.; Perera, W.R.; Wilkinson, T.M.; Donaldson, G.C.; Wedzicha, J.A. Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2006, 173, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Hens, G.; Vanaudenaerde, B.M.; Bullens, D.M.A.; Piessens, M.; Decramer, M.; Dupont, L.J.; Hellings, P.W. Sinonasal pathology in nonallergic asthma and COPD: “United airway disease” beyond the scope of allergy. Allergy 2008, 63, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Piotrowska, V.M.; Piotrowski, W.J.; Kurmanowska, Z.; Marczak, J.; Górski, P.; Antczak, A. Rhinosinusitis in COPD: Symptoms, mucosal changes, nasal lavage cells and eicosanoids. Int. J. Chronic Obstr. Pulm. Dis. 2010, 5, 107–117. [Google Scholar]
- Kelemence, A.; Abadoglu, O.; Gumus, C.; Berk, S.; Epozturk, K.; Akkurt, I. The Frequency of Chronic Rhinosinusitis/Nasal Polyp in COPD and Its Effect on the Severity of COPD. COPD J. Chronic Obstr. Pulm. Dis. 2011, 8, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Rubin, B.K. Nasal and sinus inflammation in chronic obstructive pulmonary disease. COPD 2007, 4, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Al Kadah, B.; Bumm, K.; Charalampaki, P.; Schick, B. First experience in endonasal surgery using a new 3D-Chipendoscope Laryngorhinootologie. Laryngo-Rhino-Otol. 2012, 91, 428–433. [Google Scholar]
- Jones, P.W. St. George’s Respiratory Questionnaire: MCID. COPD J. Chronic Obstr. Pulm. Dis. 2005, 2, 75–79. [Google Scholar] [CrossRef]
- Piccirillo, J.F.; Merritt, M.G., Jr.; Richards, M.L. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol. Head Neck Surg. 2002, 126, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Baumann, I.; Blumenstock, G.; DeMaddalena, H.; Piccirillo, J.F.; Plinkert, P.K. Quality of life in patients with chronic rhinosinusitis Validation of the Sino-Nasal Outcome Test-20 German Adapted Version. HNO 2007, 55, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur. Respir. J. 2002, 19, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Loehrl, T.A.; Ferre, R.M.; Toohill, R.J.; Smith, T.L. Long-term asthma outcomes after endoscopic sinus surgery in aspirin triad patients. Am. J. Otolaryngol. 2006, 27, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Stahl, E.; Lindberg, A.; Jansson, S.-A.; Rönmark, E.; Svensson, K.; Andersson, F.; Lundbäck, B. Health-related quality of life is related to COPD disease severity. Health Qual. Life Outcomes 2005, 3, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Dejima, K.; Hama, T.; Miyazaki, M.; Yasuda, S.; Fukushima, K.; Oshima, A.; Hisa, Y. A clinical study of endoscopic sinus surgery for sinusitis in patients with bronchial asthma. Int. Arch. Allergy Immunol. 2005, 138, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Uri, N.; Cohen-Kerem, R.; Barzilai, G.; Greenberg, E.; Doweck, I.; Weiler-Ravell, D. Functional endoscopic sinus surgery in the treatment of massive polyposis in asthmatic patients. J. Laryngol. Otol. 2002, 116, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Batra, P.S.; Kern, R.C.; Tripathi, A.; Conley, D.B.; Ditto, A.M.; Haines, G.K.; Grammar, L. Outcome analysis of endoscopic sinus surgery in patients with nasal polyps and asthma. Laryngoscope 2003, 113, 1703–1706. [Google Scholar] [CrossRef] [PubMed]
