Pulling Exercises for Strength Training and Rehabilitation: Movements and Loading Conditions
Abstract
:1. Introduction
2. Methods
2.1. Subjects
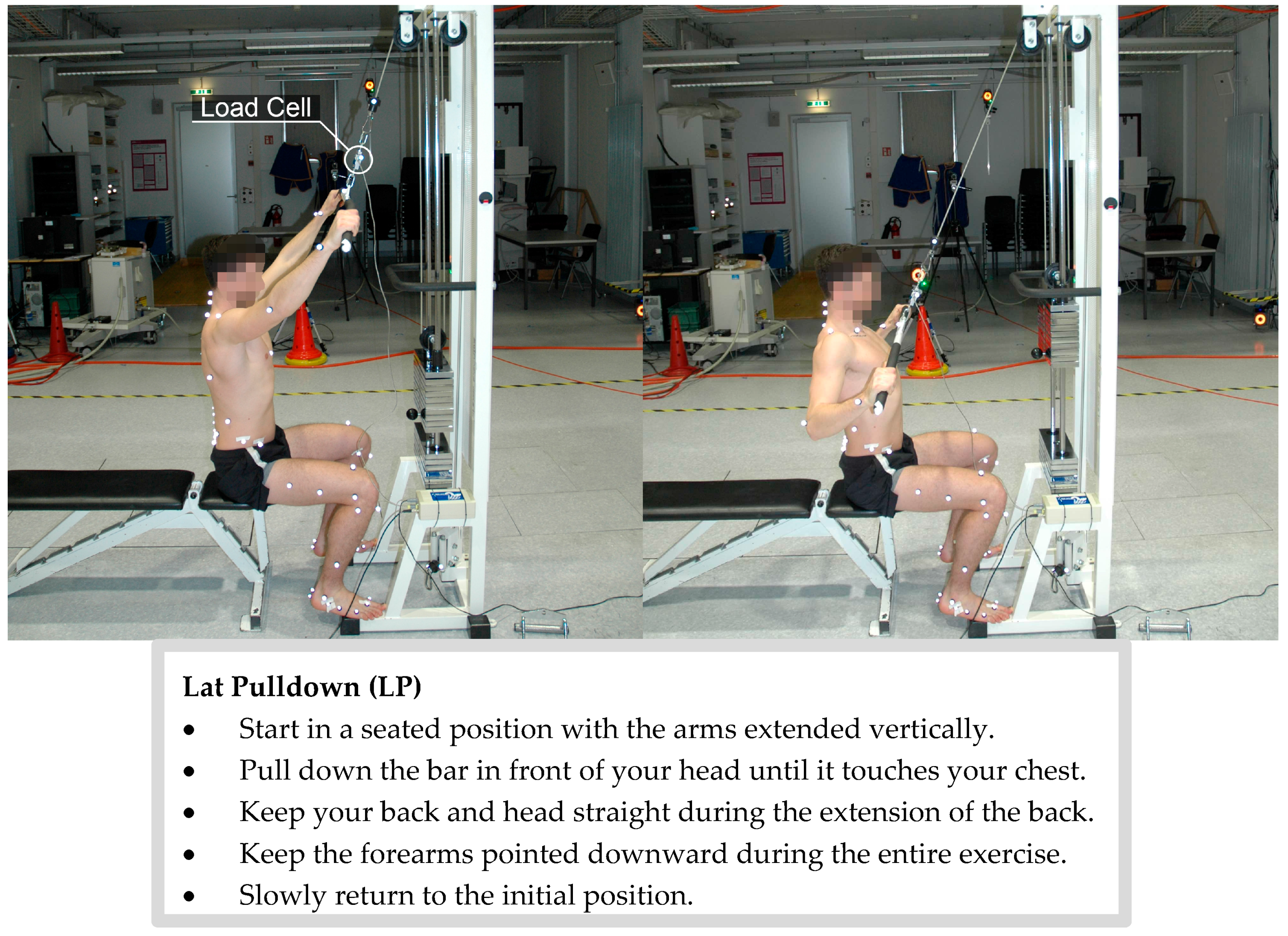
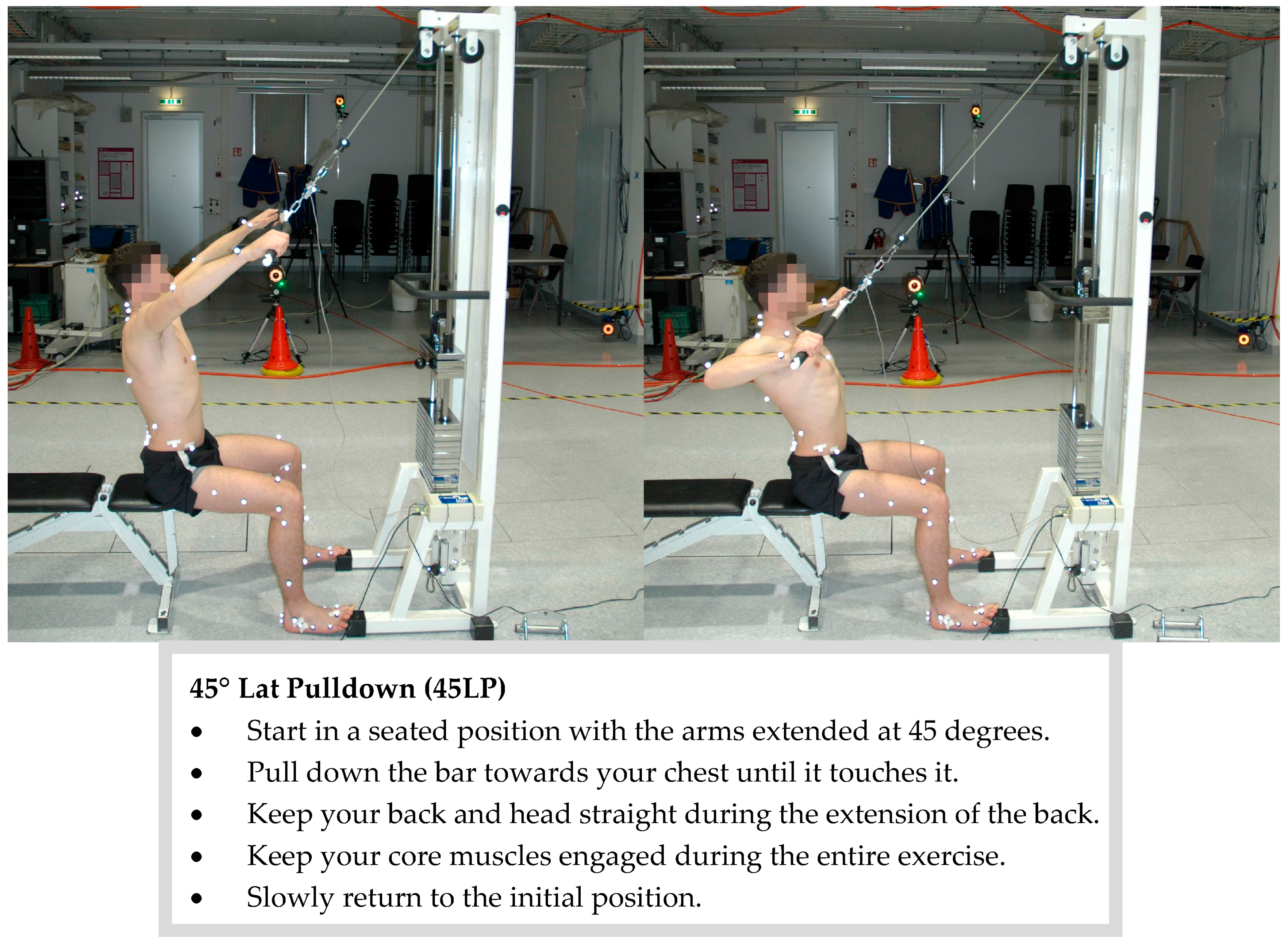
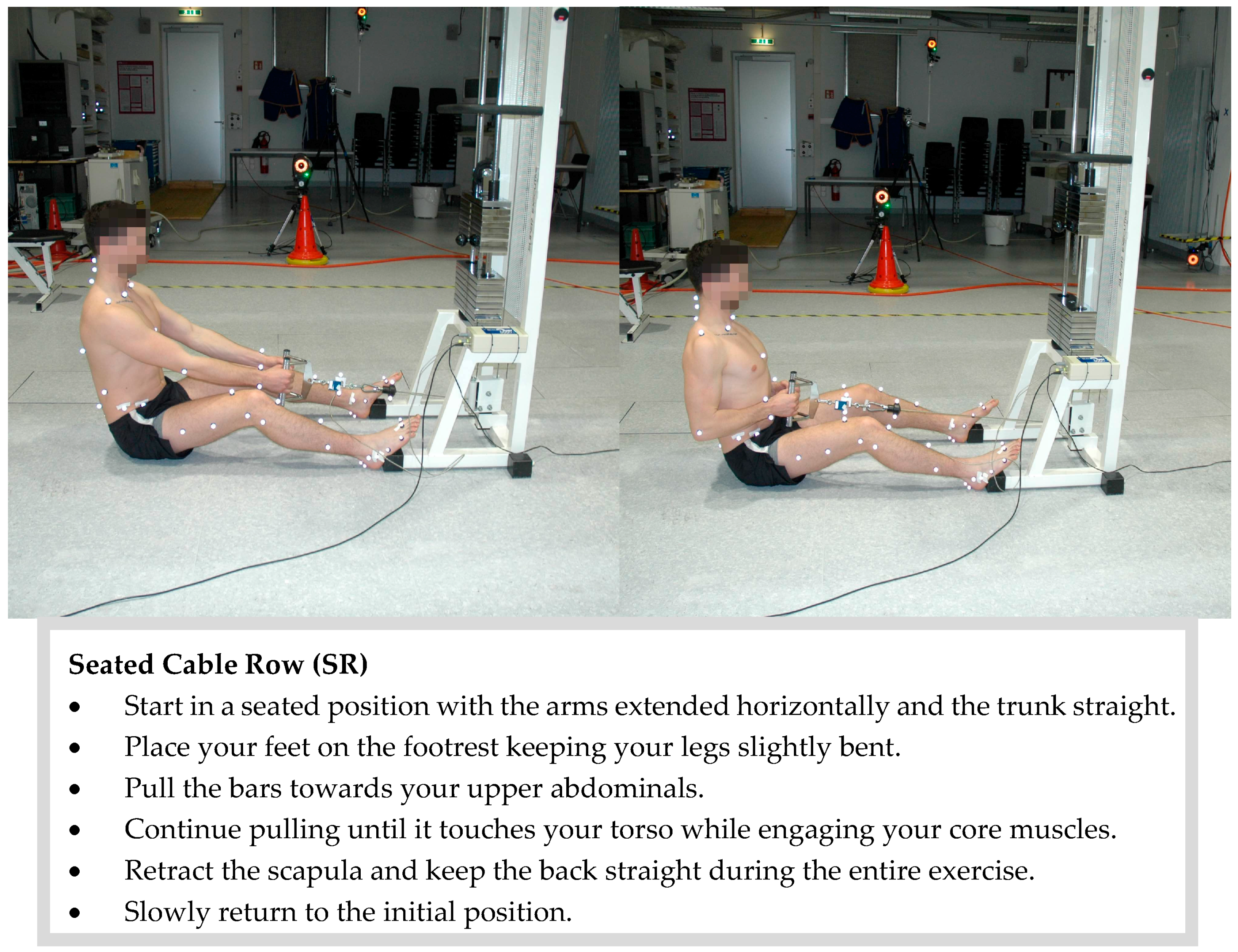
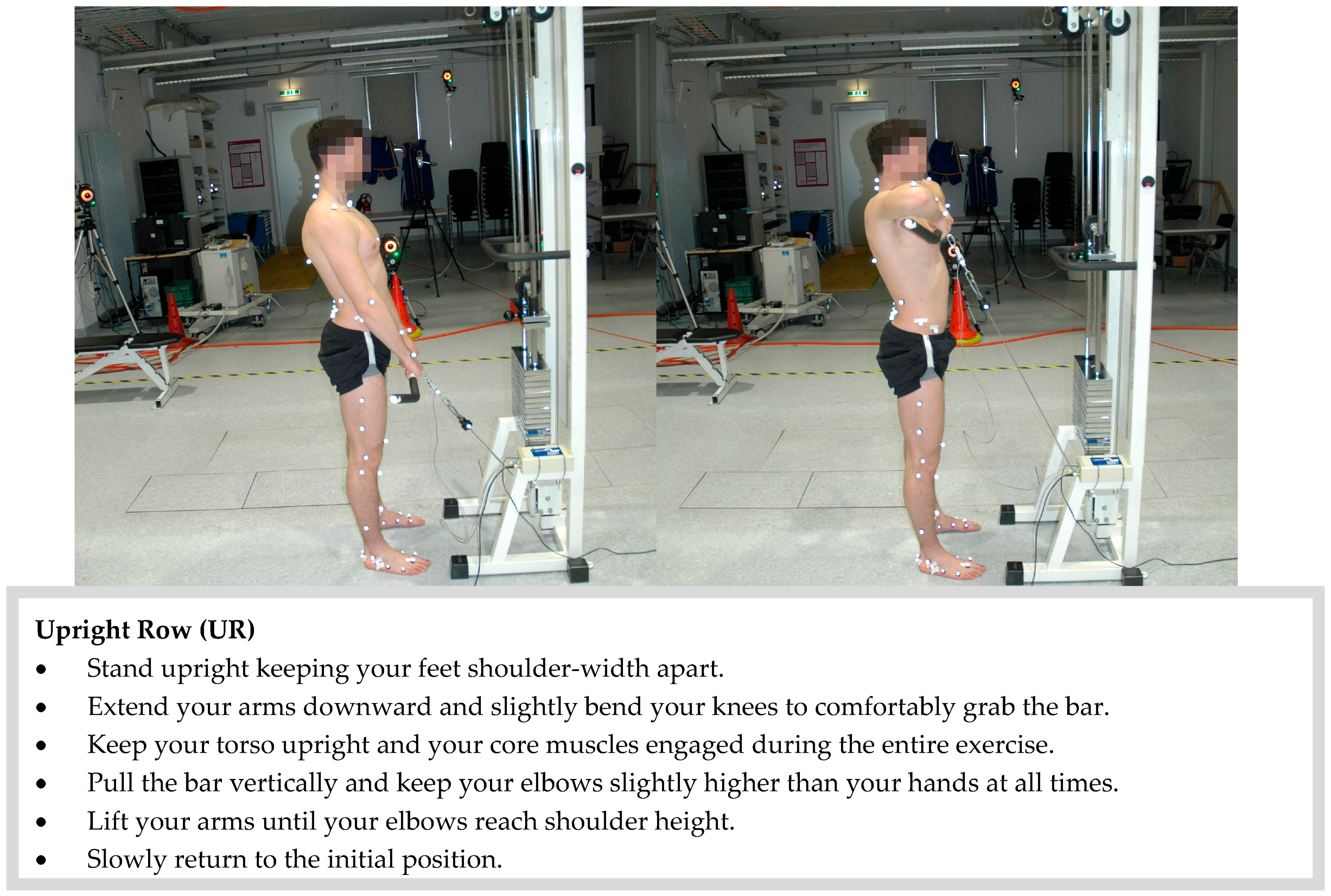
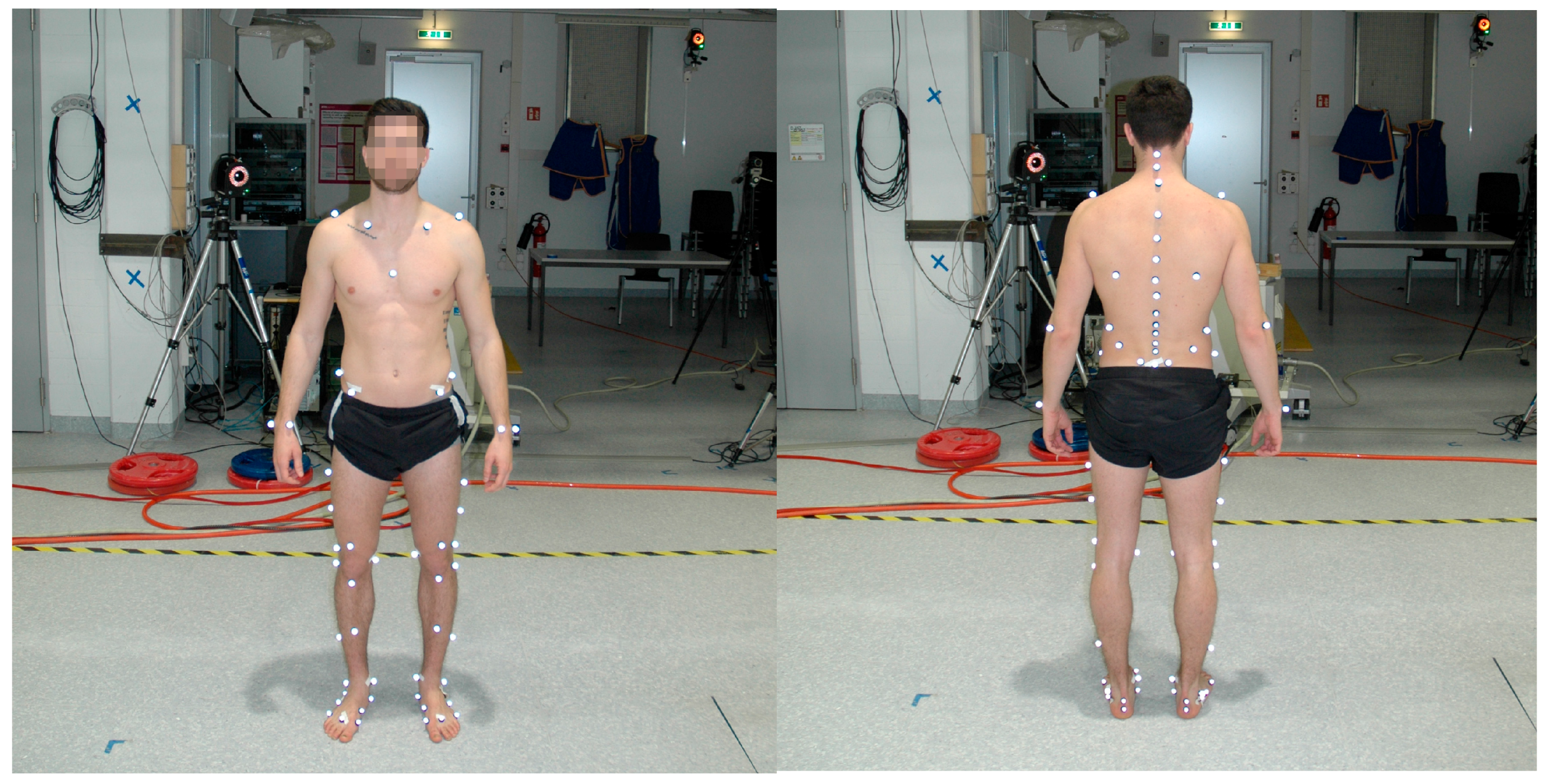
2.2. Measurement Procedures
2.3. Data Acquisition
2.4. Data Processing and Analysis
3. Results
3.1. Kinematics
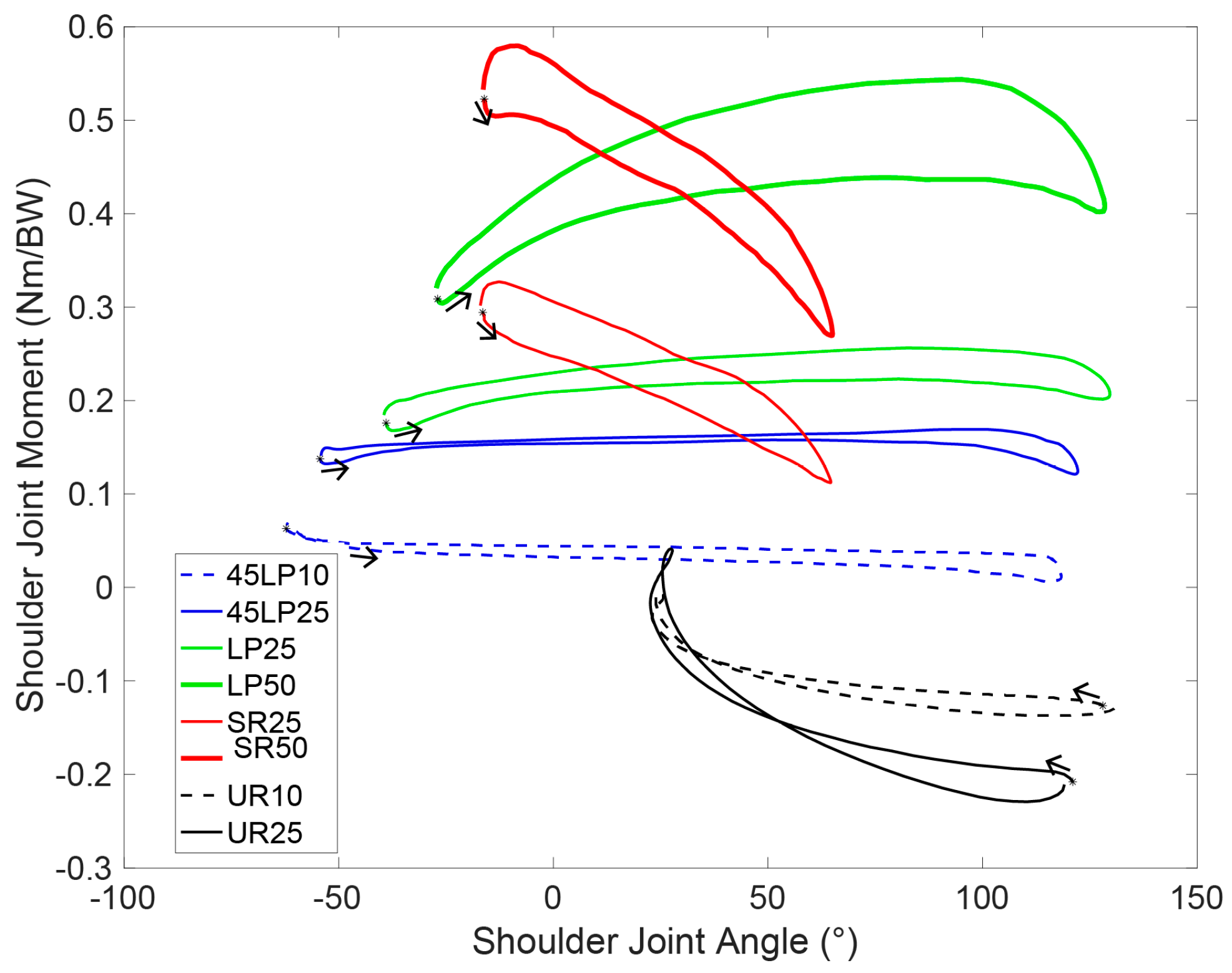
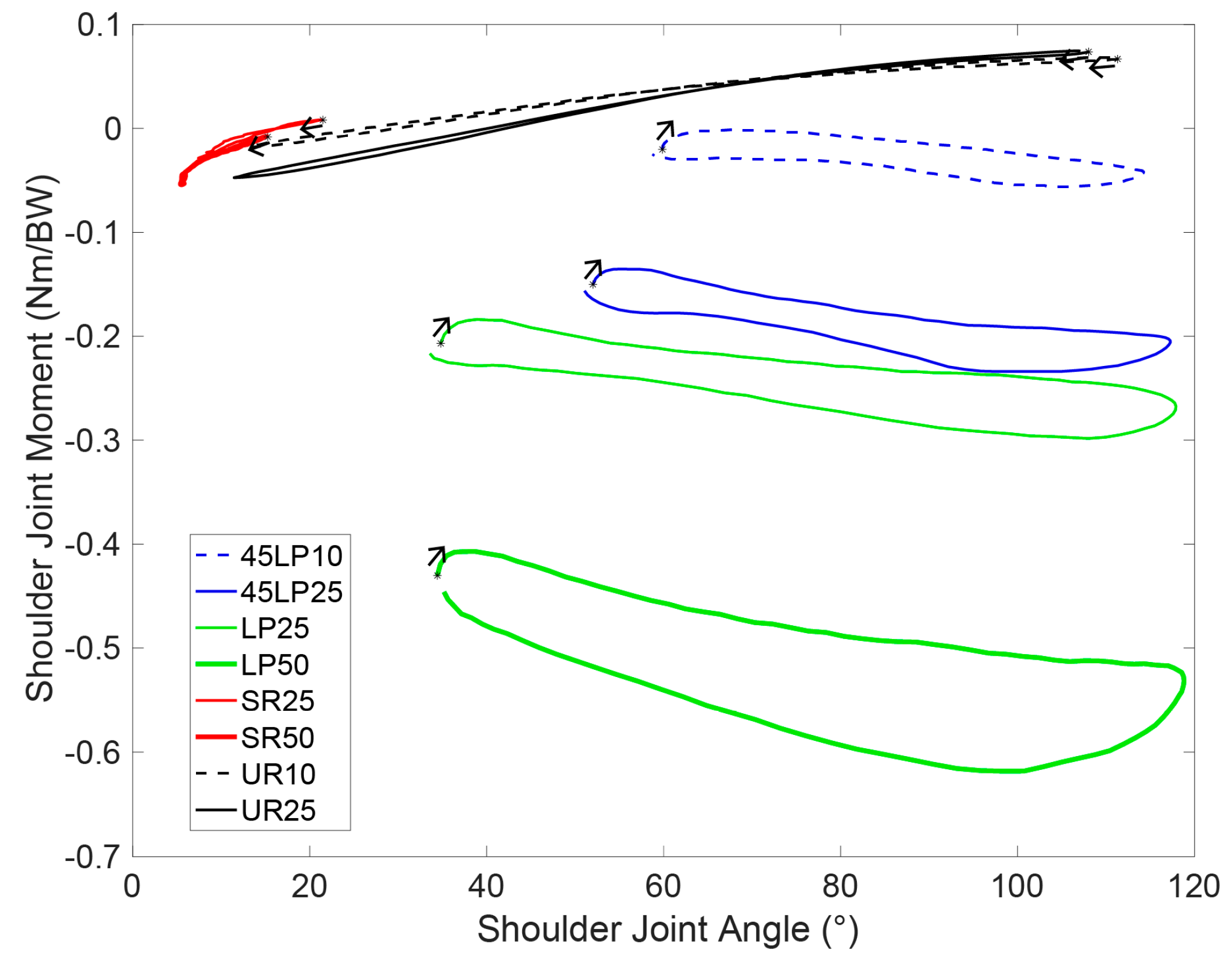
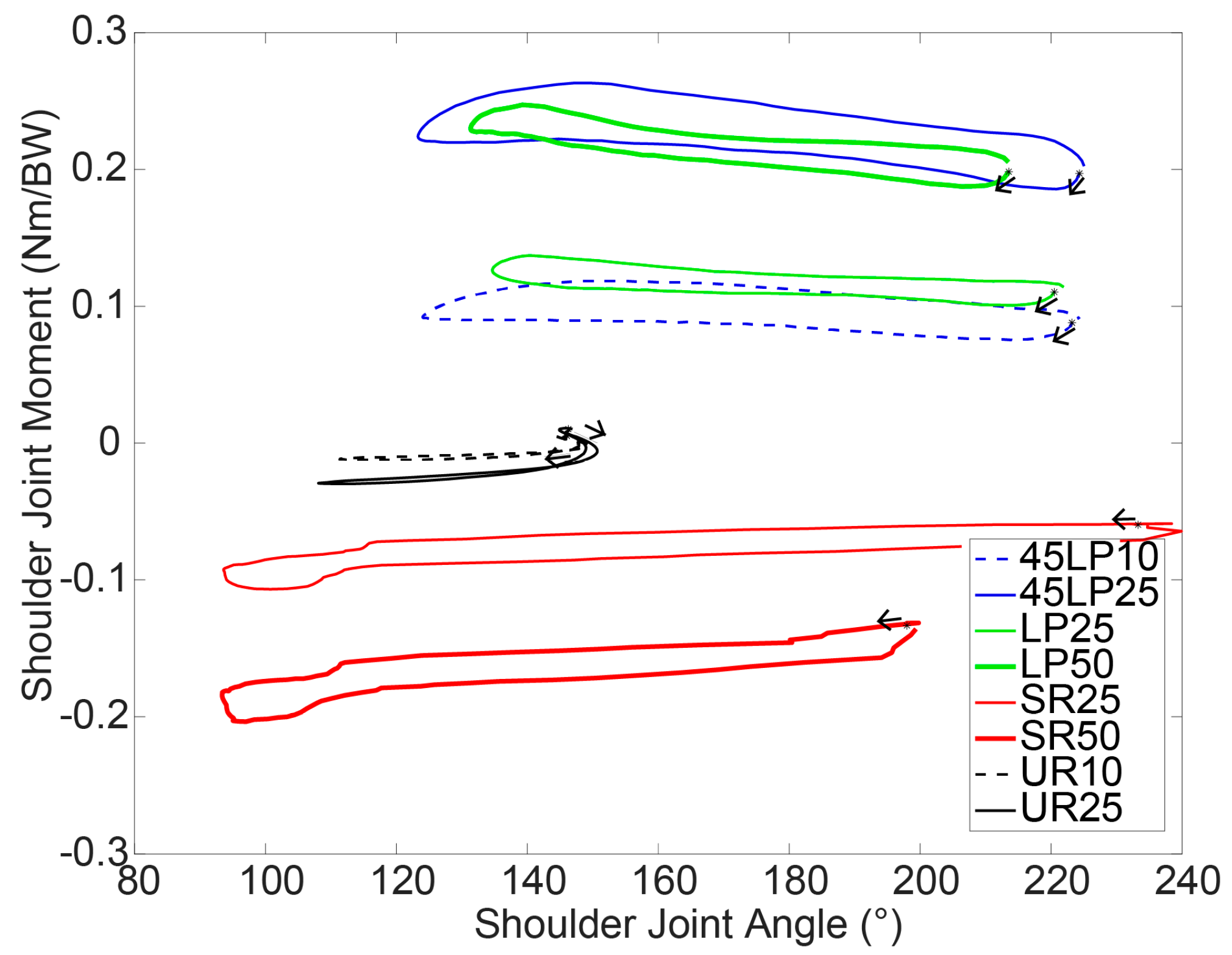
3.2. Kinetics
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Segmental Motion | Lat Pulldown | 45° Lat Pulldown | Seated Cable Row | Upright Row | |||||
|---|---|---|---|---|---|---|---|---|---|
| 25% BW | 50% BW | 10% BW | 25% BW | 25% BW | 50% BW | 10% BW | 25% BW | ||
| ROM Lumbar Rel thoracic Back (°) | Sagittal | 5.2 ± 1.2 | 9.6 ± 4.5 | 7.2 ± 3.4 | 7.2 ± 3.2 | 3.8 ± 1.4 | 5.5 ± 2.3 | 4.2 ± 1.6 | 6.7 ± 3.9 |
| Frontal | 2.1 ± 0.7 | 2.6 ± 1.0 | 1.9 ± 0.4 | 2.1 ± 0.5 | 2.0 ± 0.4 | 2.3 ± 0.8 | 1.6 ± 0.4 | 2.1 ± 0.7 | |
| Transverse | 1.4 ± 0.4 | 2.1 ± 0.5 | 1.3 ± 0.4 | 1.5 ± 0.3 | 1.0 ± 0.3 | 1.2 ± 0.5 | 1.2 ± 0.3 | 1.5 ± 0.5 | |
| ROM Shoulder Joint (°) | Sagittal | 172.9 ± 9.6 | 158.9± 15.3 | 218.8 ± 46.2 | 191.1 ± 33.3 | 78.7 ± 19.9 | 82.3 ± 10.4 | 114.9 ± 14.6 | 106.4 ± 20.0 |
| Frontal | 88.4 ± 10.6 | 86.7± 11.0 | 58.8 ± 14.8 | 69.7 ± 14.2 | 16.8 ± 5.3 | 13.1 ± 3.6 | 102.2 ± 10.6 | 100.1 ± 13.9 | |
| Transverse | 90.5 ± 13.4 | 85.1± 18.6 | 102.1 ± 8.7 | 104.0 ± 10.0 | 147.0 ± 40.6 | 111.7 ± 58.5 | 45.1 ± 5.9 | 50.3 ± 10.5 | |
| Curvature | Lat Pulldown | 45° Lat Pulldown | Seated Cable Row | Upright Row | |||||
|---|---|---|---|---|---|---|---|---|---|
| 25% BW | 50% BW | 10% BW | 25% BW | 25% BW | 50% BW | 10% BW | 25% BW | ||
| Mean Curvature (1/m) | Thoracic | 1.78 ± 0.73 | 1.85 ± 0.71 | 1.89 ± 0.74 | 1.81 ± 0.76 | 1.83 ± 0.77 | 2.16 ± 0.58 | 2.61 ± 0.62 | 2.63 ± 0.67 |
| Lumbar | 1.63 ± 1.92 | 0.58 ± 2.01 | 1.72 ± 2.01 | 1.46 ± 1.70 | −1.19 ± 1.00 | −0.45 ± 1.27 | 4.94 ± 1.58 | 4.84 ± 1.76 | |
| Max Curvature (1/m) | Thoracic | 2.03 ± 0.70 | 2.20 ± 0.72 | 2.19 ± 0.71 | 2.09 ± 0.71 | 2.09 ± 0.76 | 2.45 ± 0.54 | 2.84 ± 0.60 | 2.85 ± 0.64 |
