Development of an Antigen Capture Lateral Flow Immunoassay for the Detection of Burkholderia pseudomallei
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacteria
2.2. Ethics Statement
2.3. Immunization of Mice
2.4. Isolation of Monoclonal Antibodies
2.5. Indirect ELISA
2.6. SDS-PAGE and Western Blot
2.7. Artificial Urine
2.8. LFIA
3. Results
3.1. Bp2.1 mAb
3.2. LFIA Prototype
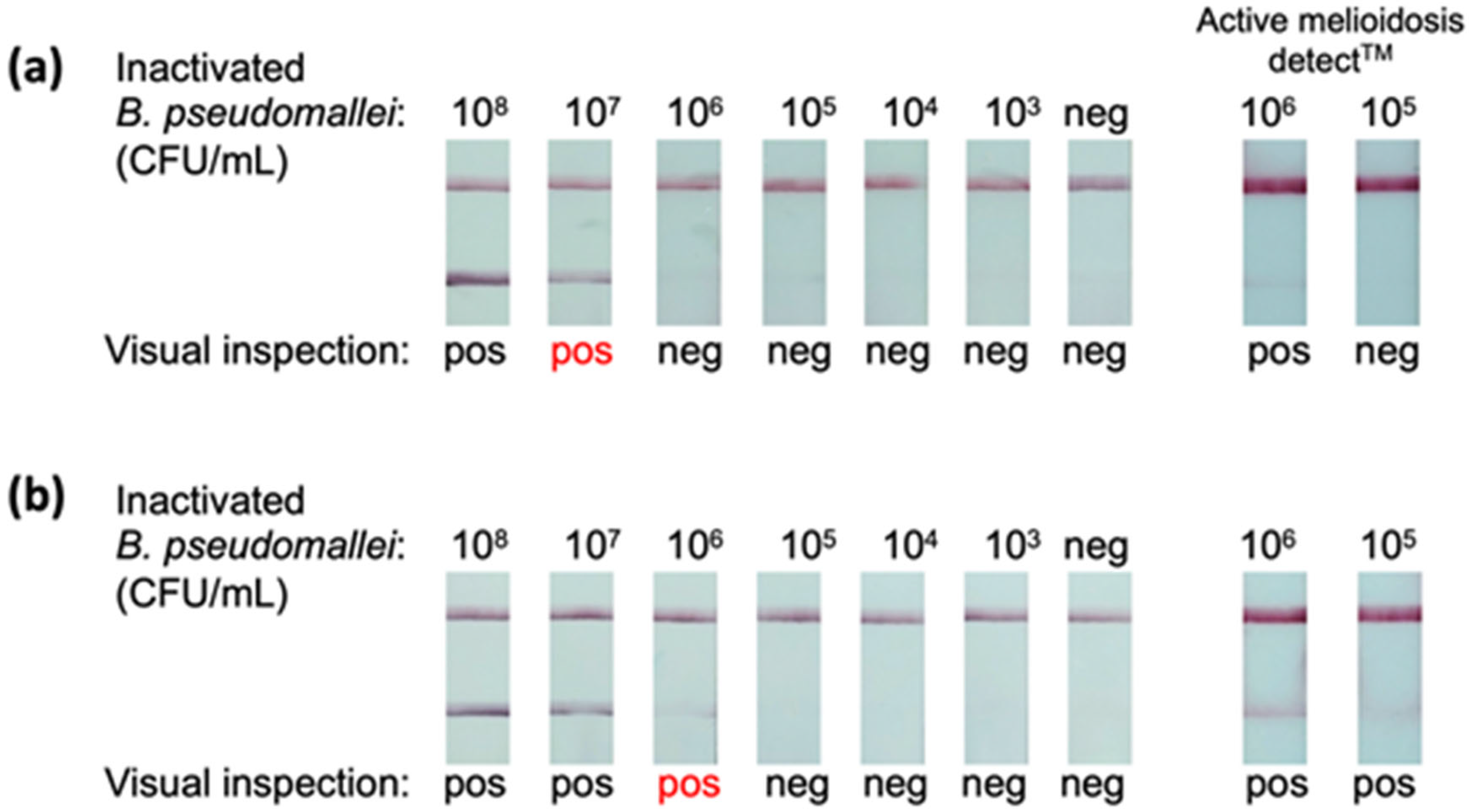
3.3. LOD
3.4. Cross-Reactivity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Phillips, E.D.; Garcia, E.C. Burkholderia pseudomallei. Trends Microbiol. 2023, 32, 105–106. [Google Scholar] [CrossRef]
- Birnie, E.; Biemond, J.J.; Wiersinga, W.J. Drivers of Melioidosis Endemicity: Epidemiological Transition, Zoonosis, and Climate Change. Curr. Opin. Infect. Dis. 2022, 35, 196–204. [Google Scholar] [CrossRef]
- Limmathurotsakul, D.; Golding, N.; Dance, D.A.B.; Messina, J.P.; Pigott, D.M.; Moyes, C.L.; Rolim, D.B.; Bertherat, E.; Day, N.P.J.; Peacock, S.J.; et al. Predicted Global Distribution of Burkholderia pseudomallei and Burden of Melioidosis. Nat. Microbiol. 2016, 1, 15008. [Google Scholar] [CrossRef] [PubMed]
- Birnie, E.; Virk, H.S.; Savelkoel, J.; Spijker, R.; Bertherat, E.; Dance, D.A.B.; Limmathurotsakul, D.; Devleesschauwer, B.; Haagsma, J.A.; Wiersinga, W.J. Global Burden of Melioidosis, 2015: A Systematic Review and Data Synthesis. Lancet Infect. Dis. 2019, 19, 892–902. [Google Scholar] [CrossRef]
- Savelkoel, J.; Dance, D.A.B.; Currie, B.J.; Limmathurotsakul, D.; Wiersinga, W.J. A Call to Action: Time to Recognise Melioidosis as a Neglected Tropical Disease. Lancet Infect. Dis. 2022, 22, e176–e182. [Google Scholar] [CrossRef] [PubMed]
- Hoffmaster, A.R.; AuCoin, D.; Baccam, P.; Baggett, H.C.; Baird, R.; Bhengsri, S.; Blaney, D.D.; Brett, P.J.; Brooks, T.J.G.; Brown, K.A.; et al. Melioidosis Diagnostic Workshop, 2013. Emerg. Infect. Dis. 2015, 21, e141045. [Google Scholar] [CrossRef] [PubMed]
- Gassiep, I.; Armstrong, M.; Norton, R. Human Melioidosis. Clin. Microbiol. Rev. 2020, 33, e00006-19. [Google Scholar] [CrossRef] [PubMed]
- Rotz, L.D.; Khan, A.S.; Lillibridge, S.R.; Ostroff, S.M.; Hughes, J.M. Public Health Assessment of Potential Biological Terrorism Agents. Emerg. Infect. Dis. 2002, 8, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Currie, B.J. Melioidosis and Burkholderia Pseudomallei: Progress in Epidemiology, Diagnosis, Treatment and Vaccination. Curr. Opin. Infect. Dis. 2022, 35, 517–523. [Google Scholar] [CrossRef]
