Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure
Abstract
:Preamble
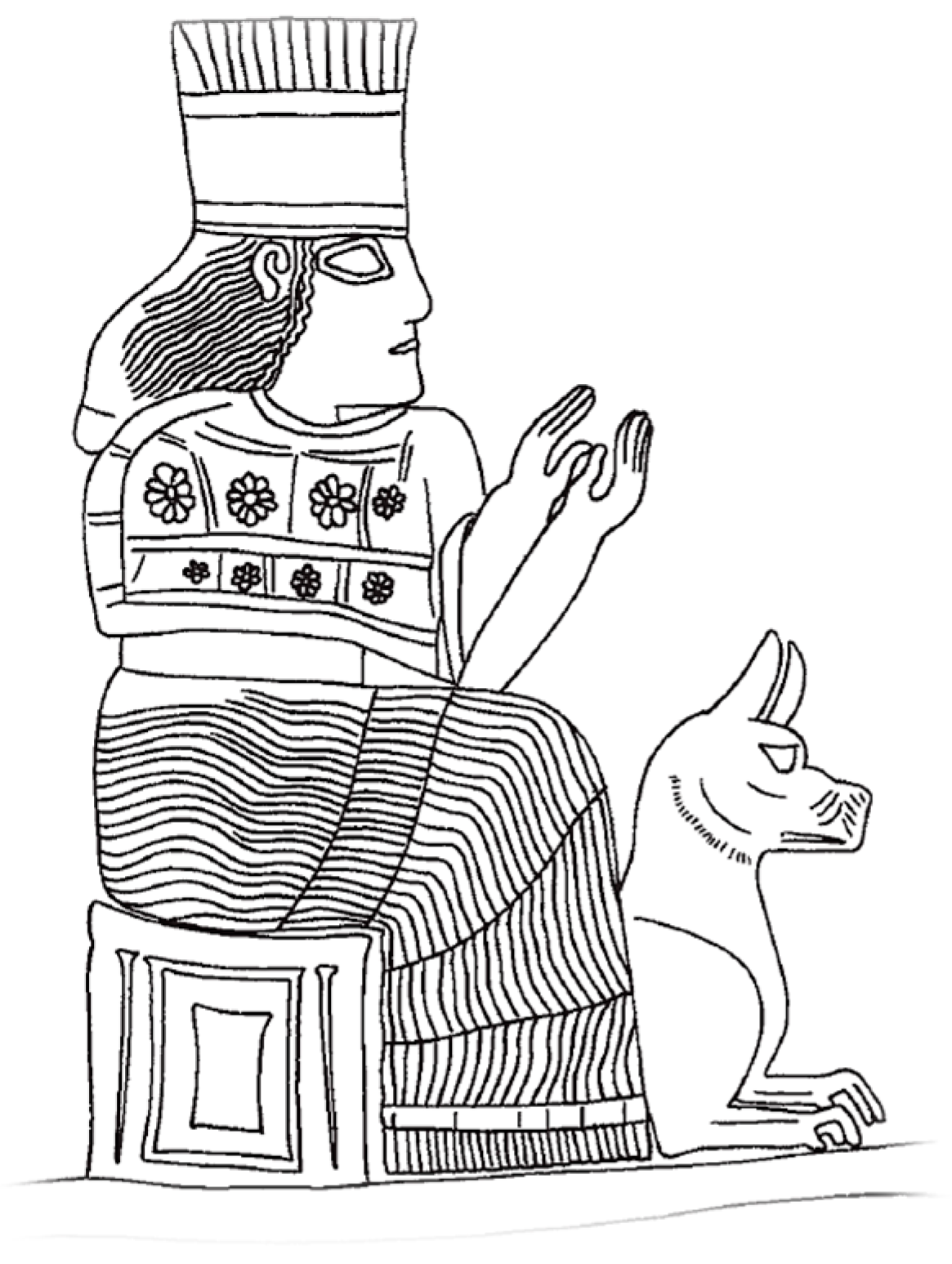
1. Rabies in Sumerian and Akkadian Civilizations
2. Rabies in Classical Antiquity
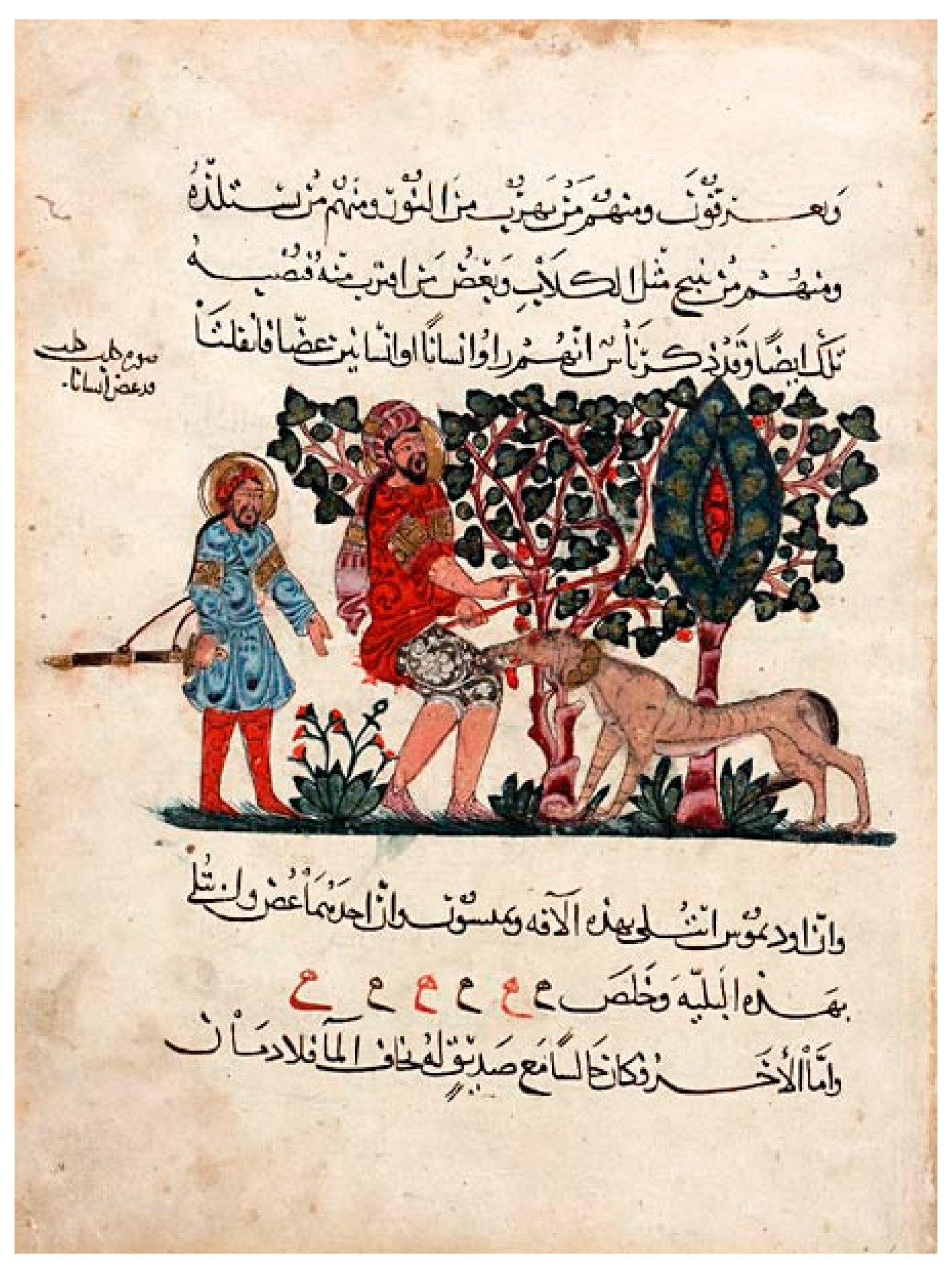
3. The Middle Ages
4. After 1492: Emergence and Control
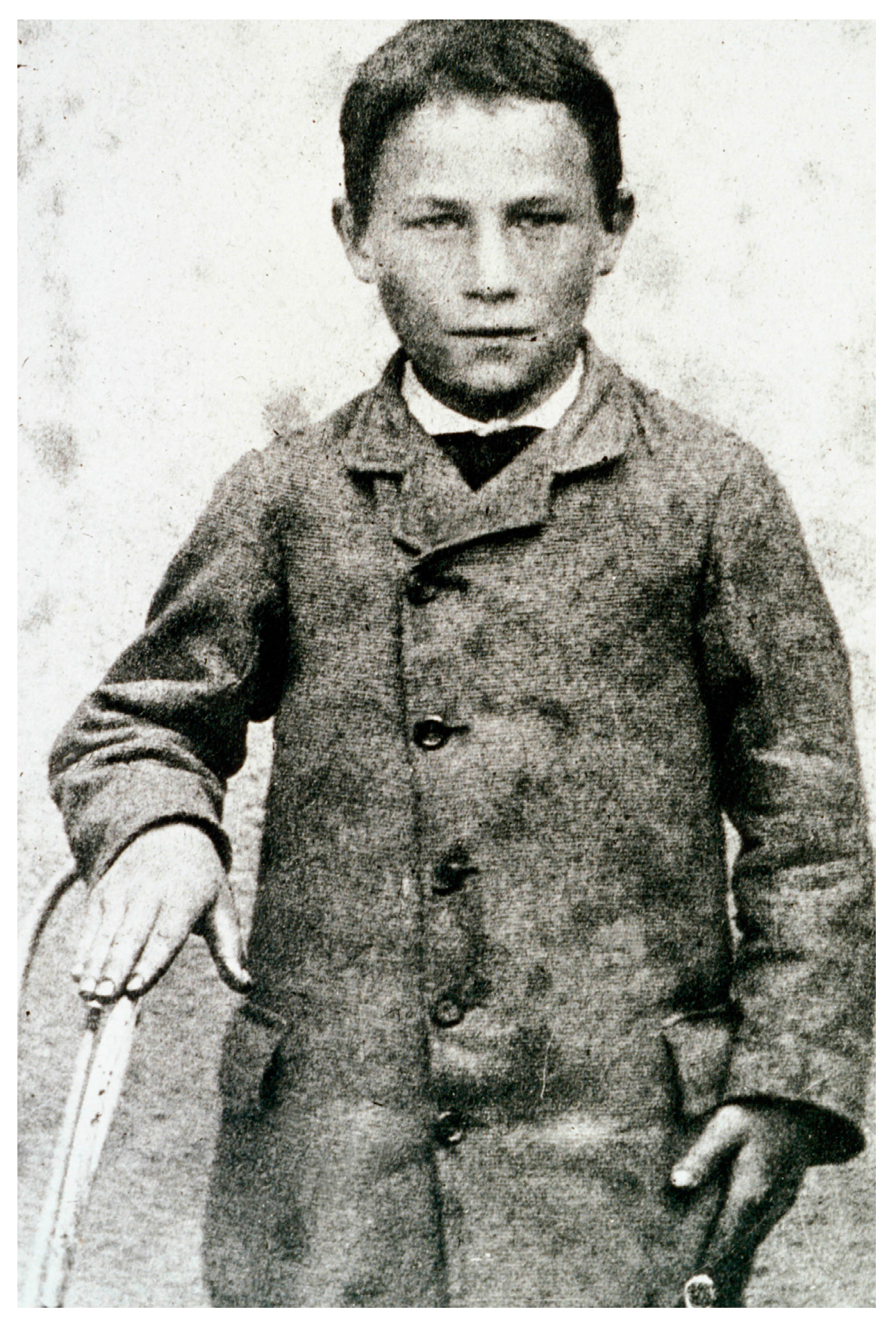
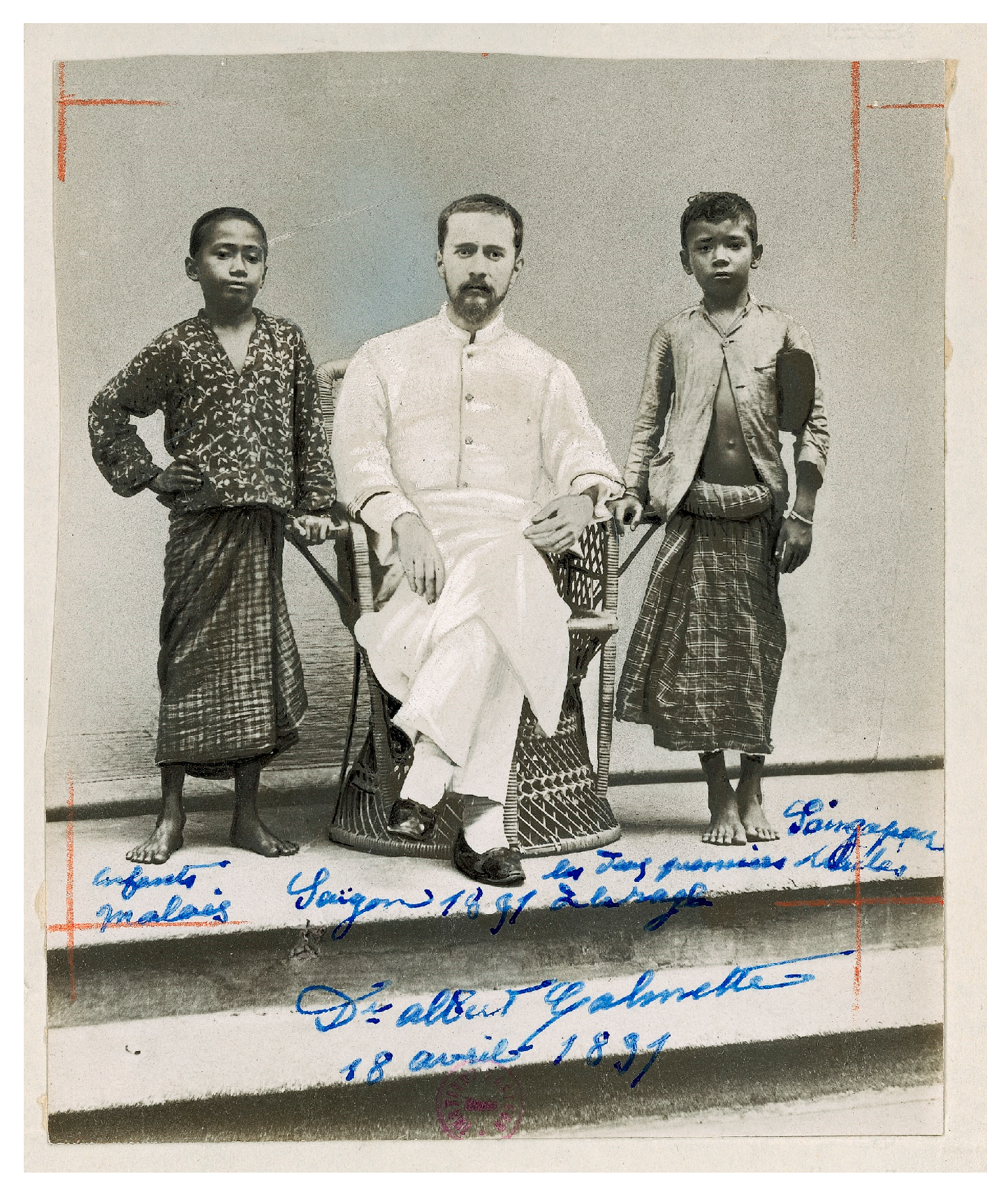
5. Pasteur and His Time
6. Modern Developments
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Dayan, T. Early domesticated dogs of the Near East. J. Archaeol. Sci. 1994, 21, 633–640. [Google Scholar] [CrossRef]
- Thalmann, O.; Shapiro, B.; Cui, P.; Schuenemann, V.J.; Sawyer, S.K.; Greenfield, D.L.; Germonpré, M.B.; Sablin, M.V.; López-Giráldez, F.; Domingo-Roura, X.; et al. Complete mitochondrial genomes of ancient canids suggest a European origin of domestic dogs. Science 2013, 342, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Armelagos, G. Disease, Darwin, and medicine in the third epidemiological transition. Evol. Anthropol. Issues News Rev. 1997, 5, 212–220. [Google Scholar] [CrossRef]
- Zuckerman, M.K.; Harper, K.N.; Barrett, R.; Armelagos, G.J. The evolution of disease: Anthropological perspectives on epidemiologic transitions. Glob. Health Action 2014. [Google Scholar] [CrossRef] [PubMed]
- Greger, M. The human/animal interface: Emergence and resurgence of zoonotic infectious diseases. Crit. Rev. Microbiol. 2007, 33, 243–299. [Google Scholar] [CrossRef] [PubMed]
- Rashidi, J.S. Paleoepidemiology of Mesopotamia and the ancient Near East: The impact of zoonotic diseases and population demographics on infectious disease patterns. Ph.D. Thesis, University of California, Los Angeles, CA, USA, 2011. [Google Scholar]
- Eshnunna. Wikipedia Free Encycl. 2014.