| Lumbar | 2.16 ± 2.01 | 1.16 ± 2.11 | 2.22 ± 2.18 | 1.96 ± 1.83 | −0.82 ± 1.06 | 0.14 ± 1.43 | 5.46 ± 1.88 | 5.58 ± 2.08 | |
| P-Values and (χ2) | Lat Pulldown | 45° Lat Pulldown | Seated Cable Row | Upright Row | ||
|---|---|---|---|---|---|---|
| Max Curvature Angle (°) | Thoracic | LP | - | |||
| 45LP | 1.000 (0.001) | - | ||||
| SR | 1.000 (0.020) | 1.000 (0.014) | - | |||
| UR | 0.000 (0.258) | 0.000 (0.250) | 0.006 (0.168) | - | ||
| Lumbar | LP | - | ||||
| 45LP | 1.000 (0.001) | - | ||||
| SR | 0.237 (0.083) | 0.473 (0.049) | - | |||
| UR | 0.000 (0.509) | 0.000 (0.475) | 0.000 (0.643) | - | ||
| Min Curvature Angle (°) | Thoracic | LP | - | |||
| 45LP | 1.000 (0.000) | - | ||||
| SR | 1.000 (0.028) | 0.932 (0.032) | - | |||
| UR | 0.001 (0.219) | 0.000 (0.219) | 0.073 (0.107) | - | ||
| Lumbar | LP | - | ||||
| 45LP | 1.000 (0.000) | - | ||||
| SR | 0.591 (0.047) | 0.755 (0.037) | - | |||
| UR | 0.000 (0.561) | 0.000 (0.543) | 0.000 (0.656) | - | ||
| ROM Curvature Angle (°) | Thoracic | LP | - | |||
| 45LP | 1.000 (0.016) | - | ||||
| SR | 1.000 (0.014) | 0.343 (0.052) | - | |||
| UR | 1.000 (0.028) | 1.000 (0.000) | 0.283 (0.083) | - | ||
| Lumbar | LP | - | ||||
| 45LP | 1.000 (0.007) | - | ||||
| SR | 0.796 (0.051) | 1.000 (0.018) | - | |||
| UR | 1.000 (0.003) | 1.000 (0.000) | 1.000 (0.016) | - | ||
| P-Values and (χ2) | LP25 | LP50 | 45LP10 | 45LP25 | SR25 | SR50 | UR10 | UR25 |
|---|---|---|---|---|---|---|---|---|
| LP25 | - | |||||||
| LP50 | - | - | ||||||
| 45LP10 | - | - | - | |||||
| 45LP25 | 0.002 (0.404) | - | - | - | ||||
| SR25 | 0.056 (0.149) | - | - | 0.000 (0.532) | - | |||
| SR50 | - | 0.608 (0.010) | - | - | - | - | ||
| UR10 | - | - | 0.000 (0.817) | - | - | - | - | |
| UR25 | 0.581 (0.131) | - | - | 0.236 (0.233) | 0.000 (0.356) | - | - | - |
| P-Values and (χ2) | LP25 | LP50 | 45LP10 | 45LP25 | SR25 | SR50 | UR10 | UR25 |
|---|---|---|---|---|---|---|---|---|
| LP25 | - | |||||||
| LP50 | - | - | ||||||
| 45LP10 | - | - | - | |||||
| 45LP25 | 0.000 (0.680) | - | - | - | ||||
| SR25 | 0.000 (0.986) | - | - | 0.000 (0.967) | - | |||
| SR50 | - | 0.000 (0.982) | - | - | - | - | ||
| UR10 | - | - | 0.356 (0.031) | - | - | - | - | |
