Fluconazole Resistance among Oral Candida Isolates from People Living with HIV/AIDS in a Nigerian Tertiary Hospital
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Participants’ Characteristics
3.2. Species Distribution and Fluconazole Susceptibility of Isolates
3.3. Fluconazole Resistance and Associated Factors
3.4. Control Subjects
4. Discussion
Supplementary Materials
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Barr, C.E. Oral diseases in HIV-1 infection. Dysphagia 1992, 7, 126–137. [Google Scholar] [CrossRef] [PubMed]
- Farah, C.S.; Ashman, R.B.; Challacombe, S.J. Oral candidosis. Clin. Dermatol. 2000, 18, 553–562. [Google Scholar] [CrossRef]
- Salerno, C.; Di Stasio, D.; Petruzzi, M.; Lauritano, D.; Gentile, E.; Guida, A.; Maio, C.; Tammaro, M.; Serpico, R.; Lucchese, A. An overview of burning mouth syndrome. Front. Biosci. (Elite Ed.) 2016, 8, 213–218. [Google Scholar]
- Moyes, D.L.; Naglik, J.R. Mucosal immunity and Candida albicans infection. Clin. Dev. Immun. 2011, 2011, 346307. [Google Scholar]
- Patel, K.P.; Erlandsen, J.E.; Kirkpatrick, W.R.; Berg, D.K.; Westbrook, S.D.; Louden, C.; Cornell, J.E.; Thompson, G.R.; Vallor, A.C.; Wickes, B.L.; et al. The changing epidemiology of oropharyngeal candidiasis in patients with HIV/AIDS in the era of antiretroviral therapy. AIDS Res. Treat. 2012, 2012, 262471. [Google Scholar] [CrossRef] [PubMed]
- Barchiesi, F.; Morbiducci, V. Emergence of oropharyngeal candidiasis caused by non-albicans species of Candida in HIV-infected patients. Eur. J. Epidemiol. 1993, 9, 455–456. [Google Scholar] [CrossRef] [PubMed]
- Hamza, O.J.; Matee, M.I.; Moshi, M.J.; Simon, E.N.; Mugusi, F.; Mikx, F.H.; Helderman, W.H.; Rijs, A.J.; van der Ven, A.J.; Verweij, P.E. Species distribution and in vitro antifungal susceptibility of oral yeast isolates from Tanzanian HIV-infected patients with primary and recurrent oropharyngeal candidiasis. BMC Microbiol. 2008, 8, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-infected Adults and Adolescents. Recommendations from CDC, the National Institutes of Health and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Morb. Mortal. Wkly. Rep. 2009, 58, 45–48. [Google Scholar]
- Pappas, P.G.; Kaufmann, C.A.; Andes, D.; Benjamin, D.K., Jr.; Calandra, T.F.; Edwards, J.E., Jr.; Filler, S.G.; Fisher, J.F.; Kullberg, B.J.; Ostrosky-Zeichner, L.; et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Disease Society of America. Clin. Infect. Dis. 2009, 48, 503–535. [Google Scholar] [CrossRef] [PubMed]
- Vandeputte, P.; Ferrari, S.; Coste, A.T. Antifungal resistance and new strategies to control fungal infections. Int. J. Microbiol. 2012, 2012, 713687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Agency for the Control of AIDS (NACA). Federal Republic of Nigeria Global AIDS Response Country Progress Report; Nigeria GARPR: Abuja, Nigeria, 2015; p. 38. Available online: http://www.unaids.org/sites/default/files/country/documents/NGA_narrative_report_2015.pdf (accessed on 12 October 2017).