- Roth, M.T.; Hoffner, H.A.; Michalowski, P. Law collections from Mesopotamia and Asia Minor: Writings from the Ancient World, 2nd ed.; Scholars Press: Atlanta, GA, USA, 1997. [Google Scholar]
- Yuhong, W. Rabies and rabid dogs in Sumerian and Akkadian literature. J. Am. Orient. Soc. 2001, 121, 32. [Google Scholar] [CrossRef]
- Goetze, A. The laws of Eshnunna. Annu. Am. Sch. Orient. Res. 1965, 31, 133. [Google Scholar] [CrossRef]
- Abusch, I.T.; Toorn, K.V.D. Mesopotamian Magic: Textual, Historical, and Interpretative Perspectives; BRILL: Leiden, The Netherlands, 1999. [Google Scholar]
- Sigrist, M. On the bite of a dog. In Love and Death in the Ancient near East: Essays in Honor of Marvin H. Pope; Marks, J.H., Good, R.M., Eds.; Four Quarters Pub Co: Guilford, CT, USA, 1987. [Google Scholar]
- Veldhuis, N. An Ur III Incantation against the bite of a snake, a scorpion, or a dog. Zeitschrift für Assyriologie und Vorderasiatische Archäologie 1993, 83, 161–169. [Google Scholar] [CrossRef]
- Geller, M.J. Ur III Incantations from the Frau Professor Hilprecht-Collection, Jena; Otto Harrassowitz Verlag: Wiesbaden-Erbenheim, Germany, 2003. [Google Scholar]
- Black, J.; Green, A. Gods, Demons and Symbols of Ancient Mesopotamia: An Illustrated Dictionary: Jeremy Black, Anthony Green: 9780292707948: Amazon.com: Books; University of Texas Press: Austin, TX, USA, 2004. [Google Scholar]
- Ornan, T. The Goddess Gula and her dog. IMSA 2004, 3, 13–30. [Google Scholar]
- Swabe, J. Chapter 22: Folklore, perceptions, science and rabies prevention and control. In Historical Perspective of Rabies in Europe and the Mediterranean Basin; King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004; pp. 311–323. [Google Scholar]
- Fustel de Coulanges. La cité antique; Flammarion: Paris, France, 2009. [Google Scholar]
- Wasik, B.; Murphy, M. In the beginning. In Rabid: A Cultural History of the World’s Most Diabolical Virus; Penguin Books: New York, NY, USA, 2013; pp. 17–36. [Google Scholar]
- Menezes, R. Rabies in India. CMAJ Can. Med. Assoc. J. 2008, 178, 564–566. [Google Scholar] [CrossRef] [PubMed]
- Bhishagratna, K.K.L. Chapter VI. In An English Translation of the Sushruta Samhita, Based on Original Sanskrit Text by Susruta; Kaviraj Kunja Lal Bhishagratna: Calcutta, India, 1907; Volume 1, pp. 728–736. [Google Scholar]
- Zhang, Y.-Z.; Xiong, C.-L.; Xiao, D.-L.; Jiang, R.-J.; Wang, Z.-X.; Zhang, L.-Z.; Fu, Z.F. Human rabies in China. Emerg. Infect. Dis. 2005, 11, 1983–1984. [Google Scholar] [CrossRef] [PubMed]
- Adedeji, A.O.; Okonko, I.O.; Eyarefe, O.D.; Adedeji, O.B.; Babalola, E.T.; Ojezele, M.O.; Nwanze, J.C.; Amusan, T.A. An overview of rabies—History, epidemiology, control and possible elimination. Afr. J. Microbiol. Res. 2010, 4, 2327–2338. [Google Scholar]
- Bellini, F.; Fossati, P.; Liverini, A. L’evoluzione della rabbia attraverso i secoli. Rassegna Dirit. Legis. E Med. Leg. Vet. 2009, 8, 27–41. [Google Scholar]
- Baer, G.M. The history of rabies. In Rabies: Scientific Basis of the Disease and Its Management; Wunner, W.H., Jackson, A.C., Eds.; Academic Press: London, UK, 2010. [Google Scholar]
- Blancou, J. Chapter 2: Rabies in Europe and the Mediterranean Basin: From Antiquity to the 19th Century. In Historical Perspective of Rabies in Europe and the Mediterranean Basin; King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004; pp. 15–46. [Google Scholar]
- Yakobson, B.A.; David, D.; Aldomy, F. Chapter 13: Rabies in Israel and Jordan. In Historical Perspective of Rabies in Europe and the Mediterranean Basin; King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004; pp. 171–183. [Google Scholar]
- Fleming, G. Rabies and Hydrophobia: Their History, Nature, Causes, Symptoms, and Prevention; Chapman and Hall: London, UK, 1872. [Google Scholar]
- Rosner, F. Rabies in the Talmud. Med. Hist. 1974, 18, 198–200. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.C.; Santos-Burgoa, C. Treatment of human rabies: A summary of its history. Rev. Saúde Pública 1994, 28, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Steele, J.H.; Fernandez, P.J. The Natural History of Rabies, 2nd Edition. In The Natural History of Rabies; Baer, G.M., Ed.; CRC Press: Boca Raton, FL, USA, 1991. [Google Scholar]
- Moreau, R. La rage de l’Antiquité au Siècle des Lumières. In Pasteur et la Rage; Rosset, R., Ed.; Informations Techniques des Services Vétérinaires—Ministère de l’Agriculture; Services Vétérinaires: Paris, France, 1985; pp. 19–28. [Google Scholar]
- Jackson, A.C. Chapter 1—History of rabies research. In Rabies, 3rd ed.; Jackson, A.C., Ed.; Academic Press: Boston, MA, USA, 2013; pp. 1–15. [Google Scholar]
- Neville, J. Chapter 1: Rabies in the Ancient World. In Historical Perspective of Rabies in Europe and the Mediterranean Basin; King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004. [Google Scholar]
- Wang, Z.G.; Chen, P.; Xie, P. History and Development in Traditional Chinese Medicine; Advanced Traditional Chinese Medicine Series; Science Press/IOS Press/Ohmsha: Beijing, China; Amsterdam, The Netherlands; Tokyo, Japan, 1999. [Google Scholar]
- On the mad dog and the dog diseased; how they are to be kept, and cured. Available online: http://www.avesta.org/vendidad/vd13sbe.htm (accessed on 21 March 2017).
- Cardiff, R.D.; Ward, J.M.; Barthold, S.W. “One medicine—one pathology”: Are veterinary and human pathology prepared? Lab. Investig. J. Tech. Methods Pathol. 2008, 88, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Schwabe, C.W. History of the scientific relationships of veterinary public health. Rev. Sci. Tech. Int. Off. Epizoot. 1991, 10, 933–949. [Google Scholar] [CrossRef]
- Lucius Junius Moderatus Columella Book. In On Agriculture, with a Recension of the Text and an English Translation; Harvard University Press: Cambridge, MA, USA, 1941; Volume 2, p. 503.
- Blancou, J. Early methods for the surveillance and control of rabies in animals. Rev. Sci. Tech. Int. Off. Epizoot. 1994, 13, 361–372. [Google Scholar] [CrossRef]
- Griffith, F.L. The Demotic Magical Papyrus of London and Leiden; Griffith, F.L., Thompson, H., Eds.; H. Grevel & Co.: London, UK, 1904. [Google Scholar]
- Aulus Cornelius Celsius Book V—Chapter 27. In De Medicina; Loeb Classical Library: London, UK; W. Heinemann Ltd.: Cambridge, MA, USA; Harvard University Press: Cambridge, MA, USA, 1935; Volume 2, p. 368.
- Köckerling, F.; Köckerling, D.; Lomas, C. Cornelius Celsus—Ancient encyclopedist, surgeon–scientist, or master of surgery? Langenbecks Arch. Surg. 2013, 398, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Claudius Aelianus (Aelian) XIV. In On the Characteristics of Animals; Scholfield AF: Cambridge, MA, USA, 1959; Volume III.
- Allbutt, T.C. Greek Medicine in Rome: The Fitzpatrick Lectures on the History of Medicine Delivered at the Royal College of Physicians of London in 1909–1910, with Other Essays; Special Edition; MacMillan & Co.: London, UK, 1921. [Google Scholar]
- Menache, S. Dogs: God’s worst enemies? Soc. Anim. 1997, 5, 23–44. [Google Scholar] [CrossRef]
- Hatami, H. History of rabies in traditional medicine’s resources and Iranian research studies: On the occasion of the World Rabies Day (28 September 2012). Int. J. Prev. Med. 2012, 3, 593–595. [Google Scholar] [PubMed]
- Tadjbakhsh, H. Traditional methods used for controlling animal diseases in Iran. Rev. Sci. Tech. Int. Off. Epizoot. 1994, 13, 599–614. [Google Scholar] [CrossRef]
- Dalfardi, B.; Esnaashary, M.H.; Yarmohammadi, H. Rabies in medieval Persian literature—The Canon of Avicenna (980–1037 AD). Infect. Dis. Poverty 2014, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Arnaldi de Villanova Capitulum. XIII. De morsu canis rabidi. In Breviariuz pratice; Antonius Carcanus: Pavia, Italy, 1485. [Google Scholar]
- Théodoridès, J.; Lépine, P. Histoire de la Rage: Cave Canem; Fondation Singer-Polignac: Masson/Paris, France, 1986. [Google Scholar]
- Guitard, E.-H.; Amblard, É. L’histoire merveilleuse de la clef de saint Hubert. Rev. Hist. Pharm. 1960, 48, 369–371. [Google Scholar]
- Bazin, H. Saint Hubert, guérisseur de la rage de l’homme et des animaux. Bull. Soc. Hist. Méd. Sci. Vét. 2007, 104–126. [Google Scholar]
- Schayes, A.-G.-B. Essai Historique sur les Usages, les Croyances, les Traditions, les Cérémonies et Pratiques Religieuses et Civiles des Belges Anciens et Modernes; Chez L’auteur, 1834. [Google Scholar]
- Donaldson, I. Ambroise Paré’s accounts of new methods for treating gunshot wounds and burns. Available online: http://www.jameslindlibrary.org/articles/ambroise-pares-accounts-of-new-methods-for-treating-gunshot-wounds-and-burns/ (accessed on 26 March 2015).