| UR25 | 0.000 (0.958) | - | - | 0.000 (0.905) | 0.000 (0.668) | - | - | - |
| P-Values and (χ2) | LP25 | LP50 | 45LP10 | 45LP25 | SR25 | SR50 | UR10 | UR25 |
|---|---|---|---|---|---|---|---|---|
| LP25 | - | |||||||
| LP50 | - | - | ||||||
| 45LP10 | - | - | - | |||||
| 45LP25 | 0.000 (0.926) | - | - | - | ||||
| SR25 | 0.000 (0.356) | - | - | 0.000 (0.925) | - | |||
| SR50 | - | 0.008 (0.225) | - | - | - | - | ||
| UR10 | - | - | 0.000 (0.957) | - | - | - | - | |
| UR25 | 0.000 (0.927) | - | - | 0.000 (0.986) | 0.001 (0.756) | - | - | - |
| P-Values and (χ2) | LP25 | LP50 | 45LP10 | 45LP25 | SR25 | SR50 | UR10 | UR25 |
|---|---|---|---|---|---|---|---|---|
| LP25 | - | |||||||
| LP50 | - | - | ||||||
| 45LP10 | - | - | - | |||||
| 45LP25 | 0.387 (0.220) | - | - | - | ||||
| SR25 | 0.000 (0.396) | - | - | 0.005 (0.220) | - | |||
| SR50 | - | 0.000 (0.680) | - | - | - | - | ||
| UR10 | - | - | 0.043 (0.139) | - | - | - | - | |
| UR25 | 0.000 (0.899) | - | - | 0.000 (0.861) | 0.000 (0.346) | - | - | - |
| ICC | LP25 | LP50 | 45LP10 | 45LP25 | SR25 | SR50 | UR10 | UR25 | |
|---|---|---|---|---|---|---|---|---|---|
| Max Curvature Angle (°) | Thoracic | 0.996 | 0.995 | 0.996 | 0.997 | 0.994 | 0.994 | 0.996 | 0.999 |
| Lumbar | 0.988 | 0.981 | 0.995 | 0.991 | 0.997 | 0.96 | 0.998 | 0.997 | |
| Min Curvature Angle (°) | Thoracic | 0.997 | 0.996 | 0.996 | 0.997 | 0.996 | 0.996 | 0.993 | 0.997 |
| Lumbar | 0.993 | 0.983 | 0.995 | 0.992 | 0.998 | 0.995 | 0.998 | 0.996 | |
| ROM Curvature Angle (°) | Thoracic | 0.979 | 0.879 | 0.971 | 0.966 | 0.923 | 0.960 | 0.938 | 0.95 |
| Lumbar | 0.906 | 0.774 | 0.979 | 0.948 | 0.966 | 0.821 | 0.988 | 0.983 | |
References
- Dagenais, S.; Caro, J.; Haldeman, S. A systematic review of low back pain cost of illness studies in the united states and internationally. Spine J. 2008, 8, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.F. The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. J. Spinal Disord. 2000, 13, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Crow, W.T.; Willis, D.R. Estimating cost of care for patients with acute low back pain: A retrospective review of patient records. J. Am. Osteopath. Assoc. 2009, 109, 229–233. [Google Scholar] [PubMed]