- Hosemann, W.; Wigand, M.E.; Gode, U.; Linger, F.; Dunker, I. Normal wound healing of the paranasal sinuses: Clinical and experimental investigations. Eur. Arch. Otorhinolaryngol. 1991, 248, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Baumann, I.; Blumenstock, G.; Praetorius, M.; Sittel, C.; Piccirillo, J.F.; Plinkert, P.K. Patients with chronic rhinosinusitis: Disease-specific and general health-related quality of life. HNO 2006, 54, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Slack, R.; Lund, V.; Brown, P.; Copley, L.; Browne, J. Long-term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Laryngoscope 2009, 119, 2459–2465. [Google Scholar] [CrossRef] [PubMed]
- Partridge, M.R.; Dal Negro, R.W.; Olivieri, D. Understanding patients with asthma and COPD: Insights from a European study. Prim. Care Respir. J. 2011, 20, 315–323. [Google Scholar] [CrossRef] [PubMed]
- May, A.; Wagner, D.; Langenbeck, U.; Weber, A. Family study of patients with aspirin intolerance and rhinosinusitis. HNO 2000, 9, 650–655. [Google Scholar] [CrossRef]
- Bourdin, A.; Gras, D.; Vachier, I.; Chanez, P. Upper airway 1: Allergic rhinitis and asthma: United disease through epithelial cells. Thorax 2009, 64, 999–1004. [Google Scholar] [CrossRef] [PubMed]
- Ciprandi, G.; Cirillo, I.; Vizzaccaro, A.; Milanese, M.; Tosca, M.A. Airway function and nasal inflammation in seasonal allergic rhinitis and asthma. Clin. Exp. Allergy 2004, 34, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Awad, O.G.; Lee, J.H.; Fasano, M.B.; Graham, S.M. Sinonasal outcomes after endoscopic sinus surgery in asthmatic patients with nasal polyps: A difference between aspirin-tolerant and aspirin-induced asthma? Laryngoscope 2008, 118, 1282–1286. [Google Scholar] [CrossRef] [PubMed]
- Vogelmeier, C.; Buhl, R.; Criee, C.P.; Gillissen, A.; Kardos, P.; Köhler, D.; Magnussen, H.; Morr, H.; Nowak, D.; Pfeiffer−Kascha, D.; et al. Leitlinie der Deutschen Atemwegsliga und der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin zur Diagnostik und Therapie von Patienten mit chronisch obstruktiver Bronchitis und Lungenemphysem (COPD). Pneumologie 2007, 61, e1–e40. (In German) [Google Scholar] [CrossRef] [PubMed]
- Ashraf, N.; Bhattacharyya, N. Determination of the “incidental” Lund scores for the staging of chronic rhinosinusitis. Otolaryngol. Head Neck Surg. 2001, 125, 483–486. [Google Scholar] [CrossRef]
- Baumann, I.; Blumenstock, G.; Zalaman, I.M.; Praetorius, M.; Klingmann, C.; Sittel, C.; Piccirillo, J.F. Impact of gender, age, and comorbidities on quality of life in patients with chronic rhinosinusitis. Rhinology 2007, 45, 268–272. [Google Scholar] [PubMed]
- Bradley, D.T.; Kountakis, S.E. Correlation between computed tomography scores and symptomatic improvement after endoscopic sinus surgery. Laryngoscope 2005, 115, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Bonfils, P.; Tavernier, L.; Abdel Rahman, H.; Mimoun, M.; Malinvaud, D. Evaluation of combined medical and surgical treatment in nasal polyposis—III. Correlation between symptoms and CT scores before and after surgery for nasal polyposis. Acta Otolaryngol. 2008, 128, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Kountakis, S.E.; Bradley, D.T. Effect of asthma on sinus computed tomography grade and symptom scores in patients undergoing revision functional endoscopic sinus surgery. Am. J. Rhinol. 2003, 17, 215–219. [Google Scholar] [PubMed]
- Lee, J.Y.; Lee, S.W.; Lee, J.D. Comparison of the surgical outcome between primary and revision endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Am. J. Otolaryngol. 2008, 29, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Seyring, C.; Bitter, T.; Boger, D.; Büntzel, J.; Esser, D.; Hoffmann, K.; Guntinas-Lichius, O. Health Services Research on Paranasal Sinus Surgery in Thuringia: Epidemiologic Key Data and Outcome. Laryngorhinootologie 2012, 91, 434–439. [Google Scholar] [PubMed]