- Meumann, E.M.; Limmathurotsakul, D.; Dunachie, S.J.; Wiersinga, W.J.; Currie, B.J. Burkholderia pseudomallei and Melioidosis. Nat. Rev. Microbiol. 2023, 22, 155–169. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Virk, H.S.; Torres, A.G.; Currie, B.J.; Peacock, S.J.; Dance, D.A.B.; Limmathurotsakul, D. Melioidosis. Nat. Rev. Dis. Primers 2018, 4, 17107. [Google Scholar] [CrossRef] [PubMed]
- DeMers, H.L.; Nualnoi, T.; Thorkildson, P.; Hau, D.; Hannah, E.E.; Green, H.R.; Pandit, S.G.; Gates-Hollingsworth, M.A.; Boutthasavong, L.; Luangraj, M.; et al. Detection and Quantification of the Capsular Polysaccharide of Burkholderia pseudomallei in Serum and Urine Samples from Melioidosis Patients. Microbiol. Spectr. 2022, 10, e00765-22. [Google Scholar] [CrossRef] [PubMed]
- Boehringer, H.R.; O’farrell, B.J. Lateral Flow Assays in Infectious Disease Diagnosis. Clin. Chem. 2021, 68, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, F.; Chiarello, M.; Cavalera, S.; Baggiani, C.; Anfossi, L. Ten Years of Lateral Flow Immunoassay Technique Applications: Trends, Challenges and Future Perspectives. Sensors 2021, 21, 5185. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Ozkaya-Ahmadov, T.; Chu, C.H.; Boya, M.; Liu, R.; Fatih Sarioglu, A. Capillary Flow Control in Lateral Flow Assays via Delaminating Timers. Sci. Adv. 2021, 7, eabf9833. [Google Scholar] [CrossRef] [PubMed]
- Houghton, R.L.; Reed, D.E.; Hubbard, M.A.; Dillon, M.J.; Chen, H.; Currie, B.J.; Mayo, M.; Sarovich, D.S.; Theobald, V.; Limmathurotsakul, D.; et al. Development of a Prototype Lateral Flow Immunoassay (LFI) for the Rapid Diagnosis of Melioidosis. PLoS Negl. Trop. Dis. 2014, 8, e2727. [Google Scholar] [CrossRef] [PubMed]
- Sarkar-Tyson, M.; Smither, S.J.; Harding, S.V.; Atkins, T.P.; Titball, R.W. Protective Efficacy of Heat-Inactivated B. Thailandensis, B. Mallei or B. pseudomallei against Experimental Melioidosis and Glanders. Vaccine 2009, 27, 4447–4451. [Google Scholar] [CrossRef] [PubMed]
- Nualnoi, T.; Kirosingh, A.; Basallo, K.; Hau, D.; Gates-Hollingsworth, M.A.; Thorkildson, P.; Crump, R.B.; Reed, D.E.; Pandit, S.; AuCoin, D.P. Immunoglobulin G Subclass Switching Impacts Sensitivity of an Immunoassay Targeting Francisella tularensis Lipopolysaccharide. PLoS ONE 2018, 13, e0195308. [Google Scholar] [CrossRef]
- Kozel, T.R.; Murphy, W.J.; Brandt, S.; Blazar, B.R.; Lovchik, J.A.; Thorkildson, P.; Percival, A.; Lyons, C.R. MAbs to Bacillus Anthracis Capsular Antigen for Immunoprotection in Anthrax and Detection of Antigenemia. Proc. Natl. Acad. Sci. USA 2004, 101, 5042–5047. [Google Scholar] [CrossRef]
- Liu, H.F.; Ma, J.; Winter, C.; Bayer, R. Recovery and Purification Process Development for Monoclonal Antibody Production. mABs 2010, 2, 480–499. [Google Scholar] [CrossRef]