- Deyo, R.A.; Cherkin, D.; Conrad, D.; Volinn, E. Cost, controversy, crisis-low-back-pain and the health of the public. Ann. Rev. Public Health 1991, 12, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.R.; Tanaka, S.; Halperin, W.E.; Cameron, L.L. Back pain prevalence in us industry and estimates of lost workdays. Am. J. Public Health 1999, 89, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.F.; Muller, R.; Grant, W.D. Low back pain in australian adults: Prevalence and associated disability. J. Manip. Physiol. Ther. 2004, 27, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Wieser, S.; Horisberger, B.; Schmidhauser, S.; Eisenring, C.; Brugger, U.; Ruckstuhl, A.; Dietrich, J.; Mannion, A.F.; Elfering, A.; Tamcan, O.; et al. Cost of low back pain in switzerland in 2005. Eur. J. Health Econ. 2011, 12, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, D.M.; Nelson, B.W. Low back strengthening for the prevention and treatment of low back pain. Med. Sci. Sports Exerc. 1999, 31, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Pengel, L.H.M.; Herbert, R.D.; Maher, C.G.; Refshauge, K.M. Acute low back pain: Systematic review of its prognosis. BMJ 2003, 327, 323. [Google Scholar] [CrossRef] [PubMed]
- Kent, P.M.; Keating, J.L. The epidemiology of low back pain in primary care. Chiropr. Osteopat. 2005, 13, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, G.B.J. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Rosenstiel, A.K.; Keefe, F.J. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 1983, 17, 33–44. [Google Scholar] [CrossRef]
- Frymoyer, J.; Cats-Baril, W. An over-view of the incidences and costs of low back pain. Orthop. Clin. N. Am. 1991, 22, 263–271. [Google Scholar]
- Hoy, D.; Brooks, P.; Blyth, F.; Buchbinder, R. The epidemiology of low back pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Leino, P.; Aro, S.; Hasan, J. Trunk muscle function and low back disorders: A ten-year follow-up study. J. Chronic Dis. 1987, 40, 289–296. [Google Scholar] [CrossRef]
- Chou, R.; Qaseem, A.; Snow, V.; Casey, D.; Cross, J.T., Jr.; Shekelle, P.; Owens, D.K.; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the american college of physicians and the american pain society. Ann. Intern. Med. 2007, 147, 478–491. [Google Scholar] [PubMed]
