The Further Adventures of Newborn Screening for Biotinidase Deficiency: Where It Is at and What We Still Need to Know
Abstract
:1. Introduction
2. Taking Care of Some Old Business
2.1. Late-Onset Multiple Carboxylase Deficiency Becomes Biotinidase Deficiency
2.2. Spreading the Word about Biotinidase Deficiency
2.3. Newborn Screening for Biotinidase Deficiency Catches on
2.4. Newborn Screening for Biotinidase Deficiency Is Not for Everybody…Yet
2.5. What about the Natural History of Biotinidase Deficiency?
2.6. We Are Correct to Screen for Biotinidase Deficiency
2.7. What Questions about Biotinidase Deficiency and Its Newborn Screening Still Need Answering?
2.8. A Legacy Fulfilled
Acknowledgments
Conflicts of Interest
References
- Wolf, B. The Story of Biotinidase Deficiency and Its Introduction into Newborn Screening: The Role of Serendipity. Int. J. Neonatal Screen. 2015, 1, 3–12. [Google Scholar] [CrossRef]
- Wolf, B.; Grier, R.E.; Parker, W.D.; Goodman, S.I.; Allen, R.J. Deficient biotinidase activity in late-onset multiple carboxylase deficiency. N. Engl. J. Med. 1983, 308, 161. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B.; Grier, R.E.; Allen, R.J.; Goodman, S.I.; Kien, C.L. Biotinidase deficiency: The enzymatic defect in late-onset multiple carboxylase deficiency. Clin. Chim. Acta 1983, 131, 273–281. [Google Scholar] [CrossRef]
- Wolf, B.; Grier, R.E.; Allen, R.J.; Goodman, S.I.; Kien, C.L.; Parker, W.D.; Howell, D.M.; Hurst, D.L. Phenotypic variation in biotinidase deficiency. J. Pediatr. 1983, 103, 233–237. [Google Scholar] [CrossRef]
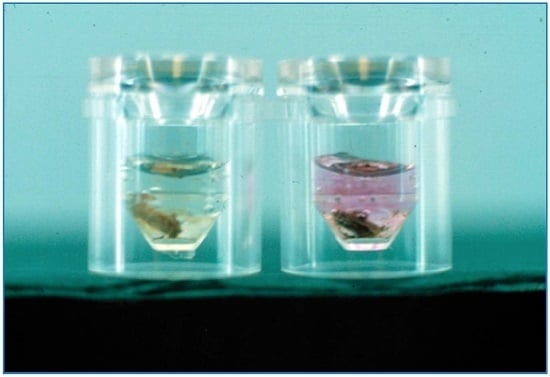
- Heard, G.S.; Secor McVoy, J.R.; Wolf, B. A screening method for biotinidase deficiency in newborns. Clin. Chem. 1984, 30, 125–127. [Google Scholar] [PubMed]
- Wolf, B.; Heard, G.S.; Jefferson, L.G.; Proud, V.K.; Nance, W.E.; Weissbecker, K.A. Clinical findings in four children with biotinidase deficiency detected through a statewide neonatal screening program. N. Engl. J. Med. 1985, 313, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Cole, H.; Reynolds, T.R.; Buck, G.B.; Lockyer, J.M.; Denson, T.; Spence, J.E.; Hymes, J.; Wolf, B. Human serum biotinidase: cDNA cloning, sequence and characterization. J. Biol. Chem. 1994, 269, 6566–6570. [Google Scholar] [PubMed]
- Knight, H.C.; Reynolds, T.R.; Meyers, G.A.; Pomponio, R.J.; Buck, G.A.; Wolf, B. Structure of the human biotinidase gene. Mamm. Genome 1998, 9, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Procter, M.; Wolf, B.; Crockett, D.K.; Mao, R. The biotinidase variants registry: A paradigm public database. Genes Genom. Genet. 2013. [Google Scholar] [CrossRef] [PubMed]
- Swango, K.L.; Demirkol, M.; Huner, G.; Pronicka, E.; Sykut-Cegielska, J.; Schulze, A.; Wolf, B. Partial biotinidase deficiency is usually due to the D444H mutation in the biotinidase gene. Hum. Genet. 1998, 102, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Pindolia, K.; Jensen, K.; Wolf, B. Three dimensional structure of human biotinidase: Computer modeling and functional correlations. Mol. Genet. Metab. 2013, 92, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Pindolia, K.; Jordan, M.; Guo, C.; Mathews, N.; Mock, D.; Strovel, E.; Blitzer, M.; Wolf, B. Development and characterization of a mouse with profound biotinidase deficiency: A biotin-responsive neurocutaneous disorder. Mol. Genet. Metab. 2010, 102, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Pindolia, K.; Chen, J.; Cardwell, C.; Cui, X.; Chopp, M.; Wolf, B. Neurological deficits in mice with profound biotinidase deficiency are associated with demylination and axonal degeneration. Neurobiol. Dis. 2012, 47, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Pindolia, K.; Li, H.; Cardwell, C.; Wolf, B. Characterization and functional analysis of cellular immunity in mice with biotinidase deficiency. Mol. Genet. Metab. 