- Mieczkowski, C.; Zhang, X.; Lee, D.; Nguyen, K.; Lv, W.; Wang, Y.; Zhang, Y.; Way, J.; Gries, J.M. Blueprint for Antibody Biologics Developability. mABs 2023, 15, 2185924. [Google Scholar] [CrossRef]
- Dubray, G.; Bezard, G. A Highly Sensitive Periodic Acid-Silver Stain for 1,2-Diol Groups of Glycoproteins and Polysaccharides in Polyacrylamide Gels. Anal. Biochem. 1982, 119, 325–329. [Google Scholar] [CrossRef]
- Shmaefsky, B. Artificial Urine for Laboratory Testing: Revisited. Am. Biol. Teach. 1995, 57, 428–430. [Google Scholar] [CrossRef]
- Hau, D.; Wade, B.; Lovejoy, C.; Pandit, S.G.; Reed, D.E.; Demers, H.L.; Green, H.R.; Hannah, E.E.; McLarty, M.E.; Creek, C.J.; et al. Development of a Dual Antigen Lateral Flow Immunoassay for Detecting Yersinia pestis. PLoS Negl. Trop. Dis. 2022, 16, e0010287. [Google Scholar] [CrossRef]
- Szekely, J.; Mongkolprasert, J.; Jeayodae, N.; Senorit, C.; Chaimuti, P.; Swangphon, P.; Nanakorn, N.; Nualnoi, T.; Wongwitwichot, P.; Pengsakul, T. Development, Analytical, and Clinical Evaluation of Rapid Immunochromatographic Antigen Test for SARS-CoV-2 Variants Detection. Diagnostics 2022, 12, 381. [Google Scholar] [CrossRef] [PubMed]
- Nualnoi, T.; Kirosingh, A.; Pandit, S.; Thorkildson, P.; Brett, P.J.; Burtnick, M.N.; AuCoin, D.P. In Vivo Distribution and Clearance of Purified Capsular Polysaccharide from Burkholderia pseudomallei in a Murine Model. PLoS Negl. Trop. Dis. 2016, 10, e0005217. [Google Scholar] [CrossRef] [PubMed]
- Perlmutter, R.M.; Hansburg, D.; Briles, D.E.; Nicolotti, R.A.; David, J.M. Subclass Restriction of Murine Anti-Carbohydrate Antibodies. J. Immunol. 1978, 121, 566–572. [Google Scholar] [CrossRef]
- Dillon, M.J.; Loban, R.A.; Reed, D.E.; Thorkildson, P.; Pflughoeft, K.J.; Pandit, S.G.; Brett, P.J.; Burtnick, M.N.; AuCoin, D.P. Contribution of Murine IgG Fc Regions to Antibody Binding to the Capsule of Burkholderia Pseudomallei. Virulence 2016, 7, 691–701. [Google Scholar] [CrossRef]
- Burtnick, M.N.; Heiss, C.; Roberts, R.A.; Schweizer, H.P.; Azadi, P.; Brett, P.J. Development of Capsular Polysaccharide-Based Glycoconjugates for Immunization against Melioidosis and Glanders. Front. Cell. Infect. Microbiol. 2012, 2, 108. [Google Scholar] [CrossRef]
- Koczula, K.M.; Gallotta, A. Lateral Flow Assays. Essays Biochem. 2016, 60, 111–120. [Google Scholar] [CrossRef]
- Omidfar, K.; Riahi, F.; Kashanian, S. Lateral Flow Assay: A Summary of Recent Progress for Improving Assay Performance. Biosensors 2023, 13, 837. [Google Scholar] [CrossRef]
- Roy, L.; Buragohain, P.; Borse, V. Strategies for Sensitivity Enhancement of Point-of-Care Devices. Biosens. Bioelectron. 2022, 10, 100098. [Google Scholar] [CrossRef]