- Paré, A. Les oeuvres d’Ambroise Paré; Chez Pierre Rigaud: Lyon, France, 1652. [Google Scholar]
- Pemberton, N.; Worboys, M. Mad Dogs and Englishmen: Rabies in Britain 1830–2000: Rabies in Britain, 1830–2000; Palgrave Macmillan: Basingstoke, UK, 2007. [Google Scholar]
- Pedanius Dioscorides. Wikipedia Free Encycl. 2015.
- De Vos, P. European Materia Medica in historical texts: Longevity of a tradition and implications for future use. J. Ethnopharmacol. 2010, 132, 28–47. [Google Scholar] [CrossRef] [PubMed]
- Le Paulmier de Grantmesnil, J.I. Palmarii Constantini de morsu caninis rabidi et hydrophobia, liber. In Iulii Palmarii, Constantini, medici Parisiensis, De Morbis Contagiosis Libri Septem: Ad Amplissimum Senatum Parisiensem; Cum Indice Gemino; Apud Claudium Marnium, [et] heredes Ioannis Aubrii: Parisiis, France, 1578; pp. 265–279. [Google Scholar]
- Nutton, V. Understanding contagious diseases: Baillou’s notes on Julien Le Paulmier’s De morbis contagiosis. Med. Storia 2011, 11, 141–151. [Google Scholar]
- Allan Observations sur la rage. Recl. Périodique Société Santé Paris Vendémiaire Brum. V, 1796.
- Ménécier, C. Notice sur la rage: avec un projet nouveau de police sanitaire sur la race canine: présenté à Son Excellence M. le ministre de l’agriculture et du commerce / par le docteur Charles Ménécier,...; Ad. Delahaye, Paris: Camoin, Marseille, France, 1864. [Google Scholar]
- DiMarco, V. The Bearer of Crazed and Venomous Fangs; iUniverse: Bloomington, Indiana, 2014. [Google Scholar]
- Ramasamy, S.; Liu, C.; Tran, H.; Gubala, A.; Gauci, P.; McAllister, J.; Vo, T. Principles of antidote pharmacology: an update on prophylaxis, post-exposure treatment recommendations and research initiatives for biological agents. Br. J. Pharmacol. 2010, 161, 721–748. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.D. Rabies; Biographies of Disease; Greenwood Press: Westport, CT, USA, 2009. [Google Scholar]
- Mike Nichols Nineteenth-Century Medicine: “Sir, the Madstone Will See You Now”. Available online: http://www.webcitation.org/6os1vFBQS (accessed on 12 March 2017).
- Nadin-Davis, S.A.; Bingham, J. Chapter 19: Europe as a source of rabies for the rest of the world. In Historical Perspective of Rabies in Europe and the Mediterranean Basin; King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004; pp. 259–280. [Google Scholar]
- Vos, A.; Nunan, C.; Bolles, D.; Müller, T.; Fooks, A.R.; Tordo, N.; Baer, G.M. The occurrence of rabies in pre-Columbian Central America: an historical search. Epidemiol. Infect. 2011, 139, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Troupin, C.; Dacheux, L.; Tanguy, M.; Sabeta, C.; Blanc, H.; Bouchier, C.; Vignuzzi, M.; Duchene, S.; Holmes, E.C.; Bourhy, H. Large-scale phylogenomic analysis reveals the complex evolutionary history of rabies virus in multiple carnivore hosts. PLOS Pathog. 2016, 12, e1006041. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.R. The History and Development of Caravels. Master’s Thesis, Texas A&M University, College Station, TX, USA, 2008. [Google Scholar]
- Babes, V. Traité de la Rage; Ballière: Paris, France, 1912. [Google Scholar]
- Barun, A.; Hanson, C.C.; Campell, K.J.; Simberloff, D. A review of small Indian mongoose management and eradications on islands. In IUCN; 2011; pp. 17–25. [Google Scholar]
- World Health Organization. WHO Expert Consultation on Rabies (First Report); WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Tierkel, E.S.; Arbona, G.; Rivera, A.; de Juan, A. Mongoose rabies in Puerto Rico. Public Health Rep. 1952, 67, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Styczynski, A. Human Rabies—Puerto Rico, 2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 65, 1474–1476. [Google Scholar] [CrossRef] [PubMed]
- Brown, K. Travelers and Doctors. The mystery of rabies in colonial South Africa. In Mad Dogs and Meerkats: A History of Resurgent Rabies in Southern Africa; Ohio University Press Series in Ecology and History; Ohio University Press: Athens, Greece, 2011; pp. 20–37. [Google Scholar]
- Van der Monde, N. Bepaling op Het Houden van Honden, Binnen Utrecht, in Het Jaar 1446, Des Woensdags na St. Michielsavont. In Tijdschrift voor Geschiedenis, Oudheden en Statistiek van Utrecht: Met Naamlijst der Geborenen, Ondertrouwden en Overledenen Binnen Utrecht en Voorsteden; Utrecht, The Netherlands, 1839; Volume 5, p. 603. [Google Scholar]
- Germany, P. Extrakt aus dem Edict wegen des Tollwerdens der Hunde vom 20 Februar 1787; 1787; p. 2. [Google Scholar]
- Müller, W.; Cox, J.; Müller, T. Rabies in Germany, Denmark and Austria. In Historical Perspective of Rabies in Europe and the Mediterranean Basin—A Testament to Rabies by Dr Arthur A. King; OIE—World Organisation for Animal Health: Paris, France; Weybridge, UK, 2004. [Google Scholar]
- Evans, A.S.; Kaslow, R.A. Viral Infections of Humans: Epidemiology and Control; Springer, 1997. [Google Scholar]
- Brockbank, E.M.; Edward, M. Sketches of the Lives and Work of the Honorary Medical Staff of the Manchester Infirmary, from Its Foundation in 1752 to 1830 When It Became the Royal Infirmary; Manchester University Press: Manchester, UK, 1904. [Google Scholar]
- Riddell, W.R. Hydrophobia: Four Centuries Ago. Public Health J. 1923, 14, 155–167. [Google Scholar]
- Meunier, L. Chapitre X—De la Rage (Caput X—De Rabie). In Les Trois Livres de Jérôme Fracastor sur la Contagion, les Maladies Contagieuses et Leur Traitement; Société D’éditions Scientifiques: Paris, France, 1893; p. 408. [Google Scholar]
- Hunter, J. Observations, and Heads of Inquiry, on Canine Madness, drawn from the Cases and Materials collected by the Society, reflecting that Disease. In Transactions of a Society for the Improvement of Medical and Chirurgical Knowledge; J. Johnson: London, UK, 1793; pp. 294–329. [Google Scholar]
- Swieten, G.V. An Abridgement of Baron Van Swieten’s Commentaries upon the Aphorisms of ... Herman Boerhaave Concerning the Knowledge and Cure of Diseases; printed for Robert Horsfield ... and Thomas Longman; London, UK, 1774. [Google Scholar]
- Soubiran, A.; Théodoridès, J. Guillotin et la rage: Un Mémoire inédit. Hist. Sci. Medicales 1982, 16, 227–236. [Google Scholar]
- Arboleda-Flórez, J. The ethics of biomedical research on prisoners. Curr. Opin. Psychiatry 2005, 18, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Colman, E. The first English medical journal: Medicina Curiosa. Lancet 1999, 354, 324–326. [Google Scholar] [CrossRef]
- Les protecteurs contre la rage. In Oeuvres Complètes de Mgr. X. Barbier de Montault, Prélat de la Maison de Sa Sainteté; Blais, Roy et Cie.: Poitiers, France, 1895; Volume X, pp. 169–226.
- Andry, C.L.F. Recherches sur la Rage; Chez Didot le Jeune: Paris, France, 1780. [Google Scholar]
- Debré, P. Louis Pasteur; Flammarion: Paris, France, 1997. [Google Scholar]
- Withey, D.A. Mad dog (bites) and Englishmen: early-modern remedies for hydrophobia. Dr Alun Withey.