- McGill, S.M. Low back stability: From formal description to issues for performance and rehabilitation. Exerc. Sport Sci. Rev. 2001, 29, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Hibbs, A.E.; Thompson, K.G.; French, D.; Wrigley, A.; Spears, I. Optimizing performance by improving core stability and core strength. Sports Med. 2008, 38, 995–1008. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Huxel, K.C.; Nesser, T.W. Relationship between core stability, functional movement, and performance. J. Strength Cond. Res. 2011, 25, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Shinkle, J.; Nesser, T.W.; Demchak, T.J.; McMannus, D.M. Effect of core strength on the measure of power in the extremities. J. Strength Cond. Res. 2012, 26, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Stone, M.H.; Fry, A.C.; Ritchie, M.; Stoessel-Ross, L.; Marsit, J.L. Injury potential and safety aspects of weightlifting movements. Strength Cond. J. 1994, 16, 15–21. [Google Scholar] [CrossRef]
- Müller, R. Fitness-Center: Verletzungen und Beschwerden Beim Training; Beratungsstelle für Unfallverhütung: Bern, Switzerland, 1999. [Google Scholar]
- Schellenberg, F.; Lindorfer, J.; List, R.; Taylor, W.; Lorenzetti, S. Kinetic and kinematic differences between deadlifts and goodmornings. BMC Sports Sci. Med. Rehabil. 2013, 5, 27. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, F.; Schmid, N.; Häberle, R.; Hörterer, N.; Taylor, W.R.; Lorenzetti, S. Loading conditions in the spine, hip and knee during different executions of back extension exercises. BMC Sports Sci. Med. Rehabil. 2017, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Doma, K.; Deakin, G.B.; Ness, K.F. Kinematic and electromyographic comparisons between chin-ups and lat-pull down exercises. Sports Biomech. 2013, 12, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Lehman, G.J.; Buchan, D.D.; Lundy, A.; Myers, N.; Nalborczyk, A. Variations in muscle activation levels during traditional latissimus dorsi weight training exercises: An experimental study. Dyn. Med. 2004, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- McAllister, M.J.; Schilling, B.K.; Hammond, K.G.; Weiss, L.W.; Farney, T.M. Effect of grip width on electromyographic