- Srithong, P.; Chaiyo, S.; Pasomsub, E.; Rengpipat, S.; Chailapakul, O.; Praphairaksit, N. A Novel Delayed Lateral Flow Immunoassay for Enhanced Detection of SARS-CoV-2 Spike Antigen. Microchim. Acta 2022, 189, 386. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Shin, J.H. Pressed Lateral Flow Assay Strips for Flow Delay-Induced Signal Enhancement in Lateral Flow Assay Strips. Biochip J. 2022, 16, 480–489. [Google Scholar] [CrossRef]
- Maze, M.J.; Elrod, M.G.; Biggs, H.M.; Bonnewell, J.; Carugati, M.; Hoffmaster, A.R.; Lwezaula, B.F.; Madut, D.B.; Maro, V.P.; Mmbaga, B.T.; et al. Investigation of Melioidosis Using Blood Culture and Indirect Hemagglutination Assay Serology among Patients with Fever, Northern Tanzania. Am. J. Trop. Med. Hyg. 2020, 103, 2510–2514. [Google Scholar] [CrossRef]
- Lau, S.K.P.; Sridhar, S.; Ho, C.C.; Chow, W.N.; Lee, K.C.; Lam, C.W.; Yuen, K.Y.; Woo, P.C.Y. Laboratory Diagnosis of Melioidosis: Past, Present and Future. Exp. Biol. Med. 2015, 240, 742–751. [Google Scholar] [CrossRef]
- Wang, M.-C.; Lin, W.-H.; Yan, J.-J.; Fang, H.-Y.; Kuo, T.-H.; Tseng, C.-C.; Wu, J.-J. Early Identification of Microorganisms in Blood Culture Prior to the Detection of a Positive Signal in the BACTEC FX System Using Matrix-Assisted Laser Desorption/Ionizatione-Time of Flight Mass Spectrometry. J. Microbiol. Immunol. Infect. 2015, 48, 419–424. [Google Scholar] [CrossRef]
- Christner, M.; Rohde, H.; Wolters, M.; Sobottka, I.; Wegscheider, K.; Aepfelbacher, M. Rapid Identification of Bacteria from Positive Blood Culture Bottles by Use of Matrix-Assisted Laser Desorption-Ionization Time of Flight Mass Spectrometry Fingerprinting. J. Clin. Microbiol. 2010, 48, 1584–1591. [Google Scholar] [CrossRef] [PubMed]
- Peeters, M.; Chung, P.; Lin, H.; Mortelmans, K.; Phe, C.; San, C.; Kuijpers, L.M.F.; Teav, S.; Phe, T.; Jacobs, J. Diagnostic Accuracy of the InBiOS AMD Rapid Diagnostic Test for the Detection of Burkholderia pseudomallei Antigen in Grown Blood Culture Broth. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1169–1177. [Google Scholar] [CrossRef] [PubMed]
- Wuthiekanun, V.; Limmathurotsakul, D.; Wongsuvan, G.; Chierakul, W. Quantitation of B. pseudomallei in Clinical Samples. Am. J. Trop. Med. Hyg. 2007, 77, 812–813. [Google Scholar] [CrossRef] [PubMed]
- Woods, K.L.; Boutthasavong, L.; NicFhogartaigh, C.; Lee, S.J.; Davong, V.; AuCoin, D.P.; Dancea, D.A.B. Evaluation of a Rapid Diagnostic Test for Detection of Burkholderia pseudomallei in the Lao People’s Democratic Republic. J. Clin. Microbiol. 2018, 56, 10–128. [Google Scholar] [CrossRef] [PubMed]