- Diderot, D.; le Rond d’Alembert, J.R. Encycl. Ou Dict. Raison. Sci. Arts Métiers Etc 1765, 13, 758.
- Berkenhout, J. An Essay on the Bite a Mad Dog: In Which the Claim to Infallibility of the Principal Preservative Remedies against the Hydrophobia Is Examined; R. Baldwin: London, UK, 1783. [Google Scholar]
- Pankhurst, R. The history and traditional treatment of rabies in Ethiopia. Med. Hist. 1970, 14, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Bouchardat, A. Rapport général (...) sur divers remèdes proposés pour prévenir ou pour combattre la rage. Bull. Acad. Natl. Méd. 1852, 18, 6–30. [Google Scholar]
- Magendie, F. Course of the lectures on the blood and on the changes which it undergoes during disease, delivered at the College de France in 1837-8—Lecture IX. Lancet 1838, 1, 361–370. [Google Scholar]
- Buisson, F. Traité sur L’hydrophobie ou Rage. Moyen de Prévenir et de Guérir Cette Maladie par BUISSON; Impr. d’Herban: Paris, France, 1836. [Google Scholar]
- Cooper, S. A Dictionary of Practical Surgery: Comprehending All the Most Interesting Improvements, from the Earliest Times down to the Present Period; an Account of the Instruments, Remedies and Applications Employed in Surgery; the Etymology and Signification of the Principal Terms; ... Forming Together a “catalogue Raisonné” of Surgical Literature ...; Collins and Hannay: New York, 1823; Vol. II. [Google Scholar]
- Hertwig, K.H. Contribution towards a better knowledge of rabies canina [Beiträge zur nähern Kentniss der Wuthkrankheit, etc.]. In The Edinburgh Medical and Surgical Journal ...; Arch. Constable & Comp.: Edinburgh, 1829; pp. 378–389. [Google Scholar]
- Roux, E.P.P. Des Nouvelles Acquisitions sur la Rage. Thèse de Médecine, Paris, France, 1883. [Google Scholar]
- Pearce, J.M.S. Louis Pasteur and rabies: A brief note. J. Neurol. Neurosurg. Psychiatry 2002, 73, 82. [Google Scholar] [CrossRef] [PubMed]
- Rosset, R. Pasteur et les vétérinaires. Bull. Soc. Fr. Hist. Méd. Sci. Vét 2003, 2, 1–25. [Google Scholar]
- Zinke, G.G. Neue Ansichten der Hundswuth; ihrer Ursachen und Folgen, nebst einer sichern Behandlungsart der von tollen Thieren gebissenen Mensch ...; C.E. Gabler: Jena, 1804. [Google Scholar]
- Baer, G.M. The natural history of rabies; Academic Press: New York, 1975. [Google Scholar]
- Théodoridès, J. Dupuytren et la rage. Hist. Sci. Médicales 1978, 3, 241–248. [Google Scholar]
- Breschet, G. Recherches expérimentales relatives au mode de transmission de la rage. In Archives générales de médecine; IIe et nouvelle série; Béchet jeune et Labet: Paris, 1840; Vol. IX, pp. 229–231. [Google Scholar]
- Wright, S. The physiology and pathology of the saliva. The Lancet 1842, 38, 737–742. [Google Scholar] [CrossRef]
- Vassali-Eandi, A.M. Notice des ravaux de la classe des sciences physiques et mathématiques. In Mémoires de l’Académie Impériale des Sciences, Littérature et Beaux-Arts de Turin pour les Années 1805–1808. Sciences Physiques et Mathématiques; Imprimerie de l’Académie Imépriale des Sciences: Turin, Italy, 1809; p. 678. [Google Scholar]
- Duboué, P.H.; Royal College of Physicians of Edinburgh. De la Physiologie Pathologique et du Traitement Rationnel de la Rage: Suite D’études de Pathogénie; V. Adrien Delahaye: Paris, France, 1879. [Google Scholar]
- Théodoridès, J. Magendie et la pathologie infectieuse. Hist. Sci. Medicales 1983, 17, 367–380. [Google Scholar]
- Magendie, F. Leçons faites au Collège de France pendant le semestre d’hiver (1851–1852) par M. Magendie, Recueillies et Analysées par le Dr V.A. Fauconneau Dufresne; Union Médicale: Paris, France, 1862. [Google Scholar]
- Davaine, C. Recherches sur quelques questions relatives à la septicémie. Bull. Acad. Natl. Méd. 1872, A36, 907–929. [Google Scholar]
- Théodoridès, J. Casimir Davaine (1812–1882): A precursor of Pasteur. Med. Hist. 1966, 10, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Wrotnowska, D. Pasteur et Davaine d’après des documents inédits. Hist Sci. Med. 1976, 9, 213–230. [Google Scholar]
- Moreau, R. Notes sur Pasteur et la rage: A propos de quelques lettres ou documents inédits. In Pasteur et la Rage; Rosset, R., Ed.; Informations Techniques des Services Vétérinaires—Ministère de l’Agriculture; Services Vétérinaires: Paris, France, 1985; pp. 69–85. [Google Scholar]
- Perrot, A.; Schwartz, M. Pasteur et ses Lieutenants: Roux, Yersin et les autres; Odile Jacob: Paris, France, 2013. [Google Scholar]
- Hicks, G. Mr. Hicks, on hydrophobia. Lond. Med. Phys. J. 1807, 18, 272–278. [Google Scholar]
- Weiss, R.A.; Esparza, J. The prevention and eradication of smallpox: A commentary on Sloane (1755) “An account of inoculation”. Philos. Trans. R. Soc. B Biol. Sci. 2015. [Google Scholar] [CrossRef] [PubMed]
- Early Efforts at Control: Variolation, Vaccination, and Isolation and Quarantine. In Smallpox and Its Eradication; Fenner, F.; Henderson, D.A.; Arita, I.; Jezek, Z.; Ladnyi, I.D. (Eds.) History of International Public Health; World Health Organization: Geneva, Switzerland, 1988; pp. 245–276. [Google Scholar]
- Gross, C.P.; Sepkowitz, K.A. The myth of the medical breakthrough: smallpox, vaccination, and Jenner reconsidered. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 1998, 3, 54–60. [Google Scholar] [CrossRef]
- Pead, P.J. Benjamin Jesty: New light in the dawn of vaccination. Lancet 2003, 362, 2104–2109. [Google Scholar] [CrossRef]
- Pead, P.J. Benjamin Jesty: The first vaccinator revealed. Lancet 2006, 368, 2202. [Google Scholar] [CrossRef]
- Boylston, A. The origins of inoculation. J.R. Soc. Med. 2012, 105, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, S.A. Sir Hans Sloane (1660–1735): His life and legacy. Ulster Med. J. 2010, 79, 25–29. [Google Scholar] [PubMed]
- Plett, P.C. Peter Plett and other discoverers of cowpox vaccination before Edward Jenner. Sudhoffs Arch. 2006, 90, 219–232. [Google Scholar] [PubMed]
- Thurston, L.; Williams, G. An examination of John Fewster’s role in the discovery of smallpox vaccination. J.R. Coll. Physicians Edinb. 2015, 45, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Valli, E. Sulla peste di Costantinopoli del 1803 giornale del dottore Eusebio Valli cittadino fiorentino...; Presso la Società Tipografica all’Apollo: Mantova, Italy, 1805. [Google Scholar]
- Castiglioni, A. VALLI, Eusebio. Encicl. Ital. Sci. Lett. Ed Arti 1937. [Google Scholar]
- Bazin, H. L’Histoire des Vaccinations; John Libbey Eurotext: Esher (Surrey), UK, 2008. [Google Scholar]
- Denis, A.L. Disease and Society in Colonial Cuba, 1790–1840. P.h.D. Thesis, University of California, Los Angeles, CA, USA, 2007. [Google Scholar]