2014, 112, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Cowan, T.M.; Blitzer, M.G.; Wolf, B. Technical standards and guidelines for the diagnosis of biotinidase deficiency. Genet. Med. 2010, 12, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Jay, A.M.; Conway, R.L.; Feldman, G.L.; Nahhas, F.; Spencer, L.; Wolf, B. Outcomes of individuals with profound and partial biotinidase deficiency ascertained by newboorn screening in Michigan over 25 years. Genet. Med. 2015, 17, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Pispa, J. Animal biotinidase. Ann. Med. Exp. Biol. Fenn. 1965, 43 (Suppl. 5), 1–39. [Google Scholar]
- Bartlett, K.; Ghniem, H.K.; Stirk, J.H.; Wastell, H.J.; Sherrah, H.S.A.; Leonard, J.V. Enzyme studies in combined carboxylase deficiency. Ann. N. Y. Acad. Sci. 1985, 447, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Gompertz, D.; Bartlett, K.; Blair, D.; Stern, C.M.M. Child with a defect in leucine metabolism associated with beta hydroxyisovaleric aciduria and beta-methylcrotonylglycinuria. Arch. Dis. Child. 1973, 48, 975–977. [Google Scholar] [CrossRef] [PubMed]
- Gompertz, D.; Goodey, P.A.; Bartlett, K. Evidence for the enzymatic defect in beta-methylcrotonylglycinuria. FEBS Lett. 1973, 32, 13–14. [Google Scholar] [CrossRef]
- Bartlett, K.; Gompertz, D. Combined carboxylase defect: Biotin-responsiveness in cultured fibroblasts. Lancet 1976, 2, 804. [Google Scholar] [CrossRef]
- Bartlett, K.; Ng, H.; Dale, G.; Green, A.; Leonard, J.V. Studies on cultured fibroblasts from patients with defects of biotin-dependent carboxylation. J. Inherit. Metab. Dis. 1981, 4, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Ghneim, H.K.; Bartlett, K. Mechanism of biotin-responsive combined carboxylase deficiency. Lancet 1982, 1, 1187–1188. [Google Scholar] [CrossRef]
- Baumgartner, R.; Suormala, T.; Wick, H.; Geisert, J.; Lehnert, W. Infantile multiple carboxylase deficiency: Evidence for normal intestinal absorption but renal loss of biotin. Helv. Pediatr. Acta 1982, 37, 499–502. [Google Scholar]
- Baumgartner, E.R.; Sourmala, T.; Wick, H.; Bonjour, J.P. Biotin-responsive multiple carboxylase deficiency (MCD): Deficient biotinidase activity associated with renal loss of biotin. J. Inherit. Metab. Dis. 1984, 7 (Suppl. 2), 123–125. [Google Scholar] [PubMed]
- Samboni, M.; Gaudry, M.; Marquet, A.; Munnich, A.; Saudubray, J.M.; Marsac, C. Search for the biochemical basis of biotin dependent multiple carboxylase deficiencies: Determination of biotin activation in cultured fibroblasts. Clin. Chim. Acta 1981, 122, 241. [Google Scholar] [CrossRef]
- Munnich, A.; Saudubray, J.M.; Ogier, H.; Coude, F.X.; Marsac, C.; Roccichioli, F.; Labarthe, J.C.; Cuzanave, C.; Laugier, J.; Harpentier, C.; et al. Deficit multiple des carboxylases. Arch. Fr. Pediatr. 1981, 38, 83. [Google Scholar] [PubMed]
- Munnich, A.; Fischer, A.; Saudubray, J.M.; Griscelli, C.; Coude, F.X.; Ogier, H.; Charpentier, C.; Frezal, J. Biotin-responsive immunoregulatory dysfunction in multiple carboxylase deficiency. J. Inherit. Metab. Dis. 1981, 4, 113–114. [Google Scholar] [CrossRef]
- Fischer, A.; Munnich, A.; Saudubray, J.M. Biotin-responsive immunoregulatory dysfunction in multiple carboyxlase deficiency. J. Clin. Immunol. 1982, 2, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Munnich, A.; Saudubray, J.M.; Cotjsson, A.; Coude, F.X.; Ogier, H.; Charpentier, C.; Marsac, C.; Garre, G.; Bourgeay-Causse, M.; Frezal, J. Biotin dependent multiple carboxylase deficiency presenting as a congenital lactic acidosis. Eur. J. Pediatr. 1981, 137, 203–206. [Google Scholar] [PubMed]