- Messeir, I.; Abrantes, P.; Africa, C.W.J. Strengths and limitations of different chromogenic media for the identification of Candida species. J. Microbiol. Res. 2012, 2, 133–140. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Reference method for antifungal disc diffusion susceptibility testing of yeasts. In Approved Guideline. (M44-A2), 2nd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2009. [Google Scholar]
- Lar, P.M.; Pam, V.K.; Tiri, Y.; Olukose, S.; Yusuf, A.; Dashen, M.M.; Mawak, J.D. Prevalence and distribution of Candida species in HIV infected persons on antiretroviral therapy in Jos. J. Med. Med. Sci. 2012, 3, 254–259. [Google Scholar]
- Okonkwo, E.C.; Alo, M.N.; Nworie, O.; Orji, J.O.; Agah, M.V. Prevalence of oral Candida albicans infections in HIV seropositive patients in Abakaliki. Am. J. Life Sci. 2013, 1, 72–76. [Google Scholar]
- Nweze, E.I.; Ogbonnaya, U.L. Oral Candida isolates among HIV-infected subjects in Nigeria. J. Microbiol. Immunol. Infect. 2011, 44, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Enwuru, C.A.; Ogunledun, A.; Idika, N.; Enwuru, N.V.; Ogbonna, F.; Aniebode, M. Fluconazole resistant opportunistic oropharyngeal Candida and non-Candida yeast-like isolates from HIV infected patients attending ARV clinics in Lagos, Nigeria. Afr. Health Sci. 2008, 8, 142–148. [Google Scholar]
- Barry, A.L.; Pfaller, M.A.; Rennie, R.P.; Fuchs, P.C.; Brown, S.D. Precision and accuracy of fluconazole susceptibility testing by broth microdilution, Etest, and disc diffusion methods. Antimicrob. Agent. Chemother. 2002, 46, 1781–1784. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J.; Messer, S.A.; Boyken, L.; Hollis, R.J. Activities of fluconazole and voriconazole against 1,586 recent clinical isolates of Candida species determined by broth microdilution, disc diffusion and Etest methods: Report from the ARTEMIS global antifungal susceptibility programme, 2001. J. Clin. Microbiol. 2003, 41, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- Enwuru, C.A.; Ogunledun, A.; Idika, N.; Enwuru, N.V. Susceptibility profile of yeast-like organisms isolated from HIV/AIDS patients: Using NCCLS macrodilution method compared with agar diffusion technique. Afr. J. Clin. Exp. Microbiol. 2008, 8, 88–96. [Google Scholar] [CrossRef]