- Frank, J. Encyclopédie des Sciences Médicales: Ou Traité Général, Méthodique et Complet des Diverses Branches de L’art de Guérir. Médecine. Pathologie Médicale/Par Joseph Frank. Deuxième Division; Imp. de Béthune et Plon: Paris, France, 1835; Volume 1. [Google Scholar]
- Rotivel, Y.; Goudal, M.; Perrin, P.; Tordo, N. Une histoire de la vaccination contre la rage. Virologie 2002, 6, 89–104. [Google Scholar]
- Galtier, P. Etudes sur la rage. Note de M. Galtier, présentée par M. Bouley. C. R. L’Académie Sci. 1879, 89, 444–446. [Google Scholar]
- Galtier, P. Les injections de virus rabique dans le torrent circulatoire ne provoquent pas l’éclosion de la rage et semblent conférer l’immunité. La rage peut être transmise par l’ingestion de la matière rabique (Note présentée par M. Bouley). Rev. Anal. Sociétés Savantes Fr. Létranger Académie Sci. 1881, 93, 180–181. [Google Scholar]
- Smith, K.A. Louis Pasteur, the father of immunology? Immunol. Mem. 2012, 3, 68. [Google Scholar] [CrossRef] [PubMed]
- Théodoridès, J. Quelques grands précurseurs de Pasteur. Hist Sci Med 1973, 336–343. [Google Scholar]
- Rosset, R. Pierre Victor Galtier: Professeur à l’Ecole Vétérinaire de Lyon, précurseur de la vaccination antirabique. In Pasteur et la Rage; Rosset, R., Ed.; Informations Techniques des Services Vétérinaires—Ministère de l’Agriculture; Services Vétérinaires: Paris, France, 1985; pp. 41–50. [Google Scholar]
- Galtier, P. Transmission du virus rabique (Observations à l’occasion du procès-verbal). Bull Acad Méd 1881, 90–94. [Google Scholar]
- Lombard, M.; Pastoret, P.P.; Moulin, A.M. A brief history of vaccines and vaccination. Rev. Sci. Tech. Int. Off. Epizoot. 2007, 26, 29–48. [Google Scholar] [CrossRef]
- Lepine, P. Galtier and research on rabies. Bull. Acad. Natl. Med. 1969, 153, 78–81. [Google Scholar] [PubMed]
- Mérieux, C. [1879–1979. It is now one hundred years since Victor Galtier, a professor of Veterinary School in Lyon, presented a paper on the prophylaxis of rabies to the Academy of Sciences]. Bull. Acad. Natl. Med. 1979, 163, 125–127; discussion 127–128. [Google Scholar]
- Williams, E. The forgotten giants behind Louis Pasteur: Contributions by the veterinarians Toussaint and Galtier. Vet. Herit. Bull. Am. Vet. Hist. Soc. 2010, 33, 33–39. [Google Scholar]
- Toussaint, H. Note contenue dans un pli cacheté et relative à un procédé pour la vaccination du mouton et du jeune chien (Note de Toussaint présentée par M. Bouley). C. R. Acad. Sci. 1880, 91, 303–304. [Google Scholar]
- Vignal, M.W. Report on M, Pasteur’s Researches on Rabies and the Treatment of Hydrophobia by Preventive Inoculation. Br. Med. J. 1886, 1, 671–673. [Google Scholar] [CrossRef] [PubMed]
- Gibier, P. Recherches Expérimentales sur la Rage et sur son Traitement/Par Paul Gibier,...; avec Une Préface de M.H. Bouley, ...; Asselin et Houzeau: Paris, France, 1884. [Google Scholar]
- Pasteur, L. De l’atténuation du virus du choléra des poules. C. R. Acad. Sci. 1880, XCI, 673–680. [Google Scholar]
- Pasteur, L.; Chamberland, C.E.; Roux, E.P.P. Sur la vaccination charbonneuse. C. R. Acad. Sci. 1881, 92, 1378–1383. [Google Scholar]
- Pasteur, L. Note sur la maladie nouvelle provoquée par la salive d’un enfant mort de la rage. Bull. Acad. Natl. Méd. 1881. [Google Scholar]
- Rappuoli, R. Inner Workings: 1885, the first rabies vaccination in humans. Proc. Natl. Acad. Sci. USA 2014, 111, 12273–12273. [Google Scholar] [CrossRef] [PubMed]
- Pasteur, L. Méthode pour prévenir la rage après morsure. C. R. Acad. Sci. 1885, 101, 765–774. [Google Scholar]
- Pasteur, L.; Chamberland, C.E.; Roux, E.P.P. Sur la rage. Bull. Acad. Natl. Méd. 1884, 661–664. [Google Scholar]
- Suzor, J.-R. Exposé pratique du traitement de la rage par la méthode Pasteur: historique et description de la rage, collection complète des communications de M. Pasteur, technique de sa méthode, resultats statistiques, etc.; Maloine: Paris, 1888. [Google Scholar]
- Plotkin, S. History of Vaccine Development; Springer Science & Business Media, 2011. [Google Scholar]
- Joseph Meister (1876–1940). Commune de Steige.
- Rupprecht, C.E.; Plotkin, S.A. 29—Rabies vaccines. In Vaccines, 6th ed.; W.B. Saunders: London, UK, 2013; pp. 646–668. [Google Scholar]
- Dubail, A. Joseph Meister, le premier être humain sauvé de la rage. Annu. Société Hist. Val Villé 1985, 10, 93–148. [Google Scholar]
- Wolpert, L. Experiments in Deceit. New York Times, 1995. [Google Scholar]
- Geison, G.L. The Private Science of Louis Pasteur; Princeton University Press: Princeton, NJ, USA, 2014. [Google Scholar]
- Académie de Versailles Louis Pasteur: Quelques Textes. Available online: http://www.histoire.ac-versailles.fr/old/pedagogie/pasteur/pasteur_ressources.htm (accessed on 4 May 2016).
- Brunet, J.-P. La rage envers Pasteur—Ou le révisionnisme en Sciences médicales. Bull. Assoc. Anc. Elèves Inst. Pasteur 2012, 54, 112–115. [Google Scholar]
- Hansen, B. America’s first medical breakthrough: How popular excitement about a French rabies cure in 1885 raised new expectations for medical progress. Am. Hist. Rev. 1998, 103, 373–418. [Google Scholar] [CrossRef] [PubMed]
- Bazin, H. Rabies or hydrophobia vaccine. In Vaccination: A History; John Libbey Eurotext: Montrouge/France; Esher (Surrey)/UK, 2011; p. 600. [Google Scholar]
- Schwartz, M. Histoire et actualité du réseau international des Instituts Pasteur. Ann. Mines Responsab. Environ. 2008, 3, 42–48. [Google Scholar] [CrossRef]
- Ilya Mechnikov—Biographical. Available online: http://www.nobelprize.org/nobel_prizes/medicine/laureates/1908/mechnikov-bio.html (accessed on 1 April 2015).
- Botvinkin, A.; Kosenko, M. Chapter 5: Rabies in the European parts of Russia, Belarus and Ukraine. King, A.A., Fooks, A.R., Aubert, M., Wandeler, A.I., Eds.; World Organization for Animal Health: Paris, France; Weybridge, UK, 2004; pp. 47–63. [Google Scholar]
- Ulyankina, T. The Pasteur Institute and the advent of immunology in Russia (1880–1917). In Immunology—Pasteur’s Heritage; Cazenave, P.-A., Talwar, G., Eds.; Wiley Eastern Limited: New Delhi, India, 1991. [Google Scholar]
- Marie, A.A. L’étude Experimentale de la Rage; O. Doin: Paris, France, 1909. [Google Scholar]
- Bernard, P.-N. Les Instituts Pasteur d’Indochine; Saigon: Ho Hi Minh City, Vietnam, 1922; p. 249. [Google Scholar]
- Dedet, J.-P. Les Instituts Pasteurs D’outre-Mer. Cent Vingt Ansde Microbiologie Français; Editions L’Harmattan: Paris, France, 2001. [Google Scholar]
- Guénel, A. The creation of the first overseas Pasteur Institute, or the beginning of Albert Calmette’s Pastorian career. Med. Hist. 1999, 43, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Calmette, A. Notes sur la rage en Indo-Chine et sur les vaccinations antirabiques pratiquées à Saïgon du 15 Avril au 1er Août 1891. Ann. Inst. Pasteur 1891, 5, 633–641. [Google Scholar]