- Feldman, G.L.; Wolf, B. Deficient acetyl-CoA carboxylase activity in multiple carboxylase deficiency. Clin. Chim. Acta 1981, 111, 147–151. [Google Scholar] [CrossRef]
- Feldman, G.L.; Hsia, Y.E.; Wolf, B. Biochemical characterization of biotin responsive multiple carboxylase deficiency: Heterogeneity within the bio genetic complementation group. Am. J. Hum. Genet. 1981, 33, 692–701. [Google Scholar] [PubMed]
- Wolf, B.; Hsia, Y.E.; Sweetman, L.; Feldman, G.; Boychuk, R.B.; Bart, R.D.; Crowell, D.H.; Di Mauro, R.M.; Nyhan, W.L. Multiple carboxylase deficiency: Cinical and biochemical improvement following neonatal biotin treatment. Pediatrics 1981, 68, 113–118. [Google Scholar] [PubMed]
- Koivusalo, M.; Pispa, J. Biotinidase activity in animal tissue. Acta Physiol. Scand. 1963, 58, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Wastell, H.; Dale, G.; Bartlett, K. A sensitive fluorimetric rate assay for biotinidase using a new derivative of biotin, biotinyl-6-aminoquinoline. Anal. Biochem. 1984, 140, 69–73. [Google Scholar] [CrossRef]
- Chan, P.W.; Bartlett, K. A new solid-phase assay for biotin and biocytin and its application to the study of patients with biotinidase deficiency. Clin. Chim. Acta 1986, 159, 185–196. [Google Scholar] [CrossRef]
- Wastell, H.J.; Bartlett, K.; Dale, G.; Shein, A. Biotinidase deficiency: A survey of 10 cases. Arch. Dis. Child. 1988, 63, 1244–1249. [Google Scholar] [CrossRef] [PubMed]
- Schubiger, G.; Caflisch, U.; Baumgartner, R.; Suormala, T.; Bachmann, C. Biotinidase deficiency: Clinical course and biochemical findings. J. Inherit. Metab. Dis. 1984, 7, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Suormala, T.; Wick, H.; Bonjour, J.P.; Baumgartner, E.R. Intestinal absorption and renal excretion of biotin in patients with biotinidase deficiency. Eur. J. Pediatr. 1985, 144, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Suormala, T.M.; Baumgartner, E.R.; Wick, H.; Scheibenreiter, S.; Schweitzer, S. Comparison of patients with complete and partial biotinidase deficiency: Biochemical studies. J. Inherit. Metab. Dis. 1990, 13, 76–92. [Google Scholar] [CrossRef] [PubMed]
- Suormala, T.; Ramaekers, V.T.; Schweitzer, S.; Fowler, B.; Laub, M.C.; Schwermer, C.; Bachmann, J.; Baumgartner, E.R. Biotinidase Km-variants: Detection and detailed biochemical investigations. J. Inherit. Metab. Dis. 1995, 18, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, E.R.; Suormala, T.M.; Wick, H.; Probst, A. Biotinidase deficiency: A cause of subacute necrotizing encephalomyelopathy (Leigh syndrome). Report of a case with lethal outcome. Pediatr. Res. 1989, 26, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, E.R.; Suormala, T.; Wick, H.; Bausch, J.; Bonjour, J.-P. Biotinidase deficiency: Factors responsible for the increased biotin requirement. J. Inherit. Metab. Dis. 1985, 8 (Suppl. 1), 59–64. [Google Scholar] [CrossRef] [PubMed]
- Ramaekers, V.Th.; Suormala, T.M.; Brab, M.; Duran, R.; Heimann, G.; Baumgartner, E.R. A biotinidase Km variant causing late onset bilateral optic neuropathy. Arch. Dis. Child. 1992, 67, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Suormala, T.M.; Baumgartner, E.R.; Bausch, J.; Holick, W.; Wick, H. Quantitative determination of biocytin in urine of patients with biotinidase deficiency using high-performance liquid chromatography. Clin. Chim. Acta 1988, 177, 253–269. [Google Scholar] [CrossRef]
- Wolf, B.; Pomponio, R.J.; Norrgard, K.J.; Lott, I.T.; Baumgartner, E.R.; Suormala, T.; Raemaekers, V.Th.; Coskun, T.; Tokatli, A.; Ozalp, I.; et al. Delayed-onset profound biotinidase deficiency. J. Pediatr. 1998, 132, 362–365. [Google Scholar] [CrossRef]