activity during the upright row. J. Strength Cond. Res. 2013, 27, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Signorile, J.E.; Zink, A.J.; Szwed, S.P. A comparative electromyographical investigation of muscle utilization patterns using various hand positions during the lat pull-down. J. Strength Cond. Res. 2002, 16, 539–546. [Google Scholar] [PubMed]
- Handa, T.; Kato, H.; Hasegawa, S.; Okada, J.; Kato, K. Comparative electromyographical investigation of the biceps brachii, latissimus dorsi, and trapezius muscles during five pull exercises. Jpn. J. Phys. Fit. Sports Med. 2005, 54, 159–168. [Google Scholar] [CrossRef]
- Cronin, J.B.; Jones, J.V.; Hagstrom, J.T. Kinematics and kinetics of the seated row and implications for conditioning. J. Strength Cond. Res. 2007, 21, 1265–1270. [Google Scholar] [PubMed]
- List, R.; Gülay, T.; Stoop, M.; Lorenzetti, S. Kinematics of the trunk and the lower extremities during restricted and unrestricted squats. J. Strength Cond. Res. 2013, 27, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Lorenzetti, S.; Gülay, T.; Stoop, M.; List, R.; Gerber, H.; Schellenberg, F.; Stüssi, E. Comparison of the angles and corresponding moments in the knee and hip during restricted and unrestricted squats. J. Strength Cond. Res. 2012, 26, 2829–2836. [Google Scholar] [CrossRef] [PubMed]
- Schütz, P.; List, R.; Zemp, R.; Schellenberg, F.; Taylor, W.R.; Lorenzetti, S. Joint angles of the ankle, knee, and hip and loading conditions during split squats. J. Appl. Biomech. 2014, 30, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Rab, G.; Petuskey, K.; Bagley, A. A method for determination of upper extremity kinematics. Gait Posture 2002, 15, 113–119. [Google Scholar] [CrossRef]
- Schmid, S.; Studer, D.; Hasler, C.C.; Romkes, J.; Taylor, W.R.; Brunner, R.; Lorenzetti, S. Using skin markers for spinal curvature quantification in main thoracic adolescent idiopathic scoliosis: An explorative radiographic study. PLoS ONE 2015, 10, e0135689. [Google Scholar] [CrossRef] [PubMed]
- Zemp, R.; List, R.; Gulay, T.; Elsig, J.P.; Naxera, J.; Taylor, W.R.; Lorenzetti, S. Soft tissue artefacts of the human back: Comparison of the sagittal curvature of the spine measured using skin markers and an open upright mri. PLoS ONE 2014, 9, e95426. [Google Scholar] [CrossRef] [PubMed]