- Sun, B.Z. Medicine as Colonial Enterprise: The Founding of the Pasteur Institute in Saigon, 1891; Columbia University Academic Commons: New York, NY, USA, 2014. [Google Scholar]
- Smith, T.G.; Wu, X.; Franka, R.; Rupprecht, C.E. Design of future rabies biologics and antiviral drugs. Adv. Virus Res. 2011, 79, 345–363. [Google Scholar] [PubMed]
- Cabot, F. Report of experimental work on the dilution method of immunization from rabies. J. Exp. Med. 1899, 4, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Semple, D. The Preparation of a Safe and Efficient Antirabic Vaccine; Scientific Memoirs by the Officers of the Medical and Sanitary Departments of the Government of India, Sanitary Commission with the Government of India, Simla: Calcutta, India, 1911; pp. 1–32. [Google Scholar]
- Chakrabarti, P. “Living versus dead”: The Pasteurian paradigm and imperial vaccine research. Bull. Hist. Med. 2010, 84, 387–423. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Smith, T.G.; Rupprecht, C.E. From brain passage to cell adaptation: The road of human rabies vaccine development. Expert Rev. Vaccines 2011, 10, 1597–1608. [Google Scholar] [CrossRef] [PubMed]
- Babes, V.; Lepp, V. Recherches sur la vaccination antirabique. 1889, 3, 384–390. [Google Scholar]
- Hosty, T.S.; Kissling, R.E.; Schaeffer, M.; Wallace, G.A.; Dibble, E.H. Human antirabies gamma globulin. Bull. World Health Organ. 1959, 20, 1111–1119. [Google Scholar] [PubMed]
- Habel, K. Rabies prophylaxis in man. Public Health Rep. 1957, 72, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Habel, K. Seroprophylaxis in experimental rabies. Public Health Rep. 1945, 60, 545–576. [Google Scholar] [CrossRef]
- Anderson, D.A. WHO guidelines dealing with immunoglobulin use impede rabies prevention. Asian Biomed. 2007, 1, 103–107. [Google Scholar]
- Expert Committee on Rabies. Third Session; Technical Report Series; World Health Organization: Geneva, Switzerland, 1957. [Google Scholar]
- Koprowski, H.; Cox, H.R. Recent developments in the prophylaxis of rabies. Am. J. Public Health Nations Health 1951, 41, 1483–1489. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, T.; Rupprecht, C.E.; Dessain, S.K.; Rangarajan, P.N.; Thiagarajan, D.; Srinivasan, V.A. Human monoclonal antibody and vaccine approaches to prevent human rabies. Curr. Top. Microbiol. Immunol. 2008, 317, 67–101. [Google Scholar] [PubMed]
- Hanlon, C.A.; Niezgoda, M.; Morrill, P.A.; Rupprecht, C.E. The incurable wound revisited: Progress in human rabies prevention? Vaccine 2001, 19, 2273–2279. [Google Scholar] [CrossRef]
- Gogtay, N.; Thatte, U.; Kshirsagar, N.; Leav, B.; Molrine, D.; Cheslock, P.; Kapre, S.V.; Kulkarni, P.S.; SII RMab Author Group. Safety and pharmacokinetics of a human monoclonal antibody to rabies virus: A randomized, dose-escalation phase 1 study in adults. Vaccine 2012, 30, 7315–7320. [Google Scholar] [CrossRef] [PubMed]
- Muhamuda, K.; Madhusudana, S.N.; Ravi, V. Use of neutralizing murine monoclonal antibodies to rabies glycoprotein in passive immunotherapy against rabies. Hum. Vaccin. 2007, 3, 192–195. [Google Scholar] [CrossRef] [PubMed]
- De Kruif, J.; Bakker, A.B.H.; Marissen, W.E.; Kramer, R.A.; Throsby, M.; Rupprecht, C.E.; Goudsmit, J. A human monoclonal antibody cocktail as a novel component of rabies postexposure prophylaxis. Annu. Rev. Med. 2007, 58, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Van Dolleweerd, C.J.; Teh, A.Y.-H.; Banyard, A.C.; Both, L.; Lotter-Stark, H.C.T.; Tsekoa, T.; Phahladira, B.; Shumba, W.; Chakauya, E.; Sabeta, C.T.; et al. Engineering, expression in transgenic plants and characterisation of E559, a rabies virus-neutralising monoclonal antibody. J. Infect. Dis. 2014, 210, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Both, L.; van Dolleweerd, C.; Wright, E.; Banyard, A.C.; Bulmer-Thomas, B.; Selden, D.; Altmann, F.; Fooks, A.R.; Ma, J.K.-C. Production, characterization, and antigen specificity of recombinant 62-71-3, a candidate monoclonal antibody for rabies prophylaxis in humans. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2013, 27, 2055–2065. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.; Dietzschold, B.; Ertl, H.; Fooks, A.R.; Freuling, C.; Fehlner-Gardiner, C.; Kliemt, J.; Meslin, F.X.; Rupprecht, C.E.; Tordo, N.; et al. Development of a mouse monoclonal antibody cocktail for post-exposure rabies prophylaxis in humans. PLoS Negl. Trop. Dis. 2009, 3, e542. [Google Scholar] [CrossRef]
- Anonymous. Antirabies Treatment. Am. J. Public Health Nations Health 1935, 25, 857–858. [Google Scholar]
- Levaditi, C. Virus rabique et culture des cellules “in vitro”. C. R. Soc. Biol. 1913, 75, 505. [Google Scholar]
- Webster, L.T.; Clow, A.D. Propagation of rabies virus in tissue culture. J. Exp. Med. 1937, 66, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Sokol, F.; Kuwert, E.; Wiktor, T.J.; Hummeler, K.; Koprowski, H. Purification of rabies virus grown in tissue culture. J. Virol. 1968, 2, 836–849. [Google Scholar] [PubMed]
- Habel, K. Laboratory techniques in rabies. Habel test for potency. Monogr. Ser. World Health Organ. 1966, 23, 140–143. [Google Scholar] [PubMed]
- Laboratory Techniques in Rabies, 3rd ed.; Kaplan, M.M.; Koprowski, H. (Eds.) World Health Organization: Geneva, Switzerland; Philadelphia, PA, USA, 1973. [Google Scholar]
- Fuenzalida, E.; Palacios, R.; Borgono, J.M. Antirabies antibody response in man to vaccine made from infected suckling-mouse brains. Bull. World Health Organ. 1964, 30, 431–436. [Google Scholar] [PubMed]
- Molner, J.G.; Willson, R.F.; Kalish, S. Rabies control in Detroit. Am. J. Public Health Nations Health 1955, 45, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Schnurrenberger, P.R.; Anderson, G.R.; Russell, J.H. Rapidity and magnitude of antibody response to duck-embryo rabies vaccine administered as a pre-exposure regimen. Bull. World Health Organ. 1967, 37, 547–551. [Google Scholar] [PubMed]
- Kaur, M.; Garg, R.; Singh, S.; Bhatnagar, R. Rabies vaccines: Where do we stand, where are we heading? Expert Rev. Vaccines 2015, 14, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Wiktor, T.J.; Sokol, F.; Kuwert, E.; Koprowski, H. Immunogenicity of concentrated and purified rabies vaccine of tissue culture origin. Proc. Soc. Exp. Biol. Med. Soc. Exp. Biol. Med. N.Y. N. 1969, 131, 799–805. [Google Scholar] [CrossRef]
- Sikes, R.K.; Cleary, W.F.; Koprowski, H.; Wiktor, T.J.; Kaplan, M.M. Effective protection of monkeys against death from street virus by post-exposure administration of tissue-culture rabies vaccine. Bull. World Health Organ. 1971, 45, 1–11. [Google Scholar] [PubMed]
- Expert Consultation on Rabies Post-Exposure Prophylaxis; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2009.