- Abrantes, P.M.; McArthur, C.P.; Africa, C.W. Multi-drug resistant (MDR) oral Candida species isolated from HIV-positive patients in South Africa and Cameroon. Diagn. Microbiol. Infect. Dis. 2014, 79, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Mulu, A.; Kassu, A.; Anagaw, B.; Moges, B.; Gelaw, A.; Alemayehu, M.; Belyhun, Y.; Biadglegne, F.; Hurissa, Z.; Moges, F.; et al. Frequent detection of azole resistant Candida species amongst late-presenting AIDS patients in northwest Ethiopia. BMC Infect. Dis. 2013, 13, 82. [Google Scholar] [CrossRef] [PubMed]
- Wabe, N.T.; Hussein, J.; Suleman, S.; Abdella, K. In vitro antifungal susceptibility of Candida albicans isolates from oral cavities of patients infected with human immunodeficiency virus in Ethiopia. J. Exp. Integr. Med. 2011, 1, 265–271. [Google Scholar] [CrossRef]
- Satana, D.; Genc, G.E.; Ertuan, Z. The antifungal susceptibilities of oral Candida species isolates from HIV-infected patients. Afr. J. Microbiol. Res. 2010, 4, 466–470. [Google Scholar]
- Aher, C.S. Species distribution, virulence factors and antifungal susceptibility profile of Candida isolated from oropharyngeal lesions of HIV infected patients. Int. J. Curr. Microbiol. App. Sci. 2014, 3, 453–460. [Google Scholar]
- Wu, C.J.; Lee, H.C.; Yang, Y.L.; Chang, C.M.; Chen, H.T.; Lin, C.C.; Lee, N.Y.; Chu, W.L.; Hsieh, L.Y.; Wang, Y.L.; et al. Oropharyngeal yeast colonization in HIV-infected outpatients in Southern Taiwan: CD4count, efavirenz therapy and intravenous drug use matter. Clin. Microbiol. Infect. 2012, 18, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.Y.; Chen, W.Y.; Li, X.; Li, H.B.; Li, H.Q.; Wang, L.; He, L.; Yang, X.P.; Wang, X.C.; Huang, Y.L.; et al. Asymptomatic oral yeast carriage and antifungal susceptibility profile of HIV-infected patients in Kunming, Yunnan province of China. BMC Infect. Dis. 2013, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekma, D.J. Twelve years of fluconazole in clinical practice: Global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin. Microbiol. Infect. 2004, 10, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.J.; Gonzalez, C.E.; Piscitelli, S.; Bacher, J.D.; Peter, J.; Torres, R.; Shetti, D.; Katsov, V.; Kligys, K.; Lyman, C.A. Correlation between in vitro and in vivo antifungal activities in experimental fluconazole-resistant oropharyngeal and esophageal candidiasis. J. Clin. Microbiol. 2000, 38, 2369–2373. [Google Scholar] [PubMed]