- Burtnick, M.N.; Dance, D.A.B.; Vongsouvath, M.; Newton, P.N.; Dittrich, S.; Sendouangphachanh, A.; Woods, K.; Davong, V.; Kenna, D.T.D.; Saiprom, N.; et al. Identification of Burkholderia cepacia Strains That Express a Burkholderia pseudomallei-like Capsular Polysaccharide. Microbiol. Spectr. 2024, 12, e03321-23. [Google Scholar] [CrossRef] [PubMed]




| No. | Code | Components |
|---|---|---|
| 1 | KB-BS-0001 | PBS + Surfynol 465 |
| 2 | KB-BS-0002 | PBS + Surfactant 10G |
| 3 | KB-BS-0003 | PBS + Tween-80 |
| 4 | KB-BS-0004 | PBS + Tween-20 |
| 5 | KB-BS-0005 | PBS + Triton X-405 |
| 6 | KB-BS-0006 | PBS + Triton X-100 |
| 7 | KB-BS-0007 | Tris base + Casein + Surfynol 465 |
| 8 | KB-BS-0008 | Tris base + Casein + Surfactant 10G |
| 9 | KB-BS-0009 | Tris base + Casein + Tween-80 |
| 10 | KB-BS-0010 | Tris base + Casein + Tween-20 |
| 11 | KB-BS-0011 | Tris base + Casein + Triton X-405 |
| 12 | KB-BS-0012 | Tris base + Casein + Triton X-100 |
| 13 | KB-BS-0013 | Tris base + Triton X-405 |
| 14 | KB-BS-0014 | Tris base + Tween-20 |
| 15 | KB-BS-0015 | Citrate-phosphate buffer pH 5.5 |
| Parameters/Components | |
|---|---|
| Reaction pad: | Unisart CN95 |
| Conjugate pad: | Ahlstrom 8964 |
| Sample pad: | Millipore C048 |
| Absorbance pad: | Whatman 470 |
| Control line: | Goat anti-mouse IgY, 0.32 μg/strip |
| Test line: | Bp2.1 mouse IgG3, 0.32 μg/strip |
| Flow rate: | 100 mm/sec |
| Conjugates: | Bp2.1 mAb gold conjugate plus chicken IgY gold conjugate |
| Chase buffer: | KB-BS-008 |
| Strip width: | 4 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nualnoi, T.; Wongwitwichot, P.; Kaewmanee, S.; Chanchay, P.; Wongpanti, N.; Ueangsuwan, T.; Siangsanor, R.; Chotirouangnapa, W.; Saechin, T.; Thungtin, S.; et al. Development of an Antigen Capture Lateral Flow Immunoassay for the Detection of Burkholderia pseudomallei. Diagnostics 2024, 14, 1033. https://doi.org/10.3390/diagnostics14101033
Nualnoi T, Wongwitwichot P, Kaewmanee S, Chanchay P, Wongpanti N, Ueangsuwan T, Siangsanor R, Chotirouangnapa W, Saechin T, Thungtin S, et al. Development of an Antigen Capture Lateral Flow Immunoassay for the Detection of Burkholderia pseudomallei. Diagnostics. 2024; 14(10):1033. https://doi.org/10.3390/diagnostics14101033
Chicago/Turabian StyleNualnoi, Teerapat, Paweena Wongwitwichot, Siriluk Kaewmanee, Pornchanan Chanchay, Nattapong Wongpanti, Tossapol Ueangsuwan, Rattikarn Siangsanor, Wannittaya Chotirouangnapa, Tanatchaporn Saechin, Suwanna Thungtin, and et al. 2024. "Development of an Antigen Capture Lateral Flow Immunoassay for the Detection of Burkholderia pseudomallei" Diagnostics 14, no. 10: 1033. https://doi.org/10.3390/diagnostics14101033