- Baaklini, E.; Angst, M.; Schellenberg, F.; Hitz, M.; Schmid, S.; Tal, A.; Taylor, W.R.; Lorenzetti, S. High-heeled walking decreases lumbar lordosis. Gait Posture 2017, 55, 12–14. [Google Scholar] [CrossRef] [PubMed]
- Kao, L.S.; Green, C.E. Analyis of Variance: Is there a difference in means and what does it mean. J. Surg. Res. 2008, 144, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chirop. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Norman, R.; Wells, R.; Neumann, P.; Frank, J.; Shannon, H.; Kerr, M. A comparison of peak vs cumulative physical work exposure risk factors for the reporting of low back pain in the automotive industry. Clin. Biomech. 1998, 13, 561–573. [Google Scholar] [CrossRef]
- Potvin, J.R.; Norman, R.W.; McGill, S.M. Reduction in anterior shear forces on the l 4l 5 disc by the lumbar musculature. Clin. Biomech. 1991, 6, 88–96. [Google Scholar] [CrossRef]
- Bloomquist, K.; Langberg, H.; Karlsen, S.; Madsgaard, S.; Boesen, M.; Raastad, T. Effect of range of motion in heavy load squatting on muscle and tendon adaptations. Eur. J. Appl. Physiol. 2013, 113, 2133–2142. [Google Scholar] [CrossRef] [PubMed]
- McMahon, G.E.; Morse, C.I.; Burden, A.; Winwood, K.; Onambélé, G.L. Impact of range of motion during ecologically valid resistance training protocols on muscle size, subcutaneous fat, and strength. J. Strength Cond. Res. 2014, 28, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Pinto, R.S.; Gomes, N.; Radaelli, R.; Botton, C.E.; Brown, L.E.; Bottaro, M. Effect of range of motion on muscle strength and thickness. J. Strength Cond. Res. 2012, 26, 2140–2145. [Google Scholar] [CrossRef] [PubMed]
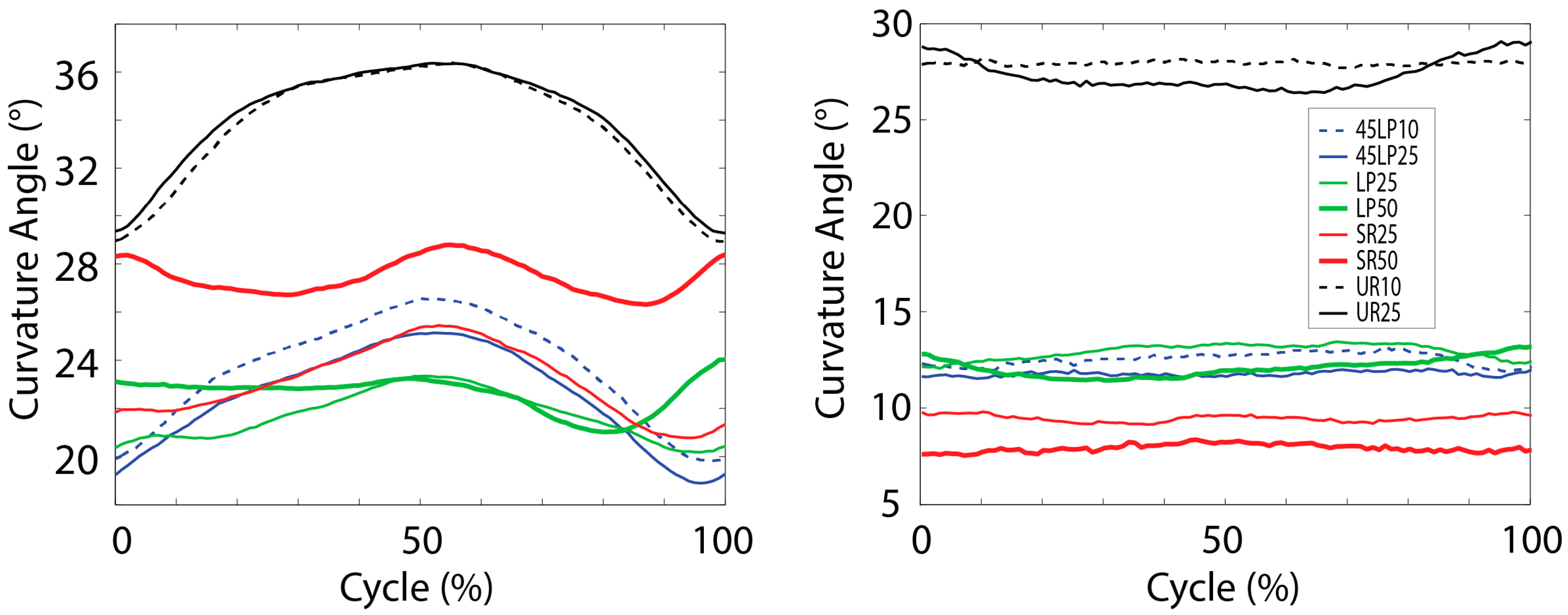
| Curvature Angle | Lat Pulldown | 45° Lat Pulldown | Seated Cable Row | Upright Row | |||||
|---|---|---|---|---|---|---|---|---|---|
| 25% BW | 50% BW | 10% BW | 25% BW | 25% BW | 50% BW | 10% BW | 25% BW | ||
| Max Curvature Angle, (°) | Thoracic | 24.8 ± 9.1 | 27.6 ± 10.7 | 27.5 ± 9.4 | 26.0 ± 9.4 | 26.4 ± 10.6 | 31.5 ± 7.9 | 37.1 *,+,† ± 8.4 | 37.1 *,+,† ± 9.4 |
| Lumbar | 16.1 ± 7.9 | 15.9 ± 6.8 | 15.8 ± 9.7 | 15.0 ± 8.4 | 12.0 ± 7.2 | 11.6 ± 6.5 | 30.7 *,+,† ± 7.6 | 31.1 *,+,† ± 8.0 | |