- Wolf, B.; Jensen, K.; Huner, G.; Demirkol, M.; Baykal, T.; Divry, P.; Rolland, M.O.; Perez-Cerda, C.; Ugarte, M.; Straussberg, R.; et al. Seventeen novel mutations that cause profound biotinidase deficiency. Mol. Genet. Metab. 2002, 77, 108–111. [Google Scholar] [CrossRef]
- Broda, E.; Baumgartner, E.R.; Scholl, S.; Stopsack, M.; Horn, A.; Rhode, H. Biotinidase determination in serum and dried blood spots-high sensitivity fluorometric ultramicro-assay. Clin. Chim. Acta 2001, 314, 175–185. [Google Scholar] [CrossRef]
- Dobrowolski, S.F.; Angeletti, J.; Banas, R.A.; Naylor, E.W. Real time PCR assays to detect common mutations in the biotinidase gene and application of mutational analysis to newborn screening for biotinidase deficiency. Mol. Genet. Metab. 2003, 78, 100–107. [Google Scholar] [CrossRef]
- Wolf, B. Worldwide survey of neonatal screening for biotinidase deficiency. J. Inherit. Metab. Dis. 1991, 14, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B.; Heard, G.S. Screening for biotinidase deficiency in newborns: Worldwide experience. Pediatrics 1990, 85, 512–517. [Google Scholar] [PubMed]
- Pomponio, R.J.; Coskun, T.; Demirkol, M.; Tokatli, A.; Ozalp, I.; Huner, G.; Baykal, T.; Wolf, B. Novel mutations cause biotinidase deficiency in Turkish children. J. Inherit. Metab. Dis. 1999, 23, 120–128. [Google Scholar] [CrossRef]
- Pomponio, R.J.; Ozand, P.I.; Al Essa, M.; Wolf, B. Novel mutations in children with profound biotinidase deficiency from Saudi Arabia. J. Inherit. Metab. Dis. 2000, 23, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Al-Jasmi, F.A.; Al-Shamai, A.; Hertecant, J.L.; Al-Hamad, S.M.; Sould, A.K. Inborn errors of metabolism in the United Arab Emirates: Disorders detected by newborn screening. J. Inherit. Metab. Dis. Rep. 2016, 28, 127–135. [Google Scholar]
- Ohlsson, A.; Guthenberg, C.; Holme, E.; von Dobein, U. Profound biotinidase deficiency: A rare disease among native Swedes. J. Inherit. Metab. Dis. 2010, 33 (Suppl. 3), S175–S180. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B. Why perform newborn screening for profound and partial biotinidase deficiency? Mol. Genet. Metab. 2015, 114, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Mc Sweeney, N.; Grunewald, S.; Bhate, S.; Gunesan, V.; Chong, W.K.; Hemingway, C. Two unusual clinical and radiological presentations of biotinidase deficiency. J. Eur. Pediatr. Neurol. Soc. 2010, 14, 535–538. [Google Scholar] [CrossRef] [PubMed]
- Grunewald, S.; Champion, M.P.; Leonard, J.V.; Schaper, J.; Morris, A.A.M. Biotinidase defiicency: A treatable leukoencephalopathy. Neuropediatrics 2004, 35, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B. Biotinidase deficiency should be considered in individuals exhibiting myelopathy with or without vision loss. Mol. Genet. Metab. 2015, 116, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Haine, S.R.; Langmuir, R.A. Optic neuropathy due to biotinidase deficiency in 19-year-old amn. JAMA Opthalmol. 2014, 132, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Bottin, L.; Prud’hon, S.; Guey, S.; Giannesini, C.; Wolf, B.; Pindoliua, K.; Stankoff, B. Biotinidase deficiency mimicking neuromylitis optica: Initially exhibiting symptoms in adulthood. Mult. Scler. J. 2015, 21, 1604–1607. [Google Scholar] [CrossRef] [PubMed]
- Carroll, A.E.; Downs, S.M. Comprehensive cost-utility analysis of newborn screening strategies. Pediatrics 2006, 117, S287–S295. [Google Scholar] [PubMed]
- Schoos, R.; Verloes, A.; Bourguignon, J.P.; Koulischer, L. Programs of systematic screening in neonatolgy. Rev. Med. Liege 1998, 53, 311–315. [Google Scholar] [PubMed]