- Smith, T.L.; Mendolia-Loffredo, S.; Loehrl, T.A.; Sparapani, R.; Laud, P.W.; Nattinger, A.B. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 2005, 115, 2199–2205. [Google Scholar] [CrossRef] [PubMed]
- Gosepath, J.; Pogodsky, T.; Mann, W.J. Characteristics of recurrent chronic rhinosinusitis after previous surgical therapy. Acta Otolaryngol. 2008, 128, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Seybt, M.W.; McMains, K.C.; Kountakis, S.E. The prevalence and effect of asthma on adults with chronic rhinosinusitis. Ear Nose Throat J. 2007, 86, 409–411. [Google Scholar] [PubMed]
- Wilkinson, T.M.; Patel, I.S.; Wilks, M.; Donaldson, G.C.; Wedzicha, J.A. Airway bacterial load and FEV1 decline in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2003, 167, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Hosemann, W. Postoperative measures to prevent recurrence of chronic pansinusitis and polyposis nasi. HNO 2003, 51, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, T.F.; Piccirillo, J.F.; Fornazieri, M.A.; Pilan, R.R.D.M.; Pinna, F.D.R.; Padua, F.G.D.M.; Voegels, R.L. Assessment of quality of life after endoscopic sinus surgery for chronic rhinosinusitis. Braz. J. Otorhinolaryngol. 2012, 78, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Ling, F.T.; Kountakis, S.E. Important clinical symptoms in patients undergoing functional endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 2007, 117, 1090–1093. [Google Scholar] [CrossRef] [PubMed]



| Symptom | Pre-op (Ø) | Post-op (Ø) | p-value |
|---|---|---|---|
| Need to blow nose | 2.51 ± 1.4 | 1.44 ± 1.2 | <0.001 |
| Sneezing | 2.00 ± 1.5 | 0.93 ± 0.9 | <0.001 |
| Runny nose | 2.21 ± 1.6 | 1.00 ± 1.1 | <0.001 |
| Cough | 2.23 ± 1.6 | 1.67 ± 1.5 | 0.010 |
| Postnasal discharge | 2.72 ± 1.7 | 1.67 ± 1.4 | 0.001 |
| Thick nasal discharge | 2.67 ± 1.6 | 1.49 ± 1.4 | <0.001 |
| Ear fullness | 1.91 ± 1.5 | 0.81 ± 1.2 | <0.001 |
| Dizziness | 1.16 ± 1.4 | 0.67 ± 1.1 | 0.005 |
| Ear pain | 0.93 ± 1.1 | 0.51 ± 0.8 | 0.033 |
| Facial pain/pressure | 2.37 ± 1.8 | 1.12 ± 1.2 | <0.001 |
| Difficulty falling asleep | 1.88 ± 1.7 | 1.26 ± 1.5 | 0.003 |
| Wake up at night | 2.60 ± 1.3 | 1.74 ± 1.4 | <0.001 |
| Lack of a good night’s sleep | 2.81 ± 1.6 | 1.53 ± 1.5 | <0.001 |
| Wake up tired | 2.49 ± 1.6 | 1.65 ± 1.5 | 0.001 |
| Fatigue | 2.70 ± 1.6 | 1.70 ± 1.2 | <0.001 |
| Reduced productivity | 2.47 ± 1.6 | 1.60 ± 1.4 | 0.001 |
| Reduced concentration | 2.14 ± 1.5 | 1.21 ± 1.2 | <0.001 |
| Frustrated/restless/irritable | 2.14 ± 1.5 | 1.09 ± 1.2 | <0.001 |
| Sad | 1.65 ± 1.6 | 0.84 ± 1.1 | 0.001 |
| Embarrassed | 1.02 ± 1.4 | 0.42 ± 0.8 | <0.001 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Kadah, B.; Helmus, G.; Dinh, Q.T.; Schick, B. The Impact of Endonasal Endoscopic Sinus Surgery on Patients with Chronic Pulmonary Diseases. Sinusitis 2017, 2, 4. https://doi.org/10.3390/sinusitis2020004
Al Kadah B, Helmus G, Dinh QT, Schick B. The Impact of Endonasal Endoscopic Sinus Surgery on Patients with Chronic Pulmonary Diseases. Sinusitis. 2017; 2(2):4. https://doi.org/10.3390/sinusitis2020004
Chicago/Turabian StyleAl Kadah, Basel, Gudrun Helmus, Quoc Thai Dinh, and Bernhard Schick. 2017. "The Impact of Endonasal Endoscopic Sinus Surgery on Patients with Chronic Pulmonary Diseases" Sinusitis 2, no. 2: 4. https://doi.org/10.3390/sinusitis2020004