- Rex, J.H.; Pfaller, M.A. Has antifungal susceptibility testing come of age? Clin. Infect. Dis. 2002, 35, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Kanafani, Z.A.; Perfect, J.R. Resistance to antifungal agents: Mechanisms and clinical impact. Clin. Infect. Dis. 2008, 46, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Odds, F.C. Should resistance to azole antifungals in vitro be interpreted as predicting clinical non-response? Drug Resist. Updates 1998, 1, 11–15. [Google Scholar] [CrossRef]
- Joshua, E.M. Issues in antifungal susceptibility testing. J. Antimicrob. Chemother. 2008, 61, 13–18. [Google Scholar]
| Candida Species | Sensitivity to Fluconazole Frequency (%) | ||
|---|---|---|---|
| Sensitive n = 53 | S-DD 1 n = 4 | Resistant n = 18 | |
| C. albicans | 47 (90.4) | 3 (75.0) | 11 (61.1) |
| C. glabrata | 1 (1.9) | 0 (0.0) | 3 (16.7) |
| C. krusei | 0 (0.0) | 0 (0.0) | 2 (11.1) |
| C. parapsilosis | 3 (5.7) | 1 (25.0) | 1 (5.6) |
| C. tropicalis | 1 (1.9) | 0 (0.0) | 1 (5.6) |
| C. famata | 1 (1.9) | 0 (0.0) | 0 (0.0) |
| Variable | Resistant Isolate n = 18 | Sensitive/S-DD 1 Isolate n = 57 | χ² | p-Value |
|---|---|---|---|---|
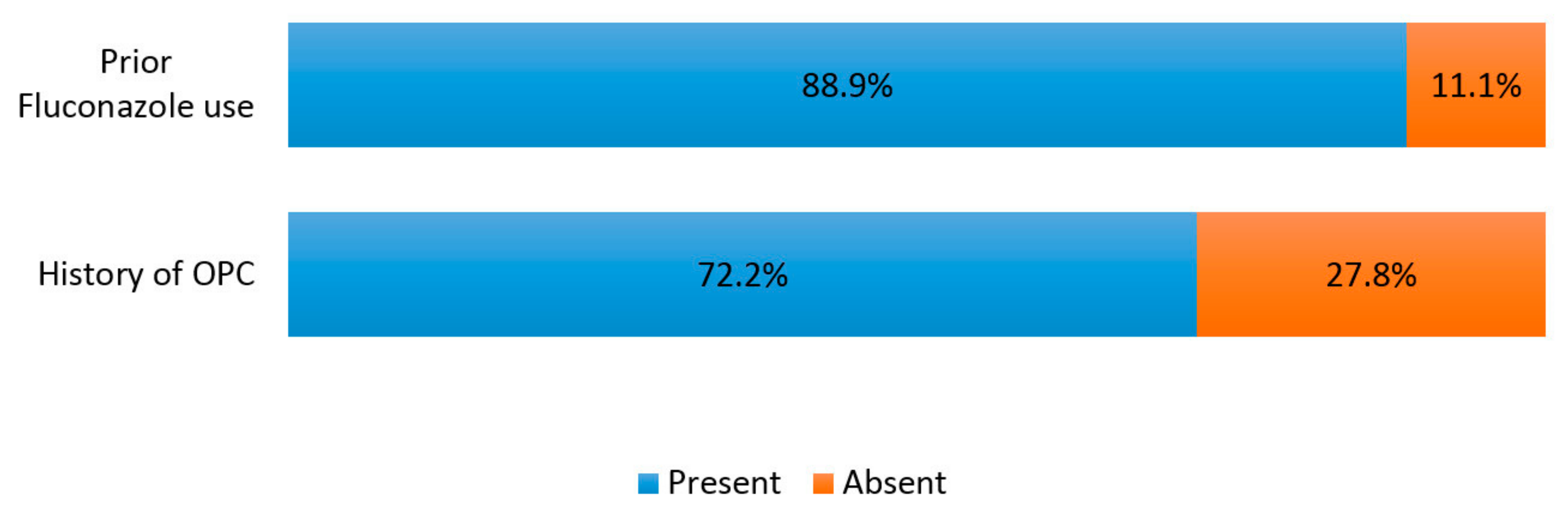
| Past Fluconazole Use | ||||
| Present | 16 (48.5) | 17 (51.5) | 19.368 | <0.001 |
| Absent | 2 (4.8) | 40 (95.2) | ||
| History of OPC | ||||
| Present | 13 (41.9) | 18 (58.1) | 9.319 | 0.002 |
| Absent | 5 (11.4) | 39 (88.6) | ||
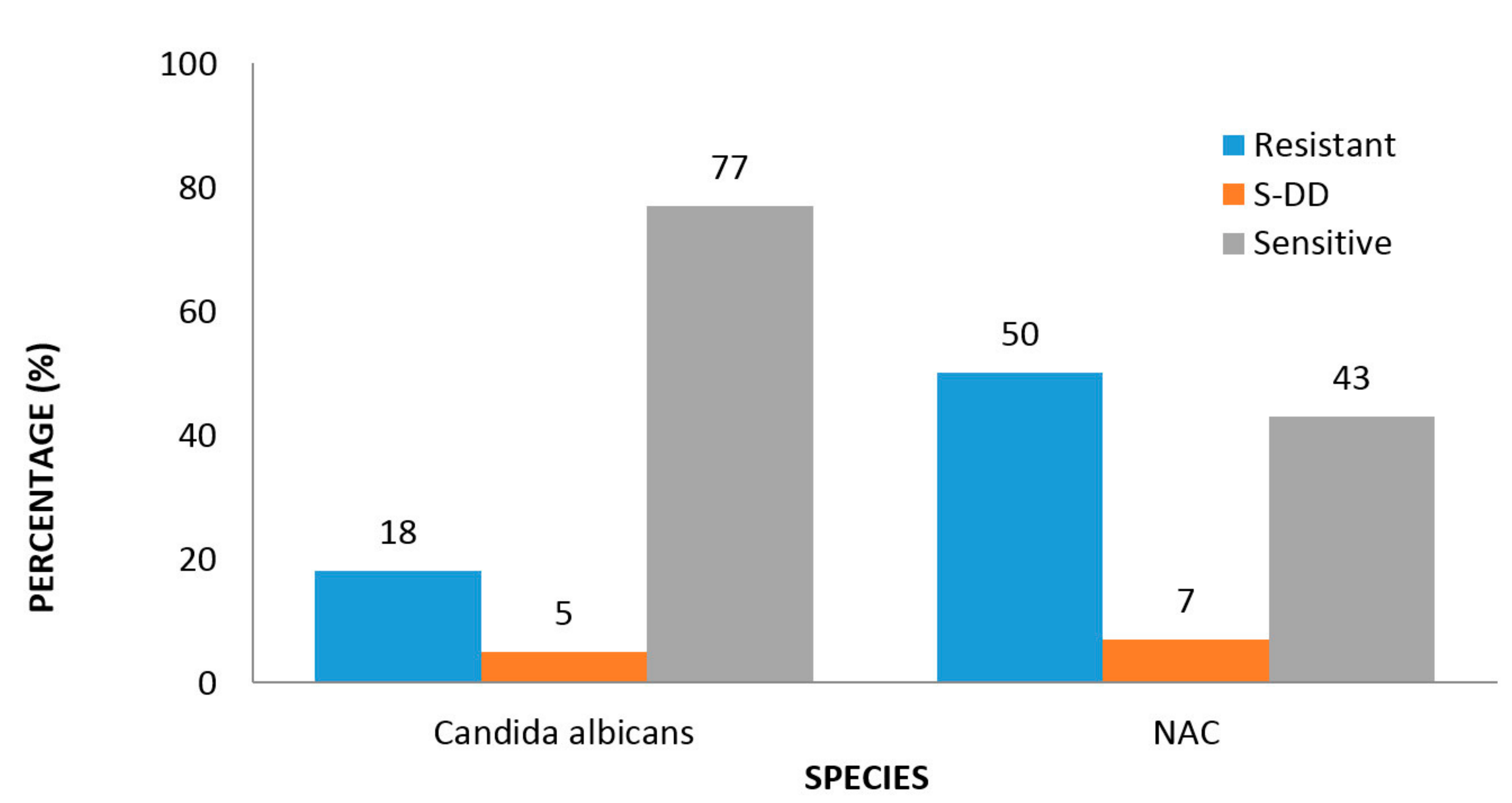
| Species | ||||
| C. albicans | 11 (18.0) | 50 (82.0) | NA 2 | 0.032 |
| NAC | 7 (50.0) | 7 (50.0) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osaigbovo, I.I.; Lofor, P.V.; Oladele, R.O. Fluconazole Resistance among Oral Candida Isolates from People Living with HIV/AIDS in a Nigerian Tertiary Hospital. J. Fungi 2017, 3, 69. https://doi.org/10.3390/jof3040069
Osaigbovo II, Lofor PV, Oladele RO. Fluconazole Resistance among Oral Candida Isolates from People Living with HIV/AIDS in a Nigerian Tertiary Hospital. Journal of Fungi. 2017; 3(4):69. https://doi.org/10.3390/jof3040069
Chicago/Turabian StyleOsaigbovo, Iriagbonse I., Patrick V. Lofor, and Rita O. Oladele. 2017. "Fluconazole Resistance among Oral Candida Isolates from People Living with HIV/AIDS in a Nigerian Tertiary Hospital" Journal of Fungi 3, no. 4: 69. https://doi.org/10.3390/jof3040069