- Vallejo-Torres, L.; Rodreguez, I.V.; Perez-Cerda, C.; Plana, J.C.; Pineda, M.; Elgarresta, A.A.; Martin-Hernandez, E.; Crouce, M.L. Cost-effectiveness analysis of newborn screening for biotinidase deficiency. Pediatrics 2015, 136, e424–e432. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B. The neurology of biotinidase deficiency. Mol. Genet. Metab. 2011, 104, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Moslinger, D.; Stockler-Ipsiroglu, S.; Scheibenreiter, S.; Tiefenthaler, M.; Muhl, A.; Seidl, R.; Strobl, W.; Plecko, B.; Suormala, T.; Baumgartner, E.R. Clinical and neuropsychological outcome in 33 patients with biotinidase deficiency ascertained by nationwide newborn screening and family studies in Austria. Eur. J. Pediatr. 2002, 161, 167–168. [Google Scholar] [CrossRef]
- Möslinger, D.; Mühl, A.; Suormala, T.; Baumgartner, R.; Ströckler-Ipsiroglu, S. Molecular characterization and neuropsychological outcome of 21 patients with profound biotinidase deficiency detected by newborn screening and family studies. Eur. J. Pediatr. 2003, 162, S46–S49. [Google Scholar] [CrossRef] [PubMed]
- Weber, P.; Schoo, S.; Baumgartner, E.R. Outcome in patients with profound biotinidase deficiency: Relevance of newborn screening. Dev. Med. Child. Neurol. 2004, 46, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B. Successful outcomes of older adolescents and adults with profound biotinidase deficiency identified by newborn screening. Genet. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Sivri, H.S.; Genc, G.A.; Tokatli, A.; Dursun, A.; Coskun, T.; Aydin, H.I.; Sennaroglu, L.; Belgin, E.; Jensen, K.; Wolf, B. Hearing loss in biotinidase deficiency: Genotype-phenotype correlation. J. Pediatr. 2007, 150, 439–442. [Google Scholar] [CrossRef] [PubMed]
- Iseeri-ERten, S.O.; Dikmen, Z.G.; Ulusu, N.N. Comparison of spectrophotometric and fluorimetric methods in evaluation of biotinidase deficiency. J. Med. Biochem. 2016, 35, 123–129. [Google Scholar]
- Hymes, J.; Fleischhauer, K.; Wolf, B. Biotinylation of histones by human serum biotinidase: Assessment of biotinyl-transferase activity in sera from normal individuals and children with biotinidase deficiency. Biochem. Mol. Med. 1995, 56, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Narang, M.A.; Dumas, R.; Ayer, R.; Gravel, R.A. Localization of holocarboxylase synthetase in the nucleus of cells: A novel role for biotin in human biology. Am. J. Hum. Genet. 2002, 71, 174. [Google Scholar]
- Narong, M.A.; Dumas, R.; Ayers, L.M.; Gravel, R.A. Reduced histone biotinylation in multiple carboxylase deficiency patients: A nuclear role of holocarboxylase synthetase. Hum. Mol. Genet. 2004, 13, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B. Biotinidase deficiency: If you have to have an inherited metabolic disease, this is the one to have. Genet. Med. 2012, 14, 565–575. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the author; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolf, B. The Further Adventures of Newborn Screening for Biotinidase Deficiency: Where It Is at and What We Still Need to Know. Int. J. Neonatal Screen. 2016, 2, 9. https://doi.org/10.3390/ijns2040009
Wolf B. The Further Adventures of Newborn Screening for Biotinidase Deficiency: Where It Is at and What We Still Need to Know. International Journal of Neonatal Screening. 2016; 2(4):9. https://doi.org/10.3390/ijns2040009
Chicago/Turabian StyleWolf, Barry. 2016. "The Further Adventures of Newborn Screening for Biotinidase Deficiency: Where It Is at and What We Still Need to Know" International Journal of Neonatal Screening 2, no. 4: 9. https://doi.org/10.3390/ijns2040009