| Min Curvature Angle, (°) | Thoracic | 18.1 ± 10.0 | 18.3 ± 10.4 | 18.2 ± 10.4 | 17.6 ± 11.0 | 19.4 ± 11.1 | 23.8 ± 9.1 | 27.9 *,+,† ± 8.9 | 28.4 *,+,† ± 9.7 |
| Lumbar | 9.7 ± 7.3 | 8.9 ± 7.2 | 9.4 ± 8.6 | 8.7 ± 7.3 | 7.2 ± 7.4 | 5.3 ± 6.6 | 25.1 *,+,† ± 6.7 | 23.9 *,+,† ± 6.6 | |
| ROM Curvature Angle, (°) | Thoracic | 6.7 ± 3.0 | 9.3 ± 2.2 | 9.3 ± 3.9 | 8.5 ± 3.8 | 7.1 ± 2.8 | 7.7 ± 2.6 | 9.2 ± 2.7 | 8.8 ± 2.7 |
| Lumbar | 6.4 ± 2.2 | 7.0 ± 2.0 | 6.3 ± 2.6 | 6.3 ± 2.5 | 4.8 ± 2.1 | 6.4 ± 2.8 | 5.6 ± 3.0 | 7.2 ± 3.9 | |
| Shoulder Joint Moment | Lat Pulldown | 45° Lat Pulldown | Seated Cable Row | Upright Row | |||||
|---|---|---|---|---|---|---|---|---|---|
| 25% BW | 50% BW | 10% BW | 25% BW | 25% BW | 50% BW | 10% BW | 25% BW | ||
| Mmax Shoulder Joint [Nm/BW] | Sagittal | 0.28 +,¶ ± 0.06 | 0.58 ± 0.11 | 0.07 ¶ ± 0.02 | 0.19 *,†,¶ ± 0.05 | 0.34 +,¶ ± 0.09 | 0.60 ± 0.11 | −0.15 + ± 0.02 | −0.24 *,+,† ± 0.04 |
| Frontal | −0.32 +,†,¶ ± 0.02 | −0.64 † ± 0.05 | −0.07 ¶ ± 0.02 | −0.25 *†,¶ ± 0.03 | −0.03 *,+,¶ ± 0.01 | −0.06 * ± 0.02 | 0.07 + ± 0.02 | 0.09 *,+,† ± 0.03 | |
| Transverse | 0.15 +,†,¶ ± 0.02 | 0.26 † ± 0.03 | 0.13 ¶ ± 0.02 | 0.27 *,†,¶ ± 0.02 | −0.11 *,+,¶ ± 0.03 | −0.22 * ± 0.05 | −0.02 + ± 0.01 | −0.04 *,+,† ± 0.01 | |
| Absolute | 0.45 †,¶ ± 0.04 | 0.89 † ± 0.08 | 0.15 ¶ ± 0.02 | 0.41 †,¶ ± 0.03 | 0.34 *,+,¶ ± 0.09 | 0.62 * ± 0.11 | 0.16 + ± 0.01 | 0.25 *,+,† ± 0.03 | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorenzetti, S.; Dayer, R.; Plüss, M.; List, R. Pulling Exercises for Strength Training and Rehabilitation: Movements and Loading Conditions. J. Funct. Morphol. Kinesiol. 2017, 2, 33. https://doi.org/10.3390/jfmk2030033
Lorenzetti S, Dayer R, Plüss M, List R. Pulling Exercises for Strength Training and Rehabilitation: Movements and Loading Conditions. Journal of Functional Morphology and Kinesiology. 2017; 2(3):33. https://doi.org/10.3390/jfmk2030033
Chicago/Turabian StyleLorenzetti, Silvio, Romain Dayer, Michael Plüss, and Renate List. 2017. "Pulling Exercises for Strength Training and Rehabilitation: Movements and Loading Conditions" Journal of Functional Morphology and Kinesiology 2, no. 3: 33. https://doi.org/10.3390/jfmk2030033