- Baer, G.M.; Abelseth, M.K.; Debbie, J.G. Oral vaccination of foxes against rabies. Am. J. Epidemiol. 1971, 93, 487–490. [Google Scholar] [CrossRef] [PubMed]
- Wells, C.W. The control of rabies in Malaya through compulsory mass vaccination of dogs. Bull. World Health Organ. 1954, 10, 731–742. [Google Scholar] [PubMed]
- Kristensson, K.; Dastur, D.K.; Manghani, D.K.; Tsiang, H.; Bentivoglio, M. Rabies: Interactions between neurons and viruses. A review of the history of Negri inclusion bodies. Neuropathol. Appl. Neurobiol. 1996, 22, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Negri Luzzani, L. Le diagnostic de la Rage par la Démonstration du Parasite Spécifique—Résultat de Dix Ans d’Expérience (Première Partie). Ann. Inst. Pasteur J. Microbiol. Publiées Sous Patronage M Pasteur Par E Duclaux 1913, 27, 907–923. [Google Scholar]
- Negri Luzzani, L. Le diagnostic de la Rage par la Démonstration du Parasite Spécifique—Résultat de Dix Ans d’Expérience (Deuxième Partie). Ann. Inst. Pasteur J. Microbiol. Publiées Sous Patronage M Pasteur Par E Duclaux 1913, 27, 1039–1062. [Google Scholar]
- Almeida, J.D.; Howatson, A.F.; Pinteric, L.; Fenje, P. Electron microscope observations on rabies virus by negative staining. Virology 1962, 18, 147–151. [Google Scholar] [CrossRef]
- Matsumoto, S. Electron microscope studies of rabies virus in mouse brain. J. Cell Biol. 1963, 19, 565–591. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, S. Electron microscopy of nerve cells infected with street rabies virus. Virology 1962, 17, 198–202. [Google Scholar] [CrossRef]
- Flamand, A.; Delagneau, J.F. Transcriptional mapping of rabies virus in vivo. J. Virol. 1978, 28, 518–523. [Google Scholar] [PubMed]
- Tordo, N.; Poch, O.; Ermine, A.; Keith, G.; Rougeon, F. Completion of the rabies virus genome sequence determination: Highly conserved domains among the L (polymerase) proteins of unsegmented negative-strand RNA viruses. Virology 1988, 165, 565–576. [Google Scholar] [CrossRef]
- Laboratory Techniques in Rabies, 4th ed.; Meslin, F.-X.; Kaplan, M.M.; Koprowski, H.; World Health Organization (Eds.) World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Duong, V.; Tarantola, A.; Ong, S.; Mey, C.; Bourhy, H.; Dussart, P.; Buchy, P. Laboratory diagnostics in dog-mediated rabies—An overview of performance and a proposed strategy in various settings. Int. J. Infect. Dis. 2016, 46, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Briggs, D.J.; Banzhoff, A.; Nicolay, U.; Sirikwin, S.; Dumavibhat, B.; Tongswas, S.; Wasi, C. Antibody response of patients after postexposure rabies vaccination with small intradermal doses of purified chick embryo cell vaccine or purified Vero cell rabies vaccine. Bull. World Health Organ. 2000, 78, 693–698. [Google Scholar] [PubMed]
- Jaiiaroensup, W.; Lang, J.; Thipkong, P.; Wimalaratne, O.; Samranwataya, P.; Saikasem, A.; Chareonwai, S.; Yenmuang, W.; Prakongsri, S.; Sitprija, V.; et al. Safety and efficacy of purified Vero cell rabies vaccine given intramuscularly and intradermally. (Results of a prospective randomized trial). Vaccine 1998, 16, 1559–1562. [Google Scholar] [CrossRef]
- Quiambao, B.P.; Dimaano, E.M.; Ambas, C.; Davis, R.; Banzhoff, A.; Malerczyk, C. Reducing the cost of post-exposure rabies prophylaxis: Efficacy of 0.1 mL PCEC rabies vaccine administered intradermally using the Thai Red Cross post-exposure regimen in patients severely exposed to laboratory-confirmed rabid animals. Vaccine 2005, 23, 1709–1714. [Google Scholar] [CrossRef] [PubMed]
- Fekadu, M.; Shaddock, J.H.; Baer, G.M. Intermittent excretion of rabies virus in the saliva of a dog two and six months after it had recovered from experimental rabies. Am. J. Trop. Med. Hyg. 1981, 30, 1113–1115. [Google Scholar] [PubMed]
- Starr, L.E.; Sellers, T.F.; Sunkes, E.J. Apparent recovery of a dog from rabies. J. Am. Vet. Med. Assoc. 1952, 121, 296. [Google Scholar] [PubMed]
- Mshelbwala, P.P.; Ogunkoya, A.B.; Maikai, B.V. Detection of rabies antigen in the saliva and brains of apparently healthy dogs slaughtered for human consumption and its public health implications in abia state, Nigeria. ISRN Vet. Sci. 2013, 2013, 468043. [Google Scholar] [CrossRef] [PubMed]
- Cleaveland, S.; Barrat, J.; Barrat, M.J.; Selve, M.; Kaare, M.; Esterhuysen, J. A rabies serosurvey of domestic dogs in rural Tanzania: Results of a rapid fluorescent focus inhibition test (RFFIT) and a liquid-phase blocking ELISA used in parallel. Epidemiol. Infect. 1999, 123, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Follmann, E.H.; Ritter, D.G.; Beller, M. Survey of fox trappers in northern Alaska for rabies antibody. Epidemiol. Infect. 1994, 113, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.T.; Petersen, B.W.; Recuenco, S.; Niezgoda, M.; Gómez, J.; Laguna-Torres, V.A.; Rupprecht, C. Evidence of rabies virus exposure among humans in the Peruvian Amazon. Am. J. Trop. Med. Hyg. 2012, 87, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Weyer, J.; Msimang-Dermaux, V.; Paweska, J.T.; le Roux, K.; Govender, P.; Coertse, J.; Markotter, W.; Nel, L.H.; Blumberg, L.H. A case of human survival of rabies, South Africa. South. Afr. J. Infect. Dis. 2016, 31, 1–3. [Google Scholar] [CrossRef]
- Hattwick, M.A.; Weis, T.T.; Stechschulte, C.J.; Baer, G.M.; Gregg, M.B. Recovery from rabies. A case report. Ann. Intern. Med. 1972, 76, 931–942. [Google Scholar] [CrossRef] [PubMed]
- Willoughby, R.E., Jr.; Tieves, K.S.; Hoffman, G.M.; Ghanayem, N.S.; Amlie-Lefond, C.M.; Schwabe, M.J.; Chusid, M.J.; Rupprecht, C.E. Survival after treatment of rabies with induction of coma. N. Engl. J. Med. 2005, 352, 2508–2514. [Google Scholar] [CrossRef] [PubMed]
- Madhusudana, S.N.; Nagaraj, D.; Uday, M.; Ratnavalli, E.; Kumar, M.V. Partial recovery from rabies in a six-year-old girl. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2002, 6, 85–86. [Google Scholar] [CrossRef]
- Presumptive abortive human rabies—Texas, 2009. MMWR Morb. Mortal. Wkly. Rep. 2010, 59, 185–190.
- Porras, C.; Barboza, J.J.; Fuenzalida, E.; Adaros, H.L.; Oviedo, A.M.; Furst, J. Recovery from rabies in man. Ann. Intern. Med. 1976, 85, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Recovery of a patient from clinical rabies—Wisconsin, 2004. MMWR Morb. Mortal. Wkly. Rep. 2004, 53, 1171–1173.
- Recovery of a patient from clinical rabies—California, 2011. MMWR Morb. Mortal. Wkly. Rep. 2012, 61, 61–65.
- Jackson, A.C.; Warrell, M.J.; Rupprecht, C.E.; Ertl, H.C. J.; Dietzschold, B.; O’Reilly, M.; Leach, R.P.; Fu, Z.F.; Wunner, W.H.; Bleck, T.P.; et al. Management of rabies in humans. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2003, 36, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.C. Recovery from rabies. N. Engl. J. Med. 2005, 352, 2549–2550. [Google Scholar] [CrossRef] [PubMed]
- Wilde, H.; Hemachudha, T.; Jackson, A.C. Viewpoint: Management of human rabies. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 979–982. [Google Scholar] [CrossRef] [PubMed]
- Deressa, A.; Hussen, K.; Abebe, D.; Gera, D. Evaluation of the Efficacy of Crude Extracts of Salix subserrata and Silene macroselen for the treatment of rabies in Ethiopia. Ethiop. Vet. J. 2010, 14, 1–16. [Google Scholar] [CrossRef]
- Yamada, K.; Noguchi, K.; Komeno, T.; Furuta, Y.; Nishizono, A. Efficacy of favipiravir (T-705) in rabies postexposure prophylaxis. J. Infect. Dis. 2016, 213, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L.H.; Hampson, K.; Fahrion, A.; Abela-Ridder, B.; Nel, L.H. Difficulties in estimating the human burden of canine rabies. Acta Trop. 2017, 165, 133–140. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Recommended Standards and Strategies for Surveillance, Prevention and Control of Communicable Diseases. A82: Rabies; World Health Organization: Geneva, Switzerland, 1999; pp. 101–103. [Google Scholar]
- Hampson, K.; Coudeville, L.; Lembo, T.; Sambo, M.; Kieffer, A.; Attlan, M.; Barrat, J.; Blanton, J.D.; Briggs, D.J.; Cleaveland, S.; et al. On behalf of the global alliance for rabies control partners for rabies prevention estimating the global burden of endemic canine rabies. PLoS Negl. Trop. Dis. 2015, 9, e0003709. [Google Scholar]
- World Health Organization. Ebola Situation Report-30 March 2016; World Health Organization: Geneva, Switzerland, 2016; p. 12. [Google Scholar]
- Abela-Ridder, B.; Knopf, L.; Martin, S.; Taylor, L.; Torres, G.; De Balogh, K. 2016: The beginning of the end of rabies? Lancet Glob. Health 2016, 4, e780–e781. [Google Scholar] [CrossRef]
- Tarantola, A.; Ly, S.; In, S.; Ong, S.; Peng, Y.; Heng, N.Y.; Buchy, P. Rabies vaccine and rabies immunoglobulin in Cambodia: Use and obstacles to use. J. Travel. Med. 2015, 22, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Tarantola, A.; Blanchi, S.; Cappelle, J.; Ly, S.; Chan, M.; In, S.; Peng, Y.; Hing, C.; Taing, C.N.; Ly, S.; Bourhy, H.; Buchy, P.; Dussart, P.; Mary, J.-Y. Rabies postexposure prophylaxis (PEP) noncompletion after dog bites: estimating the unseen to meet the needs of the underserved. Am. J. Epidemiol 2017. (Accepted for publication). [Google Scholar]
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarantola, A. Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure. Trop. Med. Infect. Dis. 2017, 2, 5. https://doi.org/10.3390/tropicalmed2020005
Tarantola A. Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure. Tropical Medicine and Infectious Disease. 2017; 2(2):5. https://doi.org/10.3390/tropicalmed2020005
Chicago/Turabian StyleTarantola, Arnaud. 2017. "Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure" Tropical Medicine and Infectious Disease 2, no. 2: 5. https://doi.org/10.3390/tropicalmed2